Abstract
Background
Elective total joint arthroplasty may be a gateway to long-term opioid use.
Questions/Purpose
We sought to review the literature on multimodal and regional analgesia as a strategy to minimize perioperative opioid use and control pain in patients undergoing total hip arthroplasty (THA) or total knee arthroplasty (TKA).
Methods
We conducted a narrative review to assess the state of the evidence informing opioid-sparing analgesics for THA and TKA. A PubMed search was conducted for English-language articles published before April 2018. We preferentially included well-designed randomized controlled trials, systematic reviews, and meta-analyses. Where the highest levels of evidence were not yet apparent, we evaluated retrospective and/or observational studies.
Results
Multimodal analgesia emphasizing nonsteroidal anti-inflammatory agents and acetaminophen is associated with decreases in perioperative opioid use for THA and TKA. Regional analgesia, including peripheral nerve blocks and local infiltration analgesia, is also associated with decreased perioperative opioid use for THA and TKA. Emerging topics in post-arthroplasty analgesia include (1) the value of nonsteroidal anti-inflammatory drugs, (2) the use of peripheral nerve catheters and extended-release local anesthetics to prolong the duration of opioid-free analgesia, and (3) novel peripheral nerve blocks, exemplified by the IPACK (interspace between the popliteal artery and posterior capsule of the knee) block for TKA.
Conclusions
The use of multimodal analgesia with regional techniques may decrease perioperative opioid use for patients undergoing THA and TKA. These techniques should be part of a comprehensive perioperative plan to promote adequate analgesia while minimizing overall opioid exposure.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-9652-2) contains supplementary material, which is available to authorized users.
Keywords: opioid crisis, orthopedic surgery, total joint arthroplasty, multimodal analgesia, regional analgesia, peripheral nerve block
Introduction
Surgery is a potential risk factor for new long-term opioid use. A recent database study comparing opioid-naïve US adults undergoing surgery to a nonoperative control cohort found a significantly higher incidence of new persistent opioid use in surgical patients (approximately 6%) than in nonsurgical patients (0.4%) [8]. Orthopedic surgery, including total joint arthroplasty (TJA), has been particularly associated with long-term opioid use and misuse [88]. The rising demand for total hip arthroplasty (THA) and total knee arthroplasty (TKA) mandates strategies to minimize opioid exposure and protect patients from long-term opioid dependence [65].
It follows that decreasing perioperative opioid exposure may contribute to a decrease in postdischarge opioid use. Multimodal nonopioid analgesia has recently been shown to decrease postoperative opioid prescribing by over 18.5% after elective THA and TKA [73]. Elements of a multimodal analgesia regimen for TJA typically include the use of regional techniques (peripheral nerve blocks, catheters, and local infiltration analgesia) combined with systemic analgesics (acetaminophen, ketamine, and nonsteroidal anti-inflammatory drugs [NSAIDs]) [89]. Each has been shown to independently decrease perioperative opioid consumption, while facilitating analgesia after a variety of surgical procedures [51]. We reviewed the evidence on multimodal and regional analgesia in decreasing perioperative opioid use for elective TJA.
Methods
We conducted a review of the literature to examine the latest evidence on the following question: Which nonopioid analgesics provide adequate pain control while minimizing opioid consumption after THA or TKA? Literature reviews for each individual analgesic were performed in PubMed for English-language articles published before April 2018. Each search initially targeted THA and TKA. If no THA- or TKA-specific literature was identified, the search was broadened to surgical procedures in general and the relevant articles extracted. Given the volume of literature in this field, a hierarchical method of inclusion was employed based on study design. If we identified a well-designed systematic review (SR) or meta-analysis (MA), the study was included. Where the highest levels of evidence were lacking, we included randomized controlled trials (RCTs), observational studies, or cohort studies. Results are described narratively.
Results
Systemic Multimodal Analgesia
The concurrent use of nonopioid systemic analgesics may provide additive or synergistic effects on pain control while minimizing opioid use and opioid-related adverse effects. Commonly studied classes of nonopioid systemic analgesics include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), N-methyl-D-aspartate (NMDA) receptor antagonists, and gabapentinoids.
Nonsteroidal Anti-inflammatory Drugs
TKA
There are two RCTs [80, 83], one observational trial [43], and one MA [58] examining the use of oral (PO) and intravenous (IV) NSAIDs (including cyclooxygenase-2 [COX-2] inhibitors) for the treatment of pain after TKA. Results indicate that the use of NSAIDs is associated with a reduction in pain scores and a significant opioid-sparing effect—a benefit that was confirmed for opioid-naïve and opioid-tolerant patients [43].
THA
There are no large-scale RCTs or SRs of the analgesic efficacy of preoperative NSAIDs in THA surgical patients. There is one SR examining the use of NSAIDs for postoperative pain after THA, which associated NSAIDs with significantly lower pain scores and opioid requirements [34].
NSAIDs have an analgesic ceiling and may be associated with platelet dysfunction, gastrointestinal irritation/bleeding, and renal dysfunction. Despite these concerns, an MA of 27 RCTs involving a variety of surgical procedures [26] and a postmarketing study of ketorolac [94] indicate that NSAIDs are not associated with an increase in postoperative bleeding.
Acetaminophen
TKA
There are two retrospective observational studies of IV acetaminophen in TKA. Neither study found an analgesic benefit nor any reduction in perioperative opioid use [44, 75]. There is one RCT comparing PO and IV acetaminophen to placebo in patients receiving comprehensive multimodal analgesia and spinal anesthesia [76]. There were no additional analgesics or opioid-sparing benefits of acetaminophen.
THA
One study examined a single dose of postoperative IV acetaminophen in patients undergoing THA [86]. It significantly reduced pain scores and opioid consumption.
Combined THA/TKA Studies
There are three SR/MAs of PO and/or IV acetaminophen analyzed in combined THA and TKA cohorts [7, 95, 107]. When added to multimodal analgesia, IV acetaminophen reduced pain and opioid consumption after TJA [107] and when compared to placebo [57]. One SR/MA comparing PO to IV acetaminophen failed to find any difference between route of administration and pain scores or opioid consumption [95].
Gabapentinoids
TKA
Two MAs associate perioperative gabapentinoids with a decrease in opioid consumption after TKA [18, 31]. However, the analgesic benefits described are inconsistent, with one MA concluding no decrease in pain with ambulation or improvement of knee flexion in patients receiving gabapentinoids [31] and the other concluding analgesic benefits [18]. A minority of the numerous RCTs/observational trials studying gabapentinoids in TKA demonstrated a decrease in postoperative pain [52, 74]. When added to a comprehensive multimodal analgesic regimen, a recent RCT concluded, gabapentin provided no additional analgesic benefits [105].
