ABSTRACT
Background & Objective: Poor people, in general, get poor quality of health services. The situation is very much worsening for the poor who live in the remote areas in the coastal belt of Bangladesh as health care facilities and services are often less complete, farther away, and therefore most costly to reach than in urban hospitals and physician. Ensure of better health service for the poor, it is essential to examine the effectiveness of Universal Health Coverage (UHC). This study sets its objectives to evaluate the health service for the poor in the coastal area of Bangladesh and develop an approach of management strategy.
Methods: This study followed a two-stage cluster sampling technique and carried out a household survey through the open-ended questionnaire. In addition, the study applied the logistic regression model to generate empirically supported assessments.
Results: Result from the disparity rate ratio (DRR) revealed that there is a big health care disparity of different income groups like poor and rich. Furthermore, results from the model demonstrated that Medicaid, Medicare, Social Health Insurance, Telemedicine and Capitation under the provision Universal Health Coverage (UHC) are statistically significant compared to reduce the health care disparity.
Conclusion: UHC becomes a critical issue for improved and quality health care system for all the groups especially, the poor in coastal Bangladesh. This study showed that Medicaid, Medicare and Social Health Insurance and Capitation perform well to provide better health care facilities for all.
KEYWORDS: Disparity, Universal health coverage, health economics, logistic regression model, coastal Bangladesh
Introduction
A socio-economic (SE) gradient in health, whereby wealthier, more highly educated person’s experience better health than poorer, less educated persons, has been well documented across and within many countries [1–4]. Poor lifestyle habits such as smoking, poor diet, and physical inactivity are more prevalent in lower socioeconomic groups [5–9]. The propensity to use preventive health services, e.g., regular medical checkups or consult minor health problems with a physician is a rare practice in the lower socioeconomic group [10,11]. This situation gets more force when they have a lack of health care facilities and financial barriers. Under these circumstances, they do not get access to reliable health care service and affordable medicine. Generally, lower socioeconomic groups (poor people) live in the remote areas such as slum, hilly area, coastal region, isolated and riverside islands and khas land (the land in which the people have common rights and therefore cannot be leased out) as health care facilities and services are often less complete, further away and therefore, most costly to reach than in urban hospitals and physician [12].
It is well recognized that poor health is a common consequence of poverty and poverty can be a consequence of poor health and it is working as a vicious cycle [13–16]. The lives of the poor are very vulnerable to health risk and there exist high health cost relative to their income because they are frequently suffering from poverty1 related diseases causing a higher level of morbidity and mortality [14,17–20]. This situation is also common in coastal Bangladesh and the health and livelihood patterns of the coastal people, especially for the poor are frequently affected by climate change [21,22]. Extreme events like the cyclone, sea-level rise, storm surge, salinity and waterlogging are the most common natural hazards in the whole coastal Bangladesh. Poor people in this region are frequently suffering from climate-induced and poverty-related diseases [21].
Now it is the time to rethink about the health care facilities of the coastal people of Bangladesh because they are the integrated part of our development. Universal health coverage (UHC) plays an important role in this issue. It is not a destination, it is a direction [23,24]. Under the provision of UHC, it is possible to make health care facilities easier in urban and rural areas. It helps to raise sufficient funds for health, reduce heavy reliance on direct out-of-pocket (OOP) expenditure and reduce and eliminate the inefficient use of resources [25,26]. It works as a bridge between cost and health coverage and protects all people of all regions from financial hardship [27]. It provides access to quality essential health services; safe, effective and affordable essential medicines and vaccines; and protects all people from financial risk during the catastrophic period [28,29].
A few countries like America, Canada, UK, and Japan get fully or partially benefits when they introduce UHC for certain groups. Virtually all European Union countries and Australia also offer such benefits because of improved access to health care substantially reduce disparities in health care utilization [9]. In Canada, a 1991 review of research covering the first two decades of Medicare (a system concern co-pays and deductibles for the aged and certain disabled person) concluded that the introduction of Medicare had succeeded in providing a common entry point to the system by removing the basic barrier of out of pocket payment [30].
