Abstract
Background
Current research on opioid use within orthopedic surgery has focused on efforts to identify patients at risk for chronic opioid use. Studies addressing prevention of opioid misuse related to orthopedic care are lacking. Evidence-based interventions to reduce the reliance on opioids for post-operative pain relief will be a key component of any comprehensive institutional opioid policy.
Questions/Purposes
The purpose of this systematic review was to evaluate institutional strategies that reduce opioid administration or consumption after orthopedic surgery.
Methods
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist, a search was conducted of the PubMed database for English-language articles that analyzed interventions by physicians, nurses, pharmacists, physical therapists, or other hospital staff to reduce post-operative opioid use or narcotic prescription amounts after surgery. Studies that contained objective outcome measures (i.e., no expert opinion articles) were selected. Investigations on the effect of pharmacologic adjuvants, cryotherapy, or regional nerve blockades on opioid use were excluded.
Results
The initial search yielded 6598 titles, of which 13 full-text articles were ultimately selected for inclusion in this systematic review. The review identified two major categories of interventions—patient-focused and provider-focused (e.g., physicians, nurses, physical therapists, pharmacists). Formal patient education programs were most effective in reducing opioid use. On the provider side, prescribing guidelines appear to decrease the overall number of pills prescribed, often without changes in patient satisfaction or requests for refills.
Conclusions
Researchers are just beginning to establish the most effective ways for institutions to reduce opioid use and promote responsible post-operative prescribing. Institutional prescribing guidelines, standardized bedside pain-management programs, and formal patient education curriculums are all evidence-based interventions that can achieve these goals. The available research also supports an interprofessional approach in any institutional opioid-reduction strategy.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-09662-y) contains supplementary material, which is available to authorized users.
Keywords: opioid policy, opioid education, opioid guidelines, pain management, orthopedic surgery
Introduction
Orthopedic surgeons practice in institutions that offer an extraordinary opportunity for combating the current opioid crisis. A campaign begun in the 1990s advocating that pain be assessed as “the fifth vital sign” linked patients’ satisfaction with pain control to hospital reimbursements, thus creating a patient-care environment in which opioids were often overprescribed. In turn, orthopedic surgeons have been identified as overprescribing opioids, leaving patients with residual pills available for diversion [7, 13, 14, 23]; however, since a patient’s pain-relief experience in an institution is dependent on a wide variety of providers, an interprofessional approach will be required for change to be implemented on an institutional level. For example, nurses and patient care technicians are most often at the patient’s bedside during a post-anesthesia care unit (PACU) or inpatient stay and in turn affect how medications are administered—and therefore how pain is interpreted. At discharge, nurses give medication instructions. Opioid prescriptions themselves are often written by physician assistants, nurse practitioners, and residents. Changes designed to improve opioid prescribing can only occur if the institution ensures that all providers are working from the same mental model of opioid administration and prescribing.