THA
There are four RCTs [12, 13, 78, 110] and two MAs [32, 64] of perioperative gabapentin for THA. Three RCTs [13, 78, 110] failed to show a decrease in perioperative opioid consumption with gabapentinoids. The MAs suggested an opioid-sparing capacity for gabapentinoids, but the analgesic benefit was inconsistent. In one RCT, when gabapentin was added to a comprehensive multimodal analgesic regimen, no clinically important reductions in postoperative morphine consumption, pain scores, opioid-related side effects, or functional improvements were found [78].
Other Analgesic Agents
N-Methyl-D-Aspartate Receptor Antagonists
NMDA receptors have been implicated in nociceptive processing. Clinically available NMDA receptor antagonists include ketamine, magnesium, and dextromethorphan.
Ketamine
TKA
There are three RCTs/observational trials examining IV ketamine in TKA [2, 5, 79]. Taken together, results suggest that addition of low-dose (sub-anesthetic) IV ketamine may decrease postoperative pain, decrease opioid consumption, and improve mobilization after TKA.
THA
There is one RCT examining the role of ketamine in THA [81]. Use of ketamine significantly decreased opioid consumption at 24-h post-surgery, facilitated rehabilitation at 1 month, and decreased postoperative chronic pain up to 6 months after THA.
Magnesium and Dextromethorphan
There are no studies specifically examining either of these agents in TKA/THA. However, data from MAs in primarily nonorthopedic patients suggest that use of IV magnesium infusion in the perioperative period [14] or oral dextromethorphan [47] are independently associated with a decrease in postoperative pain and opioid consumption.
Lidocaine
TKA
There are no studies specifically examining the use of IV lidocaine in patients undergoing TKA.
THA
There is one RCT examining the use of IV lidocaine in patients undergoing THA [67]. Compared to saline, IV lidocaine (1.5 mg/kg bolus, followed by 1.5 mg/kg/h infusion) did not offer analgesic benefits on postoperative pain scores.
Non-TKA/THA
There are three MAs [46, 48, 100] examining perioperative IV lidocaine infusions in nonorthopedic surgical procedures. Taken together, results suggest that perioperative IV lidocaine infusions may be associated with decreased postoperative pain, reduced opioid consumption, and earlier return of gastrointestinal function.
Regional Analgesia
Use of local-anesthetic-based techniques may provide mid-to-long-duration opioid-free analgesia. Commonly studied regional analgesic methods include peripheral nerve blocks, catheters, extended-duration local anesthetics, and surgeon-administered local infiltration analgesia.
Epidural Analgesia
Compared to systemic opioid analgesia, epidural analgesia is associated with superior pain control, an opioid-sparing benefit, and fewer opioid-related adverse effects after THR and TKA, two MAs show [7, 101]. These benefits appear to extend well into the postoperative period but disappear by 18 to 24 h after surgery.
A recent SR confirmed the findings from these MAs but highlighted several liabilities of epidural analgesia [11]. Important side effects of epidural analgesia include higher risk of motor/sensory block, delayed ambulation, urinary retention, and hypotension. Additional concerns include how to manage anticoagulation in the setting of an epidural catheter, and how practice settings lacking comprehensive regional anesthesia services can safely and effectively manage an epidural program [35].
Peripheral Nerve Blocks
In recent years, there has been a shift toward the use of peripheral nerve blocks (PNB) and peripheral nerve catheters (PNCs) to control pain while avoiding some liabilities of epidural analgesia.
TKA
Distributions of the femoral and sciatic nerves are targeted for PNB after TKA. Two MAs compare PNB to epidural analgesia after TKA [22, 25]. The literature additionally includes 20 MAs [1, 3, 17, 21, 24, 27, 36, 40, 50, 54–56, 60, 61, 70, 77, 98, 99, 109, 112], three SRs [4, 10, 104], and three large-scale observational studies [23, 69, 72] of combinations of PNBs and local-anesthetic infiltration techniques for analgesia and opioid-sparing capacity after TKA. Compared to placebo (or no-block), all PNBs studied provide superior analgesia and reduce IV patient-controlled analgesia (PCA), opioid consumption, and opioid-related adverse effects [1, 10, 27, 77, 104]. Importantly, the analgesia provided by PNBs appears to be comparable to epidural techniques but without the adverse effects and pragmatic pitfalls described above [11, 22, 25].
Classically, femoral nerve block (FNB) has been performed for post-TKA analgesia. An early SR on the relative benefits compared FNB to any other analgesic technique [10]. FNB was superior to opioid-containing IV PCA and equivalent to epidural for post-TKA analgesia, opioid consumption, and nausea/vomiting. The main drawback to FNB is motor weakness and concomitant increased risk of falls [71].
The adductor canal block (ACB) may offer motor nerve-sparing benefits and has been studied as an alternative to FNB in this regard. Nine MAs compare FNB to ACB for analgesia and fall risk after TKA [17, 24, 36, 40, 50, 55, 56, 99, 112]. Overall, the results suggest that ACB offers at least equivalent analgesia, but with superior ambulation potential, less quadriceps weakness, and faster recovery after TKA than FNB.
According to the conclusions of two SR/MAs [27, 61] and one MA [1], adding a sciatic nerve block to FNB [1, 27] or local infiltration analgesia [61] (vs. either alone) provides additional analgesia and further reduces postoperative opioid consumption after TKA. However, the body of evidence for sciatic nerve block has been described as overall low quality [87]. Given that sciatic nerve block can delay physical therapy and ambulation after TKA, well-designed prospective RCTs on the risks and benefits of sciatic nerve block are needed [61].
An alternative approach to target posterior knee pain after TKA has recently been described. The interspace between the popliteal artery and posterior capsule of the knee (IPACK) block delivers local anesthetic to the posterior aspect of the knee, providing analgesia while preserving motor strength [19]. One retrospective study [97] and one prospective cohort trial [82] evaluate the role of IPACK for TKA. Results for analgesia and opioid consumption were mixed, with one study suggesting improved pain scores (but no effect on opioid consumption) [82], and the other suggesting reduced opioid consumption, but no effect on pain scores [97]. However, both studies concluded IPACK plus ACB optimized physical therapy outcomes and shortened length of hospital stay.
