Abstract
Background
This study aimed to analyze the barriers affecting the utilization of antenatal care (ANC) among Senegalese mothers.
Methods
Health facility staffs were surveyed to examine the availability coverage of ANC (infrastructural capacity of health posts to handle maternal and newborn healthcare). A total of 113 women of childbearing age were surveyed to identify factors associated with the accessibility coverage (physical, economic, and information accessibility factors), acceptability coverage (socio-cultural features, social acceptance, and language), and effectiveness coverage (ratio of mothers having completed 4 visits) of ANC. Further, to identify the socio-cultural factors and the specific characteristics of the barriers, 5 focus group discussions were conducted with women of childbearing age, their husbands and mothers-in-law, community health workers, and health facility staff. The effectiveness coverage of ANC was analyzed by reviewing materials from the District Health Information System 2 of Senegal.
Results
Key barriers of ANC utilization were associated with acceptability coverage. ANC during early pregnancy was avoided owing to the negative social stigma surrounding miscarriage. The survey results indicated an extremely high miscarriage rate of 30.9% among the participants. The social stigma towards unmarried mothers caused them to hide their pregnancy, which deterred ANC utilization. The husband was the final decision maker and social supporter on ANC utilization.
Conclusion
To promote the utilization of ANC services among pregnant women in Senegal, it is important to alleviate the social stigma towards miscarriages and unmarried mothers, and to provide greater social support for pregnancies and newborn deliveries within family.
Keywords: Senegal, Antenatal Care, Health Care Utilization, Maternal Health, Newborn Health
Graphical Abstract
INTRODUCTION
In 2015, nearly 300,000 women over the world died due to complications affected by pregnancy and childbirth.1 It is well known that antenatal care (ANC) plays a pivotal role to decrease maternal mortality caused by perinatal complications through early detection, prompt treatment, and appropriate referral to upper level of care.1
The World Health Organization (WHO) has specified the purposes of ANC as following: providing psychological support for pregnancy, newborn delivery, breast-feeding, and child rearing; providing psychological and social support for newborn delivery, and increasing awareness on relevant matters among family members; monitoring pregnancies for the health and well-being of the mother and the newborn; monitoring signs of obstetric difficulties through diagnostic tests and paying close personal attention to pregnant mothers; and giving advice and encouragement to pregnant mothers by establishing relationships with family members or relatives who have experienced pregnancies.2
In light of this, WHO recommends a minimum of 4 ANC visits during pregnancy.3 The United Nations Development Programme (UNDP) reported that, though the ratio of pregnant mothers who have received ANC 4 or more times increased from 37% in 1990 to 52% in 2012, African countries continued to report rates of 50% or lower.4 A study on the ratio of pregnant mothers receiving ANC 4 or more times in Senegal in 2015 reported that the national average was 47.0%, that in urban areas was 57.0%, and that in rural areas was 40.0%.5 Sub-Saharan African countries, including Senegal, are considered to have a high maternal mortality ratio (MMR), and they have low rates of access to ANC.6,7
With the global efforts to reduce the MMR of Senegal was reduced by 41.7% from 1990 to 2015, yet the number of maternal deaths per 100,000 live births in 2015 was 315, which is still higher than the global average of 216 and the average of 239 among developing countries.6,7 Furthermore, a report of the WHO, which studied the ratio of pregnant mothers receiving ANC 4 or more times from 2000 to 2013, indicated that Senegal's participation in ANC ranked 23rd among the 32 African countries.7
The objective of this study was to improve maternal health services by identifying bottleneck affecting the ANC uptake using Tanahashi model. Several previous studies aimed to understand the barriers to ANC among pregnant mothers in Senegal, but have limitations in that they applied qualitative and quantitative analyses separately. Thus, this paper applied a mixed model (combining qualitative and quantitative methods) to examine the barriers to ANC with respect to the availability, accessibility, acceptability, and effectiveness coverage.
METHODS
Study settings
To reduce the MMR in Rufisque District, Senegal, Korea International Cooperation Agency (KOICA) and Better World have been implementing the “Maternal and Newborn Health Services Program” to increase the ratio of pregnant mothers receiving ANC 4 or more times, the number of pregnant mothers receiving postnatal care (PNC), and the rate of utilization of a skilled birth attendant. The Maternal and Newborn Health Services Program implemented by Better World includes the following activities: 7 key health facilities renovation, equipment upgrades, training for health workers, provision of mama kit, support for Badiene gokhs, community behavior change.
Study site was limited to the area in which the Maternal and Newborn Health Services Program was implemented by Better World. The area included 5 communes within Rufisque District (Rufisque Est, Rufisque Nord, Jaxxay, Tivaouane Peulh Niaga, and Bambylor). In total, 23 public health facilities, including 20 Posts de Santé, one regional hospital, one maternity center, and one Centre de Santé, were found to be in operation in the communes. Of these public health facilities, seven were selected for the program. They included the Centre de Santé de Rufisque and 6 Posts de Santé in Diorga, Jaxaay, Tivaouane Peulh, Niague, Bambilor, and Keur Ndiaye Lo.
Study design
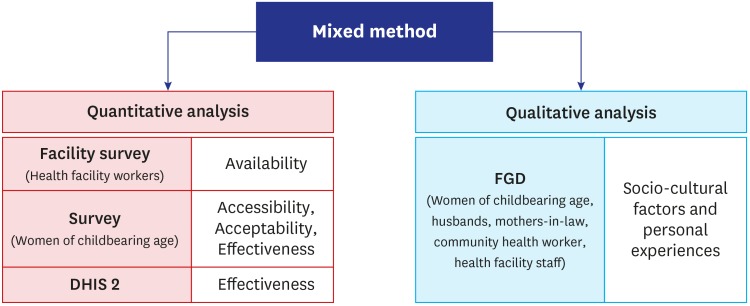
Barriers to the use of ANC were identified through Tanahashi model with mixed methods using quantitative and qualitative analyses (Fig. 1). To evaluate healthcare services, Tanahashi recommends that service utilization as well as effective coverage should be evaluated to bring about changes according to the provision of services.8 Baker et al.9 applied the Tanahashi model to perform a bottleneck analysis on coverage for maternal and newborn health interventions in Tanzania, and they identified bottlenecks in factors such as healthcare workforce, financing, and service delivery through a systematic assessment of essential maternal and newborn healthcare services.10
Fig. 1. Tanahashi model with mixed methods using quantitative and qualitative analyses.
