Abstract
Background
Prospective collection of patient-reported opioid consumption and pain levels post-surgically may hold value in highlighting solutions related to the opioid crisis. Traditional methods for collecting patient-reported outcomes after surgery, such as paper surveys, often have poor response rates, and electronic messaging may offer more convenience and therefore yield more robust data.
Questions/Purposes
The purpose of this study was to evaluate whether a novel mobile phone short message service (SMS) platform would lead to better patient response rates to surveys on pain and opioid use than data-collection tools.
Methods
An SMS text messaging platform was created and implemented between September 2017 and May 2018 at an orthopedic specialty hospital. The purpose was to collect reports on opioid consumption and pain levels twice a day for 6 weeks post-surgery from patients who had undergone total hip or knee arthroplasty or a single-level lumbar microdiscectomy or decompression spine surgery. Patients who responded to fewer than 50% of the text messages were excluded.
Results
Our mobile phone text messaging platform was used by 183 patients, demonstrating a significantly higher response rate (96.1%) than our institution’s post-operative email registry capture, as well as the majority of published response rates for post-operative outcomes captured through electronic and traditional data-collection systems. Response rate remained consistently high among the various surgeons and across patients, regardless of age.
Conclusions
This application of a widely available technology can improve the measurement of post-operative patient-reported outcomes. Such data can in turn be used in the development of strategies to reduce post-operative opioid use. The adoption of novel technologies at a patient level will play a key role in combating the opioid epidemic.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-9635-3) contains supplementary material, which is available to authorized users.
Keywords: opioid use, SMS text messaging
Introduction
Opioid misuse is among the most significant preventable public health threats facing the USA, claiming more than 600,000 lives to date [3, 8]. Rates of opioid use disorder and overdose have continued to grow, and in 2016 over 46 people died on average each day from overdoses involving prescription opioids [3]. Opioids are commonly prescribed after surgery for the management of acute pain, with orthopedic surgeons among the top opioid prescribers [15]. Within this context, there is an increasing focus on strategies to reduce opioid prescribing, including after surgery. However, accurate and reliable methods for assessing such strategies are essential to determining best practices.
The prospective collection of patient-reported data on opioid consumption and pain in the acute post-operative period may have tremendous value in understanding current challenges and developing solutions related to opioid use and misuse. Several recent studies have examined both the amount of opioid analgesics prescribed and the amount taken by patients undergoing orthopedic procedures. Sabatino and colleagues, for example, found that 61% of patients undergoing one of five orthopedic procedures in 2015 at one institution reported unused opioid medication and that an estimated 43,000 unused opioid pills were prescribed [13].
Traditional methods for collecting patient-reported outcomes after surgery, such as paper surveys, often have poor response rates, and in our clinical experience may be influenced by recall bias if not completed in a timely manner or adversely affect office workflow if completed in person during a post-operative visit. Low response rates may lead to sampling or nonresponse bias, where respondents do not represent the larger population of interest [10]. While there is no universally accepted survey response rate, 60% has been noted as a general “threshold of acceptability” [9]. In addition, traditional surveys are generally completed on a weekly or monthly basis. In New York State, initial opioid prescriptions for acute pain are limited to 7 days, at which point refills may be provided as needed. Thus, past methods for capturing and understanding post-operative opioid use and pain levels may lack sufficient granularity, necessitating novel ways of collecting patient-reported outcomes, especially after hospital discharge.
In early 2018, 77% of Americans reported having a smartphone and an even larger number had mobile phones with short message service (SMS) text message capability [12]. Thus, a novel SMS text messaging platform was created to improve collection of patient-reported opioid use and post-operative pain. We hypothesized that such a system would lead to improved patient response rates when compared to traditional data-collection tools.
Patients and Methods
A novel SMS text messaging platform was created and implemented between September 2017 and May 2018 at an orthopedic specialty hospital. The aim was to collect daily information on patient-reported opioid consumption and pain for 6 weeks post-surgery. We prospectively enrolled patients undergoing total hip or knee arthroplasty (THA or TKA, respectively) or single-level lumbar microdiscectomy or decompression with one of 16 orthopedic surgeons at our institution. Patients with opioid dependence, defined as daily opioid use during the 6 months before surgery, were deemed ineligible for enrollment. Those who had used opioids on a non-daily basis in the 6 months prior were classified as having a history of intermittent opioid use. All patients completed an informed consent form prior to enrollment, which counseled them that their phone number would be stored on a third-party web server and protected with 128-bit encryption and other reasonable, commercially available security measures.
