Abstract
Rationale:
Parents are one of several key gatekeepers to mental health (MH) services for adolescents with MH problems. Parental MH stigma is a significant barrier to treatment, yet little is known about how stigma may bias parental recognition of mental illness in youth.
Objective:
This study examines how stigma influences a critical and early stage of the help-seeking process—the recognition of MH problems in preadolescents by their parents.
Method:
Parents from a school-based anti-stigma intervention study were analyzed. Logistic regressions examined the association of stigma with parental recognition of MH problems in their preadolescent child (10–12 years old) and that of two preadolescent vignette characters described as having bipolar disorder and social anxiety disorder.
Results:
The more parents desired their preadolescent child to avoid interaction with individuals with a mental illness—that is, to be more socially distant—the less likely these parents believed their child had a MH problem, controlling for parent-reported MH symptoms and other covariates. This pattern was prominent among parents who reported high symptoms in their child. Social distance had no bearing on whether parents recognized the vignette characters as having a problem. Avoidance of individuals with a mental illness and knowledge/positive MH attitudes were not associated with problem recognition.
Conclusion:
Stigmatizing attitudes of parents may be detrimental when trying to understand the psychopathology of their own preadolescent children but not preadolescents outside their family. Stigma may present itself as a barrier to problem recognition because it may impose a significant personal cost on the family, thereby affecting the help-seeking process earlier than considered by previous work.
Keywords: stigma, mental health, help-seeking, adolescents, parents, USA
Introduction
The burden of mental health problems has steadily increased over time and become a growing concern in adolescent populations across the world (Bor et al., 2014; Polanczyk et al., 2015). Although treatment is most common among adolescents with severe psychiatric problems (Merikangas et al., 2009), fewer than half of adolescents with a disorder receive treatment (Merikangas et al., 2011; Merikangas et al., 2009; Olfson et al., 2015). Left untreated, poor mental health can negatively impact adult outcomes, including unemployment, low income, and limited social mobility (Egan et al., 2016; Goodman et al., 2011; Smith & Smith, 2010). These substantial consequences highlight the need to understand factors that impede and/or encourage adolescents to receive care, especially considering the availability of effective treatments (Chorpita et al., 2011). However, adolescent help-seeking is complex because adolescents often require adult gatekeepers to facilitate entry into formal care. The ways in which gatekeepers, particularly parents, perceive mental illness in adolescents may significantly influence the help-seeking and illness trajectories of adolescents with mental health problems. This study examines an early stage of the help-seeking process—parents’ recognition of mental health problems in adolescents.
Generally, mental health stigma is negatively associated with help-seeking and treatment use (Clement et al., 2015; Gaddis et al., 2018; Ohan et al., 2015). For adolescents especially, parental stigmatizing attitudes are strong barriers to help-seeking (Gronholm et al., 2015); however, little is known about how stigma may impact earlier stages of this process. The purpose of this study is to assess whether stigma among parents plays a role in their recognition of mental health problems in preadolescents (aged 10–12 years).
Mental Health Problem Recognition
The parent-mediated pathway to adolescent help-seeking can be summarized in three steps: (1) problem recognition—the realization that observed symptoms/behaviors are problematic; (2) decision to seek help—recognizing the benefits of treatment; and (3), treatment selection—choosing to seek informal and/or formal c are (Cauce et al., 2002). While progression through these stages is not always linear, many studies point to the importance of problem recognition—appraisals and perceptions of mental health problems—as it is strongly and positively linked with willingness to seek help and treatment utilization (Godoy et al., 2014; Logan & King, 2002; Oh & Bayer, 2015; Pescosolido et al., 2008; Teagle, 2002; Thurston et al., 2015).
Cauce and colleagues (2002) note that problem recognition can be assessed in two ways: as an objective measure of epidemiologically defined need (e.g., mental health screening, clinical assessments) or as a subjective measure of perceived need (i.e., belief that someone has a mental health problem). Although objective and subjective need are correlated features of the problem recognition construct, each is conceptualized separately (Fleishman & Zuvekas, 2007). Objective need measures provide specific information about the type, severity, and/or persistence of mental health problems, whereas subjective need taps into global perceptions of illness and indicates whether individuals identify with the sick/patient role. The presence of symptoms can inform global perceptions of adolescent mental illness among parents; yet, symptoms may not always align with the way parents perceive mental illness in their children and whether they consider specific symptom patterns as problematic (Cauce et al., 2002). For example, two-thirds of parents of children with mental health symptoms do not perceive these symptoms as part of an underlying mental health problem (Logan & King, 2002; Teagle, 2002). For the current study, we conceptualize problem recognition as a perceived need because the global belief that a mental health problem exists is related to help-seeking intentions among parents and is one of the strongest predictors of help-seeking in young populations (Oh & Bayer, 2015). Objective need measures are conceptualized as predictors of perceived problem recognition.
Previous studies reveal several influential factors contribute to the recognition of problematic adolescent mental health among parents, including the nature of the problem, prior exposure to mental illness, mental health literacy, and familial dynamics. First, severe symptoms may inflict functional impairments and substantially burden families, prompting parents to believe their adolescent child is experiencing psychological difficulties (Godoy et al., 2014; Logan & King, 2001, 2002; Teagle, 2002). Additionally, although internalizing symptoms are perceived as more severe than externalizing symptoms (Pescosolido et al., 2008), the latter are more identifiable (Thurston et al., 2015). Second, problem recognition assumes that parents have a working knowledge of the causes of mental disorders (Godoy et al., 2014). Likewise, parents who have personal experience with mental illness (family history of illness/treatment, contact with people with a mental illness) are better able to acknowledge the signs of moderate to severe psychological distress, depression (at both the symptom and disorder level), and diagnosable internalizing/externalizing problems among children/adolescents (Logan & King, 2002; Thurston et al., 2015). Lastly, characteristics of families are important. Close parent-adolescent relationships can facilitate trust in communicating mental health concerns between parents and children/adolescents, making parents more aware of their symptoms and helping them frame these symptoms as part of a larger psychiatric problem (Logan & King, 2002). Existing research, however, has overlooked the potential role of stigma in affecting how parents view adolescent mental health.
Stigma and Problem Recognition
Link and Phelan (2001) broadly conceptualize stigma as the convergence of the following interrelated components: labeling, stereotyping, separation, status loss, and discrimination. In the first component, differences between persons who are distinguished and labeled (e.g., someone has a mental illness versus not). Undesirable characteristics and negative stereotypes are then applied to labeled persons, creating a sense of separation between groups (“us” versus “them”). The culmination of these components leads to labeled persons experiencing negative social consequences including diminished social status and increased discrimination.
