Introduction
Stent insertion is a palliative treatment for inoperable airway stenosis (1). The choice of appropriate stent is mandatory to preserve airway patency. Herein, we reported the use of fibrin glue (FG) to fill an unexpected gap in diameter between an undersized self-expandable metallic stent (SEMS) and the left mainstem bronchus (LMB) after endoscopic recanalization for neoplastic stenosis.
Case presentation
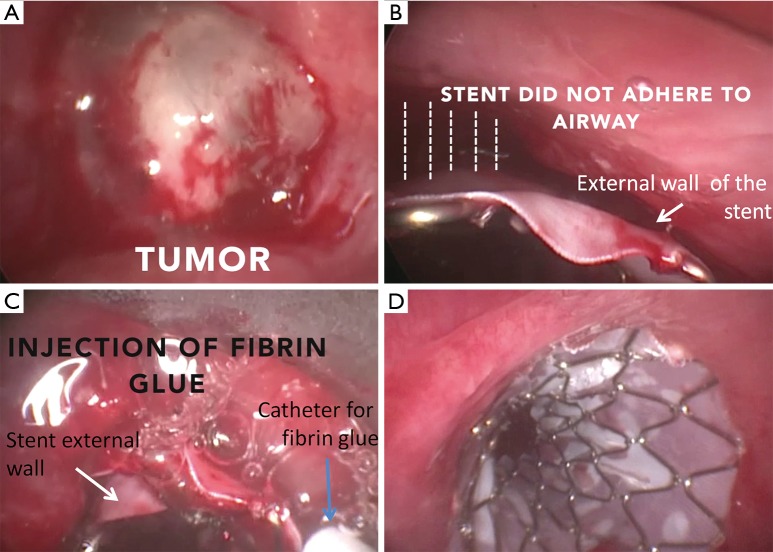
Last September 2016, a 63-year-old man was referred to our attention for management of acute respiratory distress due to adenocarcinoma that originated from left upper bronchus (LUB) and obstructed the LMB with atelectasis of the entire lung. The advanced stage disease (T4N2M1-stage IVB) contraindicated surgery and endoscopic recanalization was planned to improve dyspnoea and clinical condition. Under general anaesthesia, patient was intubated with 8.5 mm rigid bronchoscopy (Stortz; Tuttlingen, Deutschland). The tumor that obstructed the LMB was coagulated with neodymium-doped yttrium aluminium perovskite (Nd-YAP) laser (Lokki Lis Laser-Bryan Corporation; Woburn, Mass, USA) and then resected through mechanical coring technique with recanalization of LMB and left lower bronchus (LLB). A fully covered SEMS (Silmet; Novatech SA, France) 60 mm in length and 12 mm in diameter was placed into the LMB so that the mid-point of the stent covered the LUB, where tumor originated, but preserved the LLB patency. However, the stent did not adhere to the airway wall since its diameter was under-sized for the anatomy of treated airway. No further opening was obtained after stent balloon dilatation. Thus, 1.5 mL of FG (Tisseel®, Baxter AG, Vienna) was injected with a dedicated double lumen catheter (Duplocath® 180, Baxter AG, Vienna, Austria) over the external wall of the stent until it filled the gap between the stent and LMB. Then, a 12–15 mm balloon catheter (Boston Scientific, Natick, MA, USA) dilated the stent 2 or 3 times for 15–30 seconds each, until a sufficient adhesion of the stent to the airway was obtained (Figures 1,2). The dyspnoea disappeared after the procedure and chest-X-ray confirmed the proper position of the stent and the re-expansion of left lower lobe (Figure 3). The replacing the stent with another of appropriate size was planned but patient refused this procedure. He underwent chemotherapy and radiotherapy and no complications as stent migration were seen during the follow-up. He died last April 2018 for multiple metastases, 18 months after treatment.
Figure 1.
(A) Tumor obstructed left main bronchus; (B) the proximal end of the stent did not adhere to the airway wall; (C) fibrin glue filled the gap between the external wall of the stent and airway; (D) a sufficient adhesion of the stent to the airway was obtained.
Figure 2.

The video edited the main steps of the procedure as the resection of the tumor, the deployment of the stent, and its fixation with fibrin glue (2). Available online: http://www.asvide.com/article/view/29638
Figure 3.