The SMS platform was created using a secure web server and linked to a database bound to a single local internet protocol (IP) address. A third-party cloud-based service, Twilio (San Francisco, CA, USA), was used to send and receive SMS text messages to and from our database. An administrative portal was created, through a website protected by a password and two-factor authentication, to which access was limited to certain users and IP addresses. The credentialed research team used this portal to enroll new patients, follow-up on patients, and generate reports in real time. All data was transferred between systems using an encrypted secure file transfer protocol connection. Data from different sources was linked on the server using a system-generated unique key for each patient, which was used as the only patient identifier whenever possible, to minimize the risk of data compromise. A simplified diagram explaining this system architecture can be seen in Fig. 1.
Fig. 1.
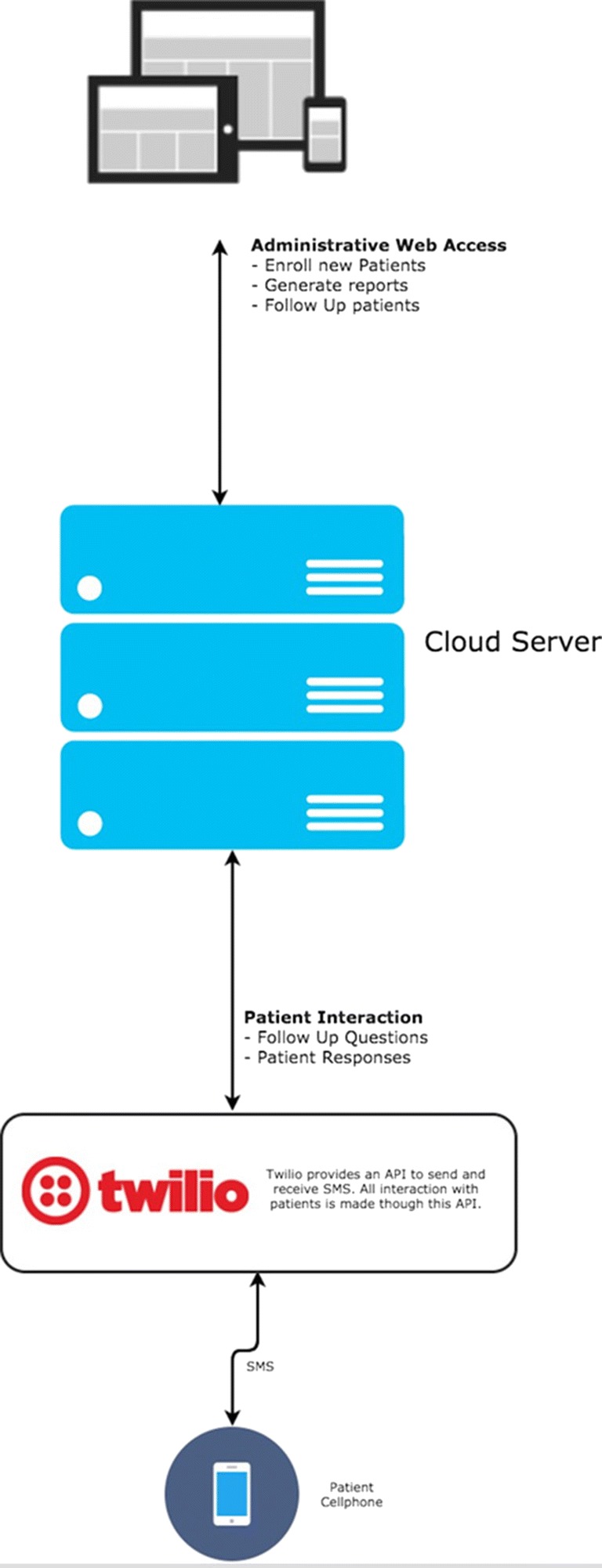
Simplified architecture diagram of SMS system
The system automatically queried patients twice a day after surgery, asking about daily pain levels (on a 0–10 numeric rating scale) and opioid consumption. The system also automatically queried patients every week, asking if they were experiencing any adverse effects they believed were related to opioid use. If patients reported no opioid use for 4 consecutive days, they were then asked if they had completed taking opioids, and if so, they were sent a string of end-of-survey questions. If patients reported they were still taking opioids at the end of 4 days, they continued to get twice-daily text messages until they reported no opioid use for 4 consecutive days, when they were asked if they had completed taking opioids. Patients still taking opioids 6 weeks after surgery were asked the end-of-survey questions. (See Online Resource 1 for details of this algorithm for data collection).
