Abstract
Introduction
Acute appendicitis is one of the more common causes of acute abdominal pain. It occurs when the lumen of the appendix is obstructed, leading to inflammation and finally perforation. The preoperative differentiation of perforated from nonperforated appendicitis is important and helpful to define prognosis and determine an adequate therapeutic approach, including consideration for nonsurgical treatment. This study recommends computed tomography (CT), a noninvasive method of investigation, be used frequently in clinically suspected cases of perforated appendicitis in the Pakistani population for better patient outcomes.
Objective
To determine the diagnostic accuracy of CT in differentiating perforated from nonperforated appendicitis by using histopathology as the gold standard.
Material and methods
A total of 236 patients with a clinical suspicion of appendicitis were included in this study. CT was performed in Liaquat National Hospital and Medical College. At the time of scanning, intravenous contrast was administered. Histopathology was used as the diagnostic gold standard. CT findings were documented using a proforma. The patient was returned to the referring department and followed after surgery for histopathology.
Results
Sensitivity, specificity, and positive and negative predictive values, as well as the accuracy of CT in the detection of perforated appendicitis, was 71.4%, 90.7%, 62.5%, 93.6%, and 87.3%, respectively.
Conclusion
CT findings can be used to select patients with perforated appendicitis for initial nonoperative management.
Keywords: acute appendicitis, computed tomography, non-perforated appendicitis
Introduction
Acute appendicitis is one of the more common causes of acute abdominal pain, with an incidence of 33.8 cases per 100,000 individuals per year, with a lifetime risk of 9%. The incidence of appendicitis has increased in recent years at an average rate of 0.5 cases per 100,000 individuals per year [1].
Appendicitis occurs when the lumen of the appendix is obstructed, leading to inflammation and finally perforation. Individuals from Hispanic and Asian origins have higher rates of perforation [1]. The incidence of perforated appendicitis is high in developing countries like Pakistan, with approximately 20% of appendicitis cases being perforated [2].
Preoperative differentiation of perforated from nonperforated appendicitis is important and helpful to define prognosis and determine an adequate therapeutic approach, including consideration for nonsurgical treatment. The incidence rate of postoperative complications in patients with perforated appendectomy is high compared to nonperforated appendectomy (28.4% vs. 4.7%) [3]. In one study, the mean length of hospital stay in the perforated group was 6.3 days while it was 2.9 days in the nonperforated group [4].
In this modern era of imaging, computed tomography (CT) has played a vital role in diagnosing appendicitis and in differentiating perforated from nonperforated appendicitis. It is noninvasive, compared to invasive methods like diagnostic laparoscopy [5-11]. In one study, the sensitivity and specificity of CT to diagnose perforated appendicitis was 69% and 97%, respectively [4].
The purpose of this study is to evaluate the usefulness of the noninvasive modality CT in differentiating perforated from nonperforated appendicitis and define its sensitivity and specificity in differentiating patients with perforated appendicitis from those with nonperforated appendicitis. Histopathology was used as the diagnostic gold standard.
The rates of appendectomy in patients with perforated appendicitis have decreased since 1995 [1]. If perforated appendicitis is diagnosed preoperatively, the management of the patient is different, as percutaneous drainage followed by interval appendectomy is recommended for patients with perforated appendicitis [1]. On the other hand, simple laparoscopic appendectomy is needed for patients with nonperforated appendicitis; therefore, it is important to diagnose perforated appendicitis preoperatively.
There is not enough or recent local data on this topic; therefore, the purpose of this study is to evaluate the accuracy of the noninvasive modality CT in differentiating perforated from nonperforated appendicitis for the local population.
Materials and methods
We conducted this cross-sectional study at the department of radiology at Liaquat National Hospital and Medical College for six months. A total of 236 patients with clinical suspicion of appendicitis and aged 15 to 70 years were included. These patients underwent surgery within a week of their CT scan. Patients who were refused surgery, referred to other hospitals, or with deranged renal function were excluded.
