Short abstract
Objective
To compare compression screws and buttress plate (CS plus BP) with compression screws only (CS) in treating patients with Hoffa fracture.
Methods
This retrospective study included Chinese patients with Hoffa fracture treated by open reduction and internal fixation. Radiographs and clinical outcomes (range of movement [ROM], bone union and Knee Society Score [KSS]) were