Abstract
Background
Resident physicians have been shown to possess negative attitudes toward individuals with substance use disorders (SUDs), even if the residents believe they have adequate knowledge and skills to care for these patients. Residents’ negative attitudes may have an adverse impact on patient engagement, treatment, and outcomes.
Questions/Purposes
The goal of this study was to examine the impact of an online training module on residents’ attitudes toward people with SUDs. We hypothesized that residents who received the educational intervention would show improved attitudes toward people with alcohol and opioid use disorders.
Methods
A web-based questionnaire, including demographic information and the Medical Condition Regard Scale (MCRS) about individuals with alcohol and opioid use disorders, was sent to internal medicine and psychiatry residents before and 6 months after they took an online training module on stigma toward individuals with SUDs.
Results
A total of 46 residents completed the initial questionnaire and 29 completed the follow-up questionnaire 6 months later. Attitudes toward individuals with SUDs, as reflected by an increase in MCRS scores, were improved 6 months after the online training module.
Conclusion
Residents’ attitudes toward individuals with SUDs improved after taking an online training module. This is encouraging, as studies have shown that attitudes toward individuals with SUDs tend to decline during residency training and negatively affect patient care. Larger studies are needed to determine if such online modules can improve attitudes of other groups of clinicians, result in sustained change over time, and improve patient outcomes.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-9643-3) contains supplementary material, which is available to authorized users.
Keywords: stigma, substance use disorders, addiction, opioids, education
Introduction
American medical education is confronting an urgent need to respond to the opioid crisis [2]. Drug-related hospital visits and deaths have more than doubled in the USA since 2000, with over 63,000 overdose deaths in 2016 [15, 23]. More than 20 million Americans met criteria for any substance use disorder (SUD) in the past year, including 15.7 million people with an alcohol use disorder and 7.7 million people with any illicit drug use disorder [10]. Resident physicians frequently encounter patients with SUDs and are caring for them in every specialty and at all levels of care. SUDs and the associated health consequences contribute to a significant clinical and public health burden. SUDs are associated with high emergency medical service utilization, infectious disease transmission, deleterious effects on every organ system, obstetrics and neonatal complications, impaired social and occupational functioning, legal system involvement, homelessness, and death.
While most medical schools and residency training programs address knowledge- and skills-based outcomes in SUD education, interventions are needed for targeting the stigma patients with SUDs face. Medical students and residents must graduate with new competencies that include interventions to reduce stigma and to better address the needs of individuals with SUDs.
Many physicians and medical trainees feel ill equipped to manage patients with SUDs, possess negative attitudes toward those withe SUDs, are pessimistic about the benefits of providing evidence-based treatment, and avoid working with patients with addictions [1, 3–6, 8, 16, 18, 22, 24–26, 28]. In fact, there is evidence that the attitudes of clinicians across specialties toward individuals with SUDs may be worse than their attitudes toward individuals with other chronic medical and psychiatric diagnoses, and these attitudes may worsen as resident physicians advance through the hidden curriculum of residency training programs [3, 5, 6, 17, 18, 20]. Clinicians might view individuals with SUDs as poorly motivated, manipulative, of lesser importance, and more dangerous or violent than other patients [1, 3–7, 9, 17, 18, 20, 26].
Such outlooks are related to prevalent societal attitudes, the perception of substance use as a moral failing, repeated negative experiences in caring for patients in acute intoxication or withdrawal, lack of exposure to individuals in recovery during medical training, and various other factors that further stigmatize those with SUDs [1, 3–7, 9, 16–18, 20, 26].
These attitudes can lead to reductions in provider involvement, depersonalized patient care, and low provider empathy [3–7, 9, 17, 18, 20, 26, 27]. Since research has established the existence of healthcare environments that are hostile to patients with SUDs, an active intervention targeting stigma and negative attitudes is a much-needed response to the opioid crisis in American medical education. Very few interventions are being studied or used in residency training, and none in surgical residency training, to improve clinicians’ attitudes toward individuals with SUDs. Several studies have examined brief interventions to improve attitudes, ranging from short educational conferences to programs targeting skill development [3, 13, 21]. Brief interventions in these studies improved attitudes temporarily; however, the duration of improvements was either unremarkable or unclear [3, 13, 21]. There is an apparent need for interventions targeting stigma with demonstrably durable effect.