Informed consent was obtained prior to the procedure. CT was performed on a Toshiba Activion™ 16 Multislice CT scanner (Toshiba Medical Systems Corp., Tokyo, Japan). The scanning protocol included the acquisition of axial helical CT sections before and after the administration of intravenous contrast, extending from the xiphoid process of the sternum to the pubic symphysis at 120-kVp and 210 mA. At the time of scanning, intravenous contrast was administered using a power injector at a rate of 5 mL per second followed by the acquisition of axial cuts at 4-mm slice thickness in the portal venous phase (60 to 70 seconds after injection of bolus contrast). Sagittal and coronal multiplanar reconstruction was also performed. CT scans were interpreted by consultant radiologists with a minimum of five years of experience. Histopathology was used as the diagnostic gold standard. CT scan findings were documented by the researcher using a proforma. Data were analyzed on Statistical Package for Social Sciences (SPSS) Statistics for Windows, Version 17.0 (SPSS Inc., Chicago, IL, US). Relevant descriptive statistics, frequency, and percentage were computed for gender, CT scan findings, and histopathology findings. Mean ± standard deviation for age were calculated. Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of perforated appendicitis on CT scan were calculated using histopathology as the gold standard. Stratification was performed to control effect modifiers like age and gender to observe the effect of these modifiers on the accuracy through chi-square test; p<0.05 was considered significant.
Results
A total of 236 patients with a clinical suspicion of appendicitis were included in this study. The average age of the patients was 40 ± 13 years; 144 (61.02%) were male and 92 (38.98%) female.
The following, seen in approximately 25% of patients, were taken as specific signs of nonperforated appendicitis on CT scan: enlarged appendiceal diameter (> 6 mm) with an occluded lumen; appendiceal wall thickening (> 2 mm); periappendiceal fat stranding; appendiceal wall enhancement; and appendicolith (Figure 1).
Figure 1. Acute appendicitis without perforation.
Axial image without contrast shows the swollen appendix with appendicolith (arrow). Periappendiceal inflammatory changes seen.
Specific signs for perforated appendicitis on CT scan included a defect in enhancing the appendiceal wall, focal area of nonenhancement with enhancing of the remaining appendiceal wall, extraluminal air, and extraluminal appendicolith or abscess formation (Figures 2-3).
Figure 2. Coronal image of abdomen showing swollen appendix (blue arrow) with marked periappendiceal inflammatory fat stranding (arrowhead). Small amount of free air also seen (white arrow).
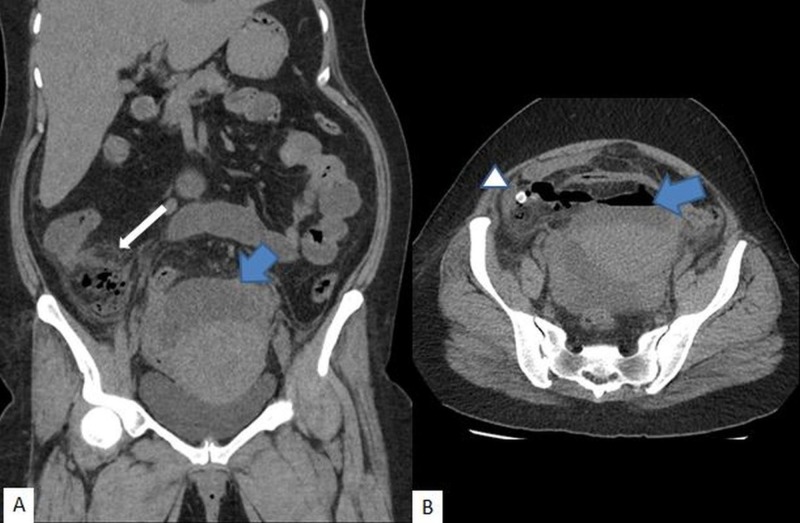
Figure 3. Acute appendicitis with perforation.
A) Coronal and B) axial images demonstrated collection (blue arrow), inflammatory changes in the right iliac fossa (white arrow); appendicolith (arrowhead)
CT reported that there were 20.34% (48/236) cases that had perforated and 79.66% had non-perforated appendicitis while histopathology reported 17.8% (42/236) with perforated and 82.2% with non-perforated appendicitis.
Sensitivity, specificity, positive and negative predictive values, as well as the accuracy of CT in the detection of perforated appendicitis, was 71.4%, 90.7%, 62.5%, 93.6%, and 87.3% respectively.
The accuracy of CT in the detection of perforated appendicitis was 85.4% in male cases and 92.2% in female cases. Similarly, concerning age groups, the accuracy of CT was above 92% for patients older than 40 years and 82.9% for younger or equal to 40 years.
Discussion
Opting for nonsurgical management in cases of perforated appendicitis depends on accurate and reliable CT interpretation. Sensitivities and specificities for CT for the diagnosis of acute appendicitis are around 90%, resulting in significantly reduced negative appendectomy rates from 15%–20% to 2%–12% [12-16]. Despite this high sensitivity, the differentiation between perforated and nonperforated appendicitis is as accurate as it should be.