Based on the numerous benefits and demand of UHC, Bangladesh has recently introduced UHC under a pilot scheme named Shasthyo Shuroksha Karmasuchi (SSK) in Ghatail, Kalihati and Modhupur Upazilas (a local and smallest administrative unit of Bangladesh) of Tangail district. This scheme is currently working for better health care for poor people. The objectives of this scheme include: improving access of the poor to inpatient care, protect poor from catastrophic health care cost, increase hospital authority for functional improvement and introduce performance-based financing models. Bangladesh government has the vision to implement UHC for all within the year 2032.
People with a lower socioeconomic background take the comparatively more medicine and used more hospital services. On the other hand, specialist services were comparatively underused by people in lower socioeconomic groups [2,31,32]. This disparity is reduced when the health care sector is guided by the UHC. Shibuya et al. [33],pointed out that UHC increases equity between different population groups. The protection against the health care cost and improves equity of access to health care lies at the core of many health sector initiatives. Aging people, poor household, unemployed, children, and underprivileged community get benefits when they are under the umbrella of UHC [34]. Hosseinpoor et al. [35],asserted that health service coverage gap is common to all sub-Saharan African countries. UHC can play an important role to reduce health service coverage gap in these countries.
Accessing the potential health impact of poor people of the southwest coastal region of Bangladesh requires an understanding of the vulnerability of populations, their capacity to respond and adapt to cope with new conditions [36]. The UHC can be the leading and alternative measure rather than the existing and traditional health care system in the southwest coastal region of Bangladesh. Under the provision of UHC, the full spectrum of quality health services address quality and efficient health care service for all.
Most of the studies pointed out that UHC has a positive role to reduce disparities of health service for different socioeconomic groups in developed countries. But it is noticed that very few literatures have explained the role of UHC for the poor in the coastal region. The main objectives of the study include: measure health disparities for the poor and rich, detect the factors contributing to reduce health disparities and develop management strategy of health care facilities for the poor.
Materials and methods
Study area
Geographical and climatic characteristics have long been concerned with issues of human health, mortality, morbidity, the length of life, poverty and human well-being [37]. Due to the vulnerability to climate change, natural hazards, acute poverty and human health, southwest coastal region (Khulna, Satkhira and Bagerhat districts) of Bangladesh is considered as the study area of this study. This region is part of an active delta of large Himalayan Rivers. The people of this area frequently fight against the devastating storm surges, cyclones, salinity, waterlogging, and other natural hazards. As a result, poor people suffer a lot and their living conditions and well-being are degraded. There is discrimination in a health care facility in this region compared to those of other regions of Bangladesh. The index of the treatment facility and education, health care facility for infant, child, elderly and poor and eligibility of getting good health care service are in backward position. Isolation of geographical condition and lack of strong political commitment are also enhancing further a backwardness of the health sector of this region.
Research plan
Key informant interview (KII)
This study depends upon 17 KIIs for a better qualitative description of disparities of health service for the poor. KIIs were conducted during the period (25–30) August 2016 at the different locations of the southwest coastal region. Few selected questions were to fulfill the objective of KII. Medical practitioners or physicians, nurses, statistical officers and supporting staffs of different Civil Surgeon offices of the southwest coastal region of Bangladesh, district EPI superintend, the staff of different private and government hospitals and drug shops, and outdoor patients participated in the response to the KII. The most important findings of the KII include: low-income groups (poor people) have disparities of health service in the coastal area; they get less opportunity to discuss their health problem with specialist physicians; they stay more in the hospital when they are sick; they have more tendency to fall into casualty; annual medical checkups and diagnosis are rare practice for the coastal poor people, they prefer unscientific health-related coping methods (e.g., Herbal treatment, religious treatment, homeopathic, drug retailer and untrained village doctor) and seldom go to the hospital seldom because of their illiteracy.