Research staff attempted to contact non-responsive patients by phone or email on a weekly basis. Patients were called if they did not respond to any questions for three consecutive days. All patients had the opportunity to stop receiving text messages at any time by responding with “STOP” to any question. Response rates for all patients enrolled in this study were then collected retrospectively. Given the high frequency and volume of questions, adequate patient response was defined as answering greater than 50% of text messages received, a threshold used previously in the literature for electronic survey compliance [11]. This response rate was then compared to our institution’s arthroplasty service email registry, which queries patients at 4 weeks post-operatively and automatically generates two follow-up weekly reminder emails for patients who have not yet responded.
Statistical analysis was performed using the SAS software package, version 9.4 (SAS Institute Inc., Cary, NC, USA). Student t tests were performed for continuous data, and χ2 or Fisher’s exact tests were performed for categorical data, as appropriate. Odds ratios along with 95% confidence intervals are reported for logistic regression analysis. Two-tailed p values of < 0.05 were considered statistically significant.
Results
Patient Characteristics
The average age of the 183 patients enrolled was 59.4 ± 10.9 years. Average body mass index (BMI) was 29.4 ± 5.8, and 87 (47.5%) patients were female. Of all patients enrolled, 44 (24.0%) underwent THA, 88 (48.1%) underwent TKA, 29 (15.8%) underwent lumbar microdiscectomy, and 22 (12.0%) underwent lumbar decompression. Thirty-seven (20.2%) patients had a self-reported or medically diagnosed psychiatric disorder, such as depression, anxiety, or history of substance misuse or dependence; 28 (15.3%) patients reported intermittent opioid use over the prior 6 months (Table 1).
Table 1.
Patient characteristics
| n ± SD | % | |
|---|---|---|
| Age | 59.4 ± 10.9 | |
| BMI | 29.4 ± 5.8 | |
| Gender | ||
| Male | 96 | 52.5 |
| Female | 87 | 47.5 |
| Surgery | ||
| THA | 44 | 24.0 |
| TKA | 88 | 48.1 |
| Lumbar decompression | 22 | 12.0 |
| Lumbar microdiscectomy | 29 | 15.8 |
| History of psychiatric disorder | 37 | 20.2 |
| History of intermittent opioid use | 28 | 15.3 |
THA total hip arthroplasty, TKA total knee arthroplasty
Response Rates
Of the 183 patients enrolled, three were excluded from analysis for either undergoing a secondary procedure in the acute post-operative period or not being prescribed or taking any opioid. Of the remaining 180 patients, 173 completed at least 50% of the twice-daily SMS post-operative questions, conferring an overall response rate of 96.1%. A logistic regression analysis revealed that age (CI, 0.93–1.11), BMI (CI, 0.81–1.03), gender (CI, 0.57–1.94), psychiatric history (CI, 0.06–2.65), and history of intermittent pre-operative opioid use (CI, 0.25–4.39) were not associated with failure to respond to SMS surveys. The seven patients who did not respond to the SMS survey questions underwent surgery by five different surgeons, which confirms that response remained high regardless of enrolling surgeon.
A review of institutional registry data for patients undergoing THA and TKA between 2016 and 2017 revealed a response rate of 66.63% (3516/5277) to an email survey sent at 4 weeks after surgery (with two automated weekly follow-up emails if no initial response was received). This percentage includes both patients who responded to the initial email and those who responded only after one or two reminders. Compared to the registry response rate, which captures outcomes at an overlapping timeframe in an identical patient population, the SMS system performs favorably with a significantly higher response rate (p < 0.001).