Spurred by the opioid epidemic, researchers on opioids and orthopedic surgery identified patient-level factors that could lead to prolonged post-operative opioid use [25, 29]. A recent high-quality meta-analysis found that prior opioid use, history of back pain, longer hospital stay, and depression had the largest effects on prolonging opioid use after surgery or trauma [16]; however, screening for at-risk patients is only a small part of a comprehensive strategy to reduce opioid consumption and administration at the hospital level [26]. To prevent a future crisis and slow the current one, hospitals must combat past prescribing practices and decrease their reliance on opioids for pain relief after surgery. The purpose of this literature review was to answer the following question: What are the institutional strategies that reduce opioid administration or consumption after orthopedic surgery? We hoped that such evidence would provide a blueprint for hospitals aiming to adopt the best policies on opioid administration; inspire collaboration among surgical teams and between hospitals and surgeons; and identify areas needed for future research.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to conduct a systematic review [17]. The goal of our search strategy was to find exemplary investigations on which to model institutional policies to reduce opioid use. We conducted a search of the PubMed database for English-language articles published prior to October 2018 using the following search terms: “opioids AND guidelines AND surgery,” “opioids AND education,” and “opioids AND orthopedic surgery.” The search terms identified 497, 4315, and 1786 titles, respectively. These titles were scanned for those that appeared to present interventions by physicians, nurses, pharmacists, physical therapists, or other hospital staff to reduce post-operative opioid use or opioid prescription amounts after surgery. The majority of titles suggested investigations on the effect of pharmacologic adjuvants, cryotherapy, or regional nerve blockades on opioid use, these were excluded (multimodal analgesia is currently the standard of care after orthopedic surgery; what methods are most effective is a separate question). Abstracts from 103 selected titles were screened to select studies that contained objective outcomes of interest. Expert opinion articles or descriptions of interventions without objective evaluation of outcomes were excluded. Subsequently, 20 full text articles were selected. Upon review of the full texts, seven articles did not present objective outcomes of interest and were excluded. Thus, 13 were found to meet final inclusion criteria for this review. References from these 13 articles were screened, but there were no studies identified in the citations that had not been already identified by the literature search.
Results
Patient-Focused Interventions
Reviewed articles are presented in Table 1. In summary, while many patient-focused interventions were multifactorial, most could be further classified as strategies focused on educating patients on minimizing opioid use [2, 30], setting appropriate pain expectations [4, 10], or identifying high-risk individuals [16]. Regarding patient education, a single-blinded randomized controlled trial of 140 patients undergoing arthroscopic rotator cuff repair compared a formal educational program to standard of care (informal education by nurses or pharmacists at discharge) [30]. The formal program consisted of a 2-min educational video and handout detailing the risks of opioid overuse. The investigators found that at 6 weeks after surgery, the control group had consumed an average of 60.6 pills, compared with 40.4 in the study group, and that the study group reported lower pain scores. As to setting patient expectations, a 1964 New England Journal of Medicine article concluded that patients counseled by the anesthesiologist on post-operative pain expectations consumed half the amount of pain medication as controls [4]. These findings were largely in line with the quicker time to opioid cessation found in a contemporary group of patients who underwent pre-operative pain-expectation counseling before orthopedic trauma surgery [10].
Table 1.
Summary of studies included in final review
| Author | Journal | Year | Study design | Intervention | Surgery | Sample | Outcomes | Level of evidence |
|---|---|---|---|---|---|---|---|---|
| Cui et al. [1] | J Clin Nurs | 2018 | Prospective cohort study | Pain management protocol for orthopedic nurses | Joint replacement and spinal fusion | 31 nurses, 148 patients | After the intervention 66.2% of patients received opioid & non-opioid analgesics (38.8% pre-intervention). Nursing pain management knowledge increased | II |