DHIS 2 = District Health Information System 2, FGD = focus group discussion.
Quantitative analysis was conducted to check the general status of maternal healthcare services from the aspect of availability, accessibility, acceptability, effectiveness. Qualitative analysis was used to perform exploratory causal analysis in research on healthcare services. Specifically, they are used to study the quality of healthcare and to identify barriers that otherwise cannot be detected through quantitative methods.11 In addition, qualitative analysis is advantageous in that it enables the understanding of social factors or personal experiences.12
Survey tool and development method
Using the Tanahashi model, the availability, accessibility, acceptability, and effectiveness coverage of healthcare regarding the use of ANC were studied. The definitions of the coverage categories of the healthcare facilities, the survey, and the questionnaire of focus group discussions (FGDs) was developed based on WHO definitions (Table 1).
Table 1. Definition of the Tanahashi model on health service coverage.
| Health service coverage | Adjusted definition of variables |
|---|---|
| Target population | -Pregnant women in Rufisque District |
| Availability coverage | -Infrastructure status and capacity of health facilities in 5 communes: ANC and PNC availability, opening hours, maternal health care service and necessary medicine availability, BEmONC, CEmONC |
| Accessibility coverage | -Physical accessibility: waiting time (quantitative analysis) |
| -Economic accessibility: transportation fee burden, service fee burden (quantitative/qualitative analysis) | |
| -Access to information: Outreach services by Badiene gokhs and access to mass media | |
| Acceptability coverage | -Cultural factors interrupting the use of maternal health care |
| -Negative social perception | |
| -Social support encouraging maternal health care service | |
| -Language barrier | |
| Effectiveness coverage | -Rate of pregnant women who received ANC at least 4 times |
ANC = antenatal care, PNC = postnatal care, BEmONC = Basic emergency obstetric and newborn care, CEmONC = comprehensive emergency obstetrics and newborn care.
The availability of healthcare facilities providing antenatal and PNC through a Post de Santé was studied. Basic emergency obstetric and newborn care (BEmONC) and comprehensive emergency obstetrics and newborn care (CEmONC) were studied according to the seven and two more signal functions designated by WHO.13 On top of that, the status of the capacities to undertake six types of maternal and newborn healthcare tests (human immunodeficiency virus testing, venereal disease research laboratory testing for syphilis, blood test for anemia, urine test for protein, urine test for glucose, and blood test for malaria), and the availability of drugs (oxytocin, misoprostol, MgSO4, calcium, normal saline and ringer lactate) were surveyed. The percentage of tests and medicines was calculated from the total average of individually averaged percentage of each facility.
Accessibility was studied with reference to physical accessibility, economic accessibility, and access to information. Physical accessibility entailed the quantitative analysis of waiting time to use healthcare services. For economic accessibility, the expenses needed to utilize maternal and newborn healthcare as well as transportation costs needed to travel to a Post de Santé were analyzed. For access to information, the status of outreach services undertaken through Badiene gokhs serving as community health workers was analyzed.
To check the acceptability, socio-cultural factors that affect the utilization of ANC services and deter social support and visits to the Post de Santé were studied. To figure out the effectiveness, the status of pregnant mothers having visited the 19 Posts de Santé 4 or more times for ANC in 2015 and 2017 was compared.
Sampling
Facility surveys were conducted targeting the Infirmier Chef de Poste (ICP) or midwife manager of each Post de Santé from 23 health facilities in Rufisque District.
Respondents of cross-sectional survey were recruited using simple random sampling among the visitors of Centre de Santé de Rufisque and 6 Posts de Santé in Diorga, Jaxaay, Tivaouane Peulh, Niague, Bambilor, and Keur Ndiaye Lo. Each facility had a sample size of 30 or more according to central limit theorem. The common requirements for the participants was childbirth experience within the last 3 years.
Women aged 15–49 in FGD was randomly chosen among the respondents of cross-sectional study. All participants of FGD except women of childbearing age were recruited using purposive sampling. Among candidates who were recommended by local Badiene gokhs in the communes and expressed an intention to participate in the study over the phone, the participants from each group were selected considering various demographic factors.
Data collection
Facility surveys on the infrastructure and capacities for ANC and maternal and newborn healthcare in each Post de Santé were conducted on the day of regular meeting for ICP and midwife managers. Among 23 health facilities, health workers from 19 public health facilities completed the answers of the questionnaires; 4 Posts de Santé that did not participate in the surveys were excluded (Table 2).
Table 2. List of surveyed health facilities in Rufisque District.
| No. | Name of health facility | Location (Commune) |
|---|---|---|
| 1 | CS de Rufisque | Rufisque Est |
| 2 | Arafat | Rufisque Est |
| 3 | Maternite Dial Bass | Rufisque Nord |
| 4 | Diorga | Rufisque Nord |
| 5 | Dangou | Rufisque Nord |
| 6 | Fass | Rufisque Nord |
| 7 | Nimzath | Rufisque Nord |
| 8 | Jaxaay | Jaxxay |
| 9 | Niacoulrab | Jaxxay |
| 10 | Darouthioub | Jaxxay |
| 11 | Tivaouane Peulh | Tivaouane peulh Niaga |
| 12 | Niague | Tivaouane peulh Niaga |
| 13 | Apix | Tivaouane peulh Niaga |
| 14 | Tawfekh | Tivaouane peulh Niaga |
| 15 | Bambilor | Bambylor |
| 16 | Keur Ndiaye Lo | Bambylor |
| 17 | Dène | Bambylor |
| 18 | Gorom | Bambylor |
| 19 | Kounoune | Bambylor |
| 20 | Wayembam | Bambylor |
The cross-sectional survey was conducted over 4 days, and it included a total of 113 women of 15–49 year-old who visited one of the 7 public health facilities included in the study and had delivered newborns within the past 3 years (Table 3). Illiterate survey participants were interviewed by a surveyor who had received prior training on the content of the survey and method of data collection.
