Abstract
Introduction:
Identification of modifiable risk factors for suicidal behaviors is a priority for the U.S. Army. This study investigated associations of nicotine dependence with suicidal behaviors among incoming soldiers.
Methods:
Lifetime DSM-IV nicotine dependence, mental disorders, suicidal behaviors, and their ages of onset were retrospectively assessed in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) New Soldier Study. Discrete-time survival analysis of person-year data from 30,436 soldiers was performed to evaluate associations of nicotine dependence with subsequent suicidal ideation, plans, and attempts. Among respondents with lifetime ideation (n=4,060), models tested associations of nicotine dependence with progression from ideation to first onset of plan, from plan to first attempt, and, among ideators without plans, from ideation to first unplanned attempt. A hierarchy of models incorporated increasing controls for other risk factors. Data were collected in 2011–2012 and analyzed in 2017–2018.
Results:
In models controlling for sociodemographic characteristics, nicotine dependence was associated with onset of all suicidal behaviors (AORs, 2.07–4.08, p<0.001) and with each type of progression of suicidal behavior (AORs, 1.48–2.44, p<0.005). After adjusting for childhood adversities and mental disorders, nicotine dependence remained associated with onset of ideation (AOR=1.27, 95% CI=1.10, 1.46, p=0.001) and attempt (AOR=1.83, 95% CI=1.41, 2.37, p<0.001); and with progression from ideation to unplanned attempt (AOR=2.03, 95% CI=1.17, 1.74, p<0.001).
Conclusions:
Nicotine dependence exhibited associations with onset of suicidal ideation and suicide attempt—and with progression from ideation to unplanned attempt—that were independent of other measured risk factors. Awareness of associations of nicotine dependence with suicidal behaviors may inform risk assessment, facilitate targeting of prevention efforts, and provide further impetus for reducing nicotine dependence.
INTRODUCTION
Regular tobacco use is associated with suicide mortality,1–4 with some studies finding a dose– response relationship between amount of tobacco use and odds of suicide.2–5 Tobacco use and dependence also exhibit associations with nonfatal suicidal behaviors,6,7 such as suicidal ideation,8–10 plan,10,11 and attempt.8,10,12 An analysis of the proportions of suicide attempts attributable to DSM-IV disorders revealed that nicotine dependence (ND; 8.4%) ranked third behind only major depression (26.6%) and borderline personality disorder (18.1%).13
Mechanisms linking tobacco use and suicidal behavior are incompletely understood; however, mental disorders likely play an important role. Tobacco use and dependence are more prevalent among individuals with psychiatric diagnoses,14 which could explain their relationship with suicidal behavior. Indeed, many studies observe marked attenuation of the associations of tobacco use/dependence with suicidal behavior when controls for mental disorders are applied.1,11,15 On the other hand, neurobiological findings suggest possible direct links between tobacco use and suicidal behavior; for example, via dysregulation of serotonin16 or hypothalamic-pituitary-adrenal axis function.17,18 Tobacco-related physical disease19 and social factors19,20 also may contribute to elevated risks of suicidal behaviors among tobacco users.
Investigations of tobacco use/dependence and suicidal behavior have been conducted primarily in civilian samples, with few studies examining their relationship among military personnel. However, one prospective study of 300,000 male U.S. Army soldiers followed from 1987 to 1996 found a dose–response relationship between amount of tobacco use and suicide risk, with soldiers smoking more than 20 cigarettes daily displaying twice the risk of suicide death compared to nonsmokers.4 The analysis accounted for effects of sociodemographic characteristics and other health behaviors (e.g., drinking, exercise), but not mental disorders. Another study of approximately 4.8 million veterans receiving Veterans Health Administration services during 2005 adjusted for mental disorders and found that ND was associated with 36% increased risk of suicide during follow-up (2006–2008).1 With respect to nonfatal suicidal behaviors, a study of Ohio Army National Guard members found that smoking at baseline predicted suicidal ideation 1 year later, but the association became nonsignificant when depression at follow-up was controlled.21 To the authors’ knowledge, no studies of service members have examined associations of tobacco use or dependence with other nonfatal suicidal behaviors (e.g., attempts).
The availability of tobacco cessation interventions22,23 implies that, if tobacco use/dependence is a contributor to suicidal behavior, it is a modifiable one. Identifying modifiable risk factors for suicidal behavior is critical to efforts to reduce suicide in the Armed Forces,24–26 and constitutes the overarching goal of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS).27,28 The comprehensive assessment of substance use, mental disorders, and other suicide risk factors in the Army STARRS New Solider Study (NSS) affords an opportunity to evaluate the joint associations of these factors with onset and progression of suicidal behaviors. Although the NSS is cross-sectional, retrospective collection of ages of onset enables estimation of effects of antecedent substance use and mental disorders on subsequent suicidal behavior.