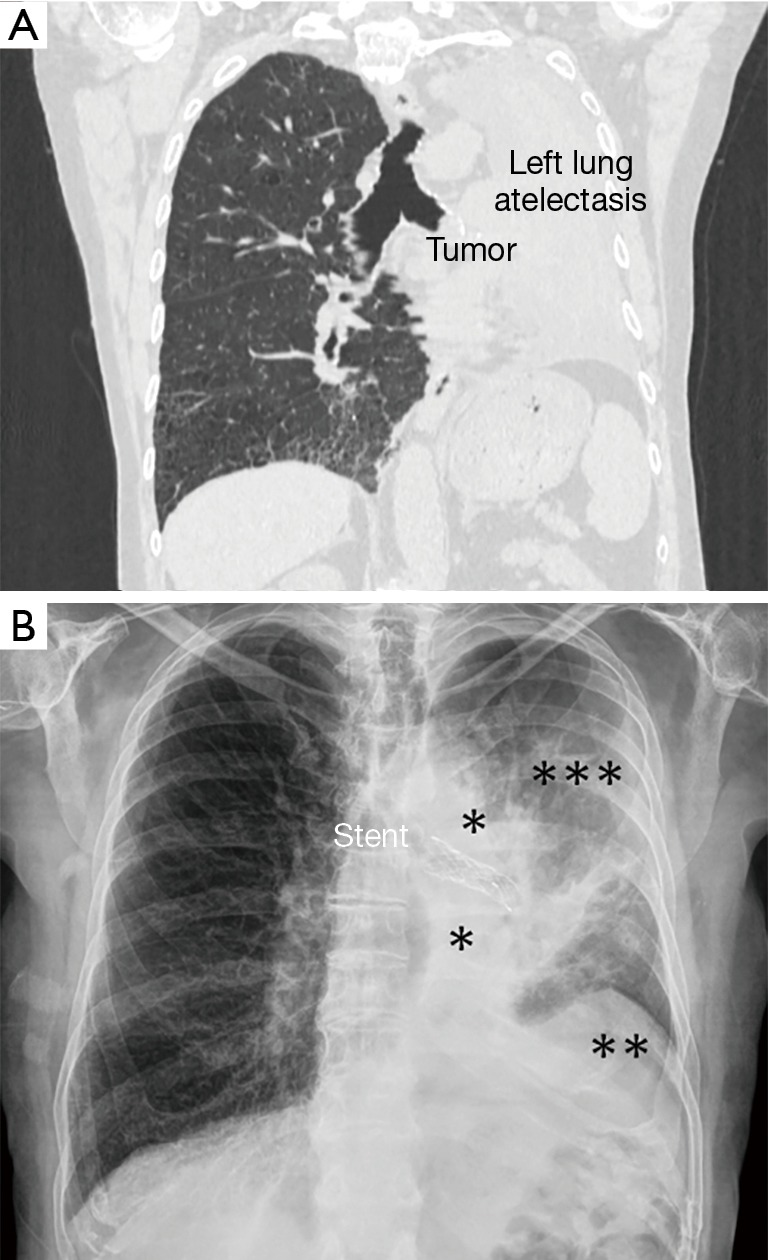
Radiological findings before treatment showed the complete atelectasis of the left lung due to neoplastic obstruction of left main bronchus (A). After treatment (B), it was evident the atelectasis of left upper lung (*) with the attraction of left diaphragm (**) and the re-expansion of the left lower lobe (***).