Distinguishing perforated from nonperforated appendicitis depends on a wide range of features as seen on CT, which include the presence of free fluid, phlegmon, abscess, extraluminal air, and bowel wall thickening; each of these characteristics favor perforation [6,17-18].
In the present study, the average age of the patients was 40 ± 13 years. Of 236 cases, 144 (61.02%) were male and 92 (38.98%) female. Similarly, in the Kim et al. study [19], there were 339 patients with a mean age of 40.8 years (range, 19 to 80 years); 183 were male (mean age, 40.5 years; range, 19 to 79 years) and 156 were female (mean age, 41.2 years; range, 19 to 80 years).
In our study, sensitivity, specificity, positive and negative predictive values, as well as the accuracy of CT in the detection of perforated appendicitis, were 71.4%, 90.7%, 62.5%, 93.6%, and 87.3%, respectively. In another study, the sensitivity and specificity of CT to diagnose perforated appendicitis was 69% and 97%, respectively [4]. In the Fraser et al. study [9], CT had a sensitivity of 62% with a specificity of 81% in predicting appendiceal perforation.
One retrospective study found that using a defect in the enhancing appendiceal wall as the sole CT finding to determine perforation increased the sensitivity, specificity, and accuracy to 95.0%, 96.8%, and 96.1%, respectively [8].
In this study, the accuracy of CT in the detection of perforated appendicitis was 85.4% in male cases and 92.2% in female cases. Similarly, concerning age groups, the accuracy of CT was greater than 92% for patients older than 40 years and 82.9% for those younger to or equal to 40 years. Despite the existence of many studies on CT diagnosis of appendicitis, to our knowledge, few have focused on the differential diagnosis of perforated vs. nonperforated appendicitis. A study by Horrow et al. involved single-section helical CT with several scanning protocols. Specifically, the section thickness ranged from 5 mm to 10 mm [6]. In addition, some examinations were performed with oral contrast material while others were performed with intravenous contrast material. In that study, a defect of the enhancing appendiceal wall was most sensitive as a single finding, but its sensitivity remained at 64%. On the other hand, a combination of four findings (abscess, phlegmon, extraluminal air, and extraluminal appendicolith) had higher diagnostic accuracy. However, the use of a combination of several findings may be complicated in an emergency. Another study [20] based specificity on a focal defect of the enhancing appendiceal wall.
Our study was limited in that it is a single-center study with a relatively small patient population. Also, the interpretation of CT scans was performed by several radiologists with a variety of experience levels.
Conclusions
A CT scan is markedly sensitive, as well as specific, for the differentiation of perforated from non-perforated appendicitis. This, in turn, helps in patient selection for initial nonoperative management.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. Anderson JE, Bickler SW, Chang DC, Talamini MA. World J Surg. 2012;36:2787–2794. doi: 10.1007/s00268-012-1749-z. [DOI] [PubMed] [Google Scholar]
- 2.Perforated appendix contributing factors. Ahmed T, Ali Z, Ali A, Anjum S. https://jumdc.tuf.edu.pk/articles/volume-1/no-2/UMDC4_Perforated-appendix.pdf JUMDC. 2010;1:11–16. [Google Scholar]
- 3.Acute perforated appendicitis: an analysis of risk factors to guide surgical decision making. Williams R, Barreto S, Thomas T, Tiong L, Travers E, Mackillop C, Lorimer M. https://www.ncbi.nlm.nih.gov/pubmed/22466494. Indian J Med Sci. 2010;64:58–65. [PubMed] [Google Scholar]
- 4.Perforated appendicitis accuracy of CT diagnosis and correlation of CT findings with length of hospital stay. Siddiqui AH, Afzal S. https://www.ncbi.nlm.nih.gov/pubmed/18182135. J Coll Physicians Surg Pak. 2007;17:721–725. [PubMed] [Google Scholar]