Table 3. Survey participants.
| Research method | Participants | Health facilities | Total | ||
|---|---|---|---|---|---|
| Rufisque Health Cente, Jaxxay, Diorga | Niague, Tivaouane Peulh | Bambilor, Keur Ndianye Lo | |||
| Quantitative analysis (n = 113) | Women aged 15–49 years | 80 | 18 | 15 | 113 |
| Qualitative analysis (n = 73) | Women aged 15–49 years | 5 | 2 | 5 | 12 |
| Mothers-in-law | 5 | 5 | 5 | 15 | |
| Husbands | 6 | 5 | 4 | 15 | |
| Badiene gokhs | 4 | 4 | 6 | 14 | |
| Health facility staff | 7 | 4 | 6 | 17 | |
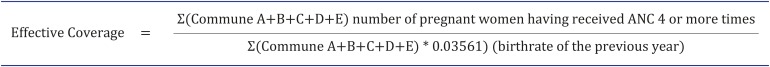
Using the District Health Information System 2 (DHIS 2) from Direction de la Santé, de la Reproduction et de la Survie de L'enfant (Department of Reproductive Health and Child Survival), the statistics of pregnant women who received ANC from January to June in 2015 and 2017 were compared to check the effects of the program interventions. The estimated number of women of childbearing age in the 5 communes was applied as the denominator in the equation used to calculate ANC usage statistics, and the number of pregnant mothers having received ANC during the relevant half-year period according to the DHIS 2 was applied as the numerator (Fig. 2).
Fig. 2. The equation used to analyze effectiveness coverage.
Since Senegal does not have a registration system for pregnant mothers, the target population of this study was estimated by applying the birthrate of the previous year to the population of the 5 communes, which was 3.56%.
ANC = antenatal care.
FGD were conducted by a moderator (preventive medicine specialist), a researcher of international public health, a Senegalese midwife (capable of speaking the local language and English), and 2 professional interpreters.
Data management
Raw data of facility survey and cross-sectional survey was entered into Statistical Package for the Social Sciences (SPSS, IBM Co., Armonk, NY, USA) version 24.0 according to the coding book. Quantitative data was investigated using frequency analysis after data cleansing.
Conversation during the whole FGD was recorded by a researcher after the translation from local language to English. The quotation of participants was directly copied from the first draft by the writer.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of the Ministry of Health and Social Action, Senegal (Reg. No. 0123/MSAS/DPRS/CNERS). Informed consent was provided by all the participants when they were enrolled.
RESULTS
Demographic characteristics of the participants
The quantitative survey included 113 women of childbearing age (Table 3). The average age of the participants was 28.5 years, 93.7% of them were married, and 80.2% of them had an educational level of primary school or lower. Further, 68.6% of the spouses of the participants had an educational level of primary school or lower (Table 4). The qualitative survey was undertaken over 4 days, and it included 12 women of childbearing age, 15 mothers-in-law, 15 husbands, 14 Badiene gokhs, and 17 public health facility staff (Table 3).
Table 4. Results of the quantitative survey.
| Variables | No. (%) (n = 111) | ||
|---|---|---|---|
| Demographics | |||
| Age, yr | |||
| 10–19 | 9 (8.1) | ||
| 20–29 | 62 (55.9) | ||
| 30–39 | 34 (30.6) | ||
| 40–49 | 6 (5.4) | ||
| Marital status | |||
| Single | 5 (4.5) | ||
| Married | 104 (93.7) | ||
| Divorced or widowed | 2 (1.8) | ||
| Race | |||
| Wolof | 36 (32.4) | ||
| Pular | 32 (28.8) | ||
| Seres | 16 (14.4) | ||
| Jola | 3 (2.7) | ||
| Soninke | 4 (3.6) | ||
| Others | 20 (18) | ||
| Women's education | |||
| Primary education | 89 (80.2) | ||
| Secondary education | 15 (13.5) | ||
| Higher education | 7 (6.3) | ||
| Employment status | |||
| Housewife (including unemployed) | 66 (59.5) | ||
| Farmer | 3 (2.7) | ||
| Merchant | 16 (14.4) | ||
| Governmental employee | 1 (0.9) | ||
| Others | 25 (22.7) | ||
| Husband's education (n = 105) | |||
| Primary education | 72 (68.6) | ||
| Secondary education | 17 (16.2) | ||
| Higher education | 16 (15.2) | ||
| Accessibility coverage | |||
| Burden of the cost of transportation to a health facility (n = 109) | |||
| Yes | 14 (12.8) | ||
| No | 95 (87.2) | ||
| Average of waiting time for maternal health services, min | 74 | ||
| Acceptability coverage | |||
| Burden of the cost of maternal health service | |||
| Yes | 20 (18) | ||
| No | 91 (82) | ||
| Miscarriage experience | |||
| Yes | 34 (30.9) | ||
| No | 77 (70) | ||
| French literacy | |||
| Yes | 42 (37.8) | ||
| No | 69 (62.2) | ||
| Decision maker of maternal health care | |||
| The woman herself | 28 (25.2) | ||
| Husband | 63 (56.8) | ||
| Mother-in-law | 15 (13.5) | ||
| Badiene gokh | 5 (4.5) | ||
| Supporter for using maternal health service | |||
| Husband | 55 (49.5) | ||
| Mother-in-law (including mother) | 23 (20.7) | ||
| Badiene gokh | 21 (18.9) | ||
| Health facility staff | 4 (3.6) | ||
| Friend | 4 (3.6) | ||
| Community leaders | 3 (2.7) | ||
| Others | 1 (0.9) | ||
| Source of information on maternal health service (n = 106) | |||
| Badiene gokh | 28 (26.4) | ||
| Mass media | 19 (17.9) | ||
| Mother-in-law (including mother) | 16 (15.1) | ||
| Friend | 14 (13.2) | ||
| Community leader | 14 (13.2) | ||
| Health facility staff | 12 (11.3) | ||
| Others | 3 (2.8) | ||
| Type of media that a respondent uses (multiple answers) | |||
| Television | 76 (68.5) | ||
| Radio | 45 (40.5) | ||
| Mobile phone | 13 (11.7) | ||
| Newspaper | 7 (6.3) | ||
| Owning a mobile phone (n = 109) | |||
| Yes | 95 (87.2) | ||
| No | 14 (12.8) | ||
| Owning a radio at home | |||
| Yes | 66 (59.5) | ||
| No | 45 (40.5) | ||
| Frequency of listening to radio (n = 108) | |||
| Almost everyday | 46 (42.6) | ||
| At least once a week | 13 (12) | ||
| Less than once a week | 17 (15.7) | ||
| Never | 32 (29.6) | ||
Service availability
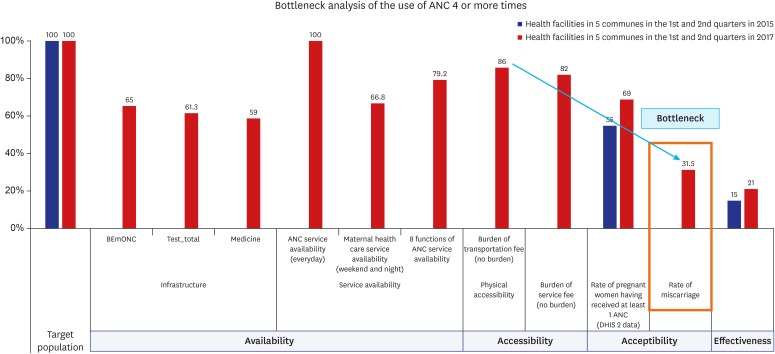
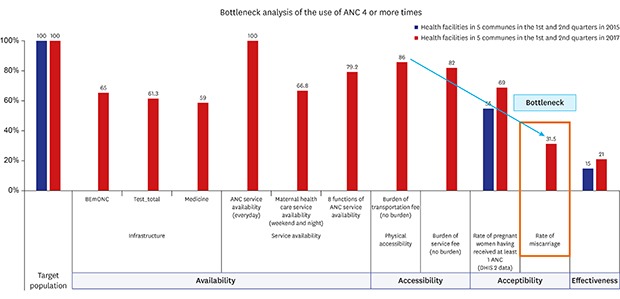
Table 5 summarizes the findings of the availability analysis. BEmONC functions were present in 65% of the 19 Posts de Santé that operated in the 5 communes, but CEmONC functions were entirely non-existent. All of 19 Posts de Santé provided ANC services on all weekdays. The availability rate of maternal and newborn healthcare operating during the weekends and at night was 66.8%, and the availability rate of 8 types of ANC functions was 79.2% (Table 5).
