Abstract
Background:
Photophobia is commonly associated with migraine, meningitis, concussion, and a variety of ocular diseases. Advances in our ability to trace multiple brain pathways through which light information is processed have paved the way to a better understanding of the neurobiology of photophobia and the complexity of the symptoms triggered by light.
Purpose:
The purpose of this review is to summarize recent anatomical and physiological studies on the neurobiology of photophobia with emphasis on migraine.
Recent findings:
Observations made in blind and seeing migraine patients, and in a variety of animal models, have led to the discovery of a novel retino-thalamo-cortical pathway that carries photic signal from melanopsinergic and non-melanopsinergic retinal ganglion cells to thalamic neurons. Activity of these neurons is driven by migraine and their axonal projections convey signals about headache and light to multiple cortical areas involved in the generation of common migraine symptoms. Novel projections of retinal ganglion cells into previously unidentified hypothalamic neurons that regulate parasympathetic and sympathetic functions have also been discovered. Finally, recent work has led to a novel understanding of color preference in migraine-type photophobia and of the roles played by the retina, thalamus and cortex.
Summary:
The findings provide a neural substrate for understanding the complexity of aversion to light in patients with migraine and neuro-ophthalmologic other disorders.
Keywords: Migraine, headache, trigeminovascular, melanopsin, hypothalamus, thalamus, visual cortex, sympathetic, parasympathetic, rods, cones, retina
INTRODUCTION
Photophobia is commonly associated with anterior segment disorders of the eye such as uveitis, cyclitis, iritis, and blepharitis [1]. Intracranial pathologies such as migraine, meningitis, subdural hemorrhage, and intracranial tumors are also associated with photophobia [2–5]. There are at least three distinct definitions of photophobia in the literature: (1) abnormal sensitivity to light [1]; (2) ocular discomfort, also termed photo-oculodynia, [6]; (3) exacerbation of headache by light [7–9]; and (4) our recent proposal to define photophobia more broadly: general aversion to light [10].
Neural pathways that meditate aversion to light differ greatly from neural pathways that mediate exacerbation of headache by light in migraineurs or from neural pathways that mediate ocular discomfort. To alter visual perception during migraine, it is reasonable to propose that a flow of nociceptive signals along the trigeminovascular pathway converges on visual pathways that terminate in the visual cortex. Conversely, to alter the perception of headache during exposure to light, it is reasonable to propose that a flow of photic signals converge on nociceptive trigeminovascular pathways that terminate in cortical areas are involved in the processing of pain perception. To induce ocular discomfort or pain in the eye by light, it is likely that light indirectly activates intraocular trigeminal nociceptors; these, in turn, activate second-order nociceptive neurons in the spinal trigeminal nucleus. To induce general aversion to light, it is reasonable to propose that light alters the activity of neural pathways that regulate affect and autonomic functions.
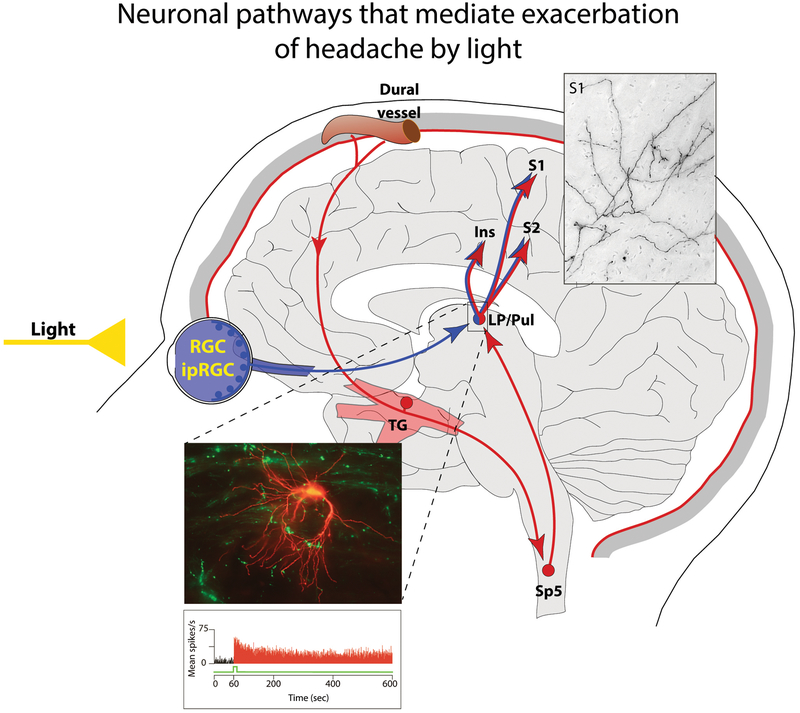
Neural pathways that mediate exacerbation of headache by light
Because the headache phase of migraine depends on flow of nociceptive signals that originate in meningeal nociceptors and are conveyed to the cortex through central trigeminovascular neurons in the spinal trigeminal nucleus and thalamus, it is reasonable to assume that the intensification of headache by light involves a cross-talk between brain pathways that process vision and those responsible for the classical pain of migraine headache. The first site in which such cross-talk may occur was identified in 2010. Using sophisticated anatomical, electrophysiological and immunohistological techniques, Noseda and colleagues [7] showed in animals that: (a) light enhances the activity of thalamic trigeminovascular neurons in a manner that resembles the way light activates melanopsinergic retinal ganglion cells (RGC); (b) a subset of dura-sensitive thalamic neurons, located mainly in the posterior most area of the thalamus, receive monosynaptic input from axons of melanopsinergic and non-melanopsinergic RGC that travel from the eye to the brain along the optic nerve; and (c) the axons of these dura-sensitive thalamic neurons, whose activity is enhanced by light, project to primary and secondary somatosensory cortices and the insula. These structures constitute the so-called pain matrix [7]. The unraveling of a pathway that carries photic signals to cortical areas where the perception of headache and its intensity are generated (Fig. 1) define a mechanism for the exacerbation of migraine headache by light.