- 5. CT in appendicitis. Chalazonitis AN, Tzovara I, Sammouti E, et al. http://dirjournal.org/sayilar/18/buyuk/pdf_DIR_154.pdf. Diagn Interv Radiol. 2008;13:19–25. [PubMed] [Google Scholar]
- 6.Differentiation of perforated from nonperforated appendicitis at CT. Horrow MM, White DS, Horrow JC. Radiology. 2003;227:46–51. doi: 10.1148/radiol.2272020223. [DOI] [PubMed] [Google Scholar]
- 7.Spiral CT findings in complicated appendicitis: pictorial essay. Taheri MS, Haghighat Khan HR, Birang SH, Azad MY, Jamali F. http://iranjradiol.com/en/articles/78918.html Iran J Radiol. 2009;6:0. [Google Scholar]
- 8.Perforated and nonperforated appendicitis: defect in enhancing appendiceal wall - depiction with multidetector row CT. Tsuboi M, Takase K, Kaneda I, et al. Radiology. 2008;246:142–147. doi: 10.1148/radiol.2461051760. [DOI] [PubMed] [Google Scholar]
- 9.Accuracy of computed tomography in predicting appendiceal perforation. Fraser JD, Aguayo P, Sharp SW, et al. J Pedia Surg. 2010;45:231–234. doi: 10.1016/j.jpedsurg.2009.10.040. [DOI] [PubMed] [Google Scholar]
- 10.Diagnostic performance of CT findings in differentiating of perforated from non perforated appendicitis. Suthikeeree W, Lertdomrongdej L, Charoensak A. http://www.thaiscience.info/journals/Article/JMAT/10657243.pdf. J Med Assoc. 2010;93:1422–1429. [PubMed] [Google Scholar]
- 11.Impact of multidetector CT examination upon accurate diagnosis and management of perforated appendicitis. Rizk H, Karam KS, Eldaly AMAF, Mostafa AA. Aini KE. http://www.kasrelainijs.eg.net/Upload/September%202008/4.pdf Kasr EL Aini J Surg. 2008;9:1–5. [Google Scholar]
- 12.The use of a computed tomography scan to rule out appendicitis in women of childbearing age is as accurate as clinical examination: a prospective randomized trial. Lopez PP, Cohn SM, Popkin CA, Jackowski J, Michalek JE. https://www.ingentaconnect.com/content/sesc/tas/2007/00000073/00000012/art00007. Am Surg. 2007;73:1232–1236. [PubMed] [Google Scholar]
- 13.Management of pediatric acute appendicitis in the computed tomographic era. Tsao K, St. Peter SD, Valusek PA, et al. J Surg Res. 2008;147:221–224. doi: 10.1016/j.jss.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Imaging of acute appendicitis and its impact on negative appendectomy and perforation rates: the St. Paul's experience. Chooi WK, Brown JA, Zetler P, Wiseman S, Cooperberg P. https://search.proquest.com/openview/79a7ac0298373407a8d55b827287b8ea/1?pq-origsite=gscholar&cbl=34862. Can Assoc Radiol. 2007;58:220–224. [PubMed] [Google Scholar]
- 15.Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Florence M, Flum DR, Jurkovich GJ, Lin P, Steele SR, Symons RG, Thirlby R. Trans Meet Am Surg Assoc. 2008;126:198–204. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 16.Effect of cross-sectional imaging on negative appendectomy and perforation rates in children. Applegate KE, Sivit CJ, Salvator AE, Borisa VJ, Dudgeon DL, Stallion AE, Grisoni ER. Radiology. 2001;220:103–107. doi: 10.1148/radiology.220.1.r01jl17103. [DOI] [PubMed] [Google Scholar]
- 17.Evaluation of perforated and nonperforated appendicitis with CT. Yeung K-W, Chang M-S, Hsiao C-P. Clin Imaging. 2004;28:422–427. doi: 10.1016/S0899-7071(03)00286-9. [DOI] [PubMed] [Google Scholar]
- 18.Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Foley TA, Earnest IV F, Nathan MA, Hough DM, Schiller HJ, Hoskin TL. Radiology. 2005;235:89–96. doi: 10.1148/radiol.2351040310. [DOI] [PubMed] [Google Scholar]
- 19.Differentiation of early perforated from nonperforated appendicitis: MDCT findings, MDCT diagnostic performance and clinical outcome. Kim MS, Park HW, Park JY, et al. Abdom Imaging. 2014;39:459–466. doi: 10.1007/s00261-014-0117-x. [DOI] [PubMed] [Google Scholar]
- 20.Appendiceal CT in 140 cases: diagnostic criteria for acute and necrotizing appendicitis. Choi YH, Fischer E, Hoda SA, et al. Clin Imaging. 1998;22:252–271. doi: 10.1016/s0899-7071(97)00080-6. [DOI] [PubMed] [Google Scholar]