Table 5. Status of surveyed health facilities.
| Category | Services | 19 Health facilities in 5 Communes, % |
|---|---|---|
| Infrastructure | BEmONCa | 65.0 |
| CEmONCb | 0 | |
| ANC testc | 62.4 | |
| Medicined | 58.9 | |
| Training | ANC training for midwives | 90.0 |
| BEmONC training for health facility staff | 92.0 | |
| Maternal health care function | Maternal service availability (everyday) | 71.1 |
| ANC service availability (everyday) | 96.7 | |
| Weekend and night service availability | 66.8 | |
| Birth complication services (weekend and night services availability) | 43.5 | |
| ANC | All | 79.5 |
| Iron supplementation | 92.0 | |
| Folic supplementation | 96.0 | |
| IPT supplementation | 92.0 | |
| Tetanus supplementation | 96.0 | |
| Monitoring hypertension | 92.0 | |
| Misoprostol for home delivery | 12.0 | |
| HIV testing | 64.0 | |
| IYCF counselling | 92.0 |
BEmONC = basic emergency obstetric and newborn care, CEmONC = comprehensive emergency obstetrics and newborn care, ANC = antenatal care, IPT = intermittent preventive treatment, HIV = human immunodeficiency virus, IYCF = infant and young child feeding.
aAdministered parenteral antibiotics, administered parenteral anticonvulsants, administered parenteral oxtyocics, performed manual removal of placenta, performed removal of retained products (manual vacuum aspiration), performed assisted vaginal delivery (with vacuum extractor or forceps), performed neonatal resuscitation with bag and mask; bBlood transfusion, caesarean section plus 7 BEmONC functions; cAvailability of ANC tests: HIV testing, VDRL testing for syphilis, blood test for anemia, urine test for protein, urine test for glucose, blood test for malaria; dAvailability of medicines: oxytocin, misoprostol, Mgso4, calcium, normal saline, ringer lactate.
Physical accessibility
The surveyed women reported that the average wait time for pregnant mothers at a Post de Santé was 74 minutes. Through FGDs, no pregnant mothers indicated difficulties in physically accessing maternal and newborn healthcare services. A large number of pregnant mothers replied that it took 10 to 15 minutes to travel to Posts de Santé by walking or using public transportation. Most FGD participants reported that they arrived before 9 AM, waited for approximately 5 to 6 hours, and then participated in treatment sessions lasting up to 45 minutes per person. Most FGD participants viewed long waiting times as a problem of the maternal and newborn healthcare system in Rufisque. A lack of treatment rooms and health facility staff was considered to be the reason for the long waiting time.
“The number of health facility staff is not sufficient, and the wait time is long because there are only 1–2 treatment rooms.” (September 14, 2017, Pregnant mother #3)
“The wait time is extremely long. Some pregnant women become too tired and wait by lying on the floor. Improvements to the long waiting times and the facilities need to be made. Even when I arrive at 9 AM, the midwives are occupied with their own affairs. The treatment sessions sometimes start only after around 10 AM. The health facility staff must be more considerate of the health of pregnant mothers.” (September 14, 2017, Mother-in-law #1)
Economic accessibility
The proportion of survey participants who answered “not being economically burdened” by transportation and examination expenses to cover the utilization of maternal and newborn healthcare was 87.2% and 82.0%, respectively. Economic accessibility-related issues were analyzed by examining the effects of costs related to transportation, examination, drug purchase, child delivery, and any other services (such as ultrasonic exams and purchase of painkillers). Most FGD participants reported that they did not feel burdened by transportation costs or examination costs (XOF franc 500–1,000). The participants, however, did indicate experiencing substantial economic burden related to the purchase of drugs outside the Posts de Santé, the costs of child delivery, and additional costs associated with ultrasonic exams or the purchase of painkillers.
“In many cases the Post de Santé is not equipped with medicines. It is extremely expensive to purchase drugs outside the Posts with the prescriptions received.” (September 15, 2017, Husband #2)
“The cost of delivering a child in a Post de Santé is approximately CFA 14,000, and that of an ultrasonic exam is CFA 10,000. These are extremely expensive.” (September 18, 2017, Badiene gokh #4)
“The cost of child delivery is extremely high. The costs increase further should there be any other complications.” (September 18, 2017, Husband #1)
“Health facility staffs tend to neglect those who don't have money. It is possible to deliver children without money, but difficult to get painkillers or other drugs prescribed.” (September 18, 2017, Husband #4)
“Due to the high cost of ultrasonic exams, they cannot be undertaken during every visit. I have two children and my wife received an ultrasonic exam only once.” (September 15, 2017, Husband #3)
“I have five children, but my wife has never received an ultrasonic exam.” (September 15, 2017, Husband #4)
“Of the husbands I have met, some of them believe that ultrasonic exams are only used to identify the sex of the child.” (September 15, 2017, Badiene gokh #1)
Most of the FGD participants living in rural areas were illiterate and unemployed. These differences in the income levels of participants from rural and urban areas resulted in differences in the economic burden of using ANC services.