Discussion
Patients view surgical outcomes differently from their physicians, and certain elements of patient recovery can be best ascertained through patient reports [2]. Within this context, strategies to better engage patients and garner their perspectives after surgery are needed to aid surgeons in better predicting and improving the surgical outcomes most relevant to patients. Among the outcomes considered important to patients after surgery are pain and pain control [16]. This study explored the use of an SMS survey system to collect patient-reported pain levels, opioid consumption, and adverse effects in the acute post-operative period after THA, TKA, and lumbar spine surgery. The system recorded a very high response rate and has the ability to capture granular data not seen with traditional phone, email, or mail surveys. Such data will become increasingly important given regulations on post-operative opioid prescribing and evolving patient expectations for quick recovery after surgery. SMS messaging has been used previously in various settings to facilitate healthcare communication and delivery, including as appointment reminders, adjuncts to asthma symptom reporting, and epidemiologic surveillance during a pandemic, among many others [1, 4, 5]. However, to our knowledge, this is the first use of an SMS system to collect patient-reported information on acute post-operative pain levels and opioid consumption.
There were several limitations to this study and our SMS platform. First, patients who do not own mobile phones capable of receiving and sending SMS messages could not participate. Second, an individual message could not exceed 160 characters, which limited the length and nature of questions we asked. Third, although the cost associated with sending a text message is small, at $0.0075 per message, it may vary depending on the service used and the volume of messages sent. Fourth, patient information regarding registry respondents was unavailable, and we cannot confirm that those who participated in the email registry are similar to those who participated in the SMS surveys. However, given the large scope of the institutional email registry, the fact that both patient groups were captured at the same hospital, and that age, BMI, and gender for patients enrolled in this study were similar to that of previously published data for all patients undergoing these procedures, we believe it is reasonable to compare these groups [6, 14]. Lastly, we did not uncover clear predictors for who would and would not respond to SMS surveys. A larger number of patients and of patient characteristics may yield significant associations that could better predict who may respond to SMS questionnaires after orthopedic surgery.
Historically, published response rates for large survey studies vary significantly, and while no specific response rate is considered universally valid, conclusions drawn from surveys with low response rates are more likely to be affected by sampling bias. In general, response rates above 80 to 90% are viewed favorably [7]. The ability to collect daily or twice-daily patient data outside of the hospital is largely unprecedented. In that light, the use of SMS surveys to collect acute post-operative patient-reported outcomes after orthopedic surgery seems viable. Other important benefits of an SMS data-capture system over traditional pen-and-paper surveys include reducing office flow disruptions and collecting more contemporaneous data and thus lowering the potential for recall bias. Possible reasons for improved patient response with the SMS system include the consistently timed daily messages, a back-end system that notified research staff of non-responsive patients, and the near ubiquity of mobile phones in our society.
In conclusion, traditional forms of data collection are inadequate to answer patients’ questions about expectations in the first days after hospital discharge or to help providers understand opioid use in that post-surgical period. To our knowledge, an SMS system that can provide real-time data collection with high response rates on an outpatient basis is unprecedented in the orthopedic literature. This novel SMS platform represents an application of a widely available technology to improve the measurement of post-operative outcomes after orthopedic surgery. This interactive SMS platform could in turn be used to enhance patient counseling, further our understanding of post-operative opioid use, and prompt new research questions as previously unknown trends are revealed.
Electronic supplementary material
(PDF 1.19 MB)
(PNG 1.51 MB)
Funding
This work was financially supported by a Hospital for Special Surgery surgeon-in-chief grant.