Sampling technique, development of questionnaire and interview questions
We followed published guidelines for the surveys with ‘Two-stage’ and ‘Divisible’ clustering sampling techniques [38]. Under this technique of probability proportional to size (PPS) is used to select the cluster. In the study, households were the sample units and the sample frame was a set of coastal people. The sample size is calculated using the given formula at 0.05 (5 percentage) point margin of error:
| (1) |
Where, DFEE is the design effect, 1.96 is the Z value for 95% confidence limits and P estimated prevalence (e.g., 37 percent in this study).
Typical cluster sizes range from 20–40 and it is suggested that every cluster should have less than or equal to 100 [39]. The survey through questionnaire and interview included n=800 (265 from the low-income group, 288 from the middle-income group, and 247 from the high-income group) respondents in 22 clusters.
Based on the findings of KII, this study carried out a survey through questionnaire and interview questions conducted from 23 September 2016 to 25 April 2017 at different coastal villages in the southwest coastal region. A single page questionnaire and interview question sheet along with ethical consent form consist of monthly income, age, gender, educational attainment, disease pattern, level of treatment satisfaction, cost of health care service, family physician services in the last year, specialist physician service in the last year, days of stay in hospital in the last year, recovery status from disease, perception about Medicaid, Capitation, Telemedicine, Social Health Insurance and Medicare at different villages of Mongla, Rampal, Morrelgonj and Sharankhola upazilas of Bagerhat district; Batiyaghata, Damuria, Dakope, Koyra and Paikgachha upazilas of Khulna district and Shyamnagar upazila of Satkhira district. The questionnaire was prepared in the English language, but interviews were conducted by the local language, Bangla. The data were collected by the professional data collectors from the household level for measuring the disparities of health care service and impact assessment of UHC. The most important findings of the survey are given in the following figure.
Monthly income 5000 Taka2 is allocated for the lower income group in the study. The middle-income group holds the range from monthly income 5001Taka to 40,000 Taka and when the monthly income is more than 40,000 Taka, it is allocated for the higher-income group. Figure 1 provides an initial visualization of the distribution of health care services used by different income groups. Respondents’ having an annual income of less than 5000 Taka constituted 28% and get disproportionately health care services and facilities. 15% respondents from the high-income group stay more days in the general hospital for proper and better medical treatment. Similarly, 57% respondents from the middle-income group stay hospital on average 17 days and it is on average 13 days for the low-income group. Respondents from the low-income group (13%) go to the clinic and hospital for annual medical checkups. It is 37% for from the middle-income group and 50% from the high-income group. In addition, 17% respondents from the low- income group depend on specialist and family physician service for better health care which is less than the respondents from middle and the high-income groups.
Figure 1.
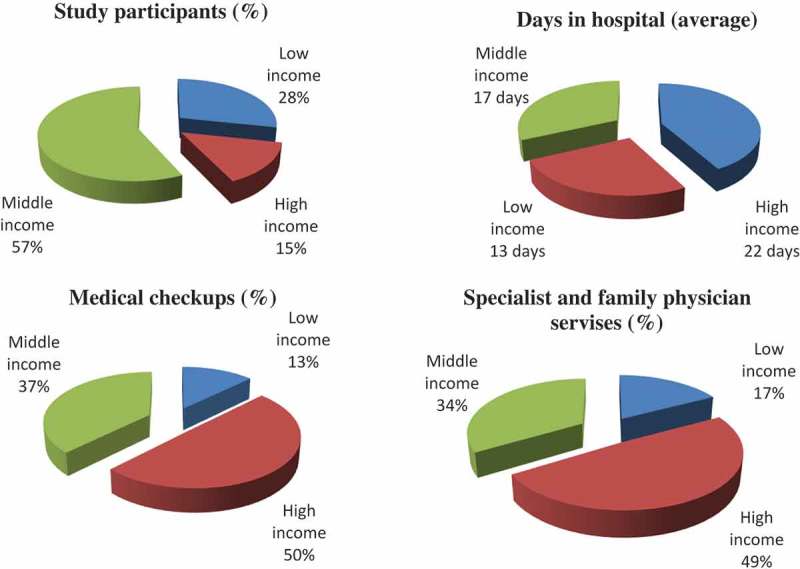
Distribution of annual health care services of the respondents.