This conceptualization informs the domains that are relevant to measuring mental health stigma. One of the most common approaches is to measure the desire for “social distance”—a person’s level of willingness to interact with a stigmatized person in different types of relationships (Link et al., 2004). Social distance captures the separation and discrimination components of stigma. Assessments of mental health knowledge and attitudes, in contrast, examine the pervasiveness of stereotypes (e.g., mental illness as a weakness) as cognitive knowledge structures in the general public (Link et al., 2004). Lastly, the labeling component relates to distinguishing differences between persons with and without a mental illness. Labeling can lead to stereotypes and discrimination, treatment engagement, or both. Because of this potential dual consequence, Link and Phelan (2013) have referred to labeling as involving a “package deal” that can simultaneously confer positive and negative consequences.
Corrigan (2004) postulates that stigma influences help-seeking among persons with mental illness in two ways. First, public stigma—negative public attitudes and actions (e.g., avoidance) towards persons with a mental illness may deter individuals with a mental illness from seeking treatment to avoid being labeled or to escape deleterious consequences like discrimination. The second way is through self-stigma—internalized public stigma—where persons may eschew treatment ito elude stigma’s negative effects on their sense of self. This framework, however, presumes stigma is a consequence of recognizing a mental illness. It does not consider whether preexisting stigmatizing attitudes disrupt problem recognition in oneself, close family members, and others early in the help-seeking process.
Research on stigma and psychiatric labeling in adolescents is less developed than in adults. The primary concerns of existing research have been the ways labels affect stigmatizing attitudes, rather than the reverse: Whether stigma affects labeling (problem recognition). For example, among Australian youth, schizophrenia/psychosis labels perceived in vignette characters were associated with the belief that these characters were dangerous or unpredictable (stereotypes), but these labels did not worsen social distance attitudes (separation and discrimination) (Wright et al., 2011). In contrast, accurate labeling of psychiatric disorders by young populations decreased stigmatizing attitudes linked to beliefs that these conditions were a sign of weakness and not illness, thereby negating certain stereotypes, but not other stigma outcomes (Yap et al., 2013).
This study builds on such past research to further understanding of stigma and problem recognition in three ways. First, prior research has generally focused on the youth perspective— how youth label a mental illness—and has neglected to consider the role parents play in recognizing mental health problems in young people. As a key gatekeeper to mental health services, it is vital to understand how stigma may affect parents’ recognition of these conditions in adolescents.
Second, the central question in past studies has been whether psychiatric labels increase stigma, not the reverse: Does stigma influence recognition of mental health problems? For the current study, we propose that stigma may influence parental recognition of mental health problems in adolescents because stigma may push parents to deny their adolescent’s symptoms or reframe their perceptions of mental illness in order to circumvent stigma’s harmful effects on their child and/or family.
Lastly, the role of stigma in parental problem recognition may be elucidated by considering how stigma relates to problem recognition in parents’ own adolescent children versus in unrelated adolescents (adolescents outside the family). When the potentially stigmatized person is a family member, the consequences of stigma may negatively impact a loved one and/or other family members (Mukolo et al., 2010; Phelan et al., 1998). As such, stigma may dissuade parents from believing their adolescent child has a mental health problem because the label may lead to harm like marginalization and discrimination for the adolescent and/or family (Pullmann et al., 2010). In contrast, stigma may not affect a parent’s ability to label mental health problems in unrelated adolescents because the label brings no immediate risk to their adolescent child or family. This question, to our knowledge, has yet to be examined.
Current Study
In this study, we examine stigma’s role in parental recognition of mental health problems in preadolescents (aged 10–12 years) and hypothesize that stigma will deter parents from perceiving problems in their own preadolescent child but not in unrelated preadolescents. We also contend that successful recognition of mental health problems by parents is most important for high-symptom preadolescents because they may greatly benefit from treatment, given that recognition in this group is strongly associated with help-seeking (Olfson et al., 2015). If stigma is a barrier to problem recognition, then high-symptom preadolescents may be at the greatest risk of having their symptoms go unidentified. We therefore also hypothesize that stigma will obstruct recognition among parents with high-symptom preadolescents but not those with low or no symptoms.
Methods
Data
The data were gleaned from a school-based anti-stigma intervention study among sixth-grade students (Painter et al., 2016). All sixth-grade students and their parents from 14 socioeconomically and racially/ethnically diverse schools from an urban/suburban school district in Texas were invited to participate in the study (60% response rate). Preadolescents sampled were similar to the 2011 Texas public school population in terms of race/ethnicity (Texas Education Agency, 2011): Latino/Hispanic (44% sampled; 50% Texas-wide), non-Latino Black/African American (22% sampled; 13% Texas-wide), and non-Latino white/White (23% sampled; 32% Texas-wide).
Schools were randomized to receive none, one, or a combination of three interventions: (1) an anti-stigma teacher-led curriculum; (2) contact with young adults who described their experiences with bipolar disorder; and/or (3), supplemental materials with anti-stigma messaging. The study included an in-class pre/post-test evaluation (2011–2012) and longitudinal in-home follow-up assessments at six-, 12-, 18-, and 24-months post-intervention (2012–2015). Parents/guardians (hereafter labeled more simply as parents) were not exposed to the interventions and were only invited to participate in longitudinal assessments (n=484). Nearly 90% of invited parents (n=432) completed a computer-based self-administered assessment at the six-month follow-up. Informed consent of the parents and assent of their preadolescent child (hereafter referred to as the parent’s child) were obtained after procedures were explained. The study was approved by Institutional Review Boards of MHMR of Tarrant County and Columbia University Medical Center.
Sample
The current study uses cross-sectional data of the parent sample from the six-month assessment (n=432), which was the first assessment conducted in the family’s home and the first time parents provided data relevant to stigma and help-seeking. Overwhelmingly, parents were in their late 30s, female, and a biological parent (not shown in Table 1). Few fathers were interviewed because parents who were the primary caregiver for the child were invited to participate. Three-quarters identified as belonging to a racial/ethnic minority group. Our sample were socioeconomically diverse: Nearly one-in-three reported household incomes under $20,000, while 30.6% reported incomes between $20,000–$39,999, 19.4% between $40,000–$74,999, and 20.5% greater than $75,000. In 2011, the national household income median was $50,502, comparable to the Texas household median of $49,392 (Noss, 2012). Whereas most parents were employed, one-fifth were not actively in the workforce. About one-quarter had a high school education and nearly 60% had at least some college education.