Peripheral Nerve Catheters
The preceding discussion highlights effective analgesia strategies in the immediate postoperative period. However, there is significant unmet clinical need to provide ongoing analgesia beyond the duration of epidural/PNBs. Accordingly, research into methods for extending the duration of PNBs has focused on the role of PNCs.
There are two narrative reviews on the use of PNCs for analgesia for a range of indications, including TKA/THA [38, 39]. The updated review included six RCTs exploring the use of adductor canal PNC after TKA [39]. Evidence was mixed for analgesia, ambulation, and opioid consumption. The author called for research into the role and utility of PNC for TKR as a priority. An accompanying editorial suggested the state of the evidence was limited to recommend PNCs routinely for TJA; although there is much benefit suggested by PNC programs, unresolved questions requiring further research include how to determine the optimal composition, duration, and value of PNC, given the resource-intense requirements [90]. Since that time, one RCT has compared ACB with adjuvant to PNC in TKA [53]. Pain scores were noninferior in the ACB group, and there were no differences in opioid consumption up to 48-h post-TKA. The authors concluded that single-shot ACB with adjuvants to extend duration may represent the more viable option for fast-track discharge after TKA.
THA
For THA, options for PNBs and PNCs include psoas compartment/lumbar plexus block, fascia iliaca block, and sciatic nerve block [63].
We identified one MA [34] and five additional RCTs [37, 66, 84, 93, 106] examining the use of lumbar plexus block/catheters for post-THA analgesia. Taken together, the data indicates that the use of a lumbar plexus block/catheter is associated with significant reductions in postoperative pain scores and opioid consumption. The optimal choices of local anesthetic, dose, and duration for lumbar plexus block/catheters for THA are currently unknown. The risk of falls caused by lumbar plexus block is also uncertain but should be considered in high-risk patients [42].
One MA compares FNB to fascia iliaca block for pain scores and opioid consumption after THA and TKA [103]. No differences were seen in either outcome, or in opioid-related side effects. The authors urge caution in interpretation of the underlying studies (described as at significant risk of bias) and calling for more high-quality large RCTs with longer follow-up intervals.
Local Infiltration Analgesia/Periarticular Analgesia
Intraoperative infiltration of local anesthetics into the surgical field or around the joint space is a technique performed by surgeons for postarthroplasty analgesia.
TKA
One SR [4] and seven MAs [3, 21, 56, 60, 70, 98, 109] suggest local infiltration analgesia (LIA)/periarticular analgesia (PAI) offers equivalent analgesia to PNBs or epidurals at rest, but inferior analgesia with movement. Opioid consumption and related side effects appear to be similar between the techniques. These results need to be interpreted with caution, however, because of significant methodological issues in the majority of the included studies [4, 87].
THA
There are four SRs [34, 41, 68, 108], two RCTs [33, 92], and two observational studies [6, 45] examining the use and value of LIA/PAI for THA. Four additional RCTs [9, 15, 59, 91] were incorporated into the SRs referenced above [34, 41, 68, 108]. Taken together, the preponderance of data suggests that LIA/PAI reduces postoperative pain scores and opioid consumption and minimizes opioid-related adverse effects when compared to placebo or no LIA/PAI. It is unknown how LIA/PAI may add benefit to comprehensive multimodal analgesia regimens. Additionally, the optimal composition (including choice of local anesthetic and adjuvants), dose, location, and method of injection are currently unclear.
Continuous-Release Local Anesthetics
Continuous-release local anesthetics are increasingly being trialed for postarthroplasty analgesia. Liposomal bupivacaine (LB) is a novel formulation which provides slow-release bupivacaine (up to 72 h). LB is approved by the US Food and Drug Administration for LIA. There are contradictory data regarding the analgesic benefits of LB for joint arthroplasty: a Cochrane review showed LB is associated with superior analgesia and significant opioid reduction compared to placebo (in mixed surgical subtypes but including TJA) [30]. However, when compared to plain bupivacaine hydrochloride, there were no benefits in pain scores, opioid consumption, or length of hospital stay.
TKA
Three MAs compare LB to placebo- or local-anesthetic-based PAI [49, 85, 102]. One failed to conclude a clear clinical advantage [85] and the other showed no benefit of LB for pain and functional outcomes after TKA [49]. In contrast, the third associated LB with superior analgesia and opioid-sparing benefits after TKA, when compared to placebo [102]. Several methodologic issues combine to confer a very high risk of bias, including low overall volume and quality of the included studies and conflict of interest concerns regarding sponsorship of studies [30].
Although not currently approved for use in PNBs, there is one RCT comparing FNB with LB versus placebo for post-TKA analgesia and opioid use [28]. LB provided superior analgesia and minimized opioid consumption up to 48 h after surgery.
THA
Two MAs compare LB to plain bupivacaine-PAI for THA [62, 111]. In both, LB significantly reduces pain scores and opioid consumption up to 48 h after THA. In addition, there was a significantly decreased incidence of nausea and vomiting in patients receiving LB. The overall quality of evidence was rated as low or very low, suggesting further well-designed trials are needed, and are likely to alter confidence in the effect. Additionally, all the included studies were small and retrospective in design.
Discussion
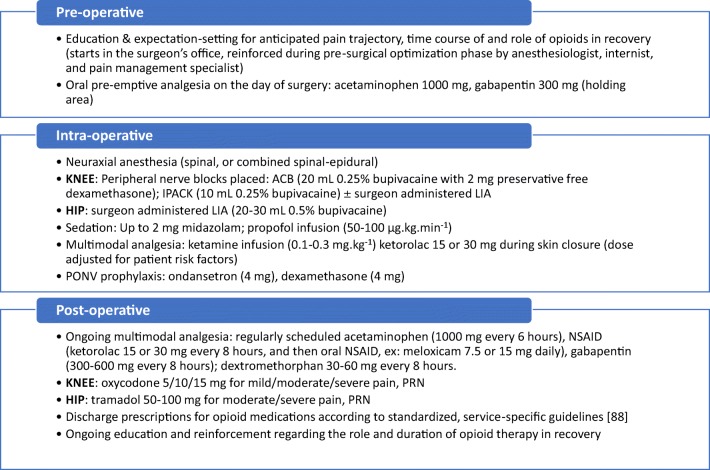
Elective TJA may be an entry to prolonged postdischarge opioid use. Our review suggests that multimodal analgesia with regional techniques may be opioid-sparing and instrumental in decreasing perioperative opioid use in patients undergoing TJA. These techniques should be used as part of a comprehensive perioperative plan to decrease overall opioid use while providing adequate analgesia (Fig. 1).
