ABSTRACT
Background: Co-occurring posttraumatic stress disorder (PTSD) and substance use disorders (SUD) are associated with a more severe course and worse outcome than either disorder alone. In Europe, few treatments have been evaluated for PTSD and SUD. Seeking Safety, a manualized, integrated, cognitive-behavioural treatment, has been shown to be effective in studies in the USA.
Objective: To test the efficacy of Seeking Safety plus treatment as usual (TAU) in female outpatients with PTSD and SUD compared to Relapse Prevention Training (RPT) plus TAU and TAU alone.
Method: In five German study centres a total of N = 343 women were randomized into one of the three study conditions. PTSD severity (primary outcome), substance use, depression and emotion dysregulation (secondary outcomes) were assessed at baseline, post-treatment, as well as at three months and six months post-treatment.
Results: Treatment participants attended M = 6.6 sessions (Seeking Safety) and M = 6.1 sessions (RPT). In an intent-to-treat analysis, Seeking Safety plus TAU, RPT plus TAU and TAU alone showed comparable decreases in PTSD severity over the course of the study. Seeking Safety plus TAU showed superior efficacy to TAU alone on depression and emotion regulation and RPT plus TAU was more effective than TAU alone on number of substance-free days and alcohol severity. Minimum-dose analyses suggest additional effects of both programmes among participants who attended at least eight group sessions.
Conclusions: With respect to PTSD symptoms, a brief dose of Seeking Safety and RPT in addition to TAU was not superior to TAU alone in women with PTSD and SUD. However, Seeking Safety and RPT showed greater reductions than TAU alone in other domains of psychopathology and substance use outcomes respectively. Future studies should investigate further variables, such as what aspects of each treatment appeal to particular patients and how best to disseminate them.
KEYWORDS: Posttraumatic stress disorder, substance use disorder, dual diagnosis, trauma, addiction, alcohol abuse, drug abuse, randomized controlled trial, Seeking Safety, relapse prevention
HIGHLIGHTS: • We compared a treatment programme for co-occurring PTSD and substance use disorders (Seeking Safety) to another cognitive behavioural treatment (Relapse Prevention Training) and to treatment as usual (TAU).•Decreases in PTSD severity were comparable in all three conditions.• The Seeking Safety group improved more on depression and emotion regulation than TAU alone.• The Relapse Prevention group improved more on alcohol and drug use than TAU alone.
Abstract
Antecedentes: La presentación concomitante del trastorno de estrés postraumático (TEPT) y los trastornos por uso de sustancias (TUS) se asocia a un curso más severo y a un peor pronóstico que el que presentan ambos trastornos por separado. En Europa, se han evaluado pocos tratamientos para el trastorno de estrés postraumático asociado a trastornos por uso de sustancias. ‘Seeking Safety’ (‘Búsqueda de Seguridad’), un tratamiento cognitivo-conductual integrado y que cuenta con manuales de tratamiento, ha mostrado ser efectivo en estudios realizados en los Estados Unidos.
Objetivo: Probar la eficacia de ‘Búsqueda de Seguridad’ asociado al tratamiento usual (TU) en pacientes de sexo femenino con TEPT y TUS, comparada con el Entrenamiento para la Prevención de Recaídas (EPR por sus siglas en inglés) asociado a TU, y comparada con el TU únicamente.
Método: Se aleatorizó un total de N=343 mujeres de cinco sedes de estudio alemanas a cada uno de los grupos de estudio. Se evaluaron la severidad del TEPT (resultado primario), el uso de sustancias, la depresión, y la disregulación emocional (resultados secundarios) al inicio, luego de finalizar la intervención, y a los tres y seis meses luego del tratamiento.
Resultados: Las participantes asistieron a un promedio de 6,6 sesiones de ‘Búsqueda de Seguridad’ y de 6,1 sesiones de EPR. Luego de realizar el análisis por intención a tratar, ‘Búsqueda de Seguridad’ asociado a TU, EPR asociado a TU, y el TU mostraron una disminución comparable en la severidad del TEPT durante el curso del estudio. ‘Búsqueda de Seguridad’ asociado a TU mostró una eficacia superior comparada con únicamente el TU sobre la depresión y la disregulación emocional, y el EPR asociado al TU fue más efectivo que únicamente el TU en el número días libres de sustancias y en la severidad del consumo de alcohol. Los análisis de dosis mínima sugirieron efectos adicionales de ambos programas sobre las participantes que asistieron a un mínimo de ocho sesiones grupales.
Conclusiones: En relación a síntomas de TEPT, una dosis breve de ‘Búsqueda de Seguridad’ y EPR asociado a TU no fueron superiores que únicamente el TU en mujeres con TEPT asociado a TUS. Sin embargo, ‘Buscando Seguridad’ y el EPR mostraron una mayor reducción que únicamente el TU tanto en otros dominios psicopatológicos como en resultados evaluados para el uso de sustancias. Los estudios a realizarse a futuro deberían investigar variables adicionales, tales como qué aspectos de cada tratamiento van mejor con ciertos tipos particulares de pacientes, y en la mejor manera de diseminarlos.
PALABRAS CLAVES: Trastorno de Estrés Postraumático, Trastorno por Uso de Sustancias, Diagnostico Dual, Trauma, Adicción, abuso de Alcohol, abuso de drogas, Ensayo controlado aleatorio, Búsqueda de Seguridad, Prevención de Recaídas.
Abstract
背景:共病的创伤后应激障碍(PTSD)和物质使用障碍(SUD)与单独的疾病相比,其病程和后果更严重。在欧洲,很少有治疗方法针对PTSD和SUD。寻求安全是一种手册化的综合的认知行为治疗,已在美国的研究中被证明是有效的。
目的:比较寻求安全+普通治疗(TAU)VS 复发预防训练(RPT)+TAU VS 只有TAU,对患有PTSD和SUD的女性门诊患者的疗效。
方法:在五个德国研究中心,共有N = 343名女性被随机分入三个研究条件之一。在基线期,治疗后以及治疗后3个月和6个月追踪期评估PTSD严重程度(主要结果)、物质使用、抑郁和情绪失调(次要结果)。
结果:被试参加M = 6.6次寻求安全治疗和M = 6.1次RPT。治疗意向分析的结果中,寻求安全+TAU,RPT+TAU和单独TAU都显示在研究过程中相当程度的PTSD减轻。寻求安全+TAU在抑郁症和情绪调节方面表现出优于单独TAU的效果,并且RPT+TAU比单独TAU对无物质滥用天数和酒精严重程度更有效。最小剂量分析表明两个治疗项目对参加至少八次小组会议的被试有更多的影响。
结论:对患有PTSD和SUD的女性的PTSD症状而言,TAU加上轻量的寻求安全和RPT的并不优于单独TAU的效果。然而,在精神病理学的其他方面和物质滥用结果,寻求安全和RPT分别显示出比单独TAU更大的减轻效果。未来的研究应该深入调查,例如每种治疗的哪些方面对特定患者有吸引力以及如何最好地传播它们。
关键词: 创伤后应激障碍, 物质使用障碍, 双重诊断, 创伤, 成瘾, 酒精滥用, 药物滥用, 随机对照试验, 寻求安全, 复发预防
1. Introduction
Substance use disorders (SUD) are among the most prevalent comorbid disorders in individuals with posttraumatic stress disorder (PTSD) (Jacobsen, Southwick, & Kosten, 2001). In people with PTSD, rates of co-occurring alcohol use disorders range from 36 to 52% and rates for SUD other than alcohol use disorders from 19 to 35% (Roberts, Roberts, Jones, & Bisson, 2015). High rates of co-occurring SUD and PTSD have also been found in studies focussing on individuals with SUD. A review of predominantly American studies indicated that the rates of current PTSD in this population range from 15 to 41% and the rates of lifetime PTSD range from 26 to 52% (Schäfer & Najavits, 2007). European studies reported similar rates of current PTSD, ranging from 15 to 37% (e.g. Dragan & Lis-Turlejska, 2007; Driessen et al., 2008; Gielen, Havermans, Tekelenburg, & Jansen, 2012). Many studies reported higher PTSD rates among women than among men, usually about twice the rate (Driessen et al., 2008; Huang, Schwandt, Ramchandani, George, & Heilig, 2012; Langeland, Draijer, & van Den Brink, 2004).
Patients with co-occurring SUD and PTSD often present with a more severe profile than patients with PTSD or SUD alone (Schäfer & Najavits, 2007). In comparison to SUD patients without comorbid PTSD, patients with both disorders are characterized by an earlier onset of substance abuse (Johnson, Striley, & Cottler, 2006), more polysubstance use (Dragan & Lis-Turlejska, 2007), greater severity of current substance use or dependence (Clark, Masson, Delucchi, Hall, & Sees, 2001; Mills, Lynskey, Teesson, Ross, & Darke, 2005; Sells et al., 2016), reduced quality of life (Evren et al., 2011) and additional mental health problems, especially depression and anxiety disorders (Sells et al., 2016). With regard to treatment, SUD patients with PTSD have been found to show a high risk of dropout (Roberts et al., 2015) and worse treatment outcomes in comparison to patients with SUD only (Najavits et al., 2007), although a recent systematic review found that a negative effect of PTSD on SUD treatment outcomes was not consistently reported (Hildebrand, Behrendt, & Hoyer, 2015). PTSD-SUD patients with a history of childhood trauma often suffer from additional problems that are characteristic for complex PTSD (Karatzias et al., 2017). These problems typically comprise difficulties in emotion regulation, interpersonal functioning and impaired sense of self (Hien, Cohen, & Campbell, 2005).