Table 1.
Sample descriptive statistics, Texas Stigma Study (2011–2015).
| Total Sample (n=399) |
Low-Symptom Subsample (n=250) |
High-Symptom Subsample (n=149) |
|
|---|---|---|---|
| Mean (SE) or % | Mean (SE) or % | Mean (SE) or % | |
| Parent Characteristics | |||
| Age | 38.39(.33) | 38.68(.41) | 37.91(.56) |
| Male | 14.5% | 16.1% | 11.9% |
| Race/Ethnic Minority | 72.4% | 78.0% | 63.1% |
| Educational Attainment | |||
| < High School | 16.8% | 21.5% | 9.0% |
| High School or GED | 24.5% | 25.1% | 23.4% |
| Some college | 36.2% | 33.6% | 40.7% |
| Bachelor’s or Graduate Degree | 22.4% | 19.8% | 26.9% |
| Household Income | |||
| < $20K | 29.5% | 30.9% | 27.0% |
| $20K - $39,999 | 30.6% | 32.0% | 28.2% |
| $40K - $74,999 | 19.4% | 16.8% | 23.8% |
| > $75K | 20.5% | 20.3% | 21.0% |
| Employment Status | |||
| Employed | 73.5% | 75.3% | 70.5% |
| Unemployed | 5.1% | 3.6% | 7.5% |
| Not in labor force | 21.4% | 21.1% | 21.9% |
| Stigma | |||
| Social distance | 1.92(.04) | 2.04(.05) | 1.72(.05) |
| Avoidance | 0.72(.06) | 0.55(.06) | 1.00(.11) |
| Knowledge/positive attitudes | 3.78(.02) | 3.73(.03) | 3.88(.03) |
|
Preadolescent Symptoms and Behaviors |
|||
| Depressive symptoms | 1.33(.09) | 0.38(.04) | 2.94(.16) |
| Anxiety symptoms | 1.13(.10) | 0.21(.03) | 2.67(.20) |
| Attention symptoms | 1.84(.09) | 0.87(.07) | 3.47(.12) |
| Aggressive behaviors | 1.09(.09) | 0.63(.08) | 1.86(.18) |
| Exposure to Mental Illness | |||
| Familiarity | 2.10 (.07) | 1.79 (.08) | 2.61 (.11) |
| Family history of mental illness | 52.9% | 39.0% | 76.1% |
| Problem Recognition | |||
| Parent perceived problem | 29.1% | 12.0% | 57.7% |
| Preadolescent self-perceived problem |
22.2% | 13.6% | 36.6% |
| Julia Vignette (n=398) | |||
| Social distance | 2.19 (.04) | ||
| eriousness of condition | 3.66 (.03) | ||
| Perceived problem | 80.9% | ||
| David Vignette (n=390) | |||
| Social distance | 1.79 (.04) | ||
| Seriousness of condition | 2.88 (.04) | ||
| Perceived problem | 45.9% | ||
Measures
Problem recognition in this study is conceptualized as the parent’s perception of their preadolescent child’s global mental health and was measured by a single-item: “ Was there a time in the past six months, when your child seemed to have an emotional or behavioral problem like being anxious, depressed, hyperactive, withdrawn, or always getting into trouble?” (Yes=1/No=0). This item was developed for the study to assess global subjective mental health as this perception signals need and action for help-seeking. Single-item assessments of perceived need are common in adult mental health literature (Fleishman & Zuvekas, 2007; Villatoro et al., 2018).
Problem recognition in unrelated adolescents was assessed using two preadolescent vignette characters described as meeting criteria based on the Diagnostic and Statistical Manual of Mental Disorders, IV (American Psychiatric Association, 2000) for bipolar disorder (Julia) and social anxiety disorder (David). After each vignette, participants responded to questions about the character, including whether they believed Julia/David was experiencing a mental illness (Yes=1/No=0). The use of vignettes in stigma research is common as this method delivers a clearly specified stimulus for measuring participant reactions (Link et al., 2004). Although vignettes are hypothetical and therefore limited in that respect, their key methodological advantages are that all respondents receive and react to the same stimulus and researchers know the exact content soliciting those reactions (Link et al., 2004).
Three stigma measures associated with the separation and stereotype stigma components were assessed. Measures were adapted from existing instruments and modified to suit a preadolescent and parent sample. First, the Social Distance Scale adapted from Wahl et al.(2011), assessed the parent’s willingness for their child to interact with individuals with a mental illness in six situations (e.g. have as a neighbor, friend, etc.; 1=Definitely yes to 4=Definitely no). Mean scores were computed (α=0.94). Vignette-based social distance was assessed for each character, where the parent reported the extent that they would want their child to interact with Julia/David in the same situations previously described (1=Definitely yes to 4=Definitely no; αs=0.91 and 0.94, respectively). Higher scores suggest greater social distance. Second, parents completed a six-item scale assessing whether they avoided persons with mental health problems in the last six-months (Yes=1/No=0). Item responses were summed (α=0.68); higher scores indicated greater avoidance. Lastly, a 24-item instrument assessed mental health knowledge and attitudes towards persons with a mental illness, adapted from Wahl et al. (2011). Knowledge was assessed by factual statements (“A mental illness is caused by something genetic or hereditary”); attitudes were assessed by opinion statements (“A person with a mental illness is able to be a good friend”). Respondents indicated the degree to which they agreed with each statement (1=Strongly disagree to 5=Strongly agree). Items where correct knowledge/positive attitudes reflected disagreement were reverse coded. Exploratory factor analyses were conducted to examine the measure’s psychometric properties in this sample. Results showed that the data best fit a one-factor scale; an overall mean score was calculated (α=0.79) where higher scores represented greater knowledge/positive attitudes.
Objective need was assessed via parent reports of their preadolescent child’s mental health using a 23-item symptoms screen (Yes=1/No=0). An accredited mental health social worker created the condensed screen using gate questions from the Major Depressive Episode, Anxiety Disorders, Attention-Deficit/Hyperactivity Disorder, and Whole Life modules of the Diagnostic Interview Schedule for Children, Version IV, a validated structured interview for assessing childhood mental disorders (DISC-IV; Shaffer et al., 2000). The screen was developed for administration within the time constraints of the study survey. Parent items were adapted from the preadolescent survey items. Exploratory factor analyses revealed three symptom domains that aligned with the DISC-IV modules: depressive (seven items), anxiety (ten items), and attention (five items) symptoms. One item was excluded for poor content validity. Summed scores were calculated for each domain and the scales demonstrated good internal consistency (αs=0.77 to 0.85). Parents also reported on their child’s acted aggressive behaviors in the past month (e.g., hit/slapped another child, threatened to hurt someone; nine items); a count of endorsed behaviors was created. For each vignette, parents indicated the degree to which they perceived Julia’s/David’s condition to be serious ( 1=Definitely no to 4=Definitely yes).