Fig. 1.
An opioid-sparing approach to total joint arthroplasty. Multimodal, nonopioid analgesics form the basis of the protocol. Note that opioids are not introduced until the postoperative phase, and then only after other nonopioid analgesics have been maximized, and sufficient analgesia has not been achieved. All eligible patients should receive regularly scheduled acetaminophen and NSAID; continue gabapentin as tolerated; add dextromethorphan as tolerated, while monitoring for adequate analgesia and side effects. ACB adductor canal block, IPACK interspace between the popliteal artery and posterior capsule of the knee, LIA local infiltration analgesia, PRN as needed, PONV postoperative nausea and vomiting.
Multimodal analgesia forms the cornerstone of post-TJA pain management, and continuation of multimodal IV agents is recommended until the patient is tolerating an oral diet. Effective analgesic choices for post-TJA pain management include NSAIDs and acetaminophen, administered on a scheduled basis, unless there are contraindications.
The use of gabapentinoids may decrease opioid consumption, but our review suggests that the analgesic efficacy for TJA is uncertain, and several publications question the overall analgesic benefits and safety of gabapentinoids [16, 20]. Gabapentinoids are associated with several adverse effects (sedation, dizziness, peripheral edema) and should be used with caution in elderly patients and those with renal dysfunction. Conversely, a recent double-blind placebo-controlled RCT demonstrated that gabapentin promoted earlier cessation of opioid therapy after surgery—including patients undergoing THA and TKA [29].
Other nonopioid analgesic agents may be useful for postoperative pain management for TJA, although there is relatively less data for these agents, including consensus regarding the precise dose and timing of administration. IV ketamine may be a particularly promising agent in opioid-tolerant patients. Less data is available for IV magnesium, PO dextromethorphan, and IV lidocaine in TJA. Nonetheless, data in nonorthopedic patients suggests that these agents may decrease postoperative pain and opioid consumption.
The current evidence base likewise supports the use of regional analgesic techniques to minimize opioid consumption after TJA. Recent years have witnessed a shift from epidural analgesia toward PNBs as the preference for balancing analgesic with adverse effects and minimizing systemic opioid requirements. Our review highlights the multiple options available for local anesthetic-based blocks, each of which achieves dual goals of maximizing analgesia and minimizing opioid use. However, the optimal combinations of PNBs and systemic analgesics are unknown. Recent evidence suggests that a combination of PNBs likely facilitates optimal balance after TKA [96], but data is lacking for THA. Novel PNBs (such as the IPACK block) offer additional targets to minimize postoperative pain, but more research is needed on efficacy. In addition, choices for individual regional modalities must take into account local expertise and resources, recognizing that not all institutions benefit from developed regional anesthesiology services. Here, the role of surgeon-administered LIA/PAI is likely to be particularly valuable.
Finally, the optimal duration of post-TJA analgesia is unclear—as are the methods required to achieve prolonged analgesia. Current and future research should focus on the role of PNCs to extend the duration of opioid-free analgesia, as well as more comparative studies of adjuvants to single-shot PNBs and PNCs.
In summary, effective strategies to minimize opioid consumption in patients undergoing TJA focus on nonopioid multimodal analgesia, including systemic and local-anesthetic-based techniques. Based on the literature presented here, acetaminophen, NSAIDs, and peripheral nerve blocks are especially valuable and are recommended by the authors. NMDA-receptor antagonists may help minimize opioid consumption in patients who have or are at risk of developing chronic pain. Future research is needed to determine the relative benefits of gabapentinoids, PNCs, extended-duration local anesthetics, and novel PNBs for protecting patients at risk for long-term opioid use after TJA.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
Conflict of Interest
Ellen M. Soffin, MD, PhD, and Christopher L. Wu, MD, declare that they have no conflicts of interest.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms:
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III
References
- 1.Abdallah FW, Madjdpour C, Brull R. Is sciatic nerve block advantageous when combined with femoral nerve block for postoperative analgesia following total knee arthroplasty? A meta-analysis. Can J Anaesth. 2016;63(5):552–568. doi: 10.1007/s12630-016-0613-2. [DOI] [PubMed] [Google Scholar]
- 2.Adam F, Chauvin M, Du Manoir B, Langlois M, Sessler DI, Fletcher D. Small-dose ketamine infusion improves postoperative analgesia and rehabilitation after total knee arthroplasty. Anesth Analg. 2005;100(2):475–480. doi: 10.1213/01.ANE.0000142117.82241.DC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albrecht E, Guyen O, Jacot-Guillarmod A, Kirkham KR. The analgesic efficacy of local infiltration analgesia vs femoral nerve block after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2016;116(5):597–609. doi: 10.1093/bja/aew099. [DOI] [PubMed] [Google Scholar]
- 4.Andersen LØ, Kehlet H. Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth. 2014;113(3):360–374. doi: 10.1093/bja/aeu155. [DOI] [PubMed] [Google Scholar]
- 5.Aveline C, Gautier JF, Vautier P, et al. Postoperative analgesia and early rehabilitation after total knee replacement: a comparison of continuous low-dose intravenous ketamine versus nefopam. Eur J Pain. 2009;13(6):613–619. doi: 10.1016/j.ejpain.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Banerjee P, McLean C. The efficacy of multimodal high-volume wound infiltration in primary total hip replacement. Orthopedics. 2011;34(9):e522–e529. doi: 10.3928/01477447-20110714-11. [DOI] [PubMed] [Google Scholar]
- 7.Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA, Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290(18):2455–2463. doi: 10.1001/jama.290.18.2455. [DOI] [PubMed] [Google Scholar]
- 8.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Busch CA, Whitehouse MR, Shore BJ, MacDonald SJ, McCalden RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res. 2010;468(8):2152–2159. doi: 10.1007/s11999-009-1198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan EY, Fransen M, Parker DA, Assam PN, Chua N. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev. 2014;5:CD009941. doi: 10.1002/14651858.CD009941.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi PT, Bhandari M, Scott J, Douketis J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev. 2003;3:CD003071. doi: 10.1002/14651858.CD003071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clarke H, Pagé GM, McCartney CJ, et al. Pregabalin reduces postoperative opioid consumption and pain for 1 week after hospital discharge but does not affect function at 6 weeks or 3 months after total hip arthroplasty. Br J Anaesth. 2015;115(6):903–911. doi: 10.1093/bja/aev363. [DOI] [PubMed] [Google Scholar]
- 13.Clarke H, Pereira S, Kennedy D, et al. Adding gabapentin to a multimodal regimen does not reduce acute pain, opioid consumption or chronic pain after total hip arthroplasty. Acta Anaesthesiol Scand. 2009;53(8):1073–1083. doi: 10.1111/j.1399-6576.2009.02039.x. [DOI] [PubMed] [Google Scholar]
- 14.De Oliveira GS, Jr, Castro-Alves LJ, Khan JH, McCarthy RJ. Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2013;119(1):178–190. doi: 10.1097/ALN.0b013e318297630d. [DOI] [PubMed] [Google Scholar]
- 15.Dobie I, Bennett D, Spence DJ, Murray JM, Beverland DE. Periarticular local anesthesia does not improve pain or mobility after THA. Clin Orthop Relat Res. 2012;470(7):1958–1965. doi: 10.1007/s11999-012-2241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doleman B, Heinink TP, Read DJ, Faleiro RJ, Lund JN, Williams JP. A systematic review and meta-regression analysis of prophylactic gabapentin for postoperative pain. Anaesthesia. 2015;70(10):1186–1204. doi: 10.1111/anae.13179. [DOI] [PubMed] [Google Scholar]
- 17.Dong CC, Dong SL, He FC. Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: a systematic review and meta-analysis. Medicine (Baltimore). 2016;95(12):e2983. doi: 10.1097/MD.0000000000002983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong J, Li W, Wang Y. The effect of pregabalin on acute postoperative pain in patients undergoing total knee arthroplasty: a meta-analysis. Int J Surg. 2016;34:148–160. doi: 10.1016/j.ijsu.2016.08.521. [DOI] [PubMed] [Google Scholar]
- 19.Elliott CE, Thobhani S. The adductor canal catheter and interspace between the popliteal artery and the posterior capsule of the knee for total knee arthroplasty. Tech Reg Anesth Pain Manag. 2014;126–129.