Conflict of Interest
Jeffrey G. Stepan, MD, Msc, Cynthia A. Kahlenberg, MD, and Jason L. Blevins, MD, declare that they have no conflicts of interest. Ajay Premkumar, MD, MPH, and Francis C. Lovecchio, MD, report a surgeon-in-chief grant from the Hospital for Special Surgery in support of this study. Todd J. Albert, MD, reports personal fees from Biomet, FacetLink, Gentis, JP Medical Publishers, Saunders/Mosby-Elsevier, United Healthcare, and Thieme; grants and personal fees from DePuy; stock ownership in ASIP, Biometrix, Breakaway Imaging, Crosstree, FacetLink, Gentis, In ViVo Therapeutics, Paradigm Spine, Spinicity, and Vertech; salary from Weill-Cornell Medical College (professor) and Hospital for Special Surgery (surgeon-in-chief); non-financial support from Scoliosis Research Society (president), Cervical Spine Research Society (past-president), American Orthopaedic Association; grants from AO Foundation/Association for the Study of Internal Fixation, Patient-Centered Outcomes Research Institute, International Spine Study Group, and National Institute of Arthritis and Musculoskeletal and Skin Diseases, all outside the submitted work. Michael B. Cross, MD, reports personal fees from Link Orthopaedics, Smith & Nephew, and Zimmer; personal fees and research support from Acelity, Exactech, Inc., and Flexion Therapeutics; stock or stock options from Imagen, Insight Medical, and Parvizi Surgical Innovation; and personal fees, research support, and stock or stock options from Intellijoint, all outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was obtained from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: IV
References
- 1.Berman A, Figueroa ME, Storey JD. Use of SMS-based surveys in the rapid response to the Ebola outbreak in Liberia: opening community dialogue. J Health Commun. 2017;22(sup1):15–23. doi: 10.1080/10810730.2016.1224279. [DOI] [PubMed] [Google Scholar]
- 2.Bream E, Charman SC, Clift B, Murray D, Black N. Relationship between patients’ and clinicians’ assessments of health status before and after knee arthroplasty. Qual Saf Health Care. 2010;19(6):e6. doi: 10.1136/qshc.2008.031310. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes—United States. Surveillance Special Report. U.S. Department of Health and Human Services. August 31, 2018. Available from https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf.
- 4.Christie A, Dagfinrud H, Dale Ø, Schulz T, Hagen KB. Collection of patient-reported outcomes—text messages on mobile phones provide valid scores and high response rates. BMC Med Res Methodol. 2014;14:52. doi: 10.1186/1471-2288-14-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyle R, Albright K, Hurley LP, Chávez C, Stowell M, Dircksen S, et al. Patient perspectives on a text messaging program to support asthma management: a qualitative study. Health Promot Pract. 2018;1524839918770209. [DOI] [PubMed]
- 6.Fang M, Noiseux N, Linson E, Cram P. The effect of advancing age on total joint replacement outcomes. Geriatr Orthop Surg Rehabil. 2015;6(3):173–179. doi: 10.1177/2151458515583515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon N. Solution corner: a question of response rate. Science Editor. 2002;25(1):25. [Google Scholar]
- 8.Gostin LO, Hodge JG, Noe SA. Reframing the opioid epidemic as a national emergency. JAMA. 2017;318(16):1539–1540. doi: 10.1001/jama.2017.13358. [DOI] [PubMed] [Google Scholar]
- 9.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–1806. doi: 10.1001/jama.2012.3532. [DOI] [PubMed] [Google Scholar]
- 10.Kjellsson G, Clarke P, Gerdtham U-G. Forgetting to remember or remembering to forget: a study of the recall period length in health care survey questions. J Health Econ. 2014;35:34–46. doi: 10.1016/j.jhealeco.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Nota SPFT, Strooker JA, Ring D. Differences in response rates between mail, e-mail, and telephone follow-up in hand surgery research. Hand (NY). 2014;9(4):504–510. doi: 10.1007/s11552-014-9618-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pew Research Center. Mobile fact sheet. Pew Research Center: Internet, Science and Technology. 2017 Jan 12. Available from http://www.pewinternet.org/fact-sheet/mobile/.
- 13.Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am. 2018;100(3):180–188. doi: 10.2106/JBJS.17.00672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh JA, Lewallen DG. Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care Res. 2014;66(6):897–906. doi: 10.1002/acr.22233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SRB. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305(13):1299–1301. doi: 10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells N, Pasero C, McCaffery M. Improving the quality of care through pain assessment and management. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available from http://www.ncbi.nlm.nih.gov/books/NBK2658/. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1.19 MB)
(PNG 1.51 MB)