Measure of disparity of health care service for different socio-economic groups
There are several ways to measure disparity or inequality of health care. The most common are slope index, relative index, health concentration index, the range and the population attributable fraction (PAF). Among all the measures, the range is the best measurement approach of disparities of health care because of its simplicity and wide acceptability. The range is a measure of disparity which compares the rate of a health variable between the advantaged group like rich people and the least advantaged group like poor people. Under this measure, the rich people are treated as the referent category.
The range can also be suitable for a relative measure of inequality, treated as the disparity rate ratio (DRR). The DRR can be explained as the relative disparity of health care between the rich and poor people. The calculation process of the absolute difference of health care disparity can be calculated using the following formula at a 95% confidence interval (CI):
| (2) |
Where represents the health outcome (recovery from diseases) for the poor people and refers to the health outcome for the rich people. Calculation of the 95% CI for the AD with the standard is calculated by the following:
| (3) |
Where and refer to the standard errors of the health outcome for the poor and rich people respectively. The health care disparity can be calculated using the following formula:
| (4) |
The standard error for the is calculated by
| (5) |
Where is the relative standard error of the difference measured by
| (6) |
Where and are the prevalence rates for the poor and rich people respectively. is essential to measure the relative standard error of the rich people which can be computed by
| (7) |
The 95% CI is calculated for both AD and DRR using the Equation (8)
Where is the point estimate of the range measurement. There is a rule of thumb that a large value of AD indicates a high level of disparity at 95% CI. Similarly, a large value of the DRR indicates a high level of disparity at 95% CI. There is a rule of thumb that the closer the value to 1 creates the larger disparity of health care service for the different socio-economic groups.
Model specification
This study proposed three health care coverage models for better comparison and assessment: one for the poor (low-income group) and the rest two of the middle-income and the high-income groups. The proposed health care model takes the following format at the convenient 0.01 percent, 0.05 percent and 0.10 levels of significance.
| (9) |
where HCC indicates the health care coverage and treated as the outcome variable. and are the coefficients associated with the attributes Capitation, Telemedicine, Medicaid, Social Health Insurance and Medicaid.
The study compared the characteristics and health outcomes of survey participants that were included in the analysis using Logistic regression model. It is suitable for a binary response. Many studies like Hamming, Henry, and Davis [40], Andreae et al. [41], Marafino et al. [42], Deb and Norton [43], Figueroa et al. [44], and Fishman, McLafferly, and Galanter [45], have successfully used logistic regression model to analyse health care disparities between different groups. Table 1 shows the proposed attributes and their hypothetical relation with the outcome variable. The disparity of health care service for different socio-economic groups is common in the southwest coastal area (see Table 2 for more details). To estimate the impacts of different determinants of health care coverage, three Logistic regression models were developed by using SPSS software version 20. Table 3 shows econometric results for three Logit models for low, middle and high-income groups.
Table 1.
Attributes and hypothesized relation.
| Attribute | Unit | Data type | Hypothesized relation |
|---|---|---|---|
| hcc: health care coverage | Number | Dummy (1.0) | |
| cap: Capitation | Number | Continuous | |
| tm: Telemedicine | Number | Dummy (1,0) | + |
| media: Medicaid | Number | Dummy (1,0) | + |
| shi: Social health insurance | Number | Continuous | |
| medca: Medicare | Number | Dummy (1,0) | + |
Table 2.
Disparity of health care service for different socio-economic groups.
| Group | Disparity rate ratio | P-value |
|---|---|---|
| Lowa-Middle income group | 0.8710** | 0.020 |
| Low-Highb income group | 0.9281* | 0.000 |
| Middle-High income group | 0.6163*** | 0.103 |
A low income group refers to poor people; b high income group refers to rich people
*Significant at 1% (0.01); **Significant at 5% (0.05); ***Significant at 10% (0.10).
Table 3.