Figure 1.
Neuronal pathways that mediate exacerbation of headache by light. Proposed mechanism for exacerbation of migraine headache by light through the convergence of the photic signals from the retina and nociceptive signals from the meninges on the same thalamic neurons that project to the somatosensory cortices. Red depicts the trigeminovascular pathway. Blue depicts visual pathway from the retina to the posterior thalamus. Inserts show distribution of trigeminovascular axons in the somatosensory cortex (top-right), monosynaptic connections between axons of RGC and dendrites of thalamic trigeminovascular neurons (bottom-left) and light effect on activation pattern of a thalamic trigeminovascular neuron (bottom-left). Abbreviations: RGC, retinal ganglion cells; ipRGC, intrinsically-photosensitive retinal ganglion cells; TG, trigeminal ganglion; Sp5, spinal trigeminal nucleus; LP, lateral posterior nucleus; Pul, pulvinar; S1, primary somatosensory cortex; S2 secondary somatosensory cortex. Adapted from [7,14,50,51]
Critical confirmation of the role of the posterior thalamus in the exacerbation of migraine headache by light was provided in an earlier study. In that investigation, sophisticated neuroimaging and in vivo electrophysiology techniques were used to demonstrate that the posterior thalamic nuclei contain large number of neurons that initially become active during migraine in patients (i.e., in the pulvinar). These neurons (i.e., in the posterior and lateral posterior nuclei) also activate in response to stimulation of the dura in animals and become sensitized [11] - to the extent that their sensitization can mediate the whole-body allodynia of migraine [12]. Additional support for the existence in humans of a direct retino-pulvinar projection has been provided in another study in which diffusion weighted imaging and probabilistic tractography were employed to map connectivity of direct pathways from the optic nerve to the pulvinar [13].
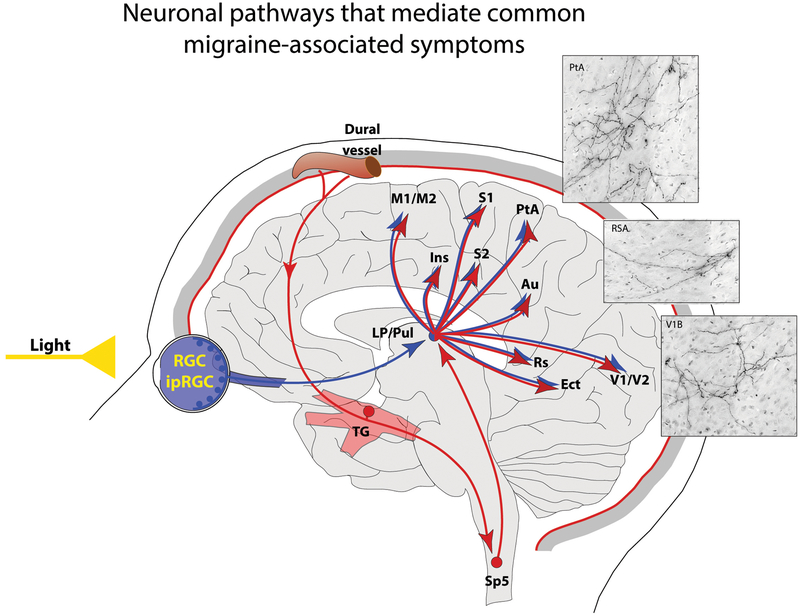
Neuronal pathways that mediate common migraine-associated symptoms
The massive projections of axons of dura- and light-sensitive thalamic neurons into visual, auditory and olfactory cortices, as well as to the motor, retrosplenial, and parietal association cortices [7,14], define distinct neuroanatomical pathways through which exposure to light during migraine can bombard these cortices with overwhelming number of signals capable of altering the normal functioning of these cortical areas. These signals, in turn, can give rise to a variety of symptoms that appear in association with the migraine experience (Fig. 2). Symptoms include compromised cognitive functions and transient decline in short-term memory, partially attributed to altered function of the retrosplenial cortex [15]; impaired motor coordination, partially attributed to the altered function of the motor cortex [16]; transient decline in ability to maintain attention, partially attributed to altered functions of the parietal association cortex [17]; abnormal perception of light, color and visual images, attributed mainly to altered processing in primary and secondary visual cortices [18,19]; and enhanced sensitivity to sound and smell, attributed to abnormal processing of auditory and olfactory stimuli by the auditory and olfactory cortices [20–22].
Figure 2.