There is a solid evidence base for the effectiveness of psychosocial interventions addressing either disorder alone, e.g. motivational enhancement therapy, cognitive behavioural therapies (CBT) such as relapse prevention or 12-step-facilitation for SUD (Kleber et al., 2007), and CBT, cognitive therapy, eye movement desensitization and reprocessing therapy (EMDR), and exposure therapy for PTSD (Courtois et al., 2017). For the treatment of patients with both disorders, interventions from both fields have been integrated in a variety of treatment models. Such models conceptualize both disorders as related and address them in a common treatment approach, which can be appealing to both patients and providers.
One of the best established integrated treatments for PTSD and SUD is Seeking Safety (Najavits, 2002), a manualized CBT model. Seeking Safety offers 25 topics, each a safe coping skill relevant to both PTSD and SUD in four domains (cognitive, behavioural, interpersonal and case management). The major goal is to increase the patient’s safety in their behaviour, thinking and relationships, i.e. to reduce PTSD symptoms, substance use and other unsafe behaviours including abusive relationships and self-harm. The programme has been translated into various European languages and can be flexibly used across all levels of care. In the USA, Seeking Safety has been investigated in a variety of vulnerable populations comprising, e.g. outpatient women and men (Najavits, Schmitz, Gotthardt, & Weiss, 2005; Najavits, Weiss, Shaw, & Muenz, 1998), adolescent girls (Najavits, Gallop, & Weiss, 2006), veterans (Boden et al., 2012), homeless women (Desai, Harpaz-Rotem, Najavits, & Rosenheck, 2008) or prisoners (Lynch, Heath, Mathews, & Cepeda, 2012; for an overview, see seekingsafety.org). One meta-analysis has been conducted on controlled studies of Seeking Safety by Lenz, Henesy, and Callender (2016), representing over 1900 patients. They found medium effect sizes for decreasing PTSD symptoms and modest effects for decreasing SUD symptoms. Among the subset of comparisons of active treatments, however, there were no significant differences. This latter finding mirrors the larger literature on comparisons of active treatment models for PTSD alone, SUD alone, and PTSD/SUD, which consistently show no significant differences between them (Hoge & Chard, 2018; Imel, Wampold, Miller, & Fleming, 2008; Simpson, Lehavot, & Petrakis, 2017). Lenz et al. (2016) also noted in their meta-analysis of Seeking Safety that their results are limited by the characteristics of the available evidence, e.g. few eligible studies and lack of follow-up assessments.
In Europe, integrated treatments for patients with co-occurring SUD and PTSD are not provided in a routine way, representing a substantial gap of services for these patients. Given the differences between health care systems and cultures, there is a need to evaluate the existing programmes in the respective countries (Magruder, McLaughlin, & Elmore Borbon, 2017). Two studies of Seeking Safety in Germany showed a good acceptance of the programme by the participants (Schäfer et al., 2010) and at least medium sized effects on PTSD symptoms, general psychopathology, interpersonal problems and alcohol use (Kaiser et al., 2015). However, both were uncontrolled studies and RCTs on Seeking Safety in Europe do not exist so far.
To address this research gap, our study compares Seeking Safety plus treatment as usual (TAU) to Relapse Prevention Training (RPT) plus TAU and to a TAU control. RPT, a standard SUD treatment, was chosen as an active control condition because it has been shown to be effective for reducing symptoms of PTSD and substance use in individuals with co-occurring PTSD and SUD (Hien, Cohen, Miele, Litt, & Capstick, 2004; Ruglass et al., 2017). The primary hypothesis was that Seeking Safety plus TAU would outperform TAU alone on PTSD reduction, but not differ from RPT plus TAU. Secondary hypotheses were analogous to the primary hypotheses but on substance use, depression and emotion regulation.
2. Methods
2.1. Design
This clinical trial used a multisite, randomized, controlled design to investigate the efficacy of an integrated treatment for PTSD and SUD (Seeking Safety; Najavits, 2002) compared to an active control group (Relapse Prevention Training; Körkel & Schindler, 2003), both in addition to TAU, and a TAU only control. It was part of a larger research network on relationships between trauma and substance abuse (CANSAS-Network; Schäfer et al., 2017). The trial was registered at the German Clinical Trials Register under the ID DRKS00004288.
2.2. Participants
The participants of this trial were recruited between September 2012 and June 2015 at the University Medical Center of Hamburg-Eppendorf, Germany, and four cooperating study centres at hospitals in large cities in Northern and Western Germany (Bielefeld, Essen, Hannover, Cologne). All study centres were substance abuse treatment departments of the respective hospitals. Study participants were recruited via substance abuse and other psychosocial counselling agencies, substance abuse and mental health clinics, psychotherapists in private practice and in the community (e.g. advertisements in subway trains, local radio and newspapers, supermarkets, online advertisements). Inclusion criteria were female sex, age 18–65, subthreshold PTSD (i.e. criterion A, B and either C or D) or full PTSD and a substance use disorder with last substance use within the previous 12 months, both according to DSM-IV criteria (American Psychiatric Association, 2000). Given that group treatments for posttraumatic disorders should preferably take place in gender-specific groups (Greenfield et al., 2007) and that the prevalence of PTSD is markedly higher in women with SUD as compared to men (Schäfer & Najavits, 2007), the study focused on female patients. Subthreshold or partial PTSD is associated with symptom distress that is comparable to full PTSD and is therefore recognized as clinically relevant (Pietrzak, Goldstein, Southwick, & Grant, 2011; Zlotnick, Franklin, & Zimmerman, 2002). Exclusion criteria were current psychosis, severe cognitive impairment and intravenous drug use within four weeks before start of study participation. We did not exclude patients with suicide or violence ideation, bipolar disorder, homelessness or criminal justice involvement. Written informed consent was obtained from all participants.
2.3. Procedures
Participants completed a baseline assessment that included semi-structured interviews and self-report scales. After the baseline assessment, they were randomized into one of the three intervention conditions: (1) Seeking Safety plus TAU, (2) Relapse Prevention Training plus TAU or (3) TAU only. Blocked randomization lists with randomly mixed block sizes were generated for each study site. An independent researcher at the coordinating study site administered the randomization lists and revealed study condition assignments to the site coordinator, who then informed the participant and the study therapist. Participants in Seeking Safety and RPT were offered 16 sessions in total: one individual introductory session with the study therapist before starting the group modality, then 14 weekly group sessions, each 90 minutes, followed by an individual termination session. Within two weeks of the termination session (or an equal time interval from baseline in case of the TAU condition or treatment dropout) a post-treatment assessment was scheduled. Additional follow-up assessments took place at three and six months post-treatment. Post-treatment and follow-up assessments were conducted by trained, blinded raters. Remuneration for each study assessment was €20 to €50 depending on the time point (baseline, post-treatment and follow-up assessments). All study procedures were approved by the ethics committees of the medical associations at each study site.
2.4. Interventions
Seeking Safety (Najavits, 2002), as described earlier, is a manualized, integrated, present-focused coping skills model to address PTSD and SUD at the same time, by the same therapist. Each topic provides a coping skill relevant to both disorders. For this study, 16 of the 25 Seeking Safety topics were selected in consultation with the treatment developer: introduction/case-management, detaching from emotional pain (grounding), safety, when substances control you, red and green flags, asking for help, setting boundaries in relationships, self-nurturing, PTSD: taking back your power, commitment, recovery thinking, coping with triggers, honesty, integrating the split self, healing from anger and termination. All were delivered in group modality except the first and last topics, which were individual.
Relapse Prevention Training (German version ‘S.T.A.R.’; Körkel & Schindler, 2003) is a manualized cognitive-behavioural group training. It was originally developed for alcohol dependent patients but for the purpose of this study all was applied to SUD in general. It teaches skills to prevent substance relapse and to manage a relapse once it has happened. Each session covers a different module and is highly structured. Of the 15 ‘S.T.A.R.’ modules, 14 were used in this trial, plus we added an individual introductory session and a termination session so as to be comparable to Seeking Safety.
As the treatment groups of both interventions were conducted as open enrolment groups, group size could vary from one session to another. Groups consisted of up to eight participants. A total of 39 therapists across all study sites delivered the treatment groups. Most therapists were psychologists, others were psychiatrists, substance abuse counsellors, social workers, nurses or occupational therapists. They received two days of training in Seeking Safety or RPT. RPT therapist training was delivered by the group of the programme author in German. For Seeking Safety, a first training was provided by the author of the programme in English, with simultaneous translation to German, where necessary. As further therapists were recruited during the ongoing study, these were trained by the study team that had also realized the German translation and adaption of the Seeking Safety manual in close cooperation with the original author. Therapists delivered only one of the two active treatments over the course of the study, but not both. Group sessions were audiotaped to ensure treatment manual adherence. Two raters for the respective treatments rated adherence to the treatment manual of a randomized selection of 10% of all group sessions and gave feedback to the therapists. The raters were trained to evaluate adherence to the treatment manual by the groups of the programme developers.
TAU meant that participants irrespective of treatment condition were free to engage in any additional treatment for SUD, PTSD or other problems throughout study participation. Participants in the TAU control group did not receive any study intervention (i.e. Seeking Safety or RPT) but they were given the opportunity to participate in the treatment after their last assessment. Both Seeking Safety and RPT were offered in addition to TAU.