The current study evaluates associations of ND with onset of suicidal ideation, plan, and attempt among incoming Army soldiers; and examines the extent to which these associations are impacted by adjustment for childhood adversities and mental disorders that also predated the suicidal behavior. Because predictive effects of tobacco use/dependence on course of suicidal behaviors have rarely been investigated,29 the analysis also evaluates associations of ND with progression from ideation to first onset of plan, from plan to first attempt, and from ideation to first unplanned attempt among respondents with a history of suicidal ideation.
METHODS
Study Population
The Army STARRS NSS27,28,30 was conducted at three U.S. Army installations from April 2011 to November 2012. Representative samples of 200–300 soldiers per site were selected on a weekly basis to attend the NSS overview and informed consent session. This process occurred while soldiers were completing intake procedures prior to Basic Combat Training. Recruitment, informed consent, and data protection procedures were approved by the Human Subjects Committees of all collaborating institutions.
Nearly all (99.9%) selected soldiers consented to the NSS self-administered questionnaire (SAQ) and 93.5% completed it. Most SAQ completers (77.1%) consented to linkage of SAQ data to their Army/Department of Defense records; these 38,507 soldiers comprised the eligible sample for the current study. Analyses incorporated a combined analysis weight that adjusted for differences between SAQ completers who consented to versus refused administrative record linkage; and included post-stratification of consent weights to known demographics and service traits of the population of soldiers attending Basic Combat Training during the study period.31
Person-year data were restricted to ages 12–34 years, resulting in exclusion of 270 respondents with age at enlistment >99th percentile. Participants in an early administration of the NSS survey (n=7,801) also were excluded, because their survey version did not contain all five ND items. The current analysis was therefore based on data from 30,436 new soldiers (4,817 females). Analyses were conducted in 2017–2018.
Measures
ND was assessed using items adapted from the Composite International Diagnostic Interview Screening Scales (CIDI-SC).32 Peak lifetime use of “cigarettes, cigars, pipes, snuff, or smokeless tobacco” was established, and respondents who reported using tobacco products at least 1–2 days a week were assessed for ND. Five yes/no questions evaluated experiences that respondents may have had because of tobacco use at any time of their lives: (1) inability to cut down or cease using tobacco despite efforts to do so, (2) physical symptoms when stopping or reducing tobacco intake, (3) physical symptoms caused by tobacco use, (4) continuing to use tobacco despite physical problems from use, and (5) physical tolerance indicated by the ability to use more tobacco without negative physical effects (e.g., restlessness) that were experienced previously. Lifetime ND was defined as meeting at least two of these criteria. Respondents with lifetime ND specified the age at which they first experienced ND symptoms, as well as the number of months during the past year that ND symptoms were present. Age of onset of ND was used in construction of the person-year dataset for discrete-time survival analysis. Number of months during the past year with ND symptoms was used to classify participants as having ND in sustained remission (0 months) versus past-year ND (>1 month) at the time of survey.
Suicidal behaviors were assessed using an expanded self-report version of the Columbia Suicidal Severity Rating Scale33 that collected ages of onset of suicidal behaviors. Ideation was considered present if respondents reported thoughts of killing themselves, or wishing they were dead or would go to sleep and never wake up. Presence of ideation prompted assessment of intent, and presence of intent prompted questions about plans. Plans were considered present if respondents reported thinking about methods of ending their lives or planning how to kill themselves. All respondents who reported ideation were asked if they had ever attempted suicide. Suicide attempt was defined as purposefully hurting oneself with the intention to die.
Models adjusted for childhood maltreatment, childhood bullying victimization, and parental impairment due to substance use. The first two adversities demonstrated predictive effects on suicidal behaviors in prior studies of the NSS sample34,35 and have been linked to increased risk of tobacco use.36,37 Parental impairment due to substance use was considered another childhood adversity that could be a common cause of ND (via genetic pathways or modeling) and suicidal behaviors.
A prior study described the derivation, via latent profile analysis, of a variable that classified NSS respondents as having experienced no maltreatment; episodic emotional maltreatment; frequent emotional and physical maltreatment; episodic emotional and sexual abuse; or frequent emotional, physical, and sexual maltreatment.34 NSS measures of childhood bullying victimization also were described previously.35 Physical and verbal bullying victimization were quantified separately, using zero to four frequency scales. Parental impairment due to substance use was assessed with the item: During your childhood or adolescence (ages 0–17), how many years was either of your parents (or the people who raised you) so seriously impaired that it interfered with their parenting, work, or other daily activities because of…an alcohol or drug problem? Responses of >1 year were considered indicative of parental impairment due to substance use. Ages at which childhood adversities were experienced were not collected; for the purpose of this analysis they were assumed to have occurred prior to the onset of suicidal behaviors.