- 20.Fabritius ML, Mathiesen O, Wetterslev J, Dahl JB. Post-operative analgesia: focus has been on benefit—are we forgetting the harm? Acta Anaesthesiol Scand. 2016;60(7):839–841. doi: 10.1111/aas.12729. [DOI] [PubMed] [Google Scholar]
- 21.Fan L, Zhu C, Zan P, et al. The comparison of local infiltration analgesia with peripheral nerve block following total knee arthroplasty (TKA): a systematic review with meta-analysis. J Arthroplasty. 2015;30(9):1664–1671. doi: 10.1016/j.arth.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 22.Fowler SJ, Symons J, Sabato S, Myles PS. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2008;100(2):154–164. doi: 10.1093/bja/aem373. [DOI] [PubMed] [Google Scholar]
- 23.Gabriel RA, Kaye AD, Nagrebetsky A, Jones MR, Dutton RP, Urman RD. Utilization of femoral nerve blocks for total knee arthroplasty. J Arthroplasty. 2016;31(8):1680–1685. doi: 10.1016/j.arth.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Gao F, Ma J, Sun W, Guo W, Li Z, Wang W. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a systematic review and meta-analysis. Clin J Pain. 2016. [DOI] [PubMed]
- 25.Gerrard AD, Brooks B, Asaad P, Hajibandeh S, Hajibandeh S. Meta-analysis of epidural analgesia versus peripheral nerve blockade after total knee joint replacement. Eur J Orthop Surg Traumatol. 2017;27(1):61–72. doi: 10.1007/s00590-016-1846-z. [DOI] [PubMed] [Google Scholar]
- 26.Gobble RM, Hoang HL, Kachniarz B, Orgill DP. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133(3):741–755. doi: 10.1097/01.prs.0000438459.60474.b5. [DOI] [PubMed] [Google Scholar]
- 27.Grape S, Kirkham KR, Baeriswyl M, Albrecht E. The analgesic efficacy of sciatic nerve block in addition to femoral nerve block in patients undergoing total knee arthroplasty: a systematic review and meta-analysis. Anaesthesia. 2016;71(10):1198–1209. doi: 10.1111/anae.13568. [DOI] [PubMed] [Google Scholar]
- 28.Hadzic A, Minkowitz HS, Melson TI, Berkowitz R, Uskova A, Ringold F, et al. Liposome bupivacaine femoral nerve block for postsurgical analgesia after total knee arthroplasty. Anesthesiology. 2016;124:1372–1383. doi: 10.1097/ALN.0000000000001117. [DOI] [PubMed] [Google Scholar]
- 29.Hah J, Mackey SC, Schmidt P, McCue R, Humphreys K, Trafton J, et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort: a randomized clinical trial. JAMA Surg. 2018;153(4):303–311. doi: 10.1001/jamasurg.2017.4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamilton TW, Athanassoglou V, Mellon S, Strickland LH, Trivella M, Murray D, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;2:CD011419. doi: 10.1002/14651858.CD011419.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamilton TW, Strickland LH, Pandit HG. A meta-analysis on the use of gabapentinoids for the treatment of acute postoperative pain following total knee arthroplasty. J Bone Joint Surg Am. 2016;98(16):1340–1350. doi: 10.2106/JBJS.15.01202. [DOI] [PubMed] [Google Scholar]
- 32.Han C, Li XD, Jiang HQ, Ma JX, Ma XL. The use of gabapentin in the management of postoperative pain after total hip arthroplasty: a meta-analysis of randomised controlled trials. J Orthop Surg Res. 2016;11(1):79. doi: 10.1186/s13018-016-0412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hofstad JK, Winther SB, Rian T, Foss OA, Husby OS, Wik TS. Perioperative local infiltration anesthesia with ropivacaine has no effect on postoperative pain after total hip arthroplasty. Acta Orthop. 2015;86(6):654–658. doi: 10.3109/17453674.2015.1053775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Højer Karlsen AP, Geisler A, Petersen PL, Mathiesen O, Dahl JB. Postoperative pain treatment after total hip arthroplasty: a systematic review. Pain. 2015;156(1):8–30. doi: 10.1016/j.pain.0000000000000003. [DOI] [PubMed] [Google Scholar]
- 35.Horlocker TT. Complications of regional anesthesia and acute pain management. Anesthesiol Clin. 2011;29(2):257–278. doi: 10.1016/j.anclin.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 36.Hussain N, Ferreri TG, Prusick PJ, et al. Adductor canal block versus femoral canal block for total knee arthroplasty: a meta-analysis: what does the evidence suggest? Reg Anesth Pain Med. 2016;41(3):314–320. doi: 10.1097/AAP.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 37.Ilfeld BM, Ball ST, Gearen PF, et al. Ambulatory continuous posterior lumbar plexus nerve blocks after hip arthroplasty: a dual-center, randomized, triple-masked, placebo-controlled trial. Anesthesiology. 2008;109(3):491–501. doi: 10.1097/ALN.0b013e318182a4a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113(4):904–902. doi: 10.1213/ANE.0b013e3182285e01. [DOI] [PubMed] [Google Scholar]
- 39.Ilfeld BM. Continuous peripheral nerve blocks: an update of the published evidence and comparison with novel alternative analgesic modalities. Anesth Analg. 2017;124(1):308–335. doi: 10.1213/ANE.0000000000001581. [DOI] [PubMed] [Google Scholar]
- 40.Jiang X, Wang QQ, Wu CA, Tian W. Analgesic efficacy of adductor canal block in total knee arthroplasty: a meta-analysis and systematic review. Orthop Surg. 2016;8(3):294–300. doi: 10.1111/os.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiménez-Almonte JH, Wyles CC, Wyles SP, et al. Is local infiltration analgesia superior to peripheral nerve blockade for pain management after THA: a network meta-analysis. Clin Orthop Relat Res. 2016;474(2):495–516. doi: 10.1007/s11999-015-4619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnson RL, Kopp SL, Hebl JR, Erwin PJ, Mantilla CB. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth. 2013;110(4):518–528. doi: 10.1093/bja/aet013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kazerooni R, Tran MH. Evaluation of celecoxib addition to pain protocol after total hip and knee arthroplasty stratified by opioid tolerance. Clin J Pain. 2015;31(10):903–908. doi: 10.1097/AJP.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 44.Kelly JS, Opsha Y, Costello J, Schiller D, Hola ET. Opioid use in knee arthroplasty after receiving intravenous acetaminophen. Pharmacotherapy. 2014;34(Suppl 1):22S–26S. doi: 10.1002/phar.1518. [DOI] [PubMed] [Google Scholar]