2.5. Measures
2.5.1. Background information
Sociodemographic and clinical background information such as age, employment, history of treatment for SUD and PTSD and history of suicide attempts was assessed as part of the comprehensive baseline assessment via a structured interview. PTSD, SUD and co-occurring axis I diagnoses were assessed with the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1997). Traumatic life events were assessed using the traumatic events checklist of the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) and the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998), two validated self-report measures. At the post-treatment and follow-up interviews, participants were also asked about any additional treatment engagement, further traumatic events and other severe adverse events (SAEs, e.g. increases in suicidality, unplanned hospital admissions).
2.5.2. Primary outcomes
PTSD symptom severity was assessed with the PTSD Symptom Scale Interview (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993). The PSS-I is a structured interview for the rating of the frequency and severity of the 17 criteria of the DSM-IV PTSD clusters intrusions, avoidance and hyperarousal. Ratings addressed the symptom severity in the past two weeks. The psychometric properties of the PSS-I have been studied in patients with PTSD and alcohol dependence and revealed good to excellent parameters of reliability and validity (Powers, Gillihan, Rosenfield, Jerud, & Foa, 2012). To ensure rater competency and interrater reliability, all raters received an initial training and supervision. Furthermore, there were regular conference calls with the study supervisory team in which individual ratings of audiotaped interview examples were compared and discussed.
In addition, PTSD severity was self-reported by participants using the PDS (Foa et al., 1997). The scale yields severity scores for the three symptom clusters and a total score. The PDS shows good reliability and validity in individuals with comorbid PTSD and alcohol dependence (Powers et al., 2012).
2.5.3. Secondary outcomes
To gather information on participants’ substance use, the Addiction Severity Index-lite (ASI-lite; Kokkevi & Hartgers, 1995; McLellan et al., 1992) was administered. The ASI-lite is a structured interview yielding composite scores for severity of substance use and related problems in the past 30 days. ASI composite scores range between 0 and 1, with higher values indicating higher severity. For the present study, an additional item assessing the number of substance-free days in the last 30 days was included.
Depression was assessed by the Beck Depression Inventory II (BDI-II; Beck, Steer, & Brown, 1996). The BDI-II is a standard self-rating instrument for depressive symptoms. BDI-II scores are highly reliable and valid across different populations (Hautzinger, Keller, & Kühner, 2006).
To assess emotion dysregulation, the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was applied. This self-report scale measures emotion regulation difficulties across six dimensions (nonacceptance of emotional responses, difficulties engaging in goal-directed behaviour when distressed, impulse control difficulties when distressed, lack of awareness of emotions, limited access to strategies for regulation and lack of emotional clarity). It yields a total emotion dysregulation score as well as six subscale scores. The DERS demonstrates good psychometric properties (Gratz & Roemer, 2004).
2.6. Statistical analyses
2.6.1. Sample size
Based on the results of a comparable trial (Hien et al., 2004), n = 67 evaluable patients per group (total: N = 201) were hypothesized a priori to be sufficient to reach a power of 80% in each of the three possible two-group comparisons, applying the closure-test-principle (alpha = 0.05). Prospectively considering 15% drop-outs during treatment and another 30% to six-month follow-up, 342 patients needed to be allocated to the trial to obtain N = 201 evaluable patients. As recruitment proceeded slower than anticipated, two study sites (Cologne and Hannover) were added to the initial three sites (Hamburg, Essen, Bielefeld) and the recruitment phase was extended from 21 to 34 months.
2.6.2. Descriptive statistics
For the provision of sample characteristics, means, medians or frequencies and percentages were computed and compared between treatment groups. Baseline group differences were examined using χ2 – tests for categorical variables, one-way ANOVAs for continuous data and Kruskal-Wallis-H-tests for non-normally distributed count data.
2.6.3. Data analysis
Baseline adjusted mixed effect models for repeated measures (MMRM) with participant as repeated structure and study site as random effect/cluster were applied for the primary and secondary outcomes. This approach uses all available cases, so potential missing values at a follow-up do not result in an exclusion of the participant. If the random effect was not significant in the sense of variance explanation, it was excluded to simplify the model. To report standardized effect estimates and the corresponding 95% confidence intervals the models were calculated using the structural equation modelling (SEM) approach. A further benefit of SEM is that the full information maximum-likelihood (FIML) method can be used to deal with missing values within variables (Dong & Peng, 2013).
To estimate the effect of the intervention on the outcome during the study, the factors group assignment and time point of measurement (follow-up) and their interaction were included in the model to test, if the intervention effects differed over time. In the case of an insignificant interaction term only the main effects group assignment and time point of measurement remained in the model. Furthermore the baseline value of the respective outcome was included to increase the power of the analysis and to adjust for potential confounding. As participants in all intervention groups were free to engage in additional treatments during their study participation, in a second approach ancillary treatment effect analyses were conducted adjusting for the extent of additional outpatient, inpatient and PTSD treatment.
Per intent-to-treat analysis, all participants were included in the models, regardless of the dose of intervention participants received. In addition, minimum-dose analyses were conducted for participants attending at least nine treatment sessions (the introduction session plus eight group sessions) applying the same models as described above. A two-tailed p < .05 was considered to be statistically significant. Baseline descriptive analyses were conducted using SPSS for Windows 22 (IBM Corp., 2013), and Stata 14.1 (Stata Corp., 2015) was used for all analyses of treatment effects.
3. Results
3.1. Sample characteristics
The participant flow from screening through six-month follow-up is illustrated in Figure 1. A total of 610 women were screened for eligibility. Of these, 343 participants were randomized. Table 1 presents the demographic and psychiatric characteristics of the sample. Most participants were unemployed (77.8%) and had a low monthly income (54.4% with less than €1000/month). Alcohol, cannabis and sedatives were the most frequently abused substances. Nearly every participant (94.5%) had at least one substance dependence diagnosis and the remaining 5.5% met substance abuse criteria. About one-fifth (21.3%) reported no alcohol or substance use in at least 30 days prior to the baseline assessment. There were no significant differences between treatment conditions on any of the above demographic, substance use-related or psychiatric variables.
Figure 1.
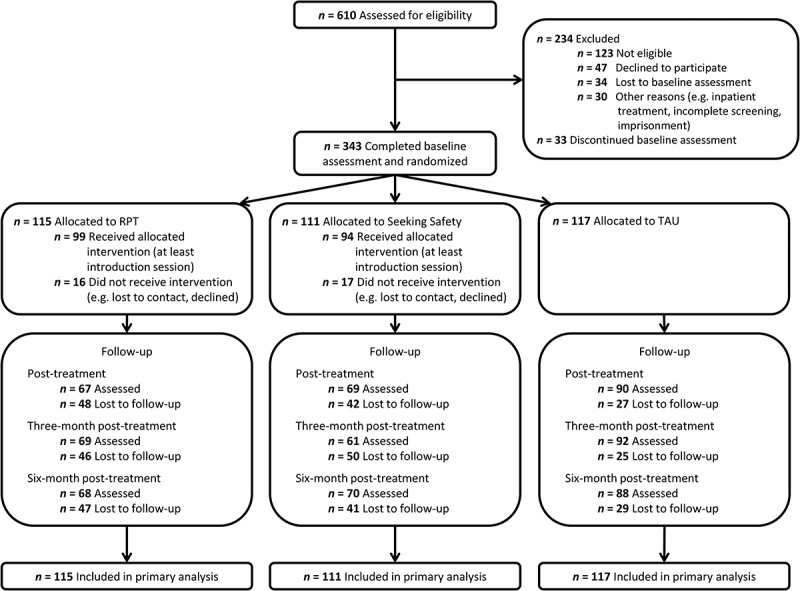
CONSORT diagram of participant flow through the protocol. RPT = Relapse Prevention Training, TAU = treatment as usual.
Table 1.
Demographic and baseline clinical characteristics by treatment group.