Final models adjusted for specific mental disorder diagnoses and total number of mental disorders that predated that suicidal behavior. A prior study described associations of the mental disorder variables with suicidal behaviors in the NSS sample.38 Survey items adapted from the CIDI-SC32 and PTSD Checklist39 were used to assess DSM-IV mental disorders. CIDI-SC/PTSD Checklist diagnoses were validated in the Army STARRS Clinical Reappraisal Study40; these included lifetime major depressive disorder, mania/hypomania, generalized anxiety disorder, panic disorder, post-traumatic stress disorder, intermittent explosive disorder, conduct disorder, oppositional defiant disorder, and alcohol use disorder (AUD) or other substance use disorder (SUD); as well as adult attention deficit-hyperactivity disorder (which was required to be symptomatic during the preceding 6 months for diagnosis). NSS survey assessment of AUD/SUD included questions about lifetime use of alcohol, marijuana/hashish, spice/synthetic cannabinoids, and any other illegal drug; and misuse of prescription stimulants, tranquilizers, and pain relievers. Lifetime problems and dependence symptoms related to use of alcohol or drugs were subsequently queried in order to establish presence of AUD/SUD. Other NSS reports provide data on prevalence of alcohol misuse, drug use, and AUD/SUD in the sample.41,42
Models included time-varying person-year and education; and time-invariant sex, race-ethnicity, religion, parental education, and nativity. Analyses also controlled for service component, site of basic training, and survey version.
Statistical Analysis
Discrete-time survival analysis with person-year as the unit of analysis and a logistic link function43 was used to estimate associations of ND with onset of suicidal ideation, plan, and attempt in the full analysis sample. Additional models were fit among respondents with a history of ideation to examine associations of ND with first onset of plan following ideation (“plan among ideators”), first attempt following ideation with a plan (“planned attempt”), and first attempt following ideation without a plan (“unplanned attempt”). A hierarchy of models were fit to evaluate how adjustment for other risk factors impacted associations of ND with the outcomes. The first set of models adjusted for sociodemographic variables, the second set added adjustment for childhood adversities, and the third set added adjustment for type and number of mental disorders with onset prior to the suicidal behavior in question.
Discrete-time survival coefficients estimated from the logistic model were exponentiated to create ORs with 95% CIs. Because NSS data were clustered and weighted, the design-based Taylor series linearization method was used to estimate SEs. Multivariable significance was examined using design-based Wald chi-square tests. Two-tailed p<0.05 was considered significant. Analyses were conducted using R, version 3.1.3 with the R library survey44 for discrete-time survival models.
RESULTS
Lifetime and past-year ND were reported by 15.5% (SE=0.2%) and 12.2% (SE=0.2%) of soldiers, respectively. Multivariable logistic regression showed that sociodemographic characteristics and childhood adversities were associated with lifetime ND (Table 1). Younger, female, non-white, college educated, and non–U.S.-native soldiers exhibited lower odds of lifetime ND. Soldiers who reported childhood maltreatment, verbal bullying victimization, and parental impairment due to substance use displayed increased risk of ND. Separate models showed that lifetime ND was associated with all lifetime mental disorders assessed in the NSS (Appendix Table 1). Prevalence of 30-day mental disorders was highest among soldiers with past-year ND, intermediate among those with ND in sustained remission, and lowest among those with no lifetime ND at the time of assessment (Figure 1).
Table 1.
Characteristics Associated With Lifetime Nicotine Dependence Among New U.S. Army Soldiers (N=30,436)
| Characteristic | AOR (95% CI) |
|---|---|
| Age (ref: 18–20 years) | |
| 21–23 years | 1.35*** (1.26, 1.44) |
| ≥24 years | 1.48*** (1.34, 1.64) |
| Sex (ref: male) | |
| Female | 0.64*** (0.57, 0.70) |
| Race/ethnicity (ref: white, non-Hispanic) | |
| Black, non-Hispanic | 0.27*** (0.23, 0.31) |
| Hispanic | 0.42*** (0.37, 0.47) |
| Other | 0.74*** (0.63, 0.87) |
| Educational degree (ref: high school) | |
| General equivalency | 0.83** (0.73, 0.94) |
| College | 0.37*** (0.30, 0.45) |
| Nativity (ref: born in U.S.) | |
| Born outside U.S. | 0.71*** (0.59, 0.85) |
| Parents’ education (ref: high school) | |
| Less than high school | 0.89 (0.77, 1.03) |
| College | 1.01 (0.94, 1.08) |
| Childhood maltreatment (ref: none) | |
| Episodic emotional maltreatment | 1.38*** (1.23, 1.55) |
| Frequent emotional and physical maltreatment | 1.89*** (1.61, 2.23) |
| Episodic emotional and sexual abuse | 2.18*** (1.72, 2.78) |
| Frequent emotional, physical, and sexual maltreatment | 2.93*** (2.08, 4.12) |
| Physically bullied during childhood (0–4 rating) | 1.03 (0.99, 1.07) |
| Verbally bullied during childhood (0–4 rating) | 1.10*** (1.08, 1.13) |
| Parent impairment due to substance abuse (reference: none) | 1.33*** (1.21, 1.46) |
Notes: Boldface indicates statistical significance
p<0.05
p<0.01
p<0.001.