- 45.Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79(2):174–183. doi: 10.1080/17453670710014950. [DOI] [PubMed] [Google Scholar]
- 46.Khan JS, Yousuf M, Victor JC, Sharma A, Siddiqui N. An estimation for an appropriate end time for an intraoperative intravenous lidocaine infusion in bowel surgery: a comparative meta-analysis. J Clin Anesth. 2016;28:95–104. doi: 10.1016/j.jclinane.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 47.King MR, Ladha KS, Gelineau AM, Anderson TA. Perioperative dextromethorphan as an adjunct for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2016;124(3):696–705. doi: 10.1097/ALN.0000000000000950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kranke P, Jokinen J, Pace NL, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015;7:CD009642. doi: 10.1002/14651858.CD009642.pub2. [DOI] [PubMed] [Google Scholar]
- 49.Kuang MJ, Du Y, Ma JX, He W, Fu L, Ma XL. The efficacy of liposomal bupivacaine using periarticular injection in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2017;32(4):1395–1402. doi: 10.1016/j.arth.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 50.Kuang MJ, Xu LY, Ma JX, et al. Adductor canal block versus continuous femoral nerve block in primary total knee arthroplasty: a meta-analysis. Int J Surg. 2016;31:17–24. doi: 10.1016/j.ijsu.2016.05.036. [DOI] [PubMed] [Google Scholar]
- 51.Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg. 2017;125(5):1749–1760. doi: 10.1213/ANE.0000000000002497. [DOI] [PubMed] [Google Scholar]
- 52.Lee JK, Chung KS, Choi CH. The effect of a single dose of preemptive pregabalin administered with COX-2 inhibitor: a trial in total knee arthroplasty. J Arthroplasty. 2015;30(1):38–42. doi: 10.1016/j.arth.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 53.Lee S, Rooban N, Vaghadia H, Sawka AN, Tang R. A randomized non-inferiority trial of adductor canal block for analgesia after total nee arthroplasty: single injection versus catheter technique. J Arthroplasty. 2018;33(4):1045–1051. doi: 10.1016/j.arth.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 54.Li D, Ma GG. Analgesic efficacy and quadriceps strength of adductor canal block versus femoral nerve block following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2614–2619. doi: 10.1007/s00167-015-3874-3. [DOI] [PubMed] [Google Scholar]
- 55.Li D, Yang Z, Xie X, Zhao J, Kang P. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. Int Orthop. 2016;40(5):925–933. doi: 10.1007/s00264-015-2998-x. [DOI] [PubMed] [Google Scholar]
- 56.Li J, Deng X, Jiang T. Combined femoral and sciatic nerve block versus femoral and local infiltration anesthesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2016;11(1):158. doi: 10.1186/s13018-016-0495-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liang L, Cai Y, Li A, Ma C. The efficiency of intravenous acetaminophen for pain control following total knee and hip arthroplasty: a systematic review and meta-analysis. Medicine (Balt). 2017;96(46):e8586. doi: 10.1097/MD.0000000000008586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lin J, Zhang L, Yang H. Perioperative administration of selective cyclooxygenase-2 inhibitors for postoperative pain management in patients after total knee arthroplasty. J Arthroplasty. 2013;28(2):207–213.e2. doi: 10.1016/j.arth.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 59.Lunn TH, Husted H, Solgaard S, et al. Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2011;36(5):424–429. doi: 10.1097/AAP.0b013e3182186866. [DOI] [PubMed] [Google Scholar]
- 60.Ma J, Zhang W, Yao S. Liposomal bupivacaine infiltration versus femoral nerve block for pain control in total knee arthroplasty: a systematic review and meta-analysis. Int J Surg. 2016;36(Pt A):44–55. doi: 10.1016/j.ijsu.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 61.Ma LP, Qi YM, Zhao DX. Comparison of local infiltration analgesia and sciatic nerve block for pain control after total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2017;12(1):85. doi: 10.1186/s13018-017-0586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ma TT, Wang YH, Jiang YF, Peng CB, Yan C, Liu ZG, et al. Liposomal bupivacaine versus traditional bupivacaine for pain control after total hip arthroplasty: a meta-analysis. Medicine (Balt). 2017;96(25):e7190. doi: 10.1097/MD.0000000000007190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Macfarlane AJ, Prasad GA, Chan VW, Brull R. Does regional anaesthesia improve outcomes after total hip arthroplasty? A systematic review. Br J Anaesth. 2009;103(3):335–345. doi: 10.1093/bja/aep208. [DOI] [PubMed] [Google Scholar]
- 64.Mao Y, Wu L, Ding W. The efficacy of preoperative administration of gabapentin/pregabalin in improving pain after total hip arthroplasty: a meta-analysis. BMC Musculoskelet Disord. 2016;17(1):373. doi: 10.1186/s12891-016-1231-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Maradit-Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marino J, Russo J, Kenny M, Herenstein R, Livote E, Chelly JE. Continuous lumbar plexus block for postoperative pain control after total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009;91(1):29–37. doi: 10.2106/JBJS.H.00079. [DOI] [PubMed] [Google Scholar]