The goal of this study was to examine the effect of a brief, one-time online training module on residents’ attitudes toward individuals with SUDs at 6-month post-intervention. We hypothesized that residents’ attitudes toward individuals with alcohol and opioid use disorders would improve after they received our educational intervention, since the module addresses a number of deficits in current residency training.
Methods
The Weill Cornell Medicine Institutional Review Board approved the study. An online training module was created based on past research on clinicians’ attitudes toward individuals with SUDs [3–6]. The module provided information on how clinicians’ attitudes toward individuals with SUDs are worse than their attitudes toward people with other medical and psychiatric conditions, explaining why this has developed (stigma, the view that substance use is a moral failing as opposed to a brain disease, prior challenging personal and clinical experiences, for example). The module also featured videos of individuals in recovery from SUDs and family members of individuals with SUDs discussing their hopeful and challenging experiences with clinicians. Lastly, it provided links to resources for more information on treating individuals with SUDs. Psychiatry and internal medicine residents in their first post-graduate year (PGY 1) were sent a link to view this 8-m module at the beginning of their residency year.
An online questionnaire was created, using a web-based survey tool (SurveyMonkey.com, LLC, San Mateo, CA, USA). The questionnaire was sent to all PGY 1 psychiatry and internal medicine residents at our institution before starting residency and viewing the online training module and then again 6 months later. The questionnaire comprised two sections: (a) demographic information, which included information about level of training, and (b) the 11-item Medical Condition Regard Scale (MCRS) for individuals with two different diagnoses, designed to assess the degree to which clinicians find individuals with a given medical condition to be “enjoyable, treatable, and worthy of medical resources” [12]. The MCRS is a valid and reliable 11-item instrument graded on a 6-point Likert scale [12]. Higher scores on the MCRS indicate higher report of enjoyment, perceived treatability, and belief in the utility of dedicating medical resources for a given condition. These measures are used as a proxy for attitude. The two diagnoses were alcohol use disorder and opioid use disorder.
Statistical Analysis
Respondents’ age, gender, specialty, and percentage of patients diagnosed with SUDs in a typical work week were described as N (%) within the pre- and post-online training module groups. Missing demographic data were present for certain fields, but data were described with missingness and not imputed. Survey answers regarding each patient population within the pre- and post-groups were also described as N (%). Survey answers were subsequently converted to numeric values after reverse scoring of questions 1, 2, 4, 9, and 11; scores were reported as the mean Likert score (i.e., the total Likert score for 11 items was divided by 11 to give the numeric value). Higher scores represented better attitudes. Wilcoxon rank-sum tests were used to compare the total scores between the pre- and post-groups for each patient population. The total MCRS scores were calculated as the average of the 11 individual survey answers. Subsequently, the total scores between the two patient populations were analyzed by Wilcoxon signed-rank tests for both the pre- and post-groups. To control for the fact that residents in the post-group reported a higher percentage of patients diagnosed with SUDs in a typical work week, multivariable linear models for each patient population were constructed, controlling for this factor. All p values were two-sided with statistical significance evaluated at the 0.05 alpha. Analyses were performed in R, version 3.4.3 (Vienna, Austria).
Results
Most study respondents were in their late 20s, and more were female than male (Table 1). A total of 46 residents completed the initial survey, with more participation from internal medicine residents given the bigger size of their residency class (internal medicine n = 35, 76%; psychiatry n = 9, 20%; two did not specify specialty). A total of 29 residents completed the post-online training survey (internal medicine n = 23, 79%; psychiatry n = 5, 17%; one did not specify specialty). In both the pre- and post-online training module groups, most participants were younger than age 35 (91% and 89%, respectively). More women (54 and 55% in the pre- and post-intervention groups, respectively) than men (41 and 41%, respectively) participated. No significant differences between the groups were found based on gender or age. The post-online training group, which was surveyed 6 months into PGY 1, reported working with more patients with SUDs, with 19 residents (66%) stating that more than 15% of their patients had an SUD in the last week vs. ten residents (22%) reporting that more than 15% of their patients had an SUD at the beginning of the year.