Childhood maltreatment profile was derived in a prior study using latent class analysis. Childhood bullying victimization was quantified using 5-point frequency scales [e.g., 0 (never) to 4 (very often)]. The model also adjusted for site of Basic Combat Training and service component (Regular Army, Army Reserve, or Army National Guard).
Figure 1.
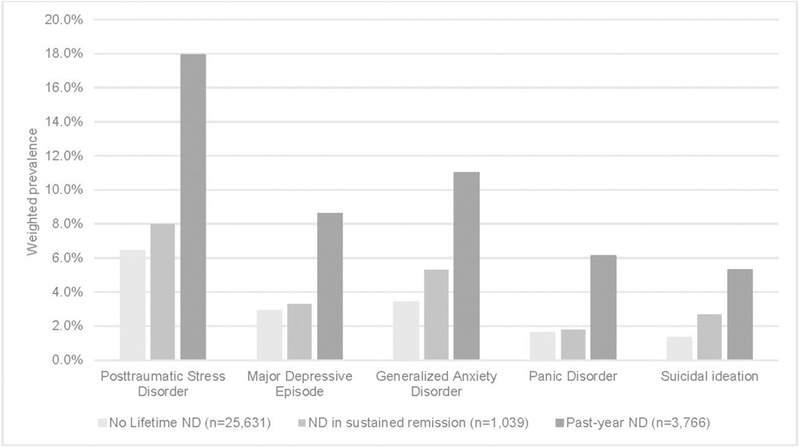
Weighted prevalence of select 30-day mental disorders among new soldiers with past-year ND, ND in sustained remission, and no lifetime history of ND.
Notes: Relative to soldiers with no lifetime ND, and adjusting for sociodemographic variables, soldiers with past-year ND displayed increased odds of all disorders shown [AORs=3.21 (for MDE) to 4.04 (for PD); p<0.001]; and soldiers with remitted ND displayed elevated odds of PTSD, GAD, and suicidal ideation [AORs=1.47 (for PTSD) to 2.15 (for suicidal ideation); p<0.05] but not MDE or PD (p>0.15). SEs for prevalence estimates ranged from 0.1% to 0.2% in the group with no lifetime ND; from 0.4% to 0.9% in the group with remitted ND; and from 0.5% to 0.7% in the group with past-year ND.
ND, nicotine dependence; MDE, major depressive episode; PD, panic disorder; PTSD, posttraumatic stress disorder; GAD, generalized anxiety disorder.
Appendix Tables 2–4 show ND and suicidal ideation, plan, and attempt by age of onset. Discrete-time survival analysis adjusting for sociodemographic characteristics (Table 2; Model 1) revealed associations between ND and onset of suicidal ideation (AOR=2.07, 95% CI=1.83, 2.34, chi-square (1), 131.17, p<0.001), suicide plan (AOR=2.67, 95% CI=2.12, 3.36, chi-square (1), 70.05, p<0.001), and suicide attempt (AOR=4.08, 95% CI=3.25, 5.13, chi-square (1), 144.70, p<0.001). Models of the progression of suicidal behaviors showed that when ideation was present, ND was associated with onset of plans (AOR=1.48, 95% CI=1.14, 1.90, chi-square (1), 8.88, p=0.003); and when plans were present, ND was associated with attempts (planned attempts; AOR=1.85, 95% CI=1.22, 2.79, chi-square (1), 8.45, p=0.004). ND also predicted attempts among ideators who denied suicide plans (unplanned attempts; AOR=2.44, 95% CI=1.65, 3.59, chi-square (1), 20.34, p<0.001).
Table 2.
Associations of Nicotine Dependence With Suicidal Behaviors, Adjusting for Sociodemographics (All Models), Childhood Adversities (Models 2 and 3), and Mental Disorders (Model 3)
| Onset of suicidal behaviors among all respondents (N=30,436) |
Progression of suicidal behaviors among ideators | |||||
|---|---|---|---|---|---|---|
| Predictor of interest |
Ideation, AOR (95% CI) |
Plan, AOR (95% CI) |
Attempt, AOR (95% CI) |
Plan (n=4060), AOR (95% CI) |
Planned attempt (n=625), AOR (95% CI) |
Unplanned attempt (n=3519), AOR (95% CI) |
| Nicotine dependence (Model 1) |
2.07*** (1.83, 2.34) |
2.67*** (2.12, 3.36) |
4.08*** (3.25, 5.13) |
1.48** (1.14, 1.90) |
1.85** (1.22, 2.79) |
2.44*** (1.65, 3.59) |
| Nicotine dependence (Model 2) |
1.65*** (1.44, 1.90) |
1.85*** (1.44, 2.38) |
2.84*** (2.22, 3.64) |
1.36* (1.05, 1.76) |
1.70* (1.11, 2.59) |
2.32*** (1.57, 3.45) |
| Nicotine dependence (Model 3) |
1.27** (1.10, 1.46) |
1.17 (0.87, 1.56) |
1.83*** (1.41, 2.37) |
0.99 (0.72, 1.36) |
1.36 (0.89, 2.08) |
2.03*** (1.36, 3.03) |
Notes: Boldface indicates statistical significance
p<0.05
p<0.01
p<0.001.