| Dwyer et al. | J Hand Surg | 2018 | Prospective cohort study | Prescribing guidelines, patient handouts | Carpal tunnel release (CTR), volar locked plating of radius (VLP) | 145 | Average prescription size decreased from 22 to 10 pills (CTR) and 39 to 25 pills (VLP) (p < 0.05 for both). Satisfaction rates were high in both cohorts (CTR, 96%; VLP, 88%) | II |
| Earp et al. [3] | J Bone Jt Surg Am | 2018 | Retrospective cohort study | Prescribing guidelines | Hand surgery | 518 | Mean prescription amounts were significantly reduced from 97.8–176.0%. After implementation, only 16.4% of patients were prescribed an amount above the protocol | III |
| Egbert et al. [4] | NEJM | 1964 | Prospective cohort study | Counseling by anesthesiologists | Any | 97 | Mostly of historical interest. Opioid consumption reduced by half | III |
| Hill et al. [9] | Ann Surg | 2018 | Retrospective cohort study | Prescribing guidelines | Partial mastectomy with or without lymph node biopsy, laparoscopic cholecystectomy, laparoscopic/open inguinal hernia repair | 915 | 224 patients in post-intervention cohort, decreases in total number of opioids prescribed ranging from 43.0–74.3%. Refill rate was unchanged | III |
| Holman et al. [10] | J Orthop Trauma | 2014 | Retrospective cohort study | Physician counseling on pain management expectations | Trauma or fracture fixation | 613 | 73% of patients in the intervention group ceased opioid use by 6 weeks (vs. 64% of the controls, p = 0.012), no difference in rates of cessation at 12 weeks or greater | III |
| Howard et al. [11] | J Am Coll Surg | 2018 | Retrospective cohort study | Prescribing guidelines | Laparoscopic cholecystectomy | 1158 | Significant reduction in opioid prescription sizes for laparoscopic appendectomy, thyroidectomy, and inguinal hernia repair | III |
| Howard et al. [12] | JAMA Surg | 2018 | Retrospective cohort study | Prescribing guidelines | Laparoscopic cholecystectomy | 370 | Median OME prescription reduced from 250 mg to 75 mg (p < 0.001) with a comparable refill rate (2.5% pre vs. 4.1% post, p < 0.40) | III |
| Mohamadi et al. [16] | J Bone Jt Surg Am | 2018 | Meta-analysis of retrospective cohort studies | N/A | N/A | 1,969,953 | Factors with the strongest associations with prolonged opioid use included prior opioid use (OR 11.04, 95% CI 9.39–12.97); history of back pain (OR 2.1, 95% CI 2.00–2.20); longer hospital stay (OR 2.03, 95% CI 1.03–4.02); depression (OR 1.62, 95% CI 1.49–1.77) | III |
| Nooromid et al. [19] | Am J Surg | 2017 | Prospective cohort study | Educational program on opioid prescribing for surgical interns | Any | 30 | Median MME prescribed per procedure was unchanged by program, though 73% of the interns stated they would prescribe fewer opioids | IV |
| Stanek et al. [27] | J Hand Surg | 2015 | Retrospective cohort study | Prescribing guidelines | First dorsal compartment release, ganglion cyst excision, ORIF MCP fracture, trigger finger release | 402 | Mean prescription sizes were significantly reduced from 15 to 48%. These changes persisted at 1 year | III |
| Stepan et al. [28] | J Hand Surg | 2018 | Retrospective cohort study | Prescribing guidelines | Hand surgery | 1348 | Mean prescription amount reduced by 52.3%. Variability in prescription sizes decreased for all procedures | III |
| Syed et al. [30] | J Shoulder Elbow Surg | 2018 | Randomized controlled trial | Pre-operative patient education | Arthroscopic rotator cuff repair | 140 | At 6 weeks post-operatively, interventional group consumed fewer opioid pills (avg. 87.2 ± 98.3 vs. 51.2 ± 57.7, p < 0.01) and also had a lower average VAS pain score (3.7 ± 2.4 vs. 2.4 ± 2.0, p = 0.001) | I |
OME oral morphine equivalents, MME morphine milligram equivalents, ORIF MCP open reduction and internal fixation metacarpal/phalangeal, VAS visual analog scale
Provider-Focused Interventions
The majority of research on provider-focused interventions compared the effect of prescriber education or formal prescribing guidelines on reducing opioid prescriptions after orthopedic surgery [1–3, 6, 9, 11, 12, 19, 27, 28]. After the introduction of provider education and guidelines, investigators found reductions in post-operative prescriptions ranging from 42.9 to 176.0% [3, 6, 9, 28]. Such guidelines may also reduce opioid prescribing for other procedures simply by increasing physician awareness [11]. The role of nurses in the bedside evaluation of patients’ pain was also an area for potential intervention. After the implementation of a nursing pain-management protocol focusing on the major aspects of comprehensive pain assessment (pain intensity, interference of pain with function and emotions, medication side effects, and perception of care), one hospital found significant decreases in patient-reported “worst pain” and interference of pain with sleep [1]. This was accompanied by a decrease in the amount of opioid administered and an increase in the administration of non-opioid analgesics.