Table 1.
Demographics
| Age | Pre-video | Post-video |
| No answer | 1 (2%) | 1 (3%) |
| 18–24 | 0 (0%) | 1 (4%) |
| 25–34 | 42 (93%) | 25 (89%) |
| 35–44 | 2 (4%) | 2 (7%) |
| 45–54 | 1 (2%) | 0 (0%) |
| Gender | Pre-video | Post-video |
| No answer | 2 (4%) | 1 (3%) |
| Female | 25 (54%) | 16 (55%) |
| Male | 19 (41%) | 12 (41%) |
| In the last typical work week, % of pts. with SUDs | Pre-video | Post-video |
| No answer | 15 (33%) | 1 (3%) |
| < 10 | 12 (39%) | 4 (14%) |
| 10–15 | 9 (29%) | 5 (18%) |
| > 15 | 10 (32%) | 19 (68%) |
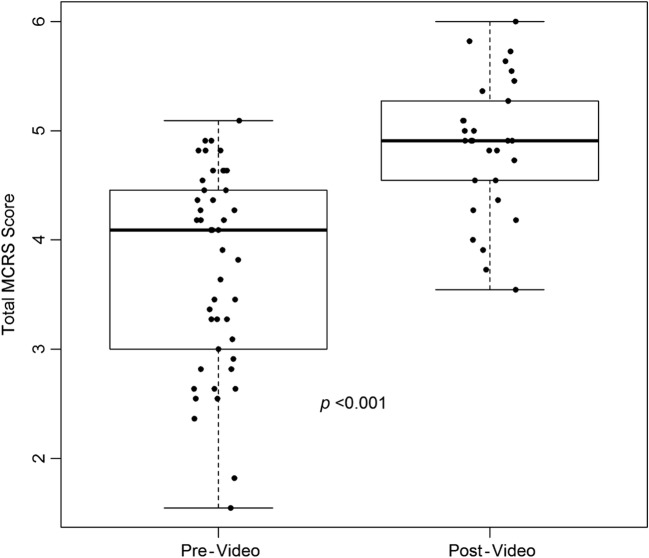
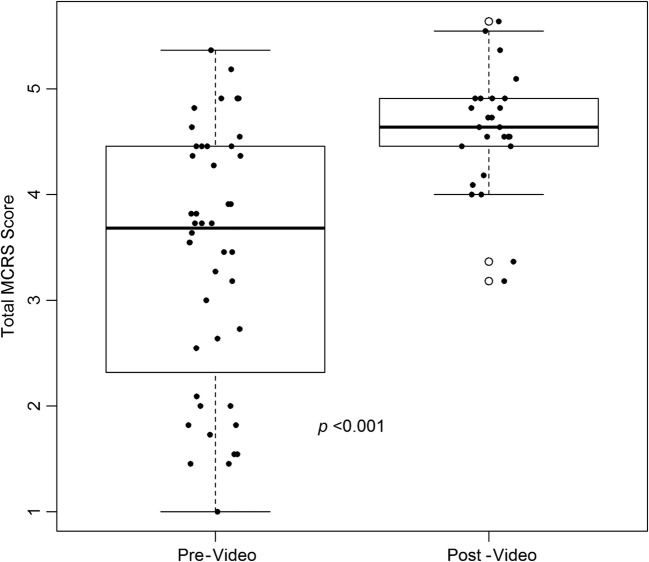
Attitudes toward individuals with alcohol and opioid use disorders, as reflected by an increase in MCRS scores, were improved 6 months after the online training module (Figs. 1 and 2). The mean MCRS scores increased from 3.74 to 4.86 and median scores from 4.09 to 4.91 for individuals with alcohol use disorder (p < 0.001). The mean MCRS scores increased from 3.41 to 4.61 and median scores from 3.68 to 4.64 for individuals with opioid use disorder (p < 0.001). In both groups, median scores were higher regarding those with alcohol use disorder than those with opioid use disorder (4.09 vs. 3.68, p < 0.001; 4.91 vs. 4.64, p = 0.004). There were no significant differences between the attitudes of internal medicine and psychiatry residents for either patient population. After controlling for the percentage of patients with an SUD seen in the last week, respondents in the post-online training group demonstrated an average 1.07 (p < 0.001) greater MCRS score regarding individuals with alcohol use disorder and an average 1.29 (p < 0.001) greater MCRS score regarding individuals with opioid use disorders.