AORs are from discrete-time survival analysis of suicidal behavior outcomes (listed in column headers), where nicotine dependence was the predictor of interest and increasing controls for other risk factors were applied in Models 1 through 3. Model 1 adjusted for person-year, sex, race/ethnicity, religion, soldier and parental education, nativity, service component, site of Basic Combat Training, and survey version. Model 2 adjusted for all of the variables included in Model 1, plus childhood adversities (maltreatment, bullying victimization [physical and verbal], and parental substance abuse). Model 3 adjusted for all of the variables included in Model 2, plus major depressive episode, mania/hypomania, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, intermittent explosive disorder, conduct disorder, oppositional defiant disorder, substance use disorder, and persistent attention deficit-hyperactivity disorder that predated the suicidal behavior; as well as number of mental disorders that predated the suicidal behavior.
Adjustment for childhood adversities attenuated the associations of ND with suicidal behaviors, but all remained statistically significant (Table 2; Model 2). Adjustment for mental disorders further weakened associations of ND with the outcomes (Table 2; Model 3); however, ND remained significantly associated with onset of ideation (AOR=1.27, 95% CI=1.10, 1.46, chi-square (1), 10.97, p=0.001) and attempt (AOR=1.83, 95% CI=1.41, 2.37, chi-square (1), 20.68, p<0.001), and with progression from ideation to unplanned attempt (AOR=2.03, 95% CI=1.36, 3.03, chi-square (1), 12.15, p<0.001).
DISCUSSION
Nicotine dependence was associated with onset and progression of suicidal behavior among incoming U.S. Army soldiers. Elevated risks among those with ND were partly explained by co-occurring childhood adversities and mental disorders that also predated the suicidal behavior. Yet the current analysis also revealed associations of ND with suicidal behaviors that were independent of those factors.
In the overall population of new soldiers, adjusting for other risk factors, ND was associated with 27% increased risk of suicidal ideation and, more strikingly, with nearly twice the risk of suicide attempt. These findings imply that detection of ND could be valuable in assessing risk of suicidal behavior among young adults, including those who enlist in the Armed Forces. The present study did not evaluate associations of ND with onset of suicidal behavior after enlistment. Additional investigation is needed to determine whether ND during service predicts onset or worsening of suicidal behavior during specific Army career stages or transitions (e.g., deployment). As follow-up data become available, future Army STARRS studies will address these questions.
In terms of progression of suicidal behavior, ND was associated with twice the risk of unplanned attempt among soldiers with a history of ideation. This finding may relate to evidence that cigarette smoking is prospectively associated with suicidal acts among patients with mood disorders.45,46 Further investigation aimed at clarifying the relationship of ND with progression of suicidal behavior is warranted, given its potential to inform clinical risk assessment of patients presenting with thoughts of suicide. It is notable that, although ND predicted progression from ideation to unplanned suicide attempt, it was not associated with the transition from plan to attempt. Future research could investigate the possibility that ND produces symptoms (e.g., irritability/agitation)47 that specifically increase risk of unplanned suicide attempt.
In general, observation of strong associations of ND with suicide attempts in the presence of stringent controls for other risk factors offers justification for continued investigation of possible causal links between these behaviors. Neurotransmitters and brain regions involved in stress response and mood regulation are impacted by acute nicotine administration, long-term use of nicotine, and withdrawal from nicotine.18 A thorough consideration of the neurobiological literature is beyond the scope of this discussion; however, it is notable that prolonged nicotine use reduces serotonin, an effect that could increase vulnerability to acting on suicidal thoughts.16 Activation or dysregulation of the hypothalamic-pituitary-adrenal axis by nicotine17,18 also may be implicated in suicidal behavior among tobacco users.
The results of this study converge with other evidence11,15,21 that co-occurring mental disorders contribute to the associations of tobacco use and dependence with suicidal behaviors. High comorbidity of ND with mental disorders was observed, and associations of ND with all suicidal behavior outcomes diminished when controls for mental disorders were applied. The current analysis did not estimate the proportion of the gross association of ND with each suicidal behavior that was mediated through mental disorders. Investigation of mediational relationships among ND, specific mental disorders, and suicidal behaviors is a valuable direction for future research.
Finally, descriptive data showed that soldiers in sustained remission from ND had substantially lower prevalence of 30-day mental disorders than those with past-year ND; and in some cases, did not differ significantly from those with no lifetime ND. Previous studies have found that risk of suicidal behavior is greatly magnified among those with active versus remitted tobacco use/dependence,9,12 and that tobacco users who achieve long-term abstinence have improved mental health outcomes relative to those whose dependence persists.48 These observations raise the possibility that risk of suicidal behavior may be mitigated if sustained remission of ND can be achieved. Further evidence of salutary effects of tobacco cessation on suicidal behavior (e.g., from intervention studies) would support targeting ND within Army suicide risk mitigation programs.