Estimation of attributes associated with health care coverage.
| Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|
| (Low income group) |
(Middle income group) |
(High income group) |
||||
| Attribute | Coefficient | P-value | Coefficient | P-value | Coefficient | P-value |
| intercept | −0.013*** | 0.097 | −0.309** | 0.045 | −1.9781* | 0.000 |
| (0.511) | (0.457) | (0.783) | ||||
| cap | 0.526* | 0.009 | 0.133*** | 0.010 | 0.483** | 0.038 |
| (0.586) | (0.325) | (0.253) | ||||
| tm | 0.103 | 0.130 | −0.895** | 0.049 | 0.461 | 0.151 |
| (0.276) | (0.962) | (0.237) | ||||
| media | 0.156* | 0.000 | 0.101 | 0.160 | 0.460 | 0.155 |
| (0.980) | (0.937) | (0.240) | ||||
| shi | 0.170* | 0.001 | 0.075** | 0.051 | 0.077** | 0.033 |
| (0.048) | (0.259) | (0.241) | ||||
| medca | 0.631*** | 0.103 | 0.282 | 0.179 | 0.222 | 0.114 |
| (9.712) | (0.693) | (0.243) | ||||
| Log-likelihood | −598.712 | −194.590 | −197.683 | |||
| McFadden R2 | 0.339 | 0.311 | 0.293 | |||
| n | 265 | 288 | 247 | |||
Standard errors are in parentheses
Health Care Coverage (hcc) is treated as the outcome or dependent variable in the model and it is figure out by the approach of indirect utility. All variables are figured out by dummy (1,0) except Capitation (cap) and Social Health Insurance (shi). The following part will explain all the variables in the models for better understanding.
Health care coverage (HCC)
Health care coverage means people receive quality health services. The goal of HCC calls for health services of many kinds, for strengthening the entire health system and for intersectional and diversified actions.
Capitation
Capitation is defined as managed care contracts or reimbursement to physicians. This is a payment methodology where a fixed amount of money is paid in advance to the insurance company for the delivery of health care services. Most health maintenance organizations (HMOs) and point-of-service (POS) pay their network physicians on a capitation basis. Under this provision, the plan sets a fixed fee for the physician for every share-based visit.
Telemedicine
Telemedicine is a kind of e-based or information communication technology (ICT) supported treatment system. Under the provision of Telemedicine, it is possible to provide service by MBBS and specialized doctors. The patient can directly consult or talk about his/her health problem to the doctor and can take advice from him through video conferencing. Digital telescope, electrocardiogram (ECG), breathing measure device and stand camera are the important components of Telemedicine. Information about a patient is directly going to the doctor through the use of such components and thus quick remedial measures are available from him.
Medicaid
Medicaid is a part of social security. This program is aimed at low-income people rather than just the aged. Certain vulnerable and needy individuals like blind, dependent children, pregnant women, and families with low incomes and resources get medical assistance under the provision of Medicaid.
Social health insurance (SHI)
SHI is a part of health care financing. It is a system of assurance to make contingencies of health care expenses. It can protect people from loss of earnings or savings due to high OOP expenditure, retirement, death or disability. Under the social insurance program, it is possible to avoid adverse selection and moral hazard problems.
Medicare
Medicare is an approach of co-pays and deductibles for the aged and certain disabled person. It includes hospital insurance (inpatient hospital services), supplementary medical insurance (outpatient services), new prescription drug benefits, etc.
Results
Disparity analysis
Lower income group or poor people in coastal Bangladesh get less health care facilities compared to those of the other middle and high-income groups. As shown in Table 2 below, health care disparity for different socio-economic groups is statistically significant with the expected sign at the convenient 1%, 5%, and 10%. Estimated results from DRR suggest that 1% income variation will lead to further fluctuation of health care disparity for all socio-economic groups.
Econometric analysis
All attributes in the first Logistic regression model for the low-income group are statistically significant at conventional levels 0.01 percent, 0.05 percent and 0.10 percent with expected signs except the Telemedicine because of high P-value. It was observed at the time of the interview that the poor respondents are not more concerned about the access and availability of health care service through Telemedicine. Thus, it is not possible to say something about Telemedicine. We also noticed that all attributes are statistically significant in the other two models for middle income and higher income groups except Medicaid and Medicare due to high P-value. During the survey time, we saw that most of the households in these groups are not interested to pay for Medicaid and Medicare because these attributes are not fulfilled their interest in health care.