An indicator variable captured family history of mental illness—a family member having or showing signs of depression, anxiety, substance use problems, or other mental health problems (Yes=1/No=0). Familiarity with mental illness was assessed using an abbreviated version of the Level of Contact Report (Holmes et al., 1999). Parents were asked about personal interaction with individuals who have a mental illness in six contexts: Seeing a mentally ill person on television (least contact); having a coworker, friend, or relative with a mental illness; living with someone who has a mental illness; and whether the parent has a mental illness (most contact). Approximately 13% of parents reported having a mental illness. Two items (having a relative or living with someone with a mental illness) were excluded because they overlapped with family history and problem recognition in the parent’s child. Combined item responses created a ranked familiarity score (0=no contact to 4=most contact).
The analyses controlled for parent characteristics, including gender (female—reference group), race/ethnicity (non-minority—reference group), and household income. Parental education, employment, and other children in the home were examined as covariates but were not associated with the outcomes and not included in the final analyses. We also controlled for child characteristics, including gender (female—reference group) and family cohesion using a 10-item measure (Olson, 1986) that assessed the extent of the family’s communication about problems/troubles, reliance for support/help, etc. (1=Not very often to 4=Always; α=0.88). The analyses also adjusted for self-perceived mental health by the preadolescent, measured using a single-item that parallels the parent item (“I seemed to have a mental health prob lem like being anxious, depressed…”; Yes=1/No=0). The purpose was to examine whether self-perceived mental health problems by preadolescents were correlated with parental recognition, because positive concordance in these perceptions (when both parents and preadolescents perceive a problem in the preadolescent) may be crucial to initiating help-seeking. Only 9% of parents and preadolescents in the sample were concordant in their recognition of mental health problems. Lastly, although parents were not exposed to the interventions, analyses control for their child’s assigned intervention group (None/Materials Control—reference group, Curriculum; Contact; Curriculum and Contact) to adjust for possible spillover of the intervention on parental attitudes/problem recognition. Only one of nine tests resulted in a significant intervention effect on problem recognition, suggesting minimal contamination.
Data Analysis
The effect of stigma on parental problem recognition in their child (Outcome 1) and vignette characters (Outcome 2) was examined. For Outcome 1, multivariable logistic regressions using the total sample controlled for: parent reports of their preadolescent child’s mental health symptoms, the parent’s familiarity with and family history of mental illness, parent characteristics (gender, race/ethnicity, income), and preadolescent characteristics (gender, self-perceived problem, and family cohesion, intervention assignment). As high-symptom preadolescents may be most at risk of having problems unrecognized by parents in the presence of stigma, despite demonstrating a need for treatment, we tested an interaction between stigma and symptomatology using the global count of mental health symptoms. Parents who rated their child in the top-tertile of number of symptoms were categorized as likely having a high-symptom child; those in the bottom-and middle-tertiles were categorized as low-symptom. On average, those in the high-symptom subsample endorsed over six times as many symptoms (M=9.08, SE=.34) as those in the bottom-and middle-tertiles combined (M=1.46, SE=.09). Although the interactions were not statistically significant, models were stratified by parent reports of child symptoms because barriers to problem recognition would likely be most detrimental to those with discernable symptomatic need for treatment. For Outcome 2, vignette-based problem recognition, the total sample of parents were analyzed. These analyses controlled for mental health exposure, parent’s perceived severity of the character’s condition, parent characteristics, intervention group, and their child’s gender. For all analyses, the stigma variables were entered first, followed by the covariates, in order to assess stigma’s effect on problem recognition over and above the covariates.
Approximately 17% of respondents are missing on the parent/preadolescent covariates and Outcome 1; about 15% are missing on the parent/preadolescent covariates and Outcome 2. Most of the missing data derive from variables collected at pre-test: income, parent gender, family history of mental illness, and family cohesion (reported by preadolescent participants). There were little missing data on the six-month assessment variables, except for preadolescent self-perceived problem (4.7% missing). Examination of the missing data revealed evidence consistent with observations being missing at random given that few characteristics (e.g., symptoms, mental illness exposure) were associated with the missingness. As such, multiple imputation was the best approach to address missing data. Longitudinal data from the pre-, post-, and six-month assessments were used to impute missing values on the parent and preadolescent variables previously mentioned. Using STATA SE 15 multiple imputation chained procedures (StataCorp, 2015), 20 data sets were imputed and combined according to Rubin’s rules (Rubin, 1987). Respondents missing on non-imputed variables were excluded (7.8 to 9.7% depending on the outcome). Complete and imputed case analyses resulted in similar patterns of results. Only imputed analyses are presented.
Results
Fewer than one-third of parents in the total sample recognized a mental health problem in their preadolescent child (see Table 1). Parental recognition varied by symptoms: While 58% of parents who reported high symptoms in their child believed that he or she had a mental health problem, a significant proportion (42%) did not equate greater symptoms to a problem. Recognition was lowest in the low-symptom subsample, a reassuring pattern because parents are expected to associate greater symptoms with an underlying mental health problem. Fewer than one-quarter of preadolescents self-perceived a problem. Far fewer preadolescents in the high-symptom subsample recognized a problem, suggesting significant discordance between the parent’s mental health perception of their child and the preadolescent’s own subjective self-report.
On average, parents demonstrated moderate levels of social distance, preferring their preadolescent child to have minimal interaction with people with a mental illness. In contrast, parents reported low avoidance of persons with a mental illness. They also had moderate knowledge/positive attitudes about mental illness, with the high-symptom subsample having better knowledge/positive attitudes than the low-symptom subsample.
Problem Recognition in Own Child
Table 2 presents the results examining the relationship of stigma with problem recognition using the total and symptom-stratified subsamples. In the reduced model for the total sample, social distance was associated with low odds of problem recognition, while avoidance was associated with high odds. Net of the covariates, only social distance was related to problem recognition (Full Model). The more social distance parents desired for their child, the less likely they were to recognize a problem. Avoidance and knowledge/positive attitudes were not significant in the full model.