“In total, 6 out 10 members of my quartier feel economically burdened when using the services offered at Posts de Santé.” (September 18, 2017, Badiene gokh #1)
“I live in a rural area. Many people are illiterate and unemployed.” (September 18, 2017, Badiene gokh #2)
“There are almost no economic activities that can be undertaken in our community. Only 1 out 20 people has a job that is adequate for supporting his/her family.” (September 18, 2017, Badiene gokh #3)
Information accessibility
In total, 66 women (59.5%) reported that they owned a radio. The most popular source of information on maternal and newborn healthcare was television programs (68.5%), followed by radio programs (40.5%). Further, 54.8% of those who listened to the radio did so more than once per week (includes “everyday listeners”). Other sources of information included Badiene gokhs (26.4%), mass media (17.9%), and mothers-in-law and mothers (15.1%). Most FGD participants responded that they obtained information regarding maternal and newborn healthcare from television programs, radio programs, or their Badiene gokhs. Specifically, the FGD participants indicated that they received a considerable amount of information from television programs. The survey item pertaining to the most effective means of conveying information regarding maternal and newborn healthcare revealed that the delivery of information through Badiene gokhs' activities within a community was considered most effective.
“A television talk show ran a campaign encouraging visits to Posts de Santé. Television campaigns have become popular since around 2010.” (September 14, 2017, Mother-in-law #1)
“Approximately 90% of all households have televisions, and some even have 4 televisions.” (September 14, 2017, Mother-in-law #1)
“Even if television campaigns are launched or counseling is provided, the role of Badiene gokhs is extremely significant in recommending the use of medical services. Badiene gokhs serve as communication intermediaries between pregnant mothers and Post de Santé staff. Badiene gokhs even work in areas that are difficult to access using public transportation and they work to improve awareness regarding ANC/PNC among pregnant mothers.” (September 18, 2017, Health facility staff #6)
Social stigma surrounding miscarriage (acceptability)
Quantitative analysis showed that 30.9% of the surveyed women had miscarriage experience. There existed a high level of fear of social stigma surrounding miscarriages among pregnant mothers.
“The Senegalese culture places the responsibilities of a miscarriage on the pregnant women. Therefore, pregnancies are often kept a secret during the initial period of the pregnancy. Some mothers even travel for long distances to visit a Post de Santé so that they can keep their pregnancy a secret.” (September 14, 2017, Badiene gokh #3)
“I assume that approximately 30%–40% of pregnant mothers keep their pregnancy a secret during the initial period of their pregnancy, and therefore, they do not seek ANC.” (September 15, 2017, Badiene gokh #4)
Hiding a pregnancy due to an increase in the number of unmarried mothers (acceptability)
Most FGD participants responded that the number of unmarried mothers has been increasing. However, due to the social atmosphere, unmarried mothers keep their pregnancy a secret and find it extremely difficult to visit the Post de Santé that operates in their community. However, these problems associated with the rising number of unmarried mothers were not commonly known within local communities.
“Women who have fears concerning miscarriages or out-of-wedlock pregnancies take 6 months to seek ANC because they are busy hiding their pregnancies.” (September 15, 2017, Pregnant mother #4)
“An unmarried woman who became pregnant in our community was afraid to visit a Post de Santé out of the fear that her pregnancy would become known. Therefore, I discussed with the Post de Santé staff to allow the woman to visit the Post de Santé at less-frequented times.” (September 18, 2017, Badiene gokh #6)
Social support encouraging the utilization of maternal and newborn healthcare (acceptability)
The utilization of maternal and newborn healthcare by pregnant mothers was generally decided by the husbands or mothers-in-law of the pregnant women, rather than by the pregnant women themselves.
The final decision maker for the utilization of maternal and newborn healthcare in Senegal was mainly the husband of pregnant mothers (56.8%), followed by the pregnant mothers themselves (25.2%), and their mothers-in-law (13.5%). Further, the husband of pregnant mothers (49.5%) encouraged the utilization of maternal and newborn healthcare the most, followed by their mother and mother-in-law (20.7%), and Badiene gokhs (18.9%). Although there were some negative perceptions on the use of Posts de Santé among some husbands and mothers-in-law, as compared to the past, such perceptions have changed substantially, in the positive direction.
“I have a daughter-in-law who is pregnant, and I gave her money to visit a Post de Santé.” (September 15, 2017, Mother-in-law #1)
“Most mothers-in-law travel with the pregnant mothers to the Post de Santé. Mothers-in-law frequently visit Posts de Santé, thanks to the effects of media campaigns.” (September 14, 2017, Health facility staff #1)
“In the past, mothers-in-law were afraid to visit Posts de Santé. There were perceptions that the use of services offered at a Post de Santé would worsen illnesses. However, through education that began a couple of years ago, and the maternal and newborn healthcare activities of Badiene gokhs, the perceptions on the utilization of maternal and newborn healthcare among mothers-in-law have changed for the better.” (September 14, 2017, Badiene gokh #2)
“My mother-in-law was positive about receiving ANC. When I became pregnant, my mother-in-law encouraged me to visit a Post de Santé.” (September 15, 2017, Pregnant mother #3)
“Many changes have occurred as compared to the past. The perceptions on the utilization of maternal and newborn healthcare among husbands have changed substantially.” (September 15, 2017, Husband #3)
Difficulties in communication due to a language barrier (acceptability)
Respondents of the cross-sectional survey consists of Wolof (n = 36), Pular (n = 32), Seres (n = 16), Jola (n = 3), Soninke (n = 4), Others (n = 20) (Table 4). In the case of facility survey with ICP and midwife managers, their races are Wolof (n = 20), Pular (n = 8), Seres (n = 5), Jola (n = 1), Soninke (n = 0), Others (n = 3) (Table 4). Residents who speak other languages have difficulty in using Posts de Santé due to a language barrier.
“Pregnant mothers using Pular had difficulty in communicating with health facility staff during treatment sessions. A patient who knew Pular had to provide interpretations.” (September 18, 2017, Pregnant mother #5)
Effectiveness
In total, 15% (713 mothers) of the present participants received ANC 4 or more times from the Posts de Santé in operation in the 5 communes during the 1st and 2nd quarters of 2015. This figure increased by 6%, to 21% (1,232 mothers), during the 1st and 2nd quarters of 2017 (Fig. 3).