|
n (%)1 |
||||
|---|---|---|---|---|
| Characteristic | Seeking Safety (n = 111) |
RPT (n = 115) |
TAU (n = 117) |
Total (n = 343) |
| Demographic | ||||
| Age, mean (SD) | 41.5 (11.7) | 40.3 (11.3) | 41.1 (11.2) | 40.9 (11.4) |
| School years complete, median (range) | 10 (7–13) | 10 (7–13) | 11 (7–13) | 10 (7–13) |
| Born in Germany | 101 (91.0) | 108 (93.9) | 101 (86.3) | 310 (90.4) |
| Married | 17 (15.3) | 21 (18.3) | 18 (15.4) | 56 (16.3) |
| Unemployed or marginally employed | 89 (80.2) | 90 (78.3) | 88 (75.2) | 267 (77.8) |
| Monthly household net income < €1000 | 59 (53.2) | 61 (53.5)a | 66 (56.4) | 186 (54.4) |
| Substance use disorder | ||||
| Alcohol | 88 (79.3) | 100 (87.0) | 102 (87.2) | 293 (85.4) |
| Sedatives | 40 (37.0)b | 38 (33.0) | 28 (23.9) | 106 (31.2) |
| Cannabis | 53 (49.1)b | 58 (50.4) | 54 (46.2) | 165 (48.5) |
| Stimulants | 30 (27.5)c | 25 (21.7) | 41 (35.0) | 96 (28.2) |
| Opiates | 24 (21.8)d | 26 (22.6) | 23 (19.7) | 73 (21.3) |
| Cocaine | 34 (31.5)b | 29 (25.2) | 34 (29.1) | 97 (28.5) |
| 30-day abstinence | 28 (25.2) | 22 (19.1) | 23 (19.7) | 73 (21.3) |
| Prior substance abuse treatment | 74 (66.7) | 75 (65.2) | 77 (66.4)e | 226 (66.1) |
| Childhood traumaf | ||||
| Emotional abuse | 84 (77.1)c | 99 (86.1) | 84 (72.4)e | 267 (78.5)* |
| Physical abuse | 51 (45.9) | 71 (61.7) | 57 (48.7) | 179 (52.2)* |
| Sexual abuse | 80 (72.1) | 91 (79.1) | 78 (67.2)e | 249 (72.8) |
| Emotional neglect | 77 (70.0)d | 98 (86.0)a | 86 (73.5) | 261 (76.5)* |
| Physical neglect | 64 (58.2)d | 79 (68.7) | 66 (56.4) | 209 (61.1) |
| Lifetime traumatic experiences | ||||
| Serious accident | 43 (38.7) | 37 (32.5)a | 36 (31.3)g | 116 (34.1) |
| Natural disaster | 1 (0.9) | 2 (1.8)h | 7 (6.1)a | 10 (3.0) |
| Family non-sexual assault | 80 (72.1) | 83 (72.8)a | 87 (75.0)e | 250 (73.3) |
| Stranger non-sexual assault | 57 (51.8)d | 53 (46.5)a | 48 (41.7)g | 158 (46.6) |
| Family sexual assault | 70 (63.1) | 79 (69.3)a | 61 (52.6)e | 210 (61.6)* |
| Stranger sexual assault | 69 (62.7)d | 61 (53.5)a | 64 (55.2)e | 194 (57.1) |
| Military combat | 1 (0.9) | 1 (0.9)h | 2 (1.7)g | 4 (1.2) |
| Sexual contact (< 18 years/partner 5+ years older) | 75 (67.6) | 89 (78.1)a | 77 (65.8) | 241 (70.5) |
| Captivity/Imprisonment | 13 (11.8)d | 19 (16.7)a | 14 (12.2)g | 46 (13.6) |
| Torture | 7 (6.4)d | 15 (13.3)h | 11 (9.6)g | 33 (9.8) |
| Life-threatening illness | 27 (24.3) | 23 (20.2)a | 28 (24.3)g | 78 (22.9) |
| Other traumatic event | 70 (64.2)c | 69 (62.2)i | 68 (60.7)j | 207 (62.3) |
| PTSD/Treatment | ||||
| Subthreshold PTSD | 26 (23.4) | 28 (24.3) | 31 (26.5) | 85 (24.8) |
| Prior trauma treatment | 30 (27.0) | 31 (27.0) | 19 (16.4)e | 80 (23.4) |
| Current mental health comorbidity | ||||
| Major depression | 44 (40.0)d | 56 (49.1)a | 53 (45.3) | 153 (44.9) |
| Anxiety disorder | 69 (62.2) | 73 (63.5) | 79 (67.5) | 221 (64.4) |
| Ever attempted suicide | 63 (56.8) | 67 (58.3) | 67 (58.3)g | 197 (57.8) |
| No. of suicide attempts, median (range) | 2 (1–25)k | 2 (1–20)l | 2 (1–50) | 2 (1–50) |
1If not otherwise specified. a n = 114. b n = 108. c n = 109. d n = 110. e n = 116. f At least moderate to severe (Childhood Trauma Questionnaire). g n = 115. h n = 113. i n = 111. j n = 112. k n = 62. l n = 66. * Significant between-group difference with p < .05. RPT = Relapse Prevention Training, TAU = treatment as usual.
With regard to trauma, most participants (93.3%) reported at least one type of childhood abuse. This rate was higher in the RPT group (98.3%) than in the Seeking Safety (91.0%) and TAU conditions (90.6%, χ2(2) = 6.84, p = .033). This difference was mainly due to significantly higher rates of emotional abuse (χ2(2) = 6.61, p = .037), physical abuse (χ2(2) = 6.50, p = .039) and emotional neglect (χ2(2) = 8.86, p = .012) in the RPT group compared to the Seeking Safety and the TAU conditions. The most common lifetime traumatic experiences reported were non-sexual assault within the family, sexual contact under the age of 18 with someone at least five years older, other traumatic events, and sexual assault within the family. There were no differences in the rates of traumatic experiences between the treatment conditions, except for sexual assault within the family which was significantly more prevalent among participants in RPT compared to Seeking Safety and TAU (χ2(2) = 6.94, p = .031). Participants reported a median of four trauma types (range 1–10). All participants met DSM-IV criteria for either subthreshold (24.8%) or full PTSD (75.2%). Additional Axis-I disorders and lifetime suicidality were also prevalent in this sample (see Table 1).
3.2. Treatment adherence
In the two treatment conditions, 15.3% (Seeking Safety) and 13.9% (RPT) of the participants did not start treatment after randomization. All other participants randomized to one of the treatments attended at least the introductory session. The mean number of sessions attended was 6.6 (SD = 5.1, range = 0–16) in Seeking Safety and 6.1 (SD = 4.9, range = 0–16) in RPT, with no significant difference between them (41.3% vs. 38.1% of available sessions; OR = 1.06, p = .671, unadjusted beta-binomial regression model). The proportion of participants attending at least eight of the 14 group sessions (‘minimum dose’) was 36.9% (n = 41) in Seeking Safety and 28.7% (n = 33) in RPT (χ2(1) = 1.74, p = .187).
3.3. Primary outcome analyses
3.3.1. Posttraumatic stress disorder (PTSD)
Statistical analyses showed no significant interaction effects of time by group on interviewer-rated (PSS-I) or self-rated (PDS) PTSD severity (see Table 2). There was a significant main effect of time on PSS-I PTSD severity scores (p = .001), but no significant effect of group (p = .748), indicating that baseline-adjusted PTSD severity scores decreased comparably in the three conditions (post-treatment–three-month follow-up = 1.38, 95% CI 0.15 to 2.61, p = .028; three-month follow-up–six-month follow-up = 0.89, 95% CI −0.34 to 2.12, p = .155; see Figure 2 for observed courses). Likewise, baseline-adjusted PDS severity scores changed significantly over time (p = .006), but there was no significant group effect (p = .153). Contrasts indicated a significant reduction in PDS scores from three- to six-months follow-up (post-treatment–three-month follow-up = 0.68, 95% CI − 0.68 to 1.87, p = .330; three-month follow-up–six-month follow-up = 1.36, 95% CI 0.17 to 2.55, p = .028). See Table 2 for observed values and between-group effects of all primary and secondary outcomes.
Table 2.
Means and standard deviations (observed values) for the primary and secondary outcomes over the study course and model based effect sizes (d) with 95%-confidence intervals for baseline-adjusted between-group differences at post-treatment and follow-up assessments for the intention-to-treat sample (n = 343).