Table 2.
Logistic regressions examining the effect of stigma on parental mental health problem recognition in their preadolescent child
| Total Sample (n=399) | Low-Symptom Subsample (n=250) | High-Symptom Subsample (n=149) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reduced Model | Full Model | Reduced Model | Full Model | Reduced Model | Full Model | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Stigma | ||||||||||||
| Social distance | 0.38*** | [0.23, 0.61] | 0.48* | [0.25, 0.90] | 0.61 | [0.29, 1.30] | 0.85 | [0.33, 2.17] | 0.28*** | [0.12, 0.64] | 0.18** | [0.06, 0.62] |
| Avoidance | 1.36** | [1.12, 1.65] | 0.95 | [0.73, 1.23] | 1.17 | [0.79, 1.72] | 0.97 | [0.61, 1.55] | 1.14 | [0.88, 1.48] | 0.88 | [0.63, 1.24] |
| Knowledge/positive attitudes |
1.24 | [0.58, 2.66] | 0.37 | [0.12, 1.09] | 1.73 | [0.47, 6.34] | 0.70 | [0.12, 3.90] | 0.59 | [0.18, 1.95] | 0.18 | [0.03, 1.03] |
| Mental Health Symptoms | ||||||||||||
| Depressive symptoms | 1.36** | [1.09, 1.68] | 1.04 | [0.50, 2.14] | 1.30 | [0.99, 1.71] | ||||||
| Anxiety symptoms | 1.04 | [0.85, 1.26] | 1.32 | [0.63, 2.75] | 0.98 | [0.79, 1.23] | ||||||
| Attention symptoms | 1.48*** | [1.23, 1.78] | 1.56* | [1.03, 2.35] | 1.41* | [1.05, 1.90] | ||||||
| Aggressive behaviors | 1.30** | [1.09, 1.54] | 0.99 | [0.69, 1.44] | 1.51*** | [1.18, 1.94] | ||||||
| Mental Health Exposure | ||||||||||||
| Familiarity | 1.39* | [1.06, 1.83] | 2.22** | [1.34, 3.68] | 1.07 | [0.70, 1.62] | ||||||
| Family history of mental illness |
2.23* | [1.10, 4.53] | 2.90* | [1.02, 8.29] | 1.42 | [0.43, 4.64] | ||||||
| Parent Characteristics | ||||||||||||
| Male | 0.69 | [0.29, 1.65] | 0.09* | [0.01, 0.79] | 1.84 | [0.41, 8.21] | ||||||
| Racial/ethnic minority | 2.45* | [1.17, 5.11] | 5.64* | [1.40, 22.78] | 2.02 | [0.73, 5.62] | ||||||
| Household Income | ||||||||||||
| < $20K | 1.00 | 1.00 | 1.00 | |||||||||
| $20K–$39,999 | 0.58 | [0.25, 1.35] | 0.68 | [0.15, 3.03] | 0.57 | [0.18, 1.82] | ||||||
| $40K–$74,999 | 1.67 | [0.66, 4.21] | 2.41 | [0.52, 11.26] | 1.60 | [0.39, 6.51] | ||||||
| > $75K | 2.91* | [1.16, 7.34] | 6.95** | [1.66, 29.02] | 1.74 | [0.41, 7.31] | ||||||
|
Preadolescent
Characteristics |
||||||||||||
| Male | 0.69 | [0.38, 1.25] | 0.86 | [0.32, 2.32] | 0.61 | [0.25, 1.51] | ||||||
| Self-perceived problem | 0.55 | [0.25, 1.17] | 0.54 | [0.09, 3.19] | 0.49 | [0.18, 1.37] | ||||||
| Family Cohesion | 0.70 | [0.43, 1.13] | 0.69 | [0.30, 1.57] | 0.54 | [0.26, 1.12] | ||||||
| Intervention Groups | ||||||||||||
| Control | 1.00 | 1.00 | 1.00 | |||||||||
| Curriculum only | 1.53 | [0.67, 3.51] | 0.69 | [0.17, 2.76] | 2.97 | [0.83, 10.64] | ||||||
| Contact only | 0.92 | [0.41, 2.08] | 0.78 | [0.22, 2.71] | 1.05 | [0.30, 3.65] | ||||||
| Curriculum/Contact | 0.56 | [0.20, 1.55] | 0.22 | [0.04, 1.28] | 0.92 | [0.20, 4.25] | ||||||
Note. Female parents as well as children and parents who identify as a member of a non-minority group are the omitted reference categories. OR=Odds ratio.CI=Confidence interval.
p<0.05
p<0.01
p<0.001.
Family history, familiarity, and parent-reported symptoms (except for anxiety symptoms) were significantly associated with high odds of problem recognition in the full model. Parent and preadolescent characteristics and family cohesion were non-significant, with the exception of greater odds among racial/ethnic minority parents and high-income households than non-minority parents and low-income households, respectively. Preadolescent self-perceptions did not impact parent recognition—if a preadolescent perceived a mental health problem, it did not increase the odds that the parent believed the same. The main results did not change by including these self-perceptions in the model. Furthermore, there were no statistically significant interactions between preadolescent self-perceived problems and parental stigma.
In symptom-stratified reduced models, only social distance was significantly associated with low odds of problem recognition in the high-symptom subsample. This pattern remained in the full model. No stigma variable was related to problem recognition in the low-symptom subsample. Figure 1 plots the predicted probabilities of the parent recognizing a mental health problem in their child across social distance scores for the fully-adjusted models from Table 2 using the total and symptom-stratified samples. For the high-symptom subsample, the probability of problem recognition dramatically declined as social distance increased, replicating with greater magnitude the pattern observed in the total sample. No marked changes in the probability of problem recognition were associated with increasing social distance in the low-symptom subsample.
Figure 1.