Discussion
Many institutions have only just begun to measure the effect of policies to reduce opioid use in the acute post-operative period, limiting the available evidence on this topic; however, this systematic review has identified several interventions that appear to be effective in reducing post-operative opioid consumption. Regarding patient-focused interventions, informal pre-operative counseling on pain expectations may reduce use [4, 10]; however, hospitals and surgical centers may find better results by creating formal pre-operative opioid educational programs. Though we identified only two studies examining formal programs, the studies were of high quality with convincing results [2, 30]. An interprofessional approach in reducing post-operative use was a consistent theme seen among studies [1, 5, 21, 24], noting interventions by physicians, residents, and nursing staff. We also identified expert opinion pieces on how pharmacists or physical therapists may play a role in decreasing opioid use; however, these articles did not report objective outcome measures and were therefore excluded from the final review [5, 15].
The historical emphasis on pain relief as a quality measure has influenced patients’ expectations on the level of pain they should have after surgery and how it should be addressed by the patient care team. Institutions can actively pre-empt misconceptions by ensuring that all members of the care team promote the same message about the role of opioids in pain relief. Nurses, patient care assistants, pharmacists, and physical therapists are key players in these conversations, as they spend more time than physicians do interacting with inpatients. Thus, current research supports the adoption of an institutional “shared mental model” that emphasizes positions on post-operative pain expectations, evaluation of pain, and administration of opioids across the patient care team [11, 20, 24].
Our review found that prescribing guidelines are almost universally effective in reducing opioid prescriptions after surgery [3, 9, 11, 27, 28]. Given a lack of hard data on the “appropriate minimum quantity” of opioids to prescribe after many procedures [14], a consensus method may be employed to formulate institutional guidelines [28]. Of note, all of the guidelines investigated included an educational component for the providers. Given that the success of the guideline is based on the proper interpretation by the prescribers, any guideline should be coupled with provider education in order to ensure a shared mental model. Guidelines that are followed blindly could lead to an increase in prescription quantities for patients who may request less.
At the end of 2016, our hospital developed service-specific opioid prescribing guidelines based on consensus panels formed by surgeons, pain management specialists, and anesthesiologists who worked within each service (adult reconstruction, spine, pediatrics, sports, trauma, foot and ankle, hand, and limb lengthening). The guidelines were rolled out at the beginning of 2017, and coupled with a mandatory prescriber education program consisting of a 1-h lecture on the opioid epidemic, regulatory concerns, and proper prescribing of opioids. In the year after our institutional intervention, almost all services saw marked decreases in the amount of pills that were being prescribed, with an impressive estimated number of pills saved (Table 2). Even the services that elected to use a qualitative guideline, such as the spine service, saw changes in prescriber behavior. For the spine service, in the pre-intervention period, 66% of prescriptions were for more than 80 pills. Following the educational program only 25% of the discharge prescriptions were for more than 80 pills.
Table 2.
Estimated number of opioid pills saved per year for select procedures after an institutional intervention to standardize prescribing practices at the Hospital for Special Surgery. Figures calculated based on the number of pills prescribed in the 8 months before the intervention compared with the number of pills prescribed in the 8 months after the intervention
| Procedure | Estimated no. of opioid pills saved/year |
|---|---|
| Spinal decompression | 19,584 |
| Spinal fusion | 6480 |
| Knee arthroscopy | 10,121 |
| Shoulder arthroscopy | 4292 |
| Minor hand procedures | 3315 |
| Carpal tunnel release | 2815 |
| Distal radius open reduction and internal fixation | 3364 |
While this review has highlighted several action points by which institutions can begin to combat the opioid crisis, there are still many unanswered questions on the ideal prescription and administration of opioids. Orthopedic surgeons are still largely unaware of how many pills a patient consumes after orthopedic surgery. A critical question—What is the minimum necessary quantity of opioid that would fulfill pain relief requirements for the majority of patients after orthopedic surgery?—is still unanswered. Our institution is currently conducting a prospective, SMS-based investigation measuring daily opioid use after various procedures [22]. Preliminary results are promising that we will be able to reduce our opioid prescription rates even further.