Neuronal pathways that mediate common migraine associated symptoms. Proposed mechanism for initiation or exacerbation of common migraine-associated symptoms by light during migraine through convergence of nociceptive signals from the meninges on thalamic neurons that project to the motor (M), parietal association (PtA), auditory (Au), retro-splenius (RS), olfactory (ECT) and visual (V) cortices. Inserts (top-right) show distribution of trigeminovascular axons in the parietal association, retro-splenius and visual cortices. Red depicts the trigeminovascular pathway. Blue depicts visual pathway from the retina to the visual cortex. Additional Abbreviations: as in Fig. 1). Adapted from [7,14,50,51]
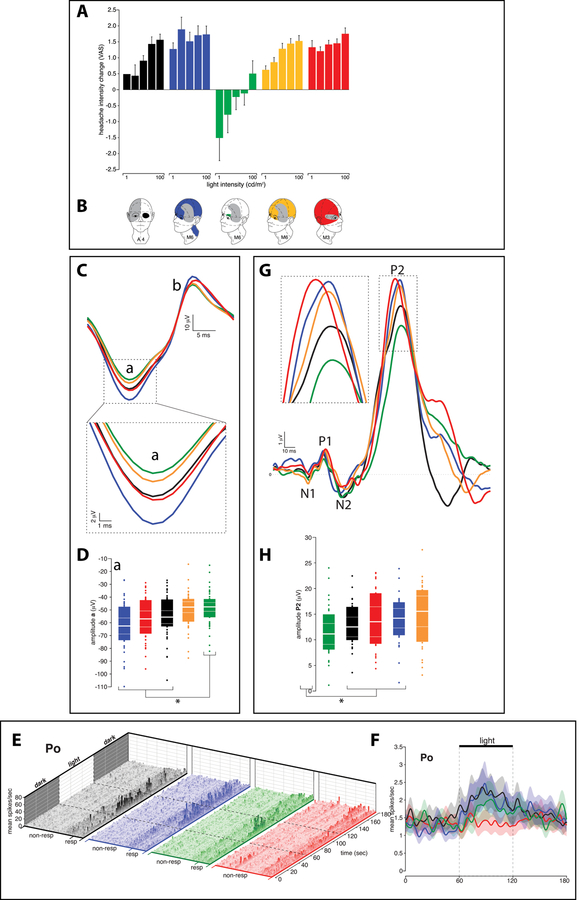
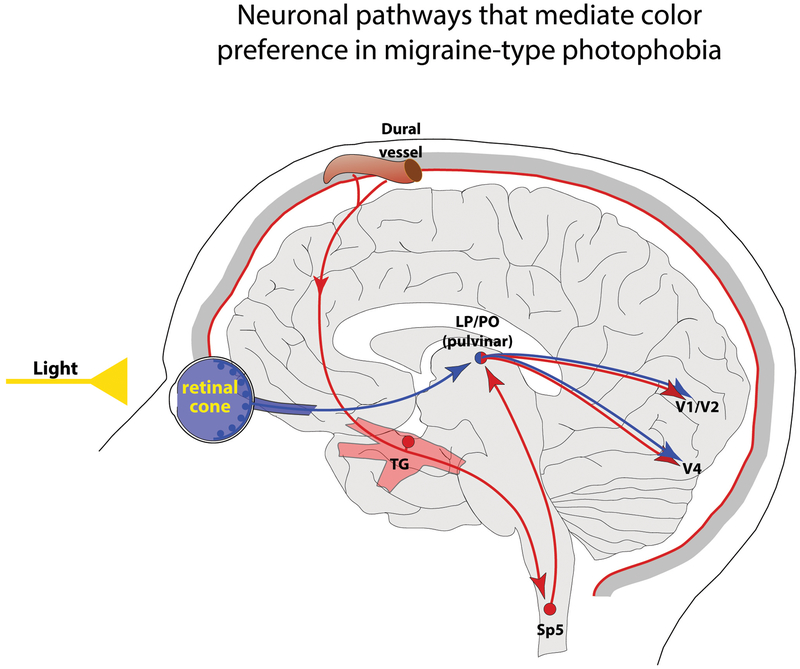
Neuronal pathways that mediate color preference in migraine patients
We originally reported that a ‘non-image forming’ pathway, which originates in melanopsinergic RGC, can explain the preferential sensitivity to blue light in blind migraine patients, who, in spite of losing the ability to form images due to degeneration of cones and rods [23] can still detect light [7]. These findings suggested that blue light could be fundamental to migraine-type photophobia and that the exacerbation of the headache by light could be minimized by devices (sunglasses, contact lens) that block the blue light [24–27]. However, a recent, carefully-designed, psychophysical study conducted in migraine patients with normal eyesight [28] revealed that, during the ictal phase, white, blue, amber, and red light exacerbates migraine headache almost equally and significantly more than green light (Fig. 3A). Using electroretinography and visual evoked potential recordings in patients, and multi-unit recording of dura- and light-sensitive thalamic neurons in rats, this same study showed that green light activates cone-driven retinal pathways to a lesser extent than white, blue and red (Fig. 3C–D). It also demonstrated that thalamic neurons are most responsive to blue and least responsive to green (Fig. 3E–F), and that cortical responses to blue, amber and red lights are significantly larger than those generated by green light (Fig. 3G–H). These findings define a novel concept in migraine-type photophobia whereby color selectivity and its effects on the severity of migraine-type photophobia appear to originate in cone-driven retinal pathways. These are fine-tuned and preserved in relay thalamic neurons outside the main visual pathway, and are eventually converted into perception by the visual cortex (Fig. 4). This interpretation is based on strong data that support the view that color processing involves cone but not rod photoreceptors, retinal ganglion cells, relay neurons in the lateral geniculate nucleus (LGN), the primary (V1), secondary (V2) visual cortices, and parts of the inferior temporal lobe (V4). To perceive color correctly, the brain needs to receive (and compare) signals that originate in 2 different classes of cones located in the same area of the retina. Signals originating in different classes of cones (i.e., red-green, blue-yellow) activate cone-opponent retinal ganglion cells whose axons project to the LGN, and relay LGN cells whose axons terminate in the visual cortex. Signals arriving in V1 from different classes of cone-opponent cells activate double-opponent neurons [19,29] whose role is to establish the neural basis of color contrast, color constancy, poor spatial resolution of color vision, and overall color encoding [30–35]. In V1, color encoding cells, which are clustered within blobs [36,37], project to distinct stripes in V2, that in turn convey color signals to the inferior and posterior inferior temporal cortex. This is where the human brain can generate the perception of millions of different colors [29]. Supporting the proposal that V1, V2 and the inferior temporal cortex are involved in the generation of color-selectivity among migraine patients are studies showing different or simply greater patterns of activation signal in the LGN [38], visual cortex [38–43], and temporal lobes [44,45] of migraine patients as compared to control subjects.