Fig. 1.
ᅟThe total Medical Condition Regard Scale (MCRS) scores for alcohol use disorder patients, pre-video vs. post-video.
Fig. 2.
ᅟThe total Medical Condition Regard Scale (MCRS) scores for opioid use disorder patients, pre-video vs. post-video.
Discussion
As hypothesized, we found that resident physicians demonstrated improvement in MCRS scores for patients with SUDs when assessed 6 months after the educational intervention. These results provide important preliminary evidence for the efficacy of a simple intervention in improving resident physicians’ attitudes toward patients with addictions, an outcome that other studies have shown may improve patient outcomes and experiences [3–7, 9, 17, 18, 20, 26, 27]. The magnitude of improvement in MCRS scores is particularly noteworthy; it is greater than the improvement attributable to addiction-focused clerkships in medical school [3, 5, 6, 17, 18, 20].
As with previous studies, ours is limited by a low survey response rate and by the unreliable nature of self-report [16, 18]. The anonymous surveys made it impossible to pair the same respondents in statistical analyses. Furthermore, our sample may not generalize to the full population of medical residents, including surgery and anesthesia residents who frequently prescribe opioids and treat patients in pain. We used the MCRS as a proxy for the more meta-cognitive concept of personal attitudes, noting that there are likely both positive and negative cognitions, affects, and behaviors that this instrument does not detect. Other factors may have led to improved attitudes, including better societal and clinical attitudes toward patients with SUDs, a possible result of greater media coverage and government response to the opioid crisis. Nonetheless, recent studies indicate that clinicians’ attitudes are largely negative and worsen over time [6].
The online module resulted in improved attitudes, we believe, by providing residents clear information they might not otherwise have encountered in their explicit or hidden medical curricula. Specifically, the module increased awareness that their own attitudes might be negative toward patients with SUDs and offered reasons. The module also offered resources for providing better care to individuals with SUDs and exposure to people in recovery. Each of these components was included in the design of the module in response to the hypothesized deficits in residency curricula.
The relative dearth of successful attitudinal interventions makes these results especially encouraging. Furthermore, that improvement remained at 6-month post-intervention suggests the possibility of longer term attitude modification.
Notably, although residents’ attitudes toward patients with opioid use disorder greatly improved, they were more negative than attitudes toward patients with alcohol use disorder, both before and after the intervention. This might be related to the known risks of opioid use, to negative clinical experiences, and to poorer outcomes [7, 9, 13, 14, 19, 20, 27]. It also represents a challenge for medical educators in addressing the opioid crisis; despite the availability of effective treatments, providers caring for patients with opioid use disorder often have flagging enthusiasm for them, even relative to patients with other SUDs. Without favorable relations with clinicians, people with opioid use disorder may be less likely to engage in and access treatment—this is concerning, given that opioid use disorder poses a greater risk of death from accidental overdose, trauma, suicide, or infectious disease than other substance use disorders. Further research is needed to understand how resident physicians perceived differences in attitudes for individuals with alcohol and opioid use disorders. Drivers of these perceptual differences could inform the design of future interventions for patients.
Future research directions include allowing longer-term follow-up of resident physicians after they take the online modules. A design including separate, parallel interventions, such as exposure to patients in recovery and education on provider stigma, would permit distinct intervention mediators to be identified and enhanced. Study is also needed in tailoring education to specific clinicians and determining its efficacy on changing specific outcomes, such as providers’ behavior, their interpersonal styles with patients with SUD, and their likelihood of engaging patients in treatment. Additionally, tailoring the modules to specific SUDs might be indicated, given the differing clinical experience and outcomes among SUDs, which might have contributed to our findings of more positive attitudes toward individuals with alcohol use disorder than with opioid use disorder.