|
M (SD) |
d (95% CI) |
|||||
|---|---|---|---|---|---|---|
| Outcome | SeSa | RPT | TAU | SeSa-TAU | SeSa-RPT | RPT-TAU |
| PSS-I | ptime x group = .277, pgroup comparison = .748 | |||||
| Baseline | 25.4 (9.7) | 27.5 (9.8) | 28.9 (9.4) | |||
| Post-treatment | 22.9 (12.4) | 24.3 (11.9) | 26.1 (10.3) | −0.15 (−0.45, 0.16) | −0.08 (−0.41, 0.24) | −0.06 (−0.37, 0.25) |
| Three-month follow-up | 22.1 (12.2) | 23.7 (11.5) | 24.5 (11.8) | −0.06 (−0.38, 0.25) | −0.11 (−0.44, 0.23) | 0.05 (−0.26, 0.35) |
| Six-month follow-up | 22.1 (11.5) | 20.7 (11.0) | 24.3 (11.4) | −0.04 (−0.35, 0.27) | 0.20 (−0.13, 0.53) | −0.24 (−0.55, 0.07) |
| PDS | ptime x group = .441, pgroup comparison = .153 | |||||
| Baseline | 25.7 (11.2) | 27.6 (10.0) | 27.7 (10.2) | |||
| Post-treatment | 20.8 (12.0) | 23.0 (11.2) | 24.0 (10.7) | −0.21 (−0.51, 0.10) | −0.13 (−0.46, 0.19) | −0.07 (−0.38, 0.24) |
| Three-month follow-up | 20.9 (13.8) | 22.5 (11.5) | 24.3 (12.5) | −0.23 (−0.54, 0.08) | −0.05 (−0.38, 0.28) | −0.18 (−0.49, 0.12) |
| Six-month follow-up | 19.4 (11.9) | 19.9 (11.7) | 23.7 (12.5) | −0.27 (−0.58, 0.04) | 0.08 (−0.25, 0.41) | −0.35* (−0.66, −0.04) |
| Drug and alcohol free days | ptime x group = .249, pgroup comparison = .019 | |||||
| Baseline | 16.6 (12.1) | 15.6 (11.9) | 15.6 (12.3) | |||
| Post-treatment | 18.3 (11.9) | 19.4 (11.7) | 16.3 (12.4) | 0.13 (−0.17, 0.44) | −0.06 (−0.38, 0.27) | 0.19 (−0.12, 0.50) |
| Three-month follow-up | 19.5 (11.6) | 21.1 (10.2) | 17.6 (11.9) | 0.14 (−0.17, 0.46) | −0.17 (−0.50, 0.17) | 0.31* (0.00, 0.62) |
| Six-month follow-up | 20.5 (11.3) | 22.4 (10.7) | 16.4 (12.7) | 0.30 (−0.01, 0.61) | −0.27 (−0.59, 0.06) | 0.57*** (0.25, 0.88) |
| ASI alcohol severity | ptime x group = .163, pgroup comparison = .018 | |||||
| Baseline | 0.28 (0.25) | 0.33 (0.29) | 0.32 (0.27) | |||
| Post-treatment | 0.22 (0.24) | 0.25 (0.24) | 0.30 (0.28) | −0.32* (−0.63, −0.01) | 0.01 (−0.32, 0.34) | −0.33* (−0.64, −0.02) |
| Three-month follow-up | 0.20 (0.23) | 0.25 (0.26) | 0.28 (0.28) | −0.27 (−0.58, 0.05) | −0.03 (−0.36, 0.31) | −0.24 (−0.55, 0.07) |
| Six-month follow-up | 0.24 (0.26) | 0.19 (0.22) | 0.27 (0.28) | −0.12 (−0.43, 0.19) | 0.37* (0.04, 0.70) | −0.49** (−0.80, −0.18) |
| ASI drug severity | ptime x group = .703, pgroup comparison = .479 | |||||
| Baseline | 0.09 (0.11) | 0.10 (0.14) | 0.09 (0.11) | |||
| Post-treatment | 0.07 (0.12) | 0.06 (0.11) | 0.08 (0.11) | −0.05 (−0.36, 0.25) | 0.08 (−0.25, 0.41) | −0.13 (−0.44, 0.18) |
| Three-month follow-up | 0.06 (0.11) | 0.06 (0.12) | 0.06 (0.10) | 0.11 (−0.20, 0.42) | 0.18 (−0.15, 0.52) | −0.07 (−0.38, 0.23) |
| Six-month follow-up | 0.05 (0.10) | 0.04 (0.10) | 0.07 (0.11) | −0.07 (−0.38, 0.24) | 0.16 (−0.17, 0.49) | −0.24 (−0.55, 0.08) |
| BDI-II | ptime x group = .748, pgroup comparison = .018 | |||||
| Baseline | 25.3 (13.2) | 29.4 (11.7) | 28.6 (10.9) | |||
| Post-treatment | 19.0 (12.4) | 26.2 (12.0) | 25.8 (12.6) | −0.42** (−0.72, −0.11) | −0.33 (−0.66, 0.00) | −0.09 (−0.39, 0.22) |
| Three-month follow-up | 19.9 (14.4) | 25.0 (14.0) | 25.2 (13.0) | −0.37* (−0.68, −0.05) | −0.28 (−0.62, 0.05) | −0.08 (−0.39, 0.22) |
| Six-month follow-up | 18.5 (12.5) | 22.3 (13.3) | 24.1 (14.0) | −0.34* (−0.65, −0.03) | −0.12 (−0.45, 0.21) | −0.22 (−0.52, 0.09) |
| DERS | ptime x group = .966, pgroup comparison = .018 | |||||
| Baseline | 100.5 (26.9) | 110.7 (24.6) | 111.9 (25.3) | |||
| Post-treatment | 95.6 (24.7) | 102.9 (26.4) | 109.1 (24.5) | −0.36* (−0.67, −0.05) | −0.14 (−0.47, 0.19) | −0.22 (−0.52, 0.09) |
| Three-month follow-up | 94.1 (27.2) | 100.9 (27.8) | 106.8 (26.1) | −0.33* (−0.64, −0.01) | −0.07 (−0.40, 0.26) | −0.26 (−0.56, 0.05) |
| Six-month follow-up | 92.7 (24.7) | 100.0 (25.2) | 107.3 (25.4) | −0.41* (−0.71, −0.10) | −0.10 (−0.43, 0.22) | −0.30 (−0.61, 0.01) |
SeSa = Seeking Safety, RPT = Relapse Prevention Training, TAU = treatment as usual, CI = Confidence Interval, PSS-I = PTSD Symptom Scale Interview (Foa et al., 1993), PDS = Posttraumatic Diagnostic Scale (Foa et al., 1997), ASI = Addiction Severity Index-lite (Kokkevi & Hartgers, 1995; McLellan et al., 1992), BDI-II = Beck Depression Inventory II (Beck et al., 1996), DERS = Difficulties in Emotion Regulation Scale (Gratz & Roemer, 2004).
3.4. Secondary outcome analyses
3.4.1. Substance use frequency and severity
There were no significant time by group interaction effects on any of the substance use outcomes. The model showed a significant group effect on the number of days without substance use (p = .019). No significant main effect of time (p = .154) on number of days without substance use was observed. Contrasts revealed that, adjusting for baseline level, participants in RPT had significantly more substance-free days than participants in the TAU group (RPT – TAU = 3.53, 95% CI 1.08 to 5.98, p = .005), with a small effect size (see Table 2). Differences between Seeking Safety and TAU and between Seeking Safety and RPT were not significant (SeSa – TAU = 1.91, 95% CI −0.54 to 4.36, p = .126; SeSa – RPT = −1.62, 95% CI −4.22 to 0.98, p = .223; see Figure 2). ASI-lite alcohol use severity scores also were significantly impacted by group (p = .018), but not by time (p = .263). Contrasts showed that RPT demonstrated significantly lower baseline-adjusted alcohol severity scores than TAU, and there also was a trend towards lower scores in Seeking Safety than in TAU (RPT – TAU = −0.07, 95% CI −0.12 to −0.02, p = .005; SeSa – TAU = −0.05, 95% CI −0.10 to 0.002, p = .062), with both exhibiting small effect sizes. There was no significant difference between the active treatments (SeSa – RPT = 0.02, 95% CI −0.03 to 0.08, p = .387). Regarding ASI-lite drug use severity scores, there were no significant effects of time (p = .241) or group (p = .479).
Figure 2.
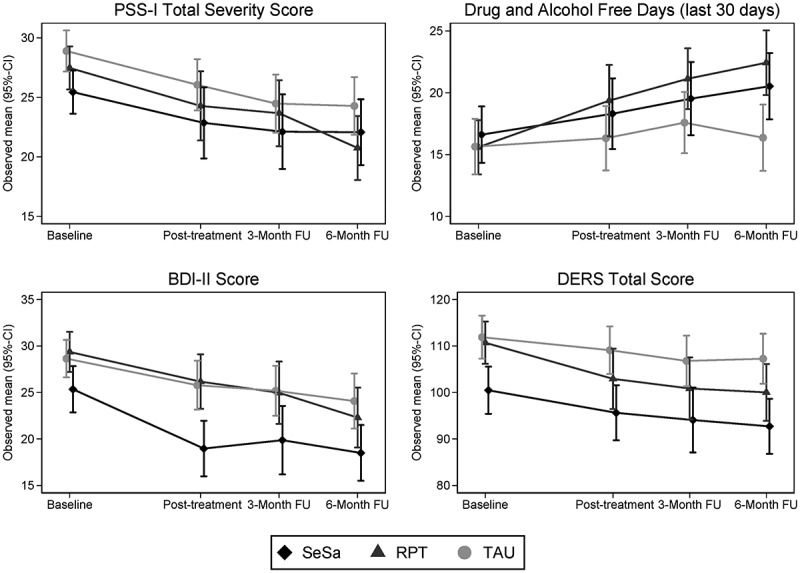
Observed courses of PSS-I PTSD severity scores (upper left), numbers of drug- and alcohol-free days (upper right), BDI-II depression scores (lower left) and DERS emotion dysregulation scores (lower right). PSS-I = PTSD Symptom Scale Interview (Foa et al., 1993), BDI-II = Beck Depression Inventory II (Beck et al., 1996), DERS = Difficulties in Emotion Regulation Scale (Gratz & Roemer, 2004), SeSa = Seeking Safety, RPT = Relapse Prevention Training, TAU = treatment as usual.
3.4.2. Depression and emotion dysregulation
Neither the BDI-II scores nor the DERS scores were significantly impacted by an interactive effect of time by group. There were significant main effects of time (p = .005) and group (p = .018) on BDI-II scores. Contrasts revealed that improvements in depressive symptoms were significantly greater in Seeking Safety as compared to TAU (SeSa – TAU = −4.10, 95% CI −6.91 to −1.29, p = .004) and, at a trend level, greater than in RPT (SeSa – RPT = −2.68, 95% CI −5.67 to 0.31, p = .079). RPT and TAU did not differ significantly on BDI-II scores (RPT – TAU = −1.42, 95% CI −4.21 to 1.38, p = .321; see Figure 2 for observed courses). DERS emotion dysregulation scores were significantly predicted by time (p = .040), with decreasing scores over time, and group (p = .018). Contrasts showed that the Seeking Safety group demonstrated significantly lower baseline-adjusted DERS scores than the TAU group (SeSa – TAU = −6.86, 95% CI −11.80 to −1.91, p = .007). There was a trend towards lower DERS scores in RPT than in TAU, and there was no significant difference between SeSa and RPT (RPT – TAU = −4.86, 95% CI −9.73 to 0.01, p = .050; SeSa – RPT = −2.00, 95% CI −7.21 to 3.22, p = .453; see Figure 2). All significant group differences in BDI-II and DERS scores had small effect sizes (see Table 2).