Another critical unanswered question is whether opioid prescriptions can be tailored to the specific patient. The “holy grail” of opioid prescribing would be to develop a method for reliably predicting the amount of opioid (if any) a patient may consider adequate for pain relief. Along with the variability in opioid receptor type and metabolism of each patient, other factors that affect post-operative opioid use are likely related to aspects difficult or impractical to quantify, such as a patient’s personality traits, sense of self-efficacy, or psychosocial well-being [8, 31]. The idea of a nociceptive-related “pain threshold” is another factor that may influence opioid consumption. In a series of 160 patients undergoing lower-extremity joint replacement, pain was measured pre-operatively using a pressure algometer [18]. Linear regression showed a negative correlation between operative site pain threshold and outpatient opioid prescriptions. While such a system would be difficult to implement on a practical clinical basis, the study serves as an example of our limited understanding of the prediction of individual opioid consumption.
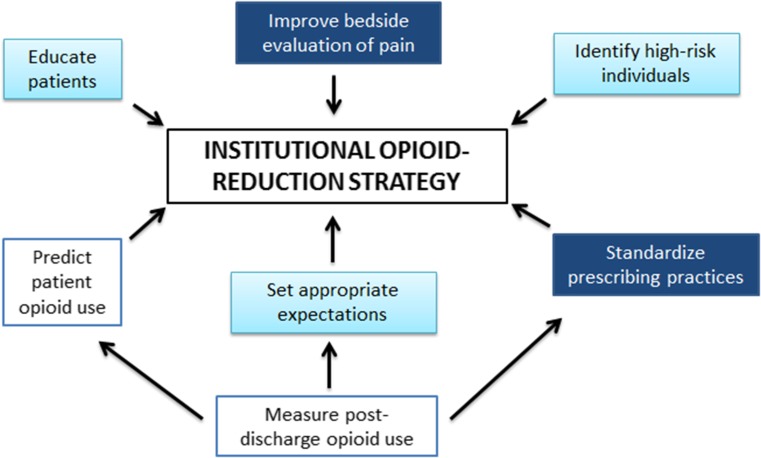
While the current opioid crisis paints a bleak picture, orthopedic institutions can take a leading role in slowing the epidemic (Fig. 1). A key component is the adoption of policies that fight historical precedents. Institutional protocols that help minimize opioid consumption on the patient side and ensure appropriate administration and prescribing on the provider side will go a long way in reversing current practices and ensuring a safe future. All who participate in patient care at the hospital or surgery center must share in the institution’s mental model of how pain should be interpreted and opioid medications administered or prescribed. The current crisis has stimulated creative opioid research and the adoption of new technologies to tackle difficult problems. We look forward to seeing how orthopedic institutions will collaborate going forward in the development of policies that will perfect how we administer opioid medications and avoid future crises.
Fig. 1.