In conclusion, our public health mandate to care for people with SUDs has gained momentum with the opioid epidemic. Previous work has demonstrated that caregivers’ attitudes toward people with addiction are important in driving patient outcome and that residents’ attitudes worsen over the course of training. We set out to study whether a simple online educational module could improve residents’ attitudes toward people with SUDs and, ideally, improve patient outcomes. We found that the attitudes of a small group of internal medicine and psychiatry residents toward individuals with alcohol and opioid use disorders improved after an online training module. Unfortunately, but interestingly, the improvement was more robust in attitudes toward those with alcohol use disorders than those with opioid use disorders. Future research should examine this difference.
Additionally, although this is a very small study, it did examine the usefulness of the same module in two specialties, internal medicine and psychiatry, with strong and lasting effects in both cases. However, surgical and other residents should be tested, particularly given the post-operative pain management needs of surgical patients. For example, Chiu and colleagues recently reported that surgical residents rely nearly exclusively on opioids for managing post-surgical pain, “often in excessive amounts,” and that they lack the education to change prescribing patterns [11]. Larger studies are needed to determine if such online modules can improve attitudes of other groups of clinicians and result in sustained change over time—and ultimately, improved outcomes for patients with SUDs.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 382 kb)
(PDF 189 kb)
Conflict of Interest
Jonathan Avery, MD, Daniel Knoepflmacher, MD, Kristopher A. Kast, MD, Miranda Greiner, MD, MPH, Joseph Avery, JD, and Julie B. Penzner, MD, declare that they have no conflicts of interest. Elizabeth Mauer, MS, reports partial support from a grant from the Clinical and Translational Science Center at Weill Cornell Medicine (UL1-TR000457-06), outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all subjects for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Adams MW. Comorbidity of mental health and substance misuse problems: a review of workers’ reported attitudes and perceptions. J Psychiatr Ment Health Nurs. 2008;15(2):101–108. doi: 10.1111/j.1365-2850.2007.01210.x. [DOI] [PubMed] [Google Scholar]
- 2.American Association of Medical Colleges. Responding to the opioid epidemic through education, patient care, and research. AAMCNews: Current Key Issues. 2018. Available from https://news.aamc.org/for-the-media/article/medical-schools-address-opioid-epidemic/
- 3.Avery J, Zerbo E. Improving psychiatry residents’ attitudes toward individuals diagnosed with substance use disorders. Harv Rev Psychiatry. 2015;23(4):296–300. doi: 10.1097/HRP.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 4.Avery J, Dixon L, Adler D, et al. Psychiatrists’ attitudes toward individuals with substance use disorders and serious mental illness. J Dual Diagn. 2013;9(4):322–326. doi: 10.1080/15504263.2013.835165. [DOI] [Google Scholar]
- 5.Avery J, Zerbo E, Ross S. Improving psychiatrists’ attitudes towards individuals with psychotic disorders and co-occurring substance use disorders. Acad Psychiatry. 2016;40(3):520–522. doi: 10.1007/s40596-015-0361-6. [DOI] [PubMed] [Google Scholar]
- 6.Avery J, Han BH, Zerbo E, et al. Changes in psychiatry residents’ attitudes towards individuals with substance use disorders over the course of residency training. Am J Addict. 2017;26(1):75–79. doi: 10.1111/ajad.12406. [DOI] [PubMed] [Google Scholar]
- 7.Ballon BC, Skinner W. “Attitude is a little thing that makes a big difference”: reflection techniques for addiction psychiatry training. Acad Psychiatry. 2008;32(3):218–224. doi: 10.1176/appi.ap.32.3.218. [DOI] [PubMed] [Google Scholar]
- 8.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the cage questionnaire. Am J Med. 1987;82(2):231–235. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 9.Capurso NA, Shorter DI. Changing attitudes in graduate medical education: a commentary on Attitudes Towards Substance Use and Schizophrenia by Avery et al. Am J Addict. 2017;26(1):83–86. doi: 10.1111/ajad.12485. [DOI] [PubMed] [Google Scholar]