Discussion
Endoscopic resection with stent insertion is the mainstay treatment to assure ventilation in inoperable patients with airway malignant stenosis. From their introduction 10 years ago, SEMSs have become widely used (1). The appropriate choice of the stent is mandatory to avoid complications and decrease the health care cost. An under-sized stent increases the risk of migration while an over-sized stent cannot open with reduction of airway patency. Generally, the diameter of the stent is chosen on the preoperative measurement of the obstructed airway using computed tomography (CT) scan with 3D reconstruction, but this measurement could differ from the real diameter of the target airway after its recanalization. In the present case, before recanalization we measured the diameter of obstructed airway with CT scan but then we selected the diameter of the stent on the basis of the rigid bronchoscopy that was used for recanalization. Yet, after recanalization and before stent deployment, no additional measurement of airway diameter was performed with other endoscopic tools and that could explain the choice of an undersized stent. After stent opening, its distal end adhered to airway but there was a gap between the mid-point and the proximal end of the stent and the airway. This condition not only could increase the risk of stent migration but also favour a rapid re-growing of the tumor from the LUB to the LMB. The most effective approach in similar situation is to replace the stent with another of appropriate size in the same session but it was unfeasible in our case since a larger stent was not readily available. Furthermore, the poor clinical condition of the patient and the risk of rapid growing of the tumor discouraged us to remove the stent and to insert a new larger stent in a few days when available. Before to use FG, we dilated the stent with a balloon to see if the stent could expand further and impact in the LMB but without success. To fix the stent using laparoscopic tacks as reported by Andreetti et al. (3,4) for tracheal stent was technically unfeasible in our case since the proximal end of the stent was located too distally for allowing the tacks deployment. FG has used in a variety of cardiothoracic situations (5-8) but no papers before the present have reported its use for fixing tracheobronchial SEMS. The rationale of our procedure was to fill the gap between the stent and the LMB with the injection of FG. Then, the balloon dilation approximated the stent to the airway and favoured its adhesion. From a technical point of view, to avoid that FG obstructed distal airway, the tip of catheter was inserted in the gap between the stent and the airway and during the injection of glue, a suction was applied into the lumen of the stent and distal airways to prevent their obstruction by glue. The two components of FG were simultaneously injected to avoid that a premature clotting could occlude the double lumen catheter. There was not a standard amount of FG used during the procedure but we injected 1.5 mL of glue until the clot filled the gap; following, no suction was applied in the target area to avoid the fibrin clot dislocation.
Despite the successful outcome obtained in this case, our procedure should be considered as a temporary treatment since FG is absorbable and is unlikely to hold the stent in place over long-term. In line with this principle, we informed the patient on the opportunity of removing the stent and replacing it with another of appropriate size in a few days when available. However, the improvement of dyspnoea and general clinical condition induced the patient to refuse an additional endoscopic procedure that could delay the administration of CT and radio-chemotherapy (RT). Following, the lack of any complications during the follow-up induced us to not replace the stent. In theory, the glue was replaced by fibrotic tissue that adhered the stent to the airway and prevented further dislocation.
Finally, our procedure could be useful for physicians to resolve a challenging situation as a size-mismatched airway stent. Despite the good outcome observed in our case, it should be considered as a temporary treatment while to replace the under-sized stent with another of appropriate size remains the strategy of choice in similar cases.
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Fiorelli A, Caterino U, Raucci A, et al. A conical self-expanding metallic stent for the management of critical complex tracheobronchial malignant stenosis. Interact Cardiovasc Thorac Surg 2017;24:293-5. [DOI] [PubMed] [Google Scholar]
- 2.Fiorelli A, Messina G, Santoriello C, et al. The video edited the main steps of the procedure as the resection of the tumor, the deployment of the stent, and its fixation with fibrin glue. Asvide 2019;6:023. Available online: http://www.asvide.com/article/view/29638
- 3.Andreetti C, D’Andrilli A, Ibrahim M, et al. Treatment of a complex tracheobronchial malignant stenosis with a modified conical semicovered self-expanding stent. J Thorac Cardiovasc Surg 2013;146:488-9. 10.1016/j.jtcvs.2013.03.007 [DOI] [PubMed] [Google Scholar]
- 4.Andreetti C, Menna C, D’Andrilli A, et al. A modified technique to simplify external fixation of the subglottic silicone stent. Interact Cardiovasc Thorac Surg 2018;27:878-80. 10.1093/icvts/ivy178 [DOI] [PubMed] [Google Scholar]
- 5.Fiorelli A, Cascone R, Di Natale D, et al. Endoscopic treatment with fibrin glue of post-intubation tracheal laceration. J Vis Surg. 2017;3:102. 10.21037/jovs.2017.06.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jessen C, Sharma P. Use of fibrin glue in thoracic surgery. Ann Thorac Surg 1985;39:521-4. 10.1016/S0003-4975(10)61991-1 [DOI] [PubMed] [Google Scholar]
- 7.Störger H, Ruef J. Closure of guide wire-induced coronary artery perforation with a two-component fibrin glue. Catheter Cardiovasc Interv 2007;70:237-40. 10.1002/ccd.21115 [DOI] [PubMed] [Google Scholar]
- 8.Fiorelli A, Frongillo E, Santini M. Bronchopleural fistula closed with cellulose patch and fibrin glue. Asian Cardiovasc Thorac Ann 2015;23:880-3. 10.1177/0218492315577725 [DOI] [PubMed] [Google Scholar]