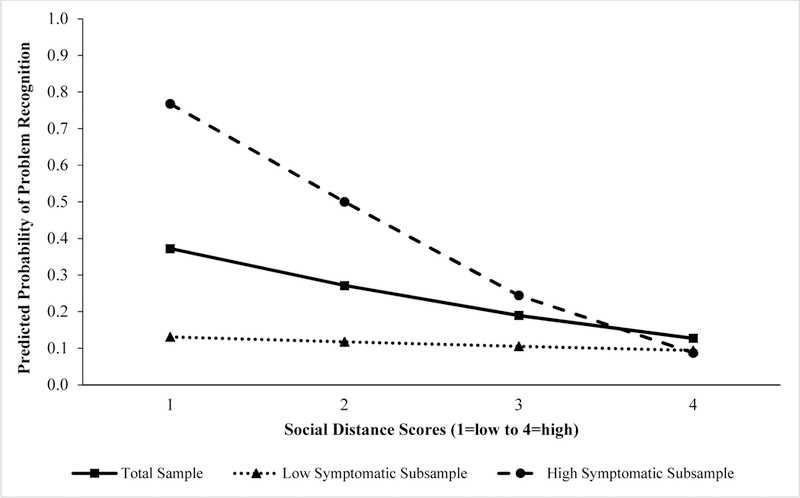
Predicted probabilities of parents recognizing mental health problems in their preadolescent child across levels of social distance in the total and symptom subsamples
NOTE: Predicted probabilities of problem recognition for “Total Sample” come from the “Total Sample: Full Model” in Table 2. Predicted probabilities for the low- and high-symptom subsamples were calculated using their respective full models. All estimates were plotted on the same chart to illustrate differences in the association of social distance with problem recognition across subsamples.
Attention symptoms and aggressive behaviors were associated with greater problem recognition in the high-symptom subsample; no other covariates were statistically significant. Attention symptoms, familiarity, family history, race/ethnicity, and income were associated with higher odds of problem recognition for the low-symptom subsample. Male versus female parents were significantly less likely to recognize a problem in the low-symptom subsample.
Problem Recognition in Vignette Characters
Parents overwhelmingly believed Julia (bipolar disorder) had a mental health problem, with many rating her condition as very serious and expressing moderate levels of social distance towards her (Table 1). In comparison, significantly fewer parents labeled David’s social anxiety disorder as a problem (p<0.001). Although parents rated his condition as moderately serious, they perceived David’s condition as less serious than Julia’s ( p<0.001) and reported significantly lower social distance towards David than Julia (p<0.001).
Table 3 presents the results of the vignette analyses. In the reduced model, higher avoidance and knowledge/positive attitudes were associated with greater odds of recognizing a problem in both characters. Social distance was non-significant. The significant effects of avoidance and knowledge/positive attitudes disappeared after adjusting for the parent’s perceived seriousness of each character’s condition and all other covariates (Full Model).
Table 3.
Logistic regressions examining the effect of stigma on parental mental health problem recognition in vignette characters
| Julia Vignette (n=398) | David Vignette (n=390) | |||||||
|---|---|---|---|---|---|---|---|---|
| Reduced Model | Full Model | Reduced Model | Full Model | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Stigma | ||||||||
| Vignette-based social distance | 0.89 | [0.60, 1.31] | 0.92 | [0.62, 1.38] | 1.35 | [0.96, 1.89] | 1.43 | [0.96, 2.14] |
| Avoidance | 1.29* | [1.00, 1.67] | 1.19 | [0.91, 1.56] | 1.27* | [1.05, 1.53] | 1.20 | [0.96, 1.50] |
| Knowledge/positive attitudes | 2.38* | [1.10, 5.18] | 1.28 | [0.52, 3.16] | 2.79** | [1.48, 5.28] | 1.63 | [0.73, 3.65] |
| Seriousness of condition | 1.91** | [1.22, 2.99] | 3.76*** | [2.65, 5.32] | ||||
| Mental Health Exposure | ||||||||
| Familiarity | 1.24 | [0.99, 1.56] | 1.25* | [1.01, 1.54] | ||||
| Family history of mental illness | 0.86 | [0.48, 1.56] | 1.10 | [0.64, 1.89] | ||||
| Parent Characteristics | ||||||||
| Male | 0.73 | [0.36, 1.48] | 0.54 | [0.26, 1.10] | ||||
| Racial/ethnic minority | 0.52 | [0.24, 1.15] | 0.37** | [0.19, 0.69] | ||||
| Household Income | ||||||||
| < $20K | 1.00 | 1.00 | ||||||
| $20K–$39,999 | 0.63 | [0.31, 1.29] | 0.81 | [0.41, 1.58] | ||||
| $40K–$74,999 | 0.93 | [0.36, 2.43] | 0.69 | [0.31, 1.51] | ||||
| > $75K | 0.72 | [0.29, 1.79] | 0.65 | [0.29, 1.43] | ||||
| Preadolescent Characteristics | ||||||||
| Male | 1.38 | [0.79, 2.40] | 1.00 | [0.61, 1.62] | ||||
| Intervention Groups | ||||||||
| Control | 1.00 | 1.00 | ||||||
| Curriculum only | 0.76 | [0.35, 1.65] | 1.65 | [0.81, 3.34] | ||||
| Contact only | 0.81 | [0.40, 1.64] | 2.25* | [1.15, 4.39] | ||||
| Curriculum/Contact | 0.81 | [0.34, 1.95] | 1.30 | [0.59, 2.83] | ||||
Note. Female parents as well as children and parents who identify as a member of a non-minority group are the omitted reference categories. Julia=vignette character with bipolar disorder. David=vignette character with social anxiety disorder. OR=Odds ratio. CI=Confidence interval.
p<0.05
p<0.01
p<0.001.
Perceiving Julia’s and David’s condition as serious was associated with problem recognition. Greater familiarity also increased the likelihood that parents believed David had a problem but not Julia. Racial/ethnic minority parents were significantly less likely than non-minority parents to believe David had a problem. Lastly, parents that had a preadolescent child who received the contact intervention versus control were twice as likely to recognize a problem in David.
Discussion
The current study examined how stigma is related to parental recognition of mental health problems in preadolescents. The findings suggest that stigma may be a hindrance when parents attempt to grasp and understand the psychopathology of their preadolescent child, but has no bearing on the successful identification of problems in unrelated preadolescents. Parental stigmatizing attitudes, specifically wanting their child to be socially distant from individuals with a mental illness (stigma separation component), are barriers to problem recognition, likely by introducing bias in the parent’s perception of what constitutes a mental illness. Thus, the impact of stigma is not only important in formulating help-seeking decisions, but may also be deeply rooted early in the help-seeking process when parents are trying to understand and label these symptoms. This connection has not been investigated in prior research.
Stigma does not always present itself as a barrier to problem recognition because it was not associated with parental perceptions of mental illness in unrelated adolescents. When the “target” of recognition is the parent’s own child, stigma may influence parents to view their symptoms as “normal behaviors” in order to protect their child and/or family from being labeled and socially excluded by others. Although stigma is typically framed as being consequential to individuals with a mental illness, stigma also affects family members by association (Mukolo et al., 2010; Phelan et al., 1998). This concept is particularly pertinent to preadolescents because parents oftentimes make mental health care decisions, and may evaluate the potential burden and cost of stigma when making these decisions. Alternatively, when the target is an unrelated adolescent, as presented by the vignette characters, these attitudes may not matter because the label does not directly affect the parent, their child, or family, resulting in no personal cost in labeling.