- 67.Martin F, Cherif K, Gentili ME, et al. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology. 2008;109(1):118–123. doi: 10.1097/ALN.0b013e31817b5a9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McCarthy D, Iohom G. Local infiltration analgesia for postoperative pain control following total hip arthroplasty: a systematic review. Anesthesiol Res Pract. 2012;2012:709531. doi: 10.1155/2012/709531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McIsaac DI, McCartney CJ, Walraven CV. Peripheral nerve blockade for primary total knee arthroplasty: a population-based cohort study of outcomes and resource utilization. Anesthesiology. 2017;126(2):312–320. doi: 10.1097/ALN.0000000000001455. [DOI] [PubMed] [Google Scholar]
- 70.Mei S, Jin S, Chen Z, Ding X, Zhao X, Li Q. Analgesia for total knee arthroplasty: a meta-analysis comparing local infiltration and femoral nerve block. Clinics (Sao Paulo). 2015;70(9):648–653. doi: 10.6061/clinics/2015(09)09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Memtsoudis SG, Danninger T, Rasul R, et al. Inpatient falls after total knee arthroplasty: the role of anesthesia type and peripheral nerve blocks. Anesthesiology. 2014;120(3):551–563. doi: 10.1097/ALN.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 72.Memtsoudis SG, Poeran J, Cozowicz C, Zubizarreta N, Ozbek U, Mazumdar M. The impact of peripheral nerve blocks on perioperative outcome in hip and knee arthroplasty—a population-based study. Pain. 2016;157(10):2341–2349. doi: 10.1097/j.pain.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 73.Memtsoudis SG, Poeran J, Zubizarreta N, Cozowica C, Morwald EE, et al. Association of multimodal pain management strategies with perioperative outcomes and resource utilization: a population-based study. Anesthesiology. 2018;128:891–902. doi: 10.1097/ALN.0000000000002132. [DOI] [PubMed] [Google Scholar]
- 74.Ménigaux C, Adam F, Guignard B, Sessler DI, Chauvin M. Preoperative gabapentin decreases anxiety and improves early functional recovery from knee surgery. Anesth Analg. 2005;100(5):1394–1399. doi: 10.1213/01.ANE.0000152010.74739.B8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nwagbologu N, Sarangarm P, D’Angio R. Effect of intravenous acetaminophen on postoperative opioid consumption in adult orthopedic surgery patients. Hosp Pharm. 2016;51(9):730–737. doi: 10.1310/hpj5109-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Neal JB, Freiberg AA, Yelle MD, Jiang Y, Zhang C, Kong X, et al. Intravenous vs oral acetaminophen as an adjunct to multimodal analgesia after total knee arthroplasty: a prospective, randomized, double-blind clinical trial. J Arthroplasty. 2017;32(10):3129–3033. doi: 10.1016/j.arth.2017.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113(5):1144–1162. doi: 10.1097/ALN.0b013e3181f4b18. [DOI] [PubMed] [Google Scholar]
- 78.Paul JE, Nantha-Aree M, Buckley N, et al. Randomized controlled trial of gabapentin as an adjunct to perioperative analgesia in total hip arthroplasty patients. Can J Anaesth. 2015;62(5):476–484. doi: 10.1007/s12630-014-0310-y. [DOI] [PubMed] [Google Scholar]
- 79.Perrin SB, Purcell AN. Intraoperative ketamine may influence persistent pain following knee arthroplasty under combined general and spinal anaesthesia: a pilot study. Anaesth Intensive Care. 2009;37(2):248–253. doi: 10.1177/0310057X0903700202. [DOI] [PubMed] [Google Scholar]
- 80.Rawal N, Viscusi E, Peloso PM, et al. Evaluation of etoricoxib in patients undergoing total knee replacement surgery in a double-blind, randomized controlled trial. BMC Musculoskelet Disord. 2013;14:300. doi: 10.1186/1471-2474-14-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Remérand F, Le Tendre C, Baud A, et al. The early and delayed analgesic effects of ketamine after total hip arthroplasty: a prospective, randomized, controlled, double-blind study. Anesth Analg. 2009;109(6):1963–1971. doi: 10.1213/ANE.0b013e3181bdc8a0. [DOI] [PubMed] [Google Scholar]
- 82.Sankineani SR, Reddy ARC, Eachempati KK, Jangale A, Gurava Reddy AV. Comparison of adductor canal block and IPACK block (interspace between the popliteal artery and the capsule of the posterior knee) with adductor canal block alone after total knee arthroplasty: a prospective control trial on pain and knee function in immediate postoperative period. Eu J Orthop Surg Traumatol. 2018;28(7):1391–1395. doi: 10.1007/s00590-018-2218-7. [DOI] [PubMed] [Google Scholar]
- 83.Schroer WC, Diesfeld PJ, LeMarr AR, Reedy ME. Benefits of prolonged postoperative cyclooxygenase-2 inhibitor administration on total knee arthroplasty recovery: a double-blind, placebo-controlled study. J Arthroplasty. 2011;26(6 Suppl):2–7. doi: 10.1016/j.arth.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 84.Siddiqui ZI, Cepeda MS, Denman W, Schumann R, Carr DB. Continuous lumbar plexus block provides improved analgesia with fewer side effects compared with systemic opioids after hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. 2007;32(5):393–398. doi: 10.1016/j.rapm.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 85.Singh PM, Borle A, Trikha A, Michos L, Sinha A, Goudra B. Role of periarticular liposomal bupivacaine infiltration in patients undergoing total knee arthroplasty—a meta-analysis of comparative trials. J Arthroplasty. 2017;32(2):675–688. doi: 10.1016/j.arth.2016.09.042. [DOI] [PubMed] [Google Scholar]
- 86.Singla NK, Hale ME, Davis JC, et al. IV acetaminophen: efficacy of a single dose for postoperative pain after hip arthroplasty: subset data analysis of 2 unpublished randomized clinical trials. Am J Ther. 2015;22(1):2–10. doi: 10.1097/MJT.0000000000000026. [DOI] [PubMed] [Google Scholar]
- 87.Soffin EM, Memtsoudis SG. Anesthesia and analgesia for total knee arthroplasty: a narrative review. Minerva Anesthesiol. 2018. 10.23736/S0375-9393.18.12383-2. [DOI] [PubMed]
- 88.Soffin EM, Waldman SA, Stack RJ, Liguori GA. An evidence-based approach to the prescription opioid epidemic in orthopedic surgery. Anesth Analg. 2017;125(5):1704–1713. doi: 10.1213/ANE.0000000000002433. [DOI] [PubMed] [Google Scholar]