Limitations
Self-report data are vulnerable to recall and reporting biases. Underreporting is a concern when respondents are asked about substance use, mental disorders, and suicidal behavior. NSS data are cross-sectional; and conclusions that ND relates to onset or progression of suicidal behavior are based on respondents’ retrospective reports of symptoms and ages at which those symptoms first occurred. Although models adjusted for a wide range of mental disorders and childhood adversities, it is possible that unmeasured variables (e.g., psychotic disorders, personality disorders49) explain the seemingly independent associations of ND with suicidal behaviors. Finally, correlates of nonfatal suicidal behaviors may differ from those of suicide mortality.25 Thus, although identifying risk factors for nonfatal suicidal behaviors is important, it does not necessarily improve understanding of factors that contribute to suicide death.
CONCLUSIONS
Lifetime ND was common among new soldiers and associated with sociodemographic characteristics, childhood adversities, and mental disorders. Associations of ND with onset and progression of suicidal behaviors were to varying extents accounted for by co-occurring risk factors, such as childhood maltreatment and mental disorders. However, ND was independently associated with onset of suicidal ideation and suicide attempt among all soldiers, and with unplanned attempts among those with a history of ideation. Awareness of relationships of ND with suicidal behaviors may inform risk assessment and targeting of suicide prevention programs. The findings reinforce the importance of preventing ND; and imply that the military’s efforts to reduce tobacco use23 may benefit the mental as well as physical well-being of service members.
Supplementary Material
ACKNOWLEDGMENTS
The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Team consists of co-principal investigators Robert J. Ursano, MD (Uniformed Services University of the Health Sciences) and Murray B. Stein, MD, MPH (University of California San Diego and VA San Diego Healthcare System); site principal investigators: Steven Heeringa, PhD (University of Michigan), James Wagner, PhD (University of Michigan), and Ronald C. Kessler, PhD (Harvard Medical School); Army liaison/consultant: Kenneth Cox, MD, MPH (US Army Public Health Center); and other team members: Pablo A. Aliaga, MA (Uniformed Services University of the Health Sciences); COL David M. Benedek, MD (Uniformed Services University of the Health Sciences); Laura Campbell-Sills, PhD (University of California San Diego); Carol S. Fullerton, PhD (Uniformed Services University of the Health Sciences); Nancy Gebler, MA (University of Michigan); Robert K. Gifford, PhD (Uniformed Services University of the Health Sciences); Paul E. Hurwitz, MPH (Uniformed Services University of the Health Sciences); Sonia Jain, PhD (University of California San Diego); Tzu-Cheg Kao, PhD (Uniformed Services University of the Health Sciences); Lisa Lewandowski-Romps, PhD (University of Michigan); Holly Herberman Mash, PhD (Uniformed Services University of the Health Sciences); James E. McCarroll, PhD, MPH (Uniformed Services University of the Health Sciences); James A. Naifeh, PhD (Uniformed Services University of the Health Sciences); Tsz Hin Hinz Ng, MPH (Uniformed Services University of the Health Sciences); Matthew K. Nock, PhD (Harvard University); Nancy A. Sampson, BA (Harvard Medical School); CDR Patcho Santiago, MD, MPH (Uniformed Services University of the Health Sciences); LTC Gary H. Wynn, MD (Uniformed Services University of the Health Sciences); and Alan M. Zaslavsky, PhD (Harvard Medical School).
Contents are solely the responsibility of the authors and do not necessarily represent the views of HHS, National Institute of Mental Health (NIMH), the Department of the Army, the Department of Veterans Affairs, or the Department of Defense.
Army STARRS was sponsored by the Department of the Army and funded under cooperative agreement number U01MH087981 (2009–2015) with HHS, NIH, NIMH (NIH/NIMH). Subsequently, STARRS-LS was sponsored and funded by the Department of Defense (USUHS grant number HU0001-15-2-0004). As a cooperative agreement, scientists employed by the NIMH and U.S. Army liaisons and consultants collaborated to develop the study protocol and data collection instruments, supervise data collection, interpret results, and prepare reports. Although a draft of the manuscript was submitted to the Army for review and comment prior to submission, this was done with the understanding that comments would be no more than advisory.
Dr. Stein has in the past 3 years been a consultant for Actelion, Aptinyx, Bionomics, Dart Neuroscience, Healthcare Management Technologies, Janssen, Oxeia Biopharmaceuticals, Pfizer, and Resilience Therapeutics. In the past 3 years, Dr. Kessler received support for his epidemiologic studies from Sanofi Aventis; was a consultant for Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Kessler is a co-owner of DataStat, Inc., a market research firm that carries out healthcare research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
None of the contents of this article have been presented elsewhere.