Figure 3.
Proposed mechanism for color preference in migraine-type photophobia. A-B. Effects of color on pain rating and headache location. C. Chromatic electroretinographies (ERGs) recorded in 43 migraine patients. Shown in the figure are superimposed means of standard light-adapted 30 Hz flickering ERG waveforms averaged (± SEM) across patients in response to each color of light. These light-adapted flickering ERG waveforms illustrate that blue, red and white lights generated significantly larger a-wave amplitudes as compared to green light (enlarged view in inset) (p<0.0001). D. Boxplot illustrating median, 95% CI, interquartile range, and observations below and above the 25th and 75th percentile, respectively. Asterisks depict the significantly greater a-wave amplitude induced by blue, red and white lights compared to green. E. 3D bar graphs illustrating firing frequency (i.e., raw data expressed in mean spikes/sec, bin size=1 sec) of 37 posterior hypothalamus neurons to 44, 59, 58 and 59 cycles (dark-light-dark, 1-min each) of photic retinal stimulation with white, blue, green and red lights, respectively. Neurons whose activity in the light increased by >2SD over baseline (i.e., in the dark), are marked as responders (resp) and shown on the right side of each collections of color-selective bar graphs. The data were collected using sophisticated 3-tetrode in vivo multi-unit recording technique. F. Differential responses of trigeminovascular and non-trigeminovascular thalamic neurons to photic stimulation with white, blue, green and red lights. G. Chromatic visual evoked potentials (VEPs) recorded in 28 migraine patients. Shown in the figure are superimposed means of standard flash VEP waveforms averaged (± SEM) across patients in response to 1,792 flashes (64 flashes per patient, 1 s inter-stimulus interval) of each color of light. The superimposed means of these flash VEPs demonstrate that blue, red and amber generated significantly larger P2 amplitude (enlarged view in inset) as compared to green (p<0.02). In contrast, no differences were found in the amplitudes of the N2 waves. H. Boxplot illustrating median (thick horizontal white line), 95% CI (thin dotted horizontal lines), interquartile range (25th-75th percentile; lower and upper box boundaries) and observations below and above the 25th and 75th percentile, respectively (individual dots). Asterisk depicts the significantly smaller P2-wave amplitude induced by the green light compared to red, blue and amber.
Adapted from [28].
Figure 4.
Neuronal pathways that mediate color preference in migraine-type photophobia. Such pathways involve sequential activation of cone photoreceptors, post-cone retinal pathways, cone-opponent retinal ganglion cells, relauy posterior thalamic neurons (located in the pulvinar, lateral posterior and posterior nuclei), and double-opponent neurons in V1, V2 and V4. Abbreviations, as in Fig. 1. Adapted from [50,51]
Neuronal pathways that mediate general aversion to light
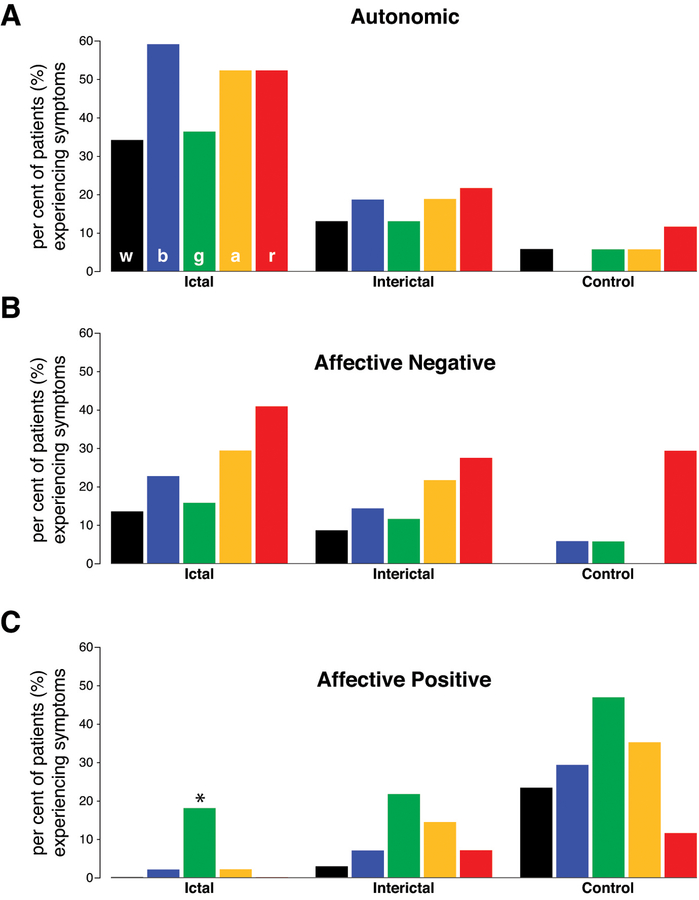
While most migraine patients report that light exacerbates their headache, a significant number of patients report that, during migraine, exposure to light is unpleasant. In a recent psychophysical study [10], we defined more completely what patients mean or feel when they say that exposure to light is “unpleasant.” In that study, patients with migraine were exposed to different colors of lights (blue, green, amber, red) during and in the absence of migraine. The perception, sensation, or emotions that each of the colors triggered were functionally grouped as (a) hypothalamic-mediated autonomic responses, (b) hypothalamic-mediated