Fig. 3. Results of the bottleneck analysis of the use of ANC 4 or more times in the health facilities from 5 communes.
ANC = antenatal care.
DISCUSSION
Sub-Saharan African countries, including Senegal, are considered to have a high MMR, and they have low rates of access to ANC.6,7 The present analysis on the effectiveness (increase rates) of health facilities in the same quarters during a year, before and after the KOICA and Better World implemented the Maternal and Newborn Health Services Program, showed that the 15% usage rate in the first and second quarters in 2015 increased to 21% during the first and second quarters of 2017. Despite these improvements, the overall use of ANC is still considered low.
In light of such low usage rates despite an increase in the awareness of the importance of ANC, the following bottlenecks and barriers were identified in the present study from the factors affecting the utilization of maternal and newborn healthcare.
The analysis of the availability of ANC indicated that only 65.0% of all Posts de Santé were capable of providing BEmONC, while no Posts de Santé were capable of providing CEmONC. Further, 79.5% of the Posts de Santé were capable of providing ANC. WHO recommends the establishment of 5 Posts de Santé (including at least 1 Post de Santé capable of CEmONC) capable of providing BEmONC per 500,000 people.13 Despite the need to provide infrastructural support to make comprehensive facility functions available in Senegal, be difficult, the provision of support for district hospitals to fulfill comprehensive facility functions could be an option.
The present results on accessibility revealed that most women of childbearing age who participated in the FGDs did not experience any physical difficulties in visiting Posts de Santé to receive maternal and newborn healthcare. Previous research on accessibility reports a significant relationship between waiting time and ANC use,14,15 and a significant relationship between ANC use and transportation conditions.15,16 However, though most FGD participants in the present study responded that they “were not burdened” by transportation and exam expenses related to the utilization of maternal and newborn healthcare, some economically disenfranchised communes reported that economic burdens were a barrier to use. Specifically, the expenses for ultrasonic (approximately XOF franc 14,000) and for the purchase of additional drugs during childbirth were viewed as economic burdens. In the case of Ghana, although free maternal healthcare services were provided to alleviate the economic burdens related to ANC utilization, most pregnant mothers still reported that they were economically burdened by the indirect expenses associated with visiting clinics, including the purchase of clothing and hair dressing activities.17 The opportunity costs associated with not being able to prepare meals for family members or to tend to crops were also considered as a part of the economic burden.18
The present findings on access to information showed that 68.5% of the participants watched television, and most participants of the FGDs reported that they sourced information regarding maternal and newborn healthcare from television programs. Previous studies report a 2.11 times higher chance that pregnant mothers who own radio or television set will receive ANC within 12 weeks of pregnancy, as compared to pregnant mothers who do not own the same.19 The FGDs conducted in the present study revealed that the media campaigns for maternal and newborn healthcare in Senegal had a positive effect on the perceptions of mothers-in-law and husbands of pregnant women regarding ANC. A mix of community-based interventions (media campaigns, education initiatives, and incentives for pregnant mothers) and system-related interventions (home visits for pregnant women and provision of equipment to clinics) is known to improve ANC coverage (at least one visit), and to reduce perinatal mortality and the occurrence of low birth weight.20 Additionally, women of high income backgrounds were found to present higher accessibility as compared to women of lower income backgrounds.21 For low income families who reside in communities and have low access to media, the utilization of community health workers to relay information is considered efficient. This study confirmed that, in addition to media campaigns, the maternal and newborn healthcare activities of Badiene gokhs have an extremely large effect on the improvement of perceptions regarding maternal and newborn healthcare. The National Agency of Statistics and Demography (NASD) of Senegal conducted studies on access to media content (once per week) among women of childbearing age, and found differences in the rates of accessing media content among urban and rural areas.22 Specifically, the access to television programs in urban and rural areas was 85% and 35.9%, respectively, and that to radio programs in urban and rural areas was 61.2% and 51.4%, respectively. Considering the low accessibility of television programs in rural areas, it may be necessary to undertake public campaigning activities through radio programs.22
The present findings on acceptability showed that long waiting times to receive maternal and newborn healthcare, increasing numbers of unmarried mothers within local communities, fears and social stigmas associated with miscarriages, language barriers of minority ethnic groups, and high illiteracy rates among women acted as barriers to the use of ANC services. It was found that, due to the fear of being stigmatized in case of a miscarriage, pregnant mothers often hide their pregnancy until a later stage of their pregnancy. According to FGDs, unmarried mothers were especially found to display high levels of fear of being pregnant and it led to late or no ANC. Magadi revealed that greater delays on the first ANC visit resulted in a reduction in the number of women who undertake 4 or more ANC visits.23 Women who have previously miscarried were also reported to contribute to lowering the adequate frequency of ANC attendance.24
According to the World Bank, in 2013, the illiteracy rate of Senegalese women (15 years or older) was 66.4%. This rate is higher than the average illiteracy rate of 47% among sub-Saharan African women in 2010.25 In addition, in 2013, the ratio of women aged over 25 years who have completed primary school education in Senegal was 21.7%, which is considered extremely low.26 The completion of 4 ANC visits is known to be linked with the level of education of women.27,28 Further, women of childbearing age in Senegal comprise several ethnic groups that speak different languages, including Wolof (39.8%), Pular (26.5%), and Serer (15.0%).22 Language barriers are known to deter the utilization of maternal and newborn healthcare and ANC.29 A method of minimizing the language barriers experienced by some minority ethnic groups during the utilization of maternal and newborn healthcare includes the utilization of community health workers who are capable of communicating with such minorities. The use of images to provide maternal and newborn healthcare for illiterate women is another method that should be considered.
An interesting finding of the present study was that the role of mothers-in-law, who previously acted as a barrier to the use of maternal and newborn healthcare, had changed. In most cases, the ability of women to make decisions on the use of medical services in developing countries is limited by family members.30 This was also the case in Senegal. As the husbands of pregnant mothers typically found it difficult to care for their spouses due to their livelihood responsibilities, mothers-in-law typically had higher levels of responsibility and authority. Although, in the past, mothers-in-law generally viewed ANC as unnecessary,31 the present study confirmed that the perception of mothers-in-law on the use of maternal and newborn healthcare had undergone gradual changes. Considering that mothers-in-law, who are highly knowledgeable, presented a tendency to support ANC,32 it is necessary to continue promoting and educating mothers-in-law on the use of maternal and newborn healthcare.