No other financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Bohnert KM, Ilgen MA, McCarthy JF, Ignacio RV, Blow FC, Katz IR. Tobacco use disorder and the risk of suicide mortality. Addiction 2014;109(1):155–162. 10.1111/add.12381. [DOI] [PubMed] [Google Scholar]
- 2.Evins AE, Korhonen T, Kinnunen TH, Kaprio J. Prospective association between tobacco smoking and death by suicide: a competing risks hazard analysis in a large twin cohort with 35-year follow-up. Psychol Med 2017;47(12):2143–2154. 10.1017/S0033291717000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lucas M, O’Reilly EJ, Mirzaei F, et al. Cigarette smoking and completed suicide: results from 3 prospective cohorts of American adults. J Affect Disord 2013;151(3):1053–1058. 10.1016/j.jad.2013.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller M, Hemenway D, Bell NS, Yore MM, Amoroso PJ. Cigarette smoking and suicide: a prospective study of 300,000 male active-duty Army soldiers. Am J Epidemiol 2000;151(11):1060–1063. 10.1093/oxfordjournals.aje.a010148. [DOI] [PubMed] [Google Scholar]
- 5.Li D, Yang X, Ge Z, et al. Cigarette smoking and risk of completed suicide: a meta-analysis of prospective cohort studies. J Psychiatr Res 2012;46(10):1257–1266. 10.1016/j.jpsychires.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Poorolajal J, Darvishi N. Smoking and suicide: a meta-analysis. PLoS ONE 2016;11(7):e0156348 10.1371/journal.pone.0156348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC. Smoking and the risk of suicidal behavior: a prospective study of a community sample. Arch Gen Psychiatry 2005;62(3):328–34. 10.1001/archpsyc.62.3.328. [DOI] [PubMed] [Google Scholar]
- 8.Bronisch T, Hofler M, Lieb R. Smoking predicts suicidality: findings from a prospective community study. J Affect Disord 2008;108(1–2):135–145. 10.1016/j.jad.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Clarke DE, Eaton WW, Petronis KR, Ko JY, Chatterjee A, Anthony JC. Increased risk of suicidal ideation in smokers and former smokers compared to never smokers: evidence from the Baltimore ECA follow-up study. Suicide Life Threat Behav 2010;40(4):307–318. 10.1521/suli.2010.40.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han B, Compton WM, Blanco C. Tobacco use and 12-month suicidality among adults in the United States. Nicotine Tob Res 2017;19(1):39–48. 10.1093/ntr/ntw136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler RC, Borges G, Sampson N, Miller M, Nock MK. The association between smoking and subsequent suicide-related outcomes in the National Comorbidity Survey panel sample. Mol Psychiatry 2009;14(12):1132–1142. 10.1038/mp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yaworski D, Robinson J, Sareen J, Bolton JM. The relation between nicotine dependence and suicide attempts in the general population. Can J Psychiatry 2011;56(3):161–170. 10.1177/070674371105600306. [DOI] [PubMed] [Google Scholar]
- 13.Bolton JM, Robinson J. Population-attributable fractions of Axis I and Axis II mental disorders for suicide attempts: findings from a representative sample of the adult, noninstitutionalized U.S. population. Am J Public Health 2010;100(12):2473–2480. 10.2105/AJPH.2010.192252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith PH, Mazure CM, McKee SA. Smoking and mental illness in the U.S. population. Tob Control 2014;23(e2):e147–e153. 10.1136/tobaccocontrol-2013-051466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Berglund PA, Borges G, et al. Smoking and suicidal behaviors in the National Comorbidity Survey: Replication. J Nerv Ment Dis 2007;195(5):369–377. 10.1097/NMD.0b013e3180303eb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malone KM, Waternaux C, Haas GL, Cooper TB, Li S, Mann JJ. Cigarette smoking, suicidal behavior, and serotonin function in major psychiatric disorders. Am J Psychiatry 2003;160(4):773–779. 10.1176/appi.ajp.160.4.773. [DOI] [PubMed] [Google Scholar]
- 17.Rohleder N, Kirschbaum C. The hypothalamic-pituitary-adrenal (HPA) axis in habitual smokers. Int J Psychophysiol 2006;59(3):236–243. 10.1016/j.ijpsycho.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 18.Richards JM, Stipelman BA, Bornovalova MA, Daughters SB, Sinha R, Lejuez CW. Biological mechanisms underlying the relationship between stress and smoking: state of the science and directions for future work. Biol Psychol 2011;88(1):1–12. 10.1016/j.biopsycho.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green M, Turner S, Sareen J. Smoking and suicide: biological and social evidence and causal mechanisms. J Epidemiol Community Health 2017;71(9):839–840. 10.1136/jech-2016-207731. [DOI] [PubMed] [Google Scholar]
- 20.Talati A, Wickramaratne PJ, Keyes KM, Hasin DS, Levin FR, Weissman MM. Smoking and psychopathology increasingly associated in recent birth cohorts. Drug Alcohol Depend 2013;133(2):724–732. 10.1016/j.drugalcdep.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodwin RD, Prescott MR, Tamburrino M, Calabrese JR, Liberzon I, Galea S. Cigarette smoking and subsequent risk of suicidal ideation among National Guard soldiers. J Affect Disord 2013;145(1):111–114. 10.1016/j.jad.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med 2008;35(2):158–176. 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith EA, Poston WS, Haddock CK, Malone RE. Installation tobacco control programs in the U.S. military. Mil Med 2016;181(6):596–601. 10.7205/MILMED-D-15-00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuehn BM. Soldier suicide rates continue to rise: military, scientists work to stem the tide. JAMA 2009;301(11):1111, 1113. 10.1001/jama.2009.342. [DOI] [PubMed] [Google Scholar]