non-autonomic responses (c) affective negative responses, and (d) affective positive responses. Their description of hypothalamic-mediated autonomic responses included a myriad of symptoms, such as the perception of chest tightness, throat tightness, shortness of breath, fast breathing, faster than usual heart rate, light-headedness, dizziness, nausea, vomiting, dry mouth, salivation, rhinorrhea, stuffy sinuses and lacrimation. Description of experiences we assigned to non-autonomic hypothalamic functions included thirst and hunger (regulation of feeding) and feelings of being drowsy, tired, sleepy and fatigued. Some patients described actual yawning and difficulties with regulation of sleep. Descriptions of negative emotions most frequently included words such as intense, irritable, angry, nervous, hopeless, needy, agitated, sad, scared, cranky, upset, depressed, disappointed, jittery, worried, stressed, anxious, panic and fear. Some individuals experienced actual crying. Positive emotions were expressed most frequently with words such as happy, relaxing, soothing, and calming. The results of that study demonstrated that (a) light triggers more changes in hypothalamic-mediated autonomic functions and negative emotions during rather than in absence of migraine or in control subjects (Fig. 5A), (b) that color is more likely to trigger negative effects in migraineurs than in control subjects (Fig. 5B), and (c) that the association between color and positive emotions is stronger in control subjects than in migraineurs (Fig. 5C). These findings expand the definition of photophobia beyond that of the commonly used criteria of “headache (intensity) worsened by light” to the extent that it explains why migraine patients avoid light even when it does not seem to worsen their head pain.
Figure 5.
Aversion to light. A. Proportion of migraine patients and control subjects experiencing autonomic responses to white, blue, green, amber, and red lights. B. Proportion of migraine patients and control subjects experiencing negative emotions in response to white, blue, green, amber, and red lights. C. Proportion of migraine patients and control subjects experiencing positive emotions in response to white, blue, green, amber, and red lights. Adapted from [10].
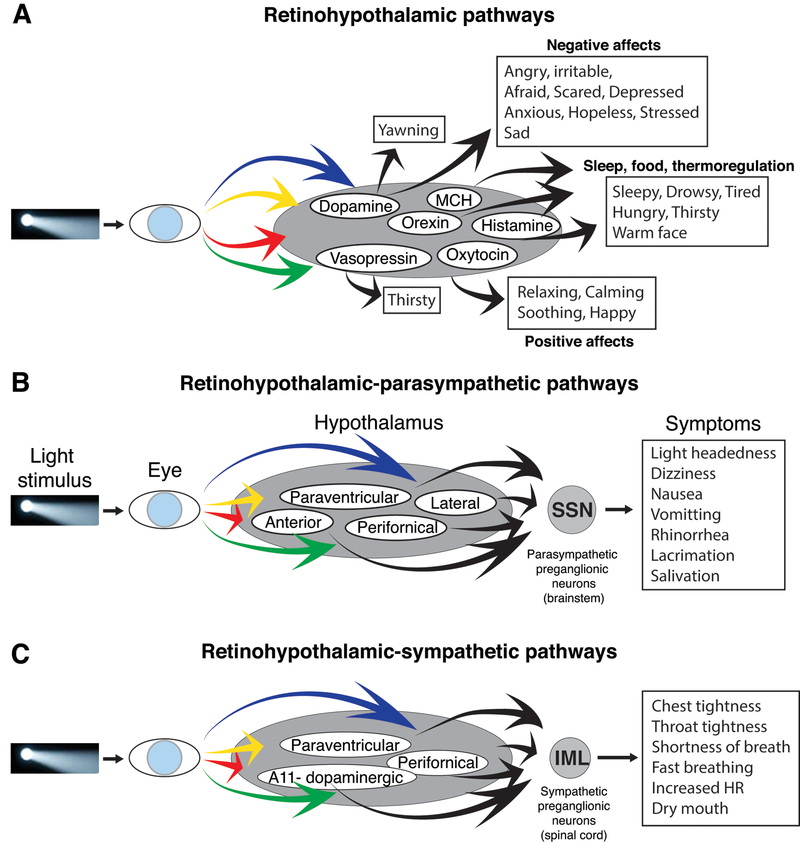
Preclinical neuroanatomical investigations that followed the psychophysical study described above showed that axons of retinal ganglion cells converge on hypothalamic neurons containing dopamine, histamine, orexin, melanin-concentrating hormone, oxytocin and vasopressin (Fig. 6A). These neurons, in turn, project directly to preganglionic parasympathetic neurons in the brainstem superior salivatory nucleus (Fig. 6B) and sympathetic preganglionic neurons in the intermediate lateral nucleus of the thoracic spinal cord (Fig. 6C). We termed these novel connections as the retinohypothalamic-parasympathetic (RHP) and retinohypothalamic-sympathetic (RHS) pathways, defining a new anatomical substrate for future studies on alterations of hypothalamic-mediated (autonomic and non-autonomic) functions by light. These are present both in migraineurs and non-migraineurs. Because the induction of all hypothalamic-mediated responses is not generally influenced by the color of light, it is likely that the retinohypothalamic interactions observed in the study are independent of color processing by the visual cortex. This scenario differs greatly from the one described above, showing that the perception of headache intensity is color-specific and most likely depends on sensory processing by the retino-thalamo-cortical pathway [46] and on its origin in retinal cones (Fig. 4).