Other stigma attitudes were not associated with problem recognition, paralleling a recent study that did not find any relationship between mental health beliefs and problem recognition among parents (Thurston et al., 2015). At the bivariate level, knowledge/positive attitudes and avoidance were independently associated with greater odds of problem recognition; yet, after controlling for social distance and mental health exposure, these effects disappeared, suggesting social distance and exposure may be more central to the recognition of mental illness in adolescents. The positively skewed distribution of the avoidance scale may have undermined detection of any effects.
Overall, strong correlates of problem recognition were symptoms, exposure to mental illness, and income. The more symptoms the parent reported, the more likely they were to believe their child had a problem. Likewise, familiarity and family history were associated with higher odds of problem recognition. The positive association of mental illness exposure and income with problem recognition in the low-symptom subsample likely suggests that these parents may have lower thresholds for considering symptoms as problematic and may be more sensitive to their child’s behaviors. Regarding the vignette characters, only familiarity was associated with problem recognition for David. Thus, increasing mental illness exposure may help raise awareness of the early signs of mental illness and attention to when there is a problem. These findings point to the value of exposure in helping parents identify mental health problems in preadolescents/adolescents, more so than the parent’s general mental health literacy.
There was no evidence that self-perceived problems by preadolescents were correlated with parental problem recognition. At the bivariate level, parents were almost twice as likely to recognize a problem in their preadolescent child when their child self-perceived a problem compared to when their child did not; this effect was null after adjusting for parent reports of their child’s symptoms and other covariates. Nevertheless, we surmise that parent-preadolescent concordance in problem recognition may be important for parents when making help-seeking decisions. Furthermore, how stigma affects this concordance remains to be explored. Preliminary examination suggests that parent social distance scores are significantly higher when parent-preadolescent problem perceptions differ (M=1.76, SE=0.06) compared to when both agree there is a problem (M=1.57, SE=0.08); this difference, however, is marginally significant (p=0.06). More research is needed to better understand the relationship between stigma and problem recognition concordance between parents and preadolescents.
Limitations
Several limitations merit consideration. Although stigma may lead to barriers in problem recognition, our cross-sectional analysis cannot establish temporal order. Regarding issues of measurement, problem recognition was measured by a single-item, assessing perceived global mental health problems rather than recognition of specific types of problems. This measure could capture low threshold problems; however, few parents who reported low symptoms in their child believed they had a mental health problem (12%). Likewise, in stratified analyses, counts of specific symptoms (except attention symptoms) were not associated with problem recognition in the low-symptom subsample. Our analysis did not include preadolescent self-reports of symptoms because we were primarily interested in how information as perceived by the parent affect recognition. We were unable to examine how the parent’s own mental health influenced problem recognition because parent mental health symptoms were not measured; however, the familiarity scale served as a proxy because it included an item that assessed the parent’s mental health status. Vignette character descriptions also were not randomized by gender: Julia was always described as having bipolar disorder and David as having social anxiety disorder. To control for potential gender bias in how parents perceived their conditions, analyses controlled for both the parent’s and their preadolescent’s gender. Additionally, while we extend the null findings in the vignette outcomes to be relevant to unrelated adolescents to the parents, recognition may be difficult in real world situations because parents may not have all available information about the adolescent’s symptoms/behaviors. Nevertheless, parents may still use information from other sources (other parents, teachers), akin to a vignette, to make judgements about other people’s children. Finally, our sample mostly comprised female parents, limiting the study’s generalizability to male parents. Although mothers have a more active role in adolescent help-seeking than fathers (Zimmerman, 2005), future studies including more fathers can help us understand parent gender differences in perceiving mental health problems in adolescents.
These limitations notwithstanding, our study has several strengths. First, to our knowledge, this is the first study to examine the role of stigma in mental health problem recognition among parents, building on past research on labeling and stigma conducted in youth populations. This study also sheds new light on how stigma may be a notable barrier early in the help-seeking process when parents are trying to decipher their child’s symptoms. Second, we assessed how stigma affected problem recognition in preadolescents within and outside the family by asking parents about their own preadolescent child and vignette characters, respectively. Through this approach, we show that parental stigma is consequential to problem recognition only when the target has a familial association to the parent, not when the target is an unrelated adolescent. Third, sensitivity analyses were performed to include parental education, employment status, and other children in the home—none were statistically significant—hence the study findings were robust to different model specifications. Lastly, because of the regional population we sampled, our study sample is racially, ethnically, and socioeconomically diverse.
Conclusions
As the field develops strategies to improve mental health help-seeking among adolescents, the larger role of stigma in infiltrating different stages of the help-seeking process needs to be considered and further studied. Stigma is not only a barrier to treatment decision-making, but it may also impede parents’ recognition of mental health problems in their children.This barrier is problematic because parents are key gatekeepers to formal treatment. If parents demonstrate difficulty in recognizing mental health problems in their children due to stigma, then treatment may be delayed or avoided altogether, and our findings suggest that it may particularly happen when there is a heightened need for treatment. These results point to the need for unique interventions that target parental stigma of mental health problems within the family unit. Moreover, public anti-stigma intervention efforts may help reduce stigma among parents at the population level and fill the problem recognition gap for adolescents so that the onus does not lie on afflicted families alone. Addressing early-stage stigma and help-seeking barriers of parents is vital to improving treatment-seeking among adolescents with a symptomatic need.
Research Highlights.
Stigma’s role on parent mental health problem recognition in youth is unknown.
Social distance obstructs parental problem recognition in their own child.
Stigma is not associated with problem recognition in adolescent vignette characters.
Stigma may affect help seeking early as parents assess their child’s mental health.