Summary of institutional strategies to combat the opioid epidemic. Patient-focused strategies are in light blue, provider-focused strategies are in dark blue, and future directions are outlined in blue
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(DOCX 12 kb)
Conflict of Interest
Francis Lovecchio, MD, Ajay Premkumar, MD, MPH, and Jeffrey G. Stepan, MD, MSc, declare that they have no conflicts of interest. Todd J. Albert, MD, reports receiving royalties from Zimmer Biomet, DePuy Synthes, JP Medical Publishers, Saunders/Mosby-Elseveir, and Thieme; owning stock in Gentis, Vital 5, Bonovo Orthopedics Inc., Biomerix, InVivo Therapeutics, Spinicity, Crosstrees Medical, Paradigm Spine LLC, Invuity, ASIP, PMIG, Pioneer, and Vertech; receiving personal fees from Nuvasive, Gentis, United Health Care, and Facet Link and non-financial support from Scoliosis Research Society; receiving salary from Hospital for Special Surgery and Weill Cornell Medical College and grants from Patient-Centered Outcomes Research Institute, ISSG, Alan L. and Jacqueline B. Stuart Spine Research Center, all outside the submitted work.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cui C, Wang L-X, Li Q, Zaslansky R, Li L. Implementing a pain management nursing protocol for orthopaedic surgical patients: Results from a PAIN OUT project. J Clin Nurs. 2018;27:1684–1691. doi: 10.1111/jocn.14224. [DOI] [PubMed] [Google Scholar]
- 2.Dwyer CL, Soong M, Hunter A, Dashe J, Tolo E, Kasparyan NG. Prospective evaluation of an opioid reduction protocol in hand surgery. J Hand Surg Am. 2018;43(6):516–522.e1. [DOI] [PubMed]
- 3.Earp BE, Silver JA, Mora AN, Blazar P. Implementing a postoperative opioid-prescribing protocol significantly reduces the total morphine milligram equivalents prescribed. J Bone Jt Surg Am. 2018;100:1698–1703. [DOI] [PubMed]
- 4.Egbert LD, Battit GE, Welch CE, Bartlett MK. Reduction of postoperative pain by encouragement and instruction of patients. N Engl J Med. 1964;270:825–827. doi: 10.1056/NEJM196404162701606. [DOI] [PubMed] [Google Scholar]
- 5.Genord C, Frost T, Eid D. Opioid exit plan: a pharmacist’s role in managing acute postoperative pain. J Am Pharm Assoc (2003). 2017;57:S92–S98. doi: 10.1016/j.japh.2017.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157:1259–1265. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta A, Kumar K, Roberts MM, et al. Pain management after outpatient foot and ankle surgery. Foot Ankle Int. 2018;39(2):149–154. doi: 10.1177/1071100717738495. [DOI] [PubMed] [Google Scholar]
- 8.Helmerhorst GTT, Lindenhovius ALC, Vrahas M, Ring D, Kloen P. Satisfaction with pain relief after operative treatment of an ankle fracture. Injury. 2012;43:1958–1961. doi: 10.1016/j.injury.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 9.Hill MV, Stucke RS, Mcmahon ML, Beeman JL, Barth RJ. An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018;267(3):468–472. doi: 10.1097/SLA.0000000000002198. [DOI] [PubMed] [Google Scholar]
- 10.Holman JE, Stoddard GJ, Horwitz DS, Higgins TF. The effect of preoperative counseling on duration of postoperative opiate use in orthopaedic trauma surgery: a surgeon-based comparative cohort study. J Orthop Trauma. 2014;28:502–506. doi: 10.1097/BOT.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 11.Howard R, Alameddine M, Klueh M, et al. Spillover effect of evidence-based postoperative opioid prescribing. J Am Coll Surg. 2018;227:374–381. doi: 10.1016/j.jamcollsurg.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in opioid prescribing through evidence-based prescribing guidelines. JAMA Surg. 2018;153:285–287. doi: 10.1001/jamasurg.2017.4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar K, Gulotta LV, Dines JS, et al. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017;45:636–641. doi: 10.1177/0363546517693665. [DOI] [PubMed] [Google Scholar]
- 14.Lovecchio F, Derman P, Stepan J, et al. Support for safer opioid prescribing practices. J Bone Jt Surg. 2017;99:1945–1955. doi: 10.2106/JBJS.17.00124. [DOI] [PubMed] [Google Scholar]