Figure 6.
Neuronal pathways that mediate general aversion to light. Proposed pathways for modulation of autonomic responses, hypothalamic functions, and emotions by light. A. Pathways for inductions of symptoms mediated by dopamine, orexin, histamine, melanin concentrating hormone, oxytocin and vasopressin. B. Pathways for induction of symptoms associated with activation of the parasympathetic system. C. Pathways for induction of symptoms associated with activation of the sympathetic system. Adapted from [10].
In summary, While the rat studies define novel frameworks for conceptualizing how light triggers the symptoms described by patients, the human studies suggest that the aversive nature of light is more complex than simply an association with headache intensification.
Photophobia and the unique effects of green light
The clinical studies described above demonstrated that the a-wave amplitude generated by a narrow band (230 nm) of green light (as captured in the ERG studies) is smaller than the a-wave amplitude generated by narrow bands of blue, red and white lights. They also demonstrate that the P2 amplitude generated by green light (as captured in the visual evoked potential studies) is smaller than the P2 amplitudes generated by blue, amber and red lights, and that green light is least likely to exacerbate migraine headache or give rise to negative emotions and unpleasant hypothalamic-mediated autonomic responses. In fact, instead of exacerbating migraine, low-intensity 230nm green light seems capable of decreasing headache intensity and increasing positive emotions (described by migraineurs in the study using words such as happy, relaxing, soothing, and calming). Although the neurobiology of the soothing effects of green light are largely unknown and likely to involve a complex psychobiology [47–49], it is reasonable to suggest that by triggering the smallest activation signals in the retina, thalamus and cortex, green light may be able to reduce the migraine-driven cortical hyperexcitability and hypothalamic hypersensitivity to physiological and emotional deviation from homeostasis.
Summary:
The discovery of a novel retino-thalamo-cortical pathway that carries photic signal from melanopsinergic and non-melanopsinergic retinal ganglion cells to thalamic trigeminovascular neurons (i.e., those involved in migraine headache) that project to multiple cortical areas provide a neural substrate for exacerbation of headache by light, distortion of visual, auditory and olfactory perception by migraine, and the transient decline in cognitive functions.
Visually-impaired migraine patient perceive blue light as most painful. This finding is attributed to activation of intrinsically photosensitoive retinal ganglion cells.
Migraine patients who are not blind perceive blue and red light as most painful, and green light as least painful. This color preference depends on signals that originate in retinal cone and post-cone pathways.
The discovery of novel projections of retinal ganglion cells into distinct groups of hypothalamic neurons that regulate parasympathetic and sympathetic functions provide a neural substrate for understanding light’s ability to alter autonomic function.
The discovery of novel projections of retinal ganglion cells into hypothalamic nuclei containing dopaminergic, histaminergic, orexinergic, oxytocinergic, and vasopressinergic neurons pave a way for understanding light’s ability to trigger positive and negative emotions.
In the context of migraine, the aversive nature of light is more complex than its association with headache intensification.
Acknowledgement:
This research was supported by NIH grants NS-051484 and NS-035611.
Footnotes
Conflict of Interest: Dr. Burstein received grants support for hisa studies on migraine pathophysiology from Teva, Allergan, Dr. Reddy, and Trigemina; he also serves as a consultant to Alder Biopharm, Allergan, Amgen, Autonomic Technologies Inc., Avanir, Biohaven, Depomed, Dr. Reddy, Electrocore, Johnson and Johnson, Neurolief, Percept, Pernix, Strategic Science and Technologies, Teva, Theranica, Trigemina. Beth Israel Deaconess Medical center and Dr. Burstein hold a provisional patent on the use of narrow band green light for the treatment of photophobia in migraine.