Another interesting result of the present study was that husbands had the decision-making authority on women's use of maternal and newborn healthcare. Considering that this decision-making authority has been shifting from mothers-in-law to husbands, it is necessary to provide training and education on the benefits of early ANC as well as the expected complications of pregnancies through newly-formed husband-centered communities.
Based on the results of this study, the following recommendations are made for implementation in future programs to increase the rate of utilization of ANC and maternal and newborn healthcare 4 or more times in Rufisque, Senegal. First, considering that the long wait time experienced by pregnant mothers in Posts de Santé was a barrier to the use of ANC, efforts to minimize waiting times and the provision of waiting areas that are equipped with adequate ventilation systems are necessary.33 In addition, it may be appropriate to consider the provision of education by community health workers during waiting times, to increase awareness among pregnant mothers on maternal and newborn health.
Second, since the social stigmas and fears associated with early pregnancies and miscarriages were barriers to ANC utilization during the initial period of the pregnancy, and because it had an effect on the ratio of pregnant mothers receiving ANC 4 or more times during their pregnancy, the importance of initial ANC visits needs to be conveyed to the husbands and mothers-in-law as well as pregnant mothers. Such attempts would increase pregnant mothers' utilization of ANC services during the early phases of pregnancy.
Third, the increasing number of unmarried mothers in Senegal has resulted in increased MMR and reduced use of ANC. Thus, it is important for Badiene gokhs in the community to find out the mothers in the early stage of pregnancy and cooperate with health facility staffs at the facility. Besides, further awareness-raising education on the use of condoms needs to be undertaken in cooperation with the Direction de la Santé de Rufisque.
Fourth, husbands are getting the most influential decision-maker on the utilization of maternal and newborn healthcare among family members. Further, the social supporter for pregnant women with reference to their utilization of maternal and newborn healthcare was also husbands. Therefore, it is necessary to implement programs to train and educate husbands on the importance of ANC to improve their perceptions.
Fifth, in order to implement effective education, programs for women visiting maternal and newborn healthcare facilities (Post de Santé, Centre de Santé, etc.) need to be developed, and information regarding the use of maternal and newborn healthcare needs to be broadcasted through different media (e.g., radio and television programs). In addition, the need for ANC should be promoted through radio and television programs that are regularly accessed by local communities. A means of communicating information that accounts for the low literacy rates in developing countries also needs to be developed.
Sixth, community health workers (Badiene gokhs), the providers of maternal care in Senegal, are known to serve as a source of information on maternal health, and they are known to be supporters of maternal health. By strengthening the capacities of Badiene gokhs, a system in which they play a central role in maternal and newborn healthcare within local communities needs to be established.
This study had some limitations with analysis of availability coverage and sampling. First, “satisfaction rates regarding the use of public health facilities,” and “the capacities of health practitioners,” which are known to be related to the utilization of ANC and the services offered at Posts de Santé, were not assessed. Additionally, the quantitative surveys were conducted with women who visited Posts de Santé, a group considered to already present a high rate of utilization of medical services. Considering this limitation, FGDs with Badiene gokhs were arranged so that they would represent the status of non-respondents who do not use ANC services. Lastly, this study sampled only a few key Posts de Santé from the 5 selected communes due to a lack of public health statistics in Senegal. To apply these findings to community level, further study with greater number of participants including needs to be followed.
Despite these limitations, the present study explored the bottlenecks and barriers to the utilization of ANC healthcare services through the FGDs that included women of childbearing age as well as other interested parties such as mothers-in-law, husbands, and Badiene gokhs. Therefore, this study is considered significant in that it analyzed the barriers from a socio-cultural standpoint through the FGDs that included multiple stakeholders, which would otherwise have been difficult to derive from a purely quantitative study. Further, this study is significant in that the survey included illiterate women by conducting interviews via trained interviewers.
In conclusion, the present study identified the bottlenecks and barriers associated with the utilization of maternal and newborn healthcare by pregnant women in Rufisque District, Dakar, Senegal. Several methods to improve the rate of utilization of ANC among pregnant women were analyzed through the FGDs that included different stakeholders (women of childbearing age, husbands, mothers-in-law, health facility staff, and community health workers). The present results confirmed that, in Senegal, husbands and mothers-in-law were becoming more supportive of maternal and newborn healthcare. However, the fear of miscarriages among pregnant women delayed their initial ANC visit. These results are expected to serve as basic materials for the development of methods to improve the utilization of ANC services in Senegal.
ACKNOWLEDGMENTS
This study was made possible through help provided by Gabriel Kim, Director of the Senegal Better World Maternal and Newborn Health Services Program as well as a number of other researchers.
Footnotes
Funding: This study was implemented as monitoring and evaluation of Maternal and Newborn Health Services Program (2015–2018) which is financially supported by Global Disease Eradication Fund of Korea International Cooperation Agency (KOICA).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim KH, Choi JW.
- Data curation: Oh J, Moon J, You S, Woo YK.
- Formal analysis: Kim KH, Oh J, Moon J.
- Methodology: Kim KH, Choi JW.
- Writing - original draft: Oh J, Moon J.
- Writing - review & editing: Kim KH, Choi JW.
References
- 1.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. [Updated 2016]. [Accessed July 12, 2018]. http://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf. [PubMed]
- 2.World Health Organization. Essential antenatal, perinatal and postpartum care: training modules. [Updated 2003]. [Accessed October 10, 2017]. http://www.euro.who.int/__data/assets/pdf_file/0013/131521/E79235.pdf.
- 3.World Health Organization, United Nations International Children's Emergency Fund, United Nations Population Fund, World Bank Group, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva: World Health Organization; 2014. [Google Scholar]
- 4.United Nations Development Programme. MDG progress reports: Africa. [Updated 2015]. [Accessed October 10, 2017]. http://www.undp.org/content/undp/en/home/librarypage/mdg/mdg-reports/africa-collection.html.