It is possible to estimate the overall explanatory power or goodness of fit by using McFadden’s R2 square [46–48]. Pseudo R square statistics between 0.2 and 0.4 are said to be adequate [46,48,49]. The estimated values of McFadden R2 of all three models are estimating 0.339, 0.311 and 0.293 respectively, which maintaining the adequate level of goodness of fit. These values imply that 33, 31 and 29% of the total variations of the outcome variable of all models can be explained by the variation of attributes. The high value of goodness of fit allows us to select the best-fitted model. Based on the high value of goodness of fit (McFadden R2), we considered health care coverage model 1 for the lower income group for policy formation.
Discussion and conclusion
Promoting and protecting health are essential to human welfare, sustained economic and social development. But it is hampered when we see health care disparity in society. Generally, lower socioeconomic groups experience poorer health status. This situation gets more force in the coastal area because of limited resources. The lower socioeconomic group relies mostly on direct payment for health (out-of-payment) for medicine and health care services. As a consequence, this group is pushed below the poverty line for paying their own health expenditure .
Under the resource constraint conditions, Capitation, Medicare, Medicaid, and Social Health Insurance through UHC can play an important role to protect the lower socioeconomic groups from financial hardship during the catastrophic period. UHC works as a bridge between cost and health coverage.
Government intervention is highly required to implement UHC successfully. Based on the estimated results, government can provide support to certain vulnerable and needy individuals like blind, dependent children, pregnant poor women, aged people, unemployed, poor and needy people, widowed and divorced women, beggars and disable people through the approach of capitation, Medicare, community or social health insurance and Medicaid.
This study fully depends upon the primary data source for empirical assessment. It tried to minimize cross-level bias. But it is not certainly said that collected data are free from certain flaws. This study warranted a systematic investigation into the health disparities among different socioeconomic groups. Therefore, a time series or longitudinal study with a broader study area would have been more being fitting. But the study could only investigate a few particular sites in a given (short) period. This has somewhat delimited the scope of the study. The description and analysis of the study are incomplete in the sense that it does not interact with the majority of coastal people about their health care status.
Footnotes
In Bangladesh, the proportion of employed population below $1.90 equivalent to BDT 155.8 at daily (ROE: 1USD=82.00 BDT at 18 February 2018) and monthly, it will 4674 Tk. in terms of purchasing power parity (PPP) (Source: Asian Development Bank 2017).
Taka is the currency of Bangladesh.
Disclosure statement
No potential conflict of interest was reported by the author.
Supplementary material
Supplemental data for this article can be accessed here.
References
- [1].Zajacova A, Lawrence EM.. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Veugelers PJ, Yip AM. Socioeconomic disparities in health care use: does universal coverage reduce inequalities in health? J Epidemiol Community Health. 2003;57(6):424–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cookson R, Propper C, Asaria M, et al. Socio‐economic inequalities in health care in England. Fiscal Stud. 2016;37(3–4):371–403. [Google Scholar]
- [4].Pless IB, Hodge M, Evans RG. If not genetics, then what? Biological pathways and population health In: Evans RG, Barer ML, Marmor TR. Why are some people healthy and others not? New York: Routledge; 2017. p. 161–188. [Google Scholar]
- [5].Björk A, Rönngren Y, Selander J, et al. Health, lifestyle habits, and physical fitness among adults with ADHD compared with a random sample of a Swedish general population. Society Health Vulnerability. 2018;9(1):1–12. [Google Scholar]