REFERENCES
- 1.Lebensohn JE: Photophobia: mechanism and implications. Am J Ophthalmol 1951, 34:1294–1300. [DOI] [PubMed] [Google Scholar]
- 2.Kawasaki A, Purvin VA: Photophobia as the presenting visual symptom of chiasmal compression. J Neuroophthalmol 2002, 22:3–8. [DOI] [PubMed] [Google Scholar]
- 3.Aurora SK, Cao Y, Bowyer SM, Welch KM: The occipital cortex is hyperexcitable in migraine: experimental evidence. Headache 1999, 39:469–476. [DOI] [PubMed] [Google Scholar]
- 4.Lamonte M, Silberstein SD, Marcelis JF: Headache associated with aseptic meningitis. Headache 1995, 35:520–526. [DOI] [PubMed] [Google Scholar]
- 5.Welty TE, Horner TG: Pathophysiology and treatment of subarachnoid hemorrhage. Clin Pharm 1990, 9:35–39. [PubMed] [Google Scholar]
- 6.Fine PG, Digre KB: A controlled trial of regional sympatholysis in the treatment of photo-oculodynia syndrome. J Neuroophthalmol 1995, 15:90–94. [PubMed] [Google Scholar]
- 7.Noseda R, Kainz V, Jakubowski M, Gooley JJ, Saper CB, Digre K, Burstein R: A neural mechanism for exacerbation of headache by light. Nat Neurosci 2010, 13:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liveing E: On megrim, sick headache. Nijmegen: Arts & Boeve Publishers; 1873. [Google Scholar]
- 9.Miller NR: Photophobia In Walsh and Hoyt’s clinical neuro-ophthlmology, edn 4th Edited by Miller NR: Williams&Wilkins; 1985:1099–1106. vol 2.] [Google Scholar]
- 10.Noseda R, Lee AJ, Nir RR, Bernstein CA, Kainz VM, Bertisch SM, Buettner C, Borsook D, Burstein R: Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci U S A 2017, 114:E5683–E5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burstein R, Jakubowski M, Garcia-Nicas E, Kainz V, Bajwa Z, Hargreaves R, Becerra L, Borsook D: Thalamic sensitization transforms localized pain into widespread allodynia. Ann Neurol 2010, 68:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burstein R, Yarnitsky D, Goor-Aryeh I, Ransil BJ, Bajwa ZH: An association between migraine and cutaneous allodynia. Ann Neurol 2000, 47:614–624. [PubMed] [Google Scholar]
- 13.Maleki N, Becerra L, Upadhyay J, Burstein R, Borsook D: Direct optic nerve pulvinar connections defined by diffusion MR tractography in humans: Implications for photophobia. Hum Brain Mapp 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noseda R, Jakubowski M, Kainz V, Borsook D, Burstein R: Cortical projections of functionally identified thalamic trigeminovascular neurons: implications for migraine headache and its associated symptoms. J Neurosci 2011, 31:14204–14217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valenstein E, Bowers D, Verfaellie M, Heilman KM, Day A, Watson RT: Retrosplenial amnesia. Brain 1987, 110 (Pt 6):1631–1646. [DOI] [PubMed] [Google Scholar]
- 16.Donchin O, Gribova A, Steinberg O, Bergman H, Vaadia E: Primary motor cortex is involved in bimanual coordination. Nature 1998, 395:274–278. [DOI] [PubMed] [Google Scholar]
- 17.Mountcastle VB, Lynch JC, Georgopoulos A, Sakata H, Acuna C: Posterior parietal association cortex of the monkey: command functions for operations within extrapersonal space. J Neurophysiol 1975, 38:871–908. [DOI] [PubMed] [Google Scholar]
- 18.Lowel S, Singer W: Selection of intrinsic horizontal connections in the visual cortex by correlated neuronal activity. Science 1992, 255:209–212. [DOI] [PubMed] [Google Scholar]
- 19.Livingstone MS, Hubel DH: Anatomy and physiology of a color system in the primate visual cortex. J Neurosci 1984, 4:309–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolberg FL, Ziegler DK: Olfactory hallucination in migraine. Arch Neurol 1982, 39:382. [DOI] [PubMed] [Google Scholar]
- 21.Wang W, Timsit-Berthier M, Schoenen J: Intensity dependence of auditory evoked potentials is pronounced in migraine: an indication of cortical potentiation and low serotonergic neurotransmission? Neurology 1996, 46:1404–1409. [DOI] [PubMed] [Google Scholar]
- 22.Hong SC, Holbrook EH, Leopold DA, Hummel T: Distorted olfactory perception: a systematic review. Acta Otolaryngol 2012, 132 Suppl 1:S27–31. [DOI] [PubMed] [Google Scholar]
- 23.Zaidi FH, Hull JT, Peirson SN, Wulff K, Aeschbach D, Gooley JJ, Brainard GC, Gregory-Evans K, Rizzo JF 3rd, Czeisler CA, et al. : Short-wavelength light sensitivity of circadian, pupillary, and visual awareness in humans lacking an outer retina. Curr Biol 2007, 17:2122–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Main A, Vlachonikolis I, Dowson A: The wavelength of light causing photophobia in migraine and tension-type headache between attacks. Headache 2000, 40:194–199. [DOI] [PubMed] [Google Scholar]
- 25.Good PA, Taylor RH, Mortimer MJ: The use of tinted glasses in childhood migraine. Headache 1991, 31:533–536. [DOI] [PubMed] [Google Scholar]
- 26.Adams WH, Digre KB, Patel BC, Anderson RL, Warner JE, Katz BJ: The evaluation of light sensitivity in benign essential blepharospasm. Am J Ophthalmol 2006, 142:82–87. [DOI] [PubMed] [Google Scholar]