- 15.Mintken PE, Moore JR, Flynn TW. Physical therapists’ role in solving the opioid epidemic. J Orthop Sports Phys Ther. 2018;48:349–353. doi: 10.2519/jospt.2018.0606. [DOI] [PubMed] [Google Scholar]
- 16.Mohamadi A, Chan JJ, Lian J, Wright CL, Marin AM, Rodriguez EK, et al. Risk factors and pooled rate of prolonged opioid use following trauma or surgery. J Bone Jt Surg. 2018;100:1332–1340. doi: 10.2106/JBJS.17.01239. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:332–336. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nickel BT, Klement MR, Byrd WA, Attarian DE, Seyler TM, Wellman SS. The James A. Rand Young Investigator’s Award: battling the opioid epidemic with prospective pain threshold measurement. J Arthroplasty. 2018;33(7S):S3–S7. [DOI] [PubMed]
- 19.Nooromid MJ, Mansukhani NA, Deschner BW, et al. Surgical interns: Preparedness for opioid prescribing before and after a training intervention. Am J Surg. 2018;215:238–242. doi: 10.1016/j.amjsurg.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olsen KR, Hall DJ, Mira JC, et al. Postoperative surgical trainee opioid prescribing practices (POST OPP): an institutional study. J Surg Res. 2018;229:58–65. doi: 10.1016/j.jss.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Pasero C, Quinlan-Colwell A, Rae D, Broglio K, Drew D. American Society for Pain Management Nursing position statement: prescribing and administering opioid doses based solely on pain intensity. Pain Manag Nurs. 2016;17:170–180. doi: 10.1016/j.pmn.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Premkumar A, Lovecchio F, Stepan JG, et al. A novel mobile phone text messaging platform improves collection of patient-reported post-operative pain and opioid use following orthopedic surgery. HSS J. 2018. 10.1007/s11420-018-9635-3 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 23.Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am. 2018;100:180–188. doi: 10.2106/JBJS.17.00672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scher C, Meador L, Van Cleave JH, Reid MC. Moving beyond pain as the fifth vital sign and patient satisfaction scores to improve pain care in the 21st century. Pain Manag Nurs. 2018;19:125–129. doi: 10.1016/j.pmn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoenfeld AJ, Jiang W, Chaudhary MA, Scully RE, Koehlmoos T, Haider AH. Sustained prescription opioid use among previously opioid-naive patients insured through TRICARE (2006-2014) JAMA Surg. 2017;152(12):1175–1176. doi: 10.1001/jamasurg.2017.2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soffin EM, Waldman SA, Stack RJ, Liguori GA. An evidence-based approach to the prescription opioid epidemic in orthopedic surgery. Anesth Analg. 2017;125:1704–1713. doi: 10.1213/ANE.0000000000002433. [DOI] [PubMed] [Google Scholar]
- 27.Stanek JJ, Renslow MA, Kalliainen LK. The effect of an educational program on opioid prescription patterns in hand surgery: a quality improvement program. J Hand Surg Am. 2015;40:341–346. doi: 10.1016/j.jhsa.2014.10.054. [DOI] [PubMed] [Google Scholar]
- 28.Stepan JG, Sacks HA, Lovecchio FC, et al. Opioid prescriber education and guidelines for ambulatory upper-extremity surgery: evaluation of an institutional protocol. J Hand Surg Am. 2018. 10.1016/j.jhsa.2018.06.014. [DOI] [PubMed]
- 29.Sun EC, Darnall B, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–1293. doi: 10.1001/jamainternmed.2016.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Syed UAM, Aleem AW, Wowkanech C, et al. Neer Award 2018: the effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial. J Shoulder Elb Surg. 2018;27(6):962–967. doi: 10.1016/j.jse.2018.02.039. [DOI] [PubMed] [Google Scholar]
- 31.van Dijk JFM, Kappen TH, Schuurmans MJ, van Wijck AJM. The relation between patients’ NRS pain scores and their desire for additional opioids after surgery. Pain Pract. 2015;15:604–609. doi: 10.1111/papr.12217. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(DOCX 12 kb)