- [6].Hemmingsson E. Early childhood obesity risk factors: socioeconomic adversity, family dysfunction, offspring distress, and junk food self-medication. Curr Obes Rep. 2018;7:204–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hertzman C, Frank J, Evans RG. Heterogeneities in health status and the determinants of population health In: Evans RG, Barer ML, Marmor TR, editors. Why are some people healthy and others not? New York: Aldine de Gruyter; 1994. p. 67–92. [Google Scholar]
- [8].Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Sci Med. 1997;44:809–819. [DOI] [PubMed] [Google Scholar]
- [9].Devis K, Gold M, Makuc D. Access to health care for the poor: does the gap remain? Rev Publ Health. 1981;2:159–182. [DOI] [PubMed] [Google Scholar]
- [10].Thompson GA, Whiffen LH. Can physicians demonstrate high quality care using paternalistic practices? A case study of paternalism in Latino physician–patient interactions. Qual Health Res. 2018;28(12):1910–1922. [DOI] [PubMed] [Google Scholar]
- [11].Weber-Gasparoni K. Examination, diagnosis, and treatment planning of the infant and toddler In: Nowak AJ, Christensen JR, Mabry TR, et al. Pediatric dentistry. Content Repository Only. Philadelphia: Saunders; 2019. p. 200–215. [Google Scholar]
- [12].Jensen HH, Saupe WE. Determinants of health insurance coverage for farm family households: a mid western study. North Central J Agric Econ. 1987;9(1):145–155. [Google Scholar]
- [13].McIntyre D, Thiede M, Dahlgren G, et al. What are the economic consequences for households of illness and of paying for health care in low-and middle-income country contexts? Soc sci med. 2006;62(4):858–865. [DOI] [PubMed] [Google Scholar]
- [14].Merchant KM, Kurz KM. Women’s nutrition through the life cycle: social and biological vulnerabilities In: Koblinsky M, Timyan J and Gay J, editors. The health of women. NewYork: Routledge; 2018. p. 63–90. [Google Scholar]
- [15].Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- [16].Samuel K, Alkire S, Zavaleta D, et al. Social isolation and its relationship to multidimensional poverty. Oxford Dev Stud. 2018;46(1):83–97. [Google Scholar]
- [17].Marmot M, Commission on Social Determinants of Health . Achieving health equity: from root causes to fair outcomes. Lancet. 2007;370(9593):1153–1163. [DOI] [PubMed] [Google Scholar]
- [18].Lleras-Muney A. Mind the gap: a review of the health gap: the challenge of an unequal world by Sir Michael Marmot. J Econ Lit. 2018;56(3):1080–1101. [Google Scholar]
- [19].Freedman LP, Maine D. Women’s mortality: a legacy of neglect In: Koblinsky M, Timyan J and Gay J, editors. The health of women. New York: Routledge; 2018. p. 147–170. [Google Scholar]
- [20].Filippi V, Ronsmans C, Campbell OM, et al. Maternal health in poor countries: the broader context and a call for action. Lancet. 2006;368(9546):1535–1541. [DOI] [PubMed] [Google Scholar]
- [21].Iqbal MH. Protecting coastal households from catastrophic health expenditure: an empirical investigation. World J Social Sci. 2018;8(3):28–41. [Google Scholar]
- [22].Sachs J. The end of poverty: economic possibilities for our time. Eur J Dent Educ. 2008;12:17–21. [DOI] [PubMed] [Google Scholar]
- [23].Turner L. First world health care at third world prices: globalization, bioethics and medical tourism. BioSocieties. 2007;2(3):303–325. [Google Scholar]
- [24].Pocock NS, Phua KH. Medical tourism and policy implications for health systems: a conceptual framework from a comparative study of Thailand, Singapore and Malaysia. Global Health. 2011;7(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Musango L, Orem JN, Elovainio R, et al. Moving from ideas to action-developing health financing systems towards universal coverage in Africa. BMC Int Health Hum Rights. 2012;12(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Odeyemi I, Nixon J. Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. Int J Equity Health. 2013;12(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Knaul FM, González-Pier E, Gómez-Dantés O, et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380(9849):1259–1279. [DOI] [PubMed] [Google Scholar]
- [28].Xu K, Evans DB, Carrin G, et al. Protecting households from catastrophic health spending. Health Affairs. 2007;26(4):972–983. [DOI] [PubMed] [Google Scholar]