- 27.Blackburn MK, Lamb RD, Digre KB, Smith AG, Warner JE, McClane RW, Nandedkar SD, Langeberg WJ, Holubkov R, Katz BJ: FL-41 tint improves blink frequency, light sensitivity, and functional limitations in patients with benign essential blepharospasm. Ophthalmology 2009, 116:997–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noseda R, Bernstein CA, Nir RR, Lee AJ, Fulton AB, Bertisch SM, Hovaguimian A, Cestari DM, Saavedra-Walker R, Borsook D, et al. : Migraine photophobia originating in cone-driven retinal pathways. Brain 2016, 139:1971–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Conway BR: Color vision, cones, and color-coding in the cortex. Neuroscientist 2009, 15:274–290. [DOI] [PubMed] [Google Scholar]
- 30.Caywood MS, Willmore B, Tolhurst DJ: Independent components of color natural scenes resemble V1 neurons in their spatial and color tuning. J Neurophysiol 2004, 91:2859–2873. [DOI] [PubMed] [Google Scholar]
- 31.Doi E, Inui T, Lee TW, Wachtler T, Sejnowski TJ: Spatiochromatic receptive field properties derived from information-theoretic analyses of cone mosaic responses to natural scenes. Neural Comput 2003, 15:397–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tailor DR, Finkel LH, Buchsbaum G: Color-opponent receptive fields derived from independent component analysis of natural images. Vision Res 2000, 40:2671–2676. [DOI] [PubMed] [Google Scholar]
- 33.Hoyer PO, Hyvarinen A: Independent component analysis applied to feature extraction from colour and stereo images. Network 2000, 11:191–210. [PubMed] [Google Scholar]
- 34.Kentridge RW, Heywood CA, Weiskrantz L: Color contrast processing in human striate cortex. Proc Natl Acad Sci U S A 2007, 104:15129–15131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Danilova MV, Mollon JD: The comparison of spatially separated colours. Vision Res 2006, 46:823–836. [DOI] [PubMed] [Google Scholar]
- 36.Tootell RB, Silverman MS, Hamilton SL, De Valois RL, Switkes E: Functional anatomy of macaque striate cortex. III. Color. J Neurosci 1988, 8:1569–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hubel DH, Livingstone MS: Segregation of form, color, and stereopsis in primate area 18. J Neurosci 1987, 7:3378–3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Datta R, Aguirre GK, Hu S, Detre JA, Cucchiara B: Interictal cortical hyperresponsiveness in migraine is directly related to the presence of aura. Cephalalgia 2013, 33:365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vincent M, Pedra E, Mourao-Miranda J, Bramati IE, Henrique AR, Moll J: Enhanced interictal responsiveness of the migraineous visual cortex to incongruent bar stimulation: a functional MRI visual activation study. Cephalalgia 2003, 23:860–868. [DOI] [PubMed] [Google Scholar]
- 40.Huang J, Zong X, Wilkins A, Jenkins B, Bozoki A, Cao Y: fMRI evidence that precision ophthalmic tints reduce cortical hyperactivation in migraine. Cephalalgia 2011, 31:925–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin PR, Reece J, Forsyth M: Noise as a trigger for headaches: relationship between exposure and sensitivity. Headache 2006, 46:962–972. [DOI] [PubMed] [Google Scholar]
- 42.Boulloche N, Denuelle M, Payoux P, Fabre N, Trotter Y, Geraud G: Photophobia in migraine: an interictal PET study of cortical hyperexcitability and its modulation by pain. J Neurol Neurosurg Psychiatry 2010, 81:978–984. [DOI] [PubMed] [Google Scholar]
- 43.Denuelle M, Boulloche N, Payoux P, Fabre N, Trotter Y, Geraud G: A PET study of photophobia during spontaneous migraine attacks. Neurology 2011, 76:213–218. [DOI] [PubMed] [Google Scholar]
- 44.Griebe M, Flux F, Wolf ME, Hennerici MG, Szabo K: Multimodal assessment of optokinetic visual stimulation response in migraine with aura. Headache 2014, 54:131–141. [DOI] [PubMed] [Google Scholar]
- 45.Antal A, Polania R, Saller K, Morawetz C, Schmidt-Samoa C, Baudewig J, Paulus W, Dechent P: Differential activation of the middle-temporal complex to visual stimulation in migraineurs. Cephalalgia 2011, 31:338–345. [DOI] [PubMed] [Google Scholar]
- 46.Noseda R, Bernstein CA, Nir RR, Lee AJ, Fulton AB, Bertisch SM, Hovaguimian A, Cestari DM, Saavedra-Walker R, Borsook D, et al. : Migraine photophobia originating in cone-driven retinal pathways. Brain 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hurlbert AC, Ling Y: Biological components of sex differences in color preference. Curr Biol 2007, 17:R623–625. [DOI] [PubMed] [Google Scholar]
- 48.Strauss ED, Schloss KB, Palmer SE: Color preferences change after experience with liked/disliked colored objects. Psychon Bull Rev 2013, 20:935–943. [DOI] [PubMed] [Google Scholar]
- 49.Palmer SE, Schloss KB: An ecological valence theory of human color preference. Proc Natl Acad Sci U S A 2010, 107:8877–8882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Noseda R, Burstein R: Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain 2013, 154 Suppl 1:S44–53. [DOI] [PubMed] [Google Scholar]
- 51.Noseda R, Burstein R: Advances in understanding the mechanisms of migraine-type photophobia. Curr Opin Neurol 2011, 24:197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]