3.5. Ancillary analyses
3.5.1. Adjustment for additional treatment
In the three study conditions, a significant proportion of participants reported additional service use (at least one session or day in treatment). From baseline to post-treatment, this included outpatient psychotherapy (SeSa 53.6%, RPT 62.7%, TAU 47.8%), other outpatient treatment (SeSa 50.7%, RPT 58.2%, TAU 56.7%) and day-clinic or inpatient treatment (SeSa 10.1%, RPT 20.9%, TAU 18.9%). Between end of treatment and the three-months follow-up these rates were 44.3% (SeSa), 58.0% (RPT) and 48.9% (TAU) for outpatient psychotherapy, 57.4% (SeSa), 65.2% (RPT) and 55.4% (TAU) for other outpatient treatment and 24.6% (SeSa), 15.9% (RPT) and 17.4% (TAU) for day-clinic or inpatient treatment. Finally, between the three-month follow-up and the six-month follow-up, participants also reported use of outpatient psychotherapy (SeSa 48.6%, RPT 61.8%, TAU 52.3%), other outpatient treatment (SeSa 38.6%, RPT 55.9%, TAU 61.4%) and day-clinic or inpatient treatment (SeSa 14.3%, RPT 20.6%, TAU 20.5%). No significant differences were observed between the three study conditions, with the exception of the proportion of participants using other outpatient treatment (e.g. psychiatric treatment, self-help groups or occupational therapy) between the two follow-ups (p = .014).
The statistical models used to test the primary and secondary hypotheses were rerun adjusting for additional treatment during the intervention and follow-up phases (trauma psychotherapy, outpatient psychotherapy, other outpatient psychosocial treatment, day-clinic or inpatient treatment). The results of these analyses were consistent with those of the unadjusted analyses reported above, except for minor differences on the level of contrasts of time effects. For PDS and BDI-II scores, while the main effect of time remained (p = .006 and p = .004, respectively), the symptom reduction from three- to six-months follow-up was no longer significant. For DERS scores, there was a significant difference between post-treatment and three-months follow-up (p = .035) that was not observed in the unadjusted ITT analysis.
3.5.2. Minimum-dose analyses
Further analyses were undertaken using the sample of n = 191 participants attending at least eight of 14 group sessions or belonging to the TAU condition. Different results were seen on PTSD severity, emotion dysregulation, alcohol use severity and depression. Specifically, there was a trend towards a significant group effect on both interviewer-rated (p = .070) and self-rated PTSD severity (p = .069), with participants in Seeking Safety tending to show lower levels of baseline-adjusted PTSD severity scores than participants in the TAU group. Although there was still a global main effect of time (p = .044), the reduction in PDS scores from three- to six-months follow-up was no longer significant. Regarding DERS emotion dysregulation, the significant time effect observed in the ITT analysis disappeared (p = .203), but the group effect remained (p < .001), with both Seeking Safety and RPT showing greater reductions on the DERS than TAU. On ASI-lite alcohol use severity scores, not only RPT but also Seeking Safety showed greater decreases than TAU. Finally, the difference between post-treatment and three-months follow-up BDI-II scores was significant but there was no longer a significant difference between these scores at three- and six-months follow-up.
3.6. Severe adverse events
In 2929 person months (i.e. one month of one person’s trial participation) a total of 122 severe adverse events (SAEs) were registered (incidence rate [IR] = 4.17 SAEs/100 person months). There were no significant differences in the incidence of SAEs between the three intervention groups (IRRSeSa vs. TAU = 0.84, 95% CI 0.55 to 1.30; IRRSeSa vs. RPT = 0.85, 95% CI 0.54 to 1.34; IRRRPT vs. TAU = 0.99, 95% CI 0.66 to 1.49). The most frequent SAEs were increases in suicidality (n = 77, 63.1%), followed by events that led to unplanned hospital admissions (n = 23, 18.9%), life-threatening events (n = 14, 11.5%, e.g. car accident, suicide attempts, medical conditions), events that necessitated an intervention to prevent persistent damage or impairment (n = 7, 5.7%, e.g. injuries caused by a physical assault, medical conditions, substance overdose) and one event (0.8%) that led to a significant disability (a case of paralysis due to a physical condition). One participant (RPT group) died from a substance overdose during the follow-up phase. A relation of study participation to the SAEs was rated as probable in three cases (mainly cases of increases in suicidal thoughts) and as definite in one case (psychological decompensation and alcohol relapses that necessitated inpatient treatment after an assessment interview).
4. Discussion
Although research and clinical practice have demonstrated that individuals with co-occurring PTSD and SUD are a clinically important population, evidence-based treatments for this comorbidity are widely lacking in routine care in Europe. This is the first RCT investigating the efficacy of Seeking Safety, an integrated model for PTSD and SUD, compared to Relapse Prevention Training and a TAU control conducted in a European country.
Results for the ITT analysis showed similar decreases in PTSD severity among the three conditions. On secondary outcomes, there were diverse effects. Congruent with our secondary hypothesis, Seeking Safety plus TAU showed superior efficacy to TAU alone and equal efficacy to RPT plus TAU on depression and emotion regulation. RPT plus TAU was more effective than TAU alone and as effective as Seeking Safety plus TAU on number of substance-free days and alcohol severity, but not drug severity. At a trend level, Seeking Safety plus TAU was more effective on alcohol severity than TAU alone and superior to RPT plus TAU on depression, and RPT plus TAU was more effective than TAU alone on emotion regulation. All of the observed group effect sizes were in the small range.
On the minimum-dose analysis we found additional treatment effects. Those who met the minimum dose of Seeking Safety in addition to TAU tended to obtain greater PTSD improvement than the TAU alone condition, on both interviewer- and self-rated measures. In addition, those in Seeking Safety plus TAU who met the minimum dose showed significantly greater reduction in alcohol use than those in TAU alone. For RPT plus TAU, those who met the minimum dose improved significantly more than those in TAU alone on emotion dysregulation. Adjusting for additional treatment did not impact the main effect patterns of the unadjusted ITT analyses.
The lack of treatment effects of Seeking Safety plus TAU and RPT plus TAU on PTSD severity compared to TAU alone in the ITT sample contrasts with the literature broadly. For example, in Hien et al. (2004) both Seeking Safety plus TAU and RPT plus TAU outperformed a TAU control on PTSD. In the meta-analysis by Lenz et al. (2016), Seeking Safety outperformed waitlist and no-treatment controls, that included standard care conditions in some studies, with a homogenous medium-sized mean effect on PTSD severity. In general, Seeking Safety has evidenced reductions in PTSD in RCTs, beyond what would be expected by a waitlist or routine care (e.g. Hien et al., 2015; Najavits, Krinsley, Waring, Gallagher, & Skidmore, 2018). We can suggest several possibilities for why Seeking Safety plus TAU did not outperform TAU on PTSD in our trial. First, we offered fewer sessions than some of the studies meta-analysed in Lenz et al. (2016). Notably, there was a trend towards superiority of Seeking Safety plus TAU above TAU alone among those participants receiving at least eight sessions in our study, which suggests that dose matters. In our study, treatment was also delivered in group modality, whereas some of the studies in Lenz et al. were individual modality. In general, research shows that it is easier to achieve stronger reductions in PTSD in individual rather than group modality (e.g. Resick et al., 2017). Another possibility is that in most previous trials the participants suffered from severe PTSD at baseline (Hien et al., 2004, 2009; Lynch et al., 2012) whereas ours had only a moderately severe sample. Improvements in symptom severity and treatment effects might be more likely in more impaired samples (Hien, Campbell, Ruglass, Hu, & Killeen, 2010; Morrissey et al., 2005). Lastly, Seeking Safety and RPT were offered in addition to usual treatment. Although the effects on symptom outcomes did not change when the use of additional treatment was controlled for, the relatively high level of standard care might have limited the possible effects of the study interventions.
Our finding that Seeking Safety plus TAU and RPT plus TAU led to similar reductions in PTSD severity is congruent with the literature indicating that no or only small significant differences exist between active treatments in the PTSD, SUD and PTSD/SUD fields (e.g. Hoge & Chard, 2018; Imel et al., 2008; Simpson et al., 2017). With regard to PTSD/SUD treatment in particular, several RCTs using trauma-focused therapies have found no significant difference on PTSD or SUD at end of treatment compared to active controls such as supportive therapy (Foa et al., 2013; Sannibale et al., 2013) and RPT (Ruglass et al., 2017).
With respect to substance use outcomes, RPT plus TAU led to significantly more improvement than TAU alone in substance use frequency and alcohol use severity. Seeking Safety plus TAU was superior to TAU alone on alcohol severity at a trend level in the ITT sample and was significantly more effective than TAU alone among participants attending at least eight group sessions. In line with previous studies comparing Seeking Safety with alternative treatments, there was no significant difference between the two active treatments in substance use outcomes (Lenz et al., 2016). Thus, while both treatments showed effects on substance use outcomes as compared to TAU, this was not the case for PTSD outcomes. A potential explanation could be that study therapists were experienced in SUD treatment but not necessarily in PTSD treatment. It is therefore possible that they were more effective in the delivery of substance use-related interventions than PTSD-related interventions. Beyond the core issues of PTSD and SUD, reducing symptoms such as emotion dysregulation and depression is an important treatment goal and, in our study, Seeking Safety outperformed TAU on these variables. Thus, our findings suggest that when providing a relatively low dose of either treatment, RPT is beneficial for improving substance use in patients with SUD and PTSD, whereas Seeking Safety is beneficial for improving other trauma-associated psychopathology like depression or emotion dysregulation.