- 10.Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51). 2016. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf
- 11.Chiu AS, Healy JM, DeWane MP, Longo WE, Yoo PS. Trainees as agents of change in the opioid epidemic: optimizing the opioid prescription practices of surgical residents. J Surg Educ. 2018;75(1):65–71. doi: 10.1016/j.jsurg.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 12.Christison GW, Haviland MG, Riggs ML. The medical condition regard scale: measuring reactions to diagnoses. Acad Med. 2002;77(3):257–262. doi: 10.1097/00001888-200203000-00017. [DOI] [PubMed] [Google Scholar]
- 13.D’Onofrio GD, Nadel E, Degutis L, et al. Improving emergency medicine residents’ approach to patients with alcohol problems: a controlled educational trial. Ann Emerg Med. 2002;40(1):50–62. doi: 10.1067/mem.2002.123693. [DOI] [PubMed] [Google Scholar]
- 14.Degenhardt L, Larney S, Kimber J, Farrell M, Hall W. Excess mortality among opioid-using patients treated with oral naltrexone in Australia. Drug Alcohol Rev. 2015;34:90–96. doi: 10.1111/dar.12205. [DOI] [PubMed] [Google Scholar]
- 15.Doherty N, Gottlieb S, McCance-Katz E, Schuchat A, Volkow N. Federal efforts to combat the opioid crisis: a status update on CARA and other initiatives. Testimony to Congressional Senate Committee on Health, Education, Labor & Pensions. 2017. Available from https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2017/federal-efforts-to-combat-opioid-crisis-status-update-cara-other-initiatives
- 16.Fiellin DA, Reid MC, O’Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med. 2000;160(13):1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- 17.Geller G, Levine DM, Mamon JA, et al. Knowledge, attitudes, and reported practices of medical students and house staff regarding the diagnosis and treatment of alcoholism. JA.MA. 1989;262(21):3115–3120. [PubMed] [Google Scholar]
- 18.Gilchrist G, Moskalewicz J, Slezakova S, et al. Staff regard towards working with substance users: a European multi-centre study. Addiction. 2011;106(6):1114–1125. doi: 10.1111/j.1360-0443.2011.03407.x. [DOI] [PubMed] [Google Scholar]
- 19.Hser YI, Saxon AJ, Huang D, et al. Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction. 2014;109:79–87. doi: 10.1111/add.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindberg M, Vergara C. Wild-Wesley, et al. Physicians-in-training attitudes toward caring for and working with patients with alcohol and drug abuse diagnoses. South Med J. 2006;99(1):28–35. doi: 10.1097/01.smj.0000197514.83606.95. [DOI] [PubMed] [Google Scholar]
- 21.Maher KH, Nereberg L, Bower KJ. Modifying residents’ professional attitudes about substance abuse treatment and training. Am J Addict. 2001;10(1):40–45. doi: 10.1080/105504901750160466. [DOI] [PubMed] [Google Scholar]
- 22.Miller NS, Sheppard LM, Colenda CC, Magen J. Why physicians are unprepared to treat patients who have alcohol- and drug-related disorders. Acad Med. 2001;76(5):410–418. doi: 10.1097/00001888-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 23.National Institute on Drug Abuse. Health consequences of drug misuse. 2017. Available from https://www.drugabuse.gov/related-topics/health-consequences-drug-misuse
- 24.Rao H, Mahadevappa H, Pillay P, Sessay M, Abraham A. A study of stigmatized attitudes towards people with mental health problems among health professionals. J Psychiatr Ment Health Nurs. 2009;16(3):279–284. doi: 10.1111/j.1365-2850.2008.01369.x. [DOI] [PubMed] [Google Scholar]
- 25.Renner JA. How to train residents to identify and treat dual diagnosis patients. Biol Psychiatry. 2004;56(10):810–816. doi: 10.1016/j.biopsych.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Richmond IC, Foster JH. Negative attitudes towards people with co-morbid mental health and substance misuse problems: an investigation of mental health professionals. J Ment Heal. 2003;12(4):393–403. doi: 10.1080/0963823031000153439. [DOI] [Google Scholar]
- 27.Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–3):23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Wakeman SE, Pham-Kanter G, Donelan K. General internists’ attitudes, practices and preparedness related to substance use disorder. J Gen Intern Med. 2016;31(2):S231–S232. doi: 10.1080/08897077.2016.1187240. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 382 kb)
(PDF 189 kb)