- 25.Nock MK, Deming CA, Fullerton CS, et al. Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry 2013;76(2):97–125. 10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ressler KJ, Schoomaker EB. Commentary on ―The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS)‖: Army STARRS: a Framingham-like study of psychological health risk factors in soldiers. Psychiatry 2014;77(2):120–129. 10.1521/psyc.2014.77.2.120. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Colpe LJ, Fullerton CS, et al. Design of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res 2013;22(4):267–275. 10.1002/mpr.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ursano RJ, Colpe LJ, Heeringa SG, et al. The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Psychiatry 2014;77(2):107–119. 10.1521/psyc.2014.77.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi SB, Lee W, Yoon JH, Won JU, Kim DW. Risk factors of suicide attempt among people with suicidal ideation in South Korea: a cross-sectional study. BMC Public Health 2017;17(1):579 10.1186/s12889-017-4491-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heeringa SG, Gebler N, Colpe LJ, et al. Field procedures in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res 2013;22(4):276–287. 10.1002/mpr.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Heeringa SG, Colpe LJ, et al. Response bias, weighting adjustments, and design effects in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res 2013;22(4):288–302. 10.1002/mpr.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13(2):93–121. 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011;168(12):1266–1277. 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stein MB, Campbell-Sills L, Ursano RJ, et al. Childhood maltreatment and lifetime suicidal behaviors among new soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). J Clin Psychiatry 2018;79(2):70–77. 10.4088/JCP.16m10900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campbell-Sills L, Kessler RC, Ursano RJ, et al. Associations of childhood bullying victimization with lifetime suicidal behaviors among new U.S. Army soldiers. Depress Anxiety 2017;34(8):701–710. 10.1002/da.22621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moore SE, Norman RE, Suetani S, Thomas HJ, Sly PD, Scott JG. Consequences of bullying victimization in childhood and adolescence: a systematic review and meta-analysis. World J Psychiatry 2017;7(1):60–76. 10.5498/wjp.v7.i1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 1999;282(17):1652–1658. 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 38.Nock MK, Ursano RJ, Heeringa SG, et al. Mental disorders, comorbidity, and pre-enlistment suicidal behavior among new soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Suicide Life Threat Behav 2015;45(5):588–599. 10.1111/sltb.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at: Annual Convention of the International Society for Traumatic Stress Studies, 1993; San Antonio, TX. [Google Scholar]
- 40.Kessler RC, Santiago PN, Colpe LJ, et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res 2013;22(4):303–321. 10.1002/mpr.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stein MB, Campbell-Sills L, Gelernter J, et al. Alcohol misuse and co-occurring mental disorders among new soldiers in the U.S. Army. Alcohol Clin Exp Res 2017;41(1):139–148. 10.1111/acer.13269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosellini AJ, Heeringa SG, Stein MB, et al. Lifetime prevalence of DSM-IV mental disorders among new soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Depress Anxiety 2015;32(1):13–24. 10.1002/da.22316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Efron B Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc 1988;83:414–425. 10.1080/01621459.1988.10478612. [DOI] [Google Scholar]
- 44.Lumley T Analysis of complex survey samples. J Stat Softw 2004;9:1–19. 10.18637/jss.v009.i08. [DOI] [Google Scholar]
- 45.Oquendo MA, Galfalvy H, Russo S, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry 2004;161(8):1433–1441. 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 46.Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, et al. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. Am J Psychiatry 2007;164(1):134–141. 10.1176/ajp.2007.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ribeiro JD, Bender TW, Buchman JM, et al. An investigation of the interactive effects of the capability for suicide and acute agitation on suicidality in a military sample. Depress Anxiety 2015;32(1):25–31. 10.1002/da.22240. [DOI] [PubMed] [Google Scholar]
- 48.Donald S, Chartrand H, Bolton JM. The relationship between nicotine cessation and mental disorders in a nationally representative sample. J Psychiatr Res 2013;47(11):1673–1679. 10.1016/j.jpsychires.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 49.Bachynski KE, Canham-Chervak M, Black SA, Dada EO, Millikan AM, Jones BH. Mental health risk factors for suicides in the U.S. Army, 2007–8. Inj Prev 2012;18(6):405–412. 10.1136/injuryprev-2011-040112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