- 5.United Nations International Children's Emergency Fund. [Updated December 2017]. [Accessed December 20, 2017]. https://data.unicef.org/topic/maternal-health/antenatal-care/
- 6.African Development Bank Group, OECD Development Center, United Nations Development Programme. African Economic Outlook 2016: Sustainable Cities and Structural Transformation. Paris: OECD Publishing; 2016. [Google Scholar]
- 7.World Health Organization, United Nations International Children's Emergency Fund, United Nations Population Fund, World Bank Group, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2015. Geneva: World Health Organization; 2015. [Google Scholar]
- 8.Tanahashi T. Health service coverage and its evaluation. Bull World Health Organ. 1978;56(2):295–303. [PMC free article] [PubMed] [Google Scholar]
- 9.Baker U, Peterson S, Marchant T, Mbaruku G, Temu S, Manzi F, et al. Identifying implementation bottlenecks for maternal and newborn health interventions in rural districts of the United Republic of Tanzania. Bull World Health Organ. 2015;93(6):380–389. doi: 10.2471/BLT.14.141879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickson KE, Simen-Kapeu A, Kinney MV, Huicho L, Vesel L, Lackritz E, et al. Every Newborn: health-systems bottlenecks and strategies to accelerate scale-up in countries. Lancet. 2014;384(9941):438–454. doi: 10.1016/S0140-6736(14)60582-1. [DOI] [PubMed] [Google Scholar]
- 11.Al-Busaidi ZQ. Qualitative research and its uses in health care. Sultan Qaboos Univ Med J. 2008;8(1):11–19. [PMC free article] [PubMed] [Google Scholar]
- 12.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization, United Nations Population Fund, United Nations International Children's Emergency Fund, Agile Model Driven Development. Monitoring Emergency Obstetric Care: a Handbook. Geneva: World Health Organization; 2009. [Google Scholar]
- 14.Nsibu CN, Manianga C, Kapanga S, Mona E, Pululu P, Aloni MN. Determinants of antenatal care attendance among pregnant women living in endemic malaria settings: experience from the Democratic Republic of Congo. Obstet Gynecol Int. 2016;2016:5423413. doi: 10.1155/2016/5423413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paredes I, Hidalgo L, Chedraui P, Palma J, Eugenio J. Factors associated with inadequate prenatal care in Ecuadorian women. Int J Gynaecol Obstet. 2005;88(2):168–172. doi: 10.1016/j.ijgo.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 16.Tlebere P, Jackson D, Loveday M, Matizirofa L, Mbombo N, Doherty T, et al. Community-based situation analysis of maternal and neonatal care in South Africa to explore factors that impact utilization of maternal health services. J Midwifery Womens Health. 2007;52(4):342–350. doi: 10.1016/j.jmwh.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Arthur E. Wealth and antenatal care use: implications for maternal health care utilisation in Ghana. Health Econ Rev. 2012;2(1):14. doi: 10.1186/2191-1991-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pell C, Meñaca A, Were F, Afrah NA, Chatio S, Manda-Taylor L, et al. Factors affecting antenatal care attendance: results from qualitative studies in Ghana, Kenya and Malawi. PLoS One. 2013;8(1):e53747. doi: 10.1371/journal.pone.0053747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geta MB, Yallew WW. Early initiation of antenatal care and factors associated with early antenatal care initiation at health facilities in Southern Ethiopia. Adv Public Health. 2017;2017:162424 [Google Scholar]
- 20.Mbuagbaw L, Medley N, Darzi AJ, Richardson M, Garga KH, Ongolo-Zogo P. Health system and community level interventions for improving antenatal care coverage and health outcomes. Cochrane Database Syst Rev. 2015;(12):1–157. doi: 10.1002/14651858.CD010994.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi C, Torvaldsen S, Hodgson R, Hayen A. Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data. BMC Pregnancy Childbirth. 2014;14(1):94. doi: 10.1186/1471-2393-14-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Senegal National Agency for Statistics and Demography. Enquête Démographique et de Santé Continue (EDS-Continue) [Updated 2015]. [Accessed October 10, 2017]. http://dhsprogram.com/pubs/pdf/FR320/FR320.pdf.
- 23.Magadi MA, Agwanda AO, Obare FO. A comparative analysis of the use of maternal health services between teenagers and older mothers in sub-Saharan Africa: evidence from Demographic and Health Surveys (DHS) Soc Sci Med. 2007;64(6):1311–1325. doi: 10.1016/j.socscimed.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 24.Muhwava LS, Morojele N, London L. Psychosocial factors associated with early initiation and frequency of antenatal care (ANC) visits in a rural and urban setting in South Africa: a cross-sectional survey. BMC Pregnancy Childbirth. 2016;16(1):18. doi: 10.1186/s12884-016-0807-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The World Bank Data. [Updated 2017]. [Accessed October 10, 2017]. https://data.worldbank.org/indicator/SE.ADT.LITR.FE.ZS?end=2013&locations=SN-ZG&start=1988&view=chart.
- 26.The World Bank Data. [Updated 2017]. [Accessed October 10, 2017]. https://data.worldbank.org/indicator/SE.PRM.CUAT.FE.ZS?locations=SN&view=chart.
- 27.Gupta S, Yamada G, Mpembeni R, Frumence G, Callaghan-Koru JA, Stevenson R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS One. 2014;9(7):e101893. doi: 10.1371/journal.pone.0101893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aliyu AA, Dahiru T. Predictors of delayed Antenatal Care (ANC) visits in Nigeria: secondary analysis of 2013 Nigeria Demographic and Health Survey (NDHS) Pan Afr Med J. 2017;26:124. doi: 10.11604/pamj.2017.26.124.9861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ayers BL, Hawley NL, Purvis RS, Moore SJ, McElfish PA. Providers' perspectives of barriers experienced in maternal health care among Marshallese women. Women Birth. 2018;31(5):e294–301. doi: 10.1016/j.wombi.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Furuta M, Salway S. Women's position within the household as a determinant of maternal health care use in Nepal. Int Fam Plan Perspect. 2006;32(1):17–27. doi: 10.1363/3201706. [DOI] [PubMed] [Google Scholar]
- 31.Chowdhury AM, Mahbub A. Chowdhury. The skilled attendance at delivery in Bangladesh: an ethnographic study. [Updated 2003]. [Accessed October 10, 2017]. http://research.brac.net/monographs/mono_22.pdf.
- 32.Simkhada B, Porter MA, van Teijlingen ER. The role of mothers-in-law in antenatal care decision-making in Nepal: a qualitative study. BMC Pregnancy Childbirth. 2010;10(1):34. doi: 10.1186/1471-2393-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chemir F, Alemseged F, Workneh D. Satisfaction with focused antenatal care service and associated factors among pregnant women attending focused antenatal care at health centers in Jimma town, Jimma zone, South West Ethiopia; a facility based cross-sectional study triangulated with qualitative study. BMC Res Notes. 2014;7(1):164. doi: 10.1186/1756-0500-7-164. [DOI] [PMC free article] [PubMed] [Google Scholar]