- 89.Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117(Suppl 3):iii62–iii72. doi: 10.1093/bja/aew362. [DOI] [PubMed] [Google Scholar]
- 90.Soffin EM, YaDeau JT. Peripheral nerve catheters: ready for a central role? Anesth Analg. 2017;124(1):4–6. doi: 10.1213/ANE.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 91.Solovyova O, Lewis CG, Abrams JH, et al. Local infiltration analgesia followed by continuous infusion of local anesthetic solution for total hip arthroplasty: a prospective, randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am. 2013;95(21):1935–1941. doi: 10.2106/JBJS.L.00477. [DOI] [PubMed] [Google Scholar]
- 92.Specht K, Leonhardt JS, Revald P, et al. No evidence of a clinically important effect of adding local infusion analgesia administrated through a catheter in pain treatment after total hip arthroplasty. Acta Orthop. 2011;82(3):315–320. doi: 10.3109/17453674.2011.570671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stevens RD, Van Gessel E, Flory N, Fournier R, Gamulin Z. Lumbar plexus block reduces pain and blood loss associated with total hip arthroplasty. Anesthesiology. 2000;93(1):115–121. doi: 10.1097/00000542-200007000-00021. [DOI] [PubMed] [Google Scholar]
- 94.Strom BL, Berlin JA, Kinman JL, et al. Parenteral ketorolac and risk of gastrointestinal and operative site bleeding. A postmarketing surveillance study. JAMA. 1996;275(5):376–382. [PubMed] [Google Scholar]
- 95.Sun L, Zhu X, Zou J, Li Y, Han W. Comparison of intravenous and oral acetaminophen for pain control after total knee and hip arthroplasty: a systematic review and meta-analysis. Medicine (Balt). 2018;97(6):e9751. doi: 10.1097/MD.0000000000009751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Terkawi AS, Mavridis D, Sessler DI, et al. Pain management modalities after total knee arthroplasty: a network meta-analysis of 170 randomized controlled trials. Anesthesiology. 2017;126:923–937. doi: 10.1097/ALN.0000000000001607. [DOI] [PubMed] [Google Scholar]
- 97.Thobhani S, Scalercio L, Elliott CE, Nossaman BD, Thomas LC, Yuratich D, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J. 2017;17:233–238. [PMC free article] [PubMed] [Google Scholar]
- 98.Wang C, Cai XZ, Yan SG. Comparison of periarticular multimodal drug injection and femoral nerve block for postoperative pain management in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2015;30(7):1281–1286. doi: 10.1016/j.arth.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 99.Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep. 2017;7:40721. doi: 10.1038/srep40721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Weibel S, Jokinen J, Pace NL, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016;116(6):770–783. doi: 10.1093/bja/aew101. [DOI] [PubMed] [Google Scholar]
- 101.Wu CL, Cohen SR, Richman JM, et al. Efficacy of postoperative patient-controlled and continuous infusion epidural analgesia versus intravenous patient-controlled analgesia with opioids: a meta-analysis. Anesthesiology. 2005;103(5):1079–1088. doi: 10.1097/00000542-200511000-00023. [DOI] [PubMed] [Google Scholar]
- 102.Wu ZQ, Min JK, Wang D, Yuan YJ, Li H. Liposome bupivacaine for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2016;11(1):84. doi: 10.1186/s13018-016-0420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xin Wang MM, Yuan Sun MM, Li Wang MM, Xuelian Hao MB. Femoral nerve block versus fascia iliaca block for pain control in total knee and hip arthroplasty. Medicine (Balt). 2017;96(27):e7382. doi: 10.1097/MD.0000000000007382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xu J, Chen XM, Ma CK, Wang XR. Peripheral nerve blocks for postoperative pain after major knee surgery. Cochrane Database Syst Rev. 2014;12:CD010937. doi: 10.1002/14651858.CD010937.pub2. [DOI] [PubMed] [Google Scholar]
- 105.YaDeau JT, Lin Y, Mayman DJ, et al. Pregabalin and pain after total knee arthroplasty: a double-blind, randomized, placebo-controlled, multidose trial. Br J Anaesth. 2015;115(2):285–293. doi: 10.1093/bja/aev217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.YaDeau JT, Tedore T, Goytizolo EA, et al. Lumbar plexus blockade reduces pain after hip arthroscopy: a prospective randomized controlled trial. Anesth Analg. 2012;115(4):968–972. doi: 10.1213/ANE.0b013e318265bacd. [DOI] [PubMed] [Google Scholar]
- 107.Yang L, Du S, Sun Y. Intravenous acetaminophen as an adjunct to multimodal analgesia after total knee and hip arthroplasty: a systematic review and meta-analysis. Int J Surg. 2017;47:135–146. doi: 10.1016/j.ijsu.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 108.Yin JB, Cui GB, Mi MS, et al. Local infiltration analgesia for postoperative pain after hip arthroplasty: a systematic review and meta-analysis. J Pain. 2014;15(8):781–799. doi: 10.1016/j.jpain.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 109.Yun XD, Yin XL, Jiang J, et al. Local infiltration analgesia versus femoral nerve block in total knee arthroplasty: a meta-analysis. Orthop Traumatol Surg Res. 2015;101(5):565–569. doi: 10.1016/j.otsr.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 110.Zhang S, Paul J, Nantha-Aree M, et al. Reanalysis of morphine consumption from two randomized controlled trials of gabapentin using longitudinal statistical methods. J Pain Res. 2015;8:79–85. doi: 10.2147/JPR.S56558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhang X, Yang Q, Zhang Z. The efficiency and safety of local liposomal bupivacaine infiltration for pain control in total hip arthroplasty: a systematic review and meta-analysis. Medicine (Balt). 2017;96(49):e8433. doi: 10.1097/MD.0000000000008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhao XQ, Jiang N, Yuan FF, Wang L, Yu B. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesth. 2016;30(5):745–754. doi: 10.1007/s00540-016-2194-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)