When interpreting our results, it also seems to be important to take into account the conditions of different service systems. Our trial evaluated Seeking Safety under the circumstances of the German health care system, while previous studies were predominantly conducted in the USA. Basic mental health care of individuals with SUD or PTSD might be different between countries, which makes direct comparisons difficult.
In addition to treatment efficacy, treatment safety is an important parameter for the evaluation of new treatments. The analysis of SAEs in our trial showed no difference regarding the incidence rates of SAEs between the three conditions. Hence, Seeking Safety and RPT did not lead to more harmful events than TAU. Consistent with previous reports on safety outcomes of the programme (Killeen et al., 2008), this indicates that Seeking Safety can be considered a safe treatment for the vulnerable group of women with SUD and PTSD.
Ultimately, there are many other treatment model variables that are important to consider beyond the ‘horse-race’ comparisons of active treatments. For example, dropout is a long-standing concern with trauma-focused models, as is low adoption by therapists. Understanding what models appeal to which patients, therapists and treatment programmes, and what is feasible for these stakeholders, will be a key part of the next generation of treatment research. Having a variety of options from which to choose, assuming equal efficacy, allows for greater empowerment to meet the diverse needs of individuals with PTSD/SUD. Both Seeking Safety and RPT also have the advantage that they are low-threshold, allowing in patients with active substance use and other vulnerabilities. Moreover, they are easy to disseminate. For example, with Seeking Safety, no specific degree or level of experience of providers is required for routine clinical implementation (Najavits et al., 2014).
4.1. Limitations
This is one of the largest trials on the efficacy of Seeking Safety so far. The strengths of our study include its prospective, three-armed, randomized design with parallel treatments, sufficient statistical power, repeated outcome measurement with blinded raters, and recruitment strategies that resulted in a sample with various types and severity of trauma and SUD. However, some limitations of our study have to be acknowledged. First, we only included women because of the higher prevalence of co-occurring PTSD in female patients with SUD. Therefore, our findings cannot be generalized to men with PTSD and SUD. Although participants were randomly assigned to the three groups, there were baseline differences in rates of some traumatic experiences. However, we compensated by using baseline-adjusted statistical models for all treatment outcomes. Moreover, as previously discussed, we applied a partial dose of Seeking Safety in outpatient group modality. Variations of these parameters might yield different results. Furthermore, participants in the active treatment conditions were able to engage in or continue other treatment for psychological problems or substance use (treatment as usual). While this limits the internal validity of this study as conclusions with regard to the effects of Seeking Safety only or Relapse Prevention Training only cannot be drawn, it increases its ecological validity, as patients with PTSD and SUD in real life settings also tend to engage in more than just one weekly group contact. Furthermore, when the use of additional treatment was controlled for, the pattern of treatment effects remained unchanged. We also analysed only psychopathology outcomes and did not address broader variables that would be relevant to public health and to Seeking Safety in particular such as changes in coping skills, social and work functioning, and cognitions. Due to the study being conducted with German therapists, these did not go through a formal certification in conducting Seeking Safety by the developer of the programme. However, treatment adherence was evaluated by a rater trained by the group of the developer.
5. Conclusion
Women with co-occurring PTSD and SUD are a highly vulnerable and underserved population. In this study, relatively few sessions of Seeking Safety and Relapse Prevention Training in addition to TAU showed effects that were superior to a TAU alone condition. While none of the active interventions was more effective than TAU alone in improving PTSD severity in the ITT sample, Seeking Safety outperformed TAU alone on decreasing depression and emotion regulation difficulties and RPT outperformed TAU alone on substance use outcomes. Additional analyses suggested more effects of Seeking Safety and RPT in those participants who attended a minimum treatment dose. Our results for Seeking Safety plus TAU in comparison to TAU alone were divergent from prior literature on Seeking Safety conducted in the USA, which found that Seeking Safety outperformed waitlist or standard care conditions. This may reflect cultural or other differences between the healthcare systems in the two countries, or methodology differences between our trial and those in the USA. Future studies should investigate variables in addition to outcomes per se, such as what aspects of each treatment appeal to particular patients and therapists and how best to disseminate them.
Acknowledgments
The authors thank all participants and the staff of all study centres, in particular R. Hiersemann, M. Bamberg, H. Dirks, A. Dotten, L. Dreetz, M. Huppertz, J. Reeder and B. Röllenbleck for their contributions. The authors also wish to thank K. Wegscheider, M. Bullinger and C. Muhtz for their participation in the independent data and safety monitoring committee (DSMC), S. Barnow, M. Härter, M. Klein, M. Mülhan, U. Ravens-Sieberer, R. Thomasius and S. Pawils as further members of the CANSAS-Study Group, and P. Resick, M. Cloitre and E. Foa for their participation in the advisory board.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- Beck A. T., Steer R. A., & Brown G. K. (1996). BDI-II, beck depression inventory: Manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bernstein D. P., & Fink L. (1998). Childhood trauma questionnaire: A retrospective self-report. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Boden M. T., Kimerling R., Jacobs-Lentz J., Bowman D., Weaver C., Carney D., … Trafton J. A. (2012). Seeking Safety treatment for male veterans with a substance use disorder and post-traumatic stress disorder symptomatology. Addiction, 107(3), 578–15. [DOI] [PubMed] [Google Scholar]
- Clark H. W., Masson C. L., Delucchi K. L., Hall S. M., & Sees K. L. (2001). Violent traumatic events and drug abuse severity. Journal of Substance Abuse Treatment, 20(2), 121–127. [DOI] [PubMed] [Google Scholar]
- Courtois C. A., Sonis J., Brown L. S., Cook J., Fairbank J. A., Friedman M., … Schulz P. (2017). Clinical practice guidelines for the treatment of posttraumatic stress disorder (PTSD) in adults. Washington, DC: American Psychological Association. [Google Scholar]
- Desai R. A., Harpaz-Rotem I., Najavits L. M., & Rosenheck R. A. (2008). Impact of the Seeking Safety program on clinical outcomes among homeless female veterans with psychiatric disorders. Psychiatric Services, 59(9), 996–1003. [DOI] [PubMed] [Google Scholar]
- Dong Y., & Peng C. Y. (2013). Principled missing data methods for researchers. Springerplus, 2(1), 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragan M., & Lis-Turlejska M. (2007). Prevalence of posttraumatic stress disorder in alcohol dependent patients in Poland. Addictive Behaviors, 32(5), 902–911. [DOI] [PubMed] [Google Scholar]
- Driessen M., Schulte S., Luedecke C., Schaefer I., Sutmann F., Ohlmeier M., … Havemann-Reinicke U. (2008). Trauma and PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism, Clinical and Experimental Research, 32(3), 481–488. [DOI] [PubMed] [Google Scholar]
- Evren C., Sar V., Dalbudak E., Cetin R., Durkaya M., Evren B., & Celik S. (2011). Lifetime PTSD and quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation. Psychiatry Research, 186(1), 85–90. [DOI] [PubMed] [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., & Williams J. B. W. (1997). Structured Clinical Interview for DSM-IV Axis I disorders (SCID I). New York, NY: Biometric Research Department. [Google Scholar]
- Foa E. B., Cashman L., Jaycox L., & Perry K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychological Assessment, 9(4), 445–451. [Google Scholar]
- Foa E. B., Riggs D. S., Dancu C. V., & Rothbaum B. O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6(4), 459–473. [Google Scholar]
- Foa E. B., Yusko D. A., McLean C. P., Suvak M. K., Bux D. A. Jr., Oslin D., … Volpicelli J. (2013). Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. JAMA, 310(5), 488–495. [DOI] [PubMed] [Google Scholar]
- Gielen N., Havermans R. C., Tekelenburg M., & Jansen A. (2012). Prevalence of post-traumatic stress disorder among patients with substance use disorder: It is higher than clinicians think it is. European Journal of Psychotraumatology, 3. doi: 10.3402/ejpt.v3i0.17734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K. L., & Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Greenfield S. F., Brooks A. J., Gordon S. M., Green C. A., Kropp F., McHugh R., … Miele G. M. (2007). Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence, 86(1), 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hautzinger M., Keller F., & Kühner C. (2006). Beck Depression Inventar II (BDI 2). Frankfurt: Harcourt Test Service. [Google Scholar]
- Hien D. A., Campbell A. N., Ruglass L. M., Hu M. C., & Killeen T. (2010). The role of alcohol misuse in PTSD outcomes for women in community treatment: A secondary analysis of NIDA’s women and trauma study. Drug and Alcohol Dependence, 111(1–2), 114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D. A., Cohen L. R., & Campbell A. N. (2005). Is traumatic stress a vulnerability factor for women with substance use disorders? Clinical Psychology Review, 25(6), 813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D. A., Cohen L. R., Miele G. M., Litt L. C., & Capstick C. (2004). Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry, 161(8), 1426–1432. [DOI] [PubMed] [Google Scholar]
- Hien D. A., Levin F. R., Ruglass L. M., Lopez-Castro T., Papini S., Hu M. C., … Herron A. (2015). Combining Seeking Safety with sertraline for PTSD and alcohol use disorders: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 83(2), 359–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D. A., Wells E. A., Jiang H., Suarez-Morales L., Campbell A. N., Cohen L. R., … Nunes E. V. (2009). Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology, 77(4), 607–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrand A., Behrendt S., & Hoyer J. (2015). Treatment outcome in substance use disorder patients with and without comorbid posttraumatic stress disorder: A systematic review. Psychotherapy Research: Journal of the Society for Psychotherapy Research, 25(5), 565–582. [DOI] [PubMed] [Google Scholar]
- Hoge C. W., & Chard K. M. (2018). A window into the evolution of trauma-focused psychotherapies for posttraumatic stress disorder. JAMA, 319(4), 343–345. [DOI] [PubMed] [Google Scholar]
- Huang M. C., Schwandt M. L., Ramchandani V. A., George D. T., & Heilig M. (2012). Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcoholism, Clinical and Experimental Research, 36(6), 1099–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp (2013). IBM SPSS statistics for windows (Version 22.0). Armonk, NY: IBM Corp. [Google Scholar]
- Imel Z. E., Wampold B. E., Miller S. D., & Fleming R. R. (2008). Distinctions without a difference: Direct comparisons of psychotherapies for alcohol use disorders. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 22(4), 533–543. [DOI] [PubMed] [Google Scholar]
- Jacobsen L. K., Southwick S. M., & Kosten T. R. (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. The American Journal of Psychiatry, 158(8), 1184–1190. [DOI] [PubMed] [Google Scholar]
- Johnson S. D., Striley C., & Cottler L. B. (2006). The association of substance use disorders with trauma exposure and PTSD among African American drug users. Addictive Behaviors, 31(11), 2063–2073. [DOI] [PubMed] [Google Scholar]
- Kaiser D., Grundmann J., Schulze C., Stubenvoll M., Kosar M., Junker M., … Schafer I. (2015). A pilot study of Seeking Safety in a sample of German women outpatients with substance dependence and posttraumatic stress disorder. Journal of Psychoactive Drugs, 47(5), 401–408. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Cloitre M., Maercker A., Kazlauskas E., Shevlin M., Hyland P., … Brewin C. R. (2017). PTSD and Complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeen T., Hien D., Campbell A., Brown C., Hansen C., Jiang H., … Nunes E. (2008). Adverse events in an integrated trauma-focused intervention for women in community substance abuse treatment. Journal of Substance Abuse Treatment, 35(3), 304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleber H. D., Weiss R. D., Anton R. F., George T. P., Greenfield S. F., & Kosten T. R. Steering Committee on Practice Guidelines (2007). Treatment of patients with substance use disorders, second edition. American Psychiatric Association. The American Journal of Psychiatry, 164(Supp. 4), 5–123. [PubMed] [Google Scholar]
- Kokkevi A., & Hartgers C. (1995). EuropASI: European adaptation of a multidimensional assessment instrument for drug and alcohol dependence. European Addiction Research, 1(4), 208–210. [Google Scholar]
- Körkel J., & Schindler C. (2003). Relapse prevention with alcohol addicts - the structured training program S.T.A.R. (1st ed.). Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Langeland W., Draijer N., & van Den Brink W. (2004). Psychiatric comorbidity in treatment-seeking alcoholics: The role of childhood trauma and perceived parental dysfunction. Alcoholism, Clinical and Experimental Research, 28(3), 441–447. [DOI] [PubMed] [Google Scholar]
- Lenz A. S., Henesy R., & Callender K. (2016). Effectiveness of Seeking Safety for co-occurring posttraumatic stress disorder and substance use. Journal of Counseling & Development, 94(1), 51–61. [Google Scholar]
- Lynch S. M., Heath N. M., Mathews K. C., & Cepeda G. J. (2012). Seeking Safety: An intervention for trauma-exposed incarcerated women? Journal of Trauma & Dissociation : the Official Journal of the International Society for the Study of Dissociation (ISSD), 13(1), 88–101. [DOI] [PubMed] [Google Scholar]
- Magruder K. M., McLaughlin K. A., & Elmore Borbon D. L. (2017). Trauma is a public health issue. European Journal of Psychotraumatology, 8(1), 1375338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan A. T., Kushner H., Metzger D., Peters R., Smith I., Grissom G., … Argeriou M. (1992). The fifth edition of the addiction severity index. Journal of Substance Abuse Treatment, 9(3), 199–213. [DOI] [PubMed] [Google Scholar]
- Mills K. L., Lynskey M., Teesson M., Ross J., & Darke S. (2005). Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): Prevalence and correlates. Drug and Alcohol Dependence, 77(3), 243–249. [DOI] [PubMed] [Google Scholar]
- Morrissey J. P., Jackson E. W., Ellis A. R., Amaro H., Brown V. B., & Najavits L. M. (2005). Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatric Services, 56(10), 1213–1222. [DOI] [PubMed] [Google Scholar]
- Najavits L. M. (2002). Seeking Safety: A treatment manual for PTSD and substance abuse. New York, NY: Guilford Press. [Google Scholar]
- Najavits L. M., Gallop R. J., & Weiss R. D. (2006). Seeking Safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. The Journal of Behavioral Health Services & Research, 33(4), 453–463. [DOI] [PubMed] [Google Scholar]
- Najavits L. M., Hamilton N., Miller N., Griffin J., Welsh T., & Vargo M. (2014). Peer-led Seeking Safety: Results of a pilot outcome study with relevance to public health. Journal of Psychoactive Drugs, 46(4), 295–302. [DOI] [PubMed] [Google Scholar]
- Najavits L. M., Harned M. S., Gallop R. J., Butler S. F., Barber J. P., Thase M. E., & Crits-Christoph P. (2007). Six-month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite national trial. Journal of Studies on Alcohol and Drugs, 68(3), 353–361. [DOI] [PubMed] [Google Scholar]
- Najavits L. M., Krinsley K., Waring M. E., Gallagher M. W., & Skidmore C. (2018). A randomized controlled trial for veterans with PTSD and substance use disorder: Creating change versus Seeking Safety. Substance Use & Misuse, 53(11), 1788–1800. [DOI] [PubMed] [Google Scholar]
- Najavits L. M., Schmitz M., Gotthardt S., & Weiss R. D. (2005). Seeking Safety plus exposure therapy: An outcome study on dual diagnosis men. Journal of Psychoactive Drugs, 37(4), 425–435. [DOI] [PubMed] [Google Scholar]
- Najavits L. M., Weiss R. D., Shaw S. R., & Muenz L. R. (1998). “Seeking Safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress, 11(3), 437–456. [DOI] [PubMed] [Google Scholar]
- Pietrzak R. H., Goldstein R. B., Southwick S. M., & Grant B. F. (2011). Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the USA: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Anxiety Disorders, 25(3), 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers M. B., Gillihan S. J., Rosenfield D., Jerud A. B., & Foa E. B. (2012). Reliability and validity of the PDS and PSS-I among participants with PTSD and alcohol dependence. Journal of Anxiety Disorders, 26(5), 617–623. [DOI] [PubMed] [Google Scholar]
- Resick P. A., Wachen J. S., Dondanville K. A., Pruiksma K. E., Yarvis J. S., Peterson A. L., … Young-McCaughan S. (2017). Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 74(1), 28–36. [DOI] [PubMed] [Google Scholar]
- Roberts N. P., Roberts P. A., Jones N., & Bisson J. I. (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. [DOI] [PubMed] [Google Scholar]
- Ruglass L. M., Lopez-Castro T., Papini S., Killeen T., Back S. E., & Hien D. A. (2017). Concurrent treatment with prolonged exposure for co-occurring full or subthreshold posttraumatic stress disorder and substance use disorders: A randomized clinical trial. Psychotherapy and Psychosomatics, 86(3), 150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sannibale C., Teesson M., Creamer M., Sitharthan T., Bryant R. A., Sutherland K., … Peek-O’Leary M. (2013). Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction, 108(8), 1397–1410. [DOI] [PubMed] [Google Scholar]
- Schäfer I., & Najavits L. M. (2007). Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse. Current Opinion in Psychiatry, 20(6), 614–618. [DOI] [PubMed] [Google Scholar]
- Schäfer I., Pawils S., Driessen M., Harter M., Hillemacher T., Klein M., … Barnow S. (2017). Understanding the role of childhood abuse and neglect as a cause and consequence of substance abuse: The German CANSAS network. European Journal of Psychotraumatology, 8(1), 1304114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer I., Schulze C., Dilling A., Barghaan D., Bullinger M., & Stubenvoll M. (2010). Acceptance of an integrative treatment for PTSD and substance abuse (“Seeking Safety”) among female patients with alcohol dependence. Suchttherapie, 11, 60–68. [Google Scholar]
- Sells J. R., Waters A. J., Schwandt M. L., Kwako L. E., Heilig M., George D. T., & Ramchandani V. A. (2016). Characterization of comorbid PTSD in treatment-seeking alcohol dependent inpatients: Severity and personality trait differences. Drug and Alcohol Dependence, 163, 242–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T. L., Lehavot K., & Petrakis I. L. (2017). No wrong doors: Findings from a critical review of behavioral randomized clinical trials for individuals with co-occurring alcohol/drug problems and posttraumatic stress disorder. Alcoholism, Clinical and Experimental Research, 41(4), 681–702. [DOI] [PubMed] [Google Scholar]
- Stata Corp (2015). Stata statistical software: Release 14. College Station, TX: Stata Corp. [Google Scholar]
- Zlotnick C., Franklin C. L., & Zimmerman M. (2002). Does “subthreshold” posttraumatic stress disorder have any clinical relevance? Comprehensive Psychiatry, 43(6), 413–419. [DOI] [PubMed] [Google Scholar]