- [29].Buse K, Hawkes S. Health in the sustainable development goals: ready for a paradigm shift? Global Health. 2015;11(13):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Badgley RF. Social and economic disparities under Canadian health care. Int J Health Serv. 1991;21:659–671. [DOI] [PubMed] [Google Scholar]
- [31].Lockett H, Lai J, Tuason C, et al. Primary healthcare utilisation among adults with mood and anxiety disorders: an analysis of the New Zealand health survey. J Prim Health Care. 2018;10(1):68–75. [DOI] [PubMed] [Google Scholar]
- [32].Sayal K, Prasad V, Daley D, et al. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry. 2018;5(2):175–186. [DOI] [PubMed] [Google Scholar]
- [33].Shibuya K, Hashimoto H, Ikegami N, et al. Future of Japan’s system of good health at low cost with equity: beyond universal coverage. Lancet. 2011;378(9798):1265–1273. [DOI] [PubMed] [Google Scholar]
- [34].Mills A, Ally M, Goudge J, et al. Progress towards universal coverage: the health systems of Ghana, South Africa and Tanzania. Health Policy Plan. 2012;27 Suppl 1:i4–i12. [DOI] [PubMed] [Google Scholar]
- [35].Hosseinpoor AR, Victoa CG, Bergen N, et al. Towards universal health coverage: the role of within-country wealth-related inequality in 28 countries in sub-Saharan Africa. Bull World Health Organ. 2011;8(9):881–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sharma R. Impacts on human health of climate and land use change in the Hindu Kush-Himalayan region: overview of available information and research agenda. Mt Res Dev. 2012;32(4):480–486. [Google Scholar]
- [37].Pavlovic M, Jazbec A, Simic D, et al. Variation in survival in coastal and continental region of Croatia-results of a longitudinal study. Eur J Epidemiol. 2000;16(11):1061–1068. [DOI] [PubMed] [Google Scholar]
- [38].Korn EL, Graubard BI. Epidemiologic studies utilizing surveys: accounting for the sampling design. Am J Public Health. 1991;81(9):1166–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Aliga A, Ren R.. 2006. Cluster optimal sample size for demographic and health survey. Available from: https://iase-web.org/documents/papers/icots/3J3_ALIA.pdf
- [40].Hammig B, Henry J, Davis D. Disparities in health care coverage among US Born and Mexican/Central American Born labor workers in the US. J Immigr Minor Health. 2019;21(1):66–72. [DOI] [PubMed] [Google Scholar]
- [41].Andreae MH, Gabry JS, Goodrich B, et al. Antiemetic prophylaxis as a marker of health care disparities in the national anesthesia clinical outcomes registry. Anesthesia Analg. 2018;126(2):588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Marafino BJ, Park M, Davies JM, et al. Validation of prediction models for critical care outcomes using natural language processing of electronic health record data. JAMA Network Open. 2018;1(8):e185097–e185097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. [DOI] [PubMed] [Google Scholar]
- [44].Figueroa JF, Zheng J, Orav EJ, et al. Medicare program associated with narrowing hospital readmission disparities between Black and White patients. Health Affairs. 2018;37(4):654–661. [DOI] [PubMed] [Google Scholar]
- [45].Fishman J, McLafferty S, Galanter W. Does spatial access to primary care affect emergency department utilization for nonemergent conditions? Health Serv Res. 2018;53(1):489–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Agimass F, Mekonnen A. Low-income fishermen’s willingness-to-pay for fisheries and watershed management: an application of choice experiment to Lake Tana, Ethiopia’. Ecol Econ. 2011;71:162–170. [Google Scholar]
- [47].Hensher DA, Rose JM, Greene WH. Applied choice analysis: a primer. UK: Cambridge University Press; 2010. [Google Scholar]
- [48].Birol E, Karousakis K, Koundouri P.. Using a choice experiment to estimate the non-use values of wetlands: the case of Cheimaditida wetland in Greece. Environmental Economy and Policy Research Discussion Paper Series. UK: Department of Land Economy, University of Cambridge; 2005. [Google Scholar]
- [49].Bennett J, Blamey R. The choice modeling approach to environmental valuation. In: Elgar E, editor. The choice content repository only to environmental valuation. Cheltenham: Edward Elgar Publishing; 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