Acknowledgements
The study was supported by grants #R01MH095254 and #5-T32-MH 13043 from the National Institute of Mental Health (NIMH) and by the Latino Research Initiative at The University of Texas at Austin. The authors thank Mental Health Connection of Tarrant County, the project staff, and the youth and parents who participated in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (2000). Diagnositc and statistical manual of mental disorders:DSM-IV Washington, DC: American Psychiatric Association. [Google Scholar]
- Bor W, Dean AJ, Najman J, & Hayatbakhsh R (2014). Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Australian & New Zealand Journal of Psychiatry, 48, 606–616. [DOI] [PubMed] [Google Scholar]
- Cauce AM, Domenech-Rodríguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, et al. (2002). Cultural and contextual influences in mental health help-seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology, 70, 44–55. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Ebesutani C, Young J, Becker KD, Nakamura BJ, et al. (2011). Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology Science and Practice, 18, 154–172. [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45, 11–27. [DOI] [PubMed] [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. American Psychologist, 59, 614–625. [DOI] [PubMed] [Google Scholar]
- Egan M, Daly M, & Delaney L (2016). Adolescent psychological distress, unemployment, and the Great Recession: Evidence from the National Longitudinal Study of Youth 1997. Social Science & Medicine, 156, 98–105. [DOI] [PubMed] [Google Scholar]
- Fleishman JA, & Zuvekas SH (2007). Global self-rated mental health: Associations with other mental health measures and with role functioning. Medical Care, 45, 602–609. [DOI] [PubMed] [Google Scholar]
- Gaddis SM, Ramirez D, & Hernandez EL (2018). Contextualizing public stigma: Endorsed mental health treatment stigma on college and university campuses. Social Science & Medicine, 197, 183–191. [DOI] [PubMed] [Google Scholar]
- Godoy L, Mian ND, Eisenhower AS, & Carter AS (2014). Pathways to service receipt: Modeling parent help-seeking for childhood mental health problems. Adm Policy Ment Health, 41, 469–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman A, Joyce R, & Smith JP (2011). The long shadow cast by childhood physical and mental problems on adult life. PNAS, 108, 6032–6037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronholm PC, Forn T, Roberts RE, Thornicroft G, Laurens KR, & Evans-Lacko S(2015). Mental health service use by young people: The role of caregiver characteristics. PLoS ONE, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EP, Corrigan PW, Williams P, Canar J, & Kubiak MA (1999). Changing attitudes about schizophrenia. Schizophrenia Bulletin, 25, 447–456. [DOI] [PubMed] [Google Scholar]
- Link BG, & Phelan JC (2013). Labeling and stigma. In Aneshensel CS, & Phelan JC (Eds.), Handbook of the Sociology of Mental Health Springer, Dordrecht, pp. 525–541. [Google Scholar]
- Link BG, Yang LH, Phelan JC, & Collins PY (2004). Measuring mental illness stigma. Schizophrenia Bulletin, 30, 511–541. [DOI] [PubMed] [Google Scholar]
- Logan DE, & King CA (2001). Parental facilitation of adolescent mental health service utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice, 8, 319–333. [Google Scholar]
- Logan DE, & King CA (2002). Parental identification of depression and mental health service use among depressed adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 296–304. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J. p., Burstein M, Swendsen J, Avenevoli S, Case B, et al. (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Nakamura EF, & Kessler RC (2009). Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci, 11, 7–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukolo A, Heflinger CA, & Wallston KA (2010). The stigma of childhood mental disorders: A conceptual framework. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noss A (2012). Household income for states: 2010 and 2011 In U.S.C. Bureau (Ed.), American Community Survey Briefs. [Google Scholar]
- Oh E, & Bayer JK (2015). Parents’ help-seeking processes for early childhood mental health problems. Child and Adolescent Mental Health, 20, 149–154. [DOI] [PubMed] [Google Scholar]
- Ohan JL, Seward RJ, Stallman HM, Bayliss DM, & Sanders MR (2015). Parents’ barriers to using school psychology services for their child’s mental health problems. School Mental Health, 7, 287–297. [Google Scholar]
- Olfson M, Druss BG, & Marcus SC (2015). Trends in mental health care among children and adolescents. The New England Journal of Medicine, 372, 2029–2038. [DOI] [PubMed] [Google Scholar]
- Olson DH (1986). Circumplex Model II: Validation Studies and FACES III. Family Process, 25, 337–351 [DOI] [PubMed] [Google Scholar]
- Painter K, Phelan JC, DuPont-Reyes MJ, Barkin KF, Villatoro AP, & Link BG (2016). Evaluation of anti-stigma interventions with sixth-grade students: A school-based field experiment. Psychiatric Services, 68, 345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Jensen PS, Martin JK, Perry BL, Olafsdottir S, & Fettes D (2008). Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 339–349. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Bromet EJ, & Link BG (1998). Psychiatric illness and family stigma. Schizophrenia Bulletin, 24, 115–126. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Salum GA, Sugaya LS, Caye A, & Rohde LA (2015). Annual Research Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56, 345–365. [DOI] [PubMed] [Google Scholar]
- Pullmann MD, VanHooser S, Hoffman C, & Heflinger CA (2010). Barriers to and supports of family participation in a rural system of care for children with serious emotional problems. Community Mental Health Journal, 46, 211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin D (1987). Multiple imputation for non-respondents in surveys Wiley & Sons, New York. [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, & Schwab-Stone M (2000). NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Smith JP, & Smith GC (2010). Long-term economic costs of psychological problems during childhood. Social Science & Medicine, 71, 110–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14 College Station, TX: StataCorp LP. [Google Scholar]
- Teagle SE (2002). Parental problem recognition and child mental health service use. Mental Health Services Research, 4, 257–266. [DOI] [PubMed] [Google Scholar]
- Texas Education Agency. (2011). Snapshot 2011: State Totals Austin, TX. [Google Scholar]
- Thurston IB, Phares V, Coates EE, & Bogart LM (2015). Clinical problem recognition and help-seeking intentions among Black and White parents. Journal of Clinical Child & Adolescent Psychology, 44, 604–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villatoro AP, Mays VM, Ponce NA, & Aneshensel CS (2018). Perceived need for mental health care: The intersection of race, ethnicity, gender, and socioeconomic status. Society and Mental Health, 8, 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl OF, Susin J, Kaplan L, Lax A, & Zatina D (2011). Changing knowledge and attitudes with a middle school mental health education curriculum. Stigma Res Action, 1, 44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A, Jorm AF, & Mackinnon AJ (2011). Labeling of mental diosrders and stigma in young people. Social Science & Medicine, 73, 498–506. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Reavley N, Mackinnon AJ, & Jorm AF (2013). Psychiatric labels and other influences on young people’s stigmatizing attitudes: Findings from an Australian national survey. Journal of Affective Disorders, 148, 299–309. [DOI] [PubMed] [Google Scholar]
- Zimmerman FJ (2005). Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health Services Research, 40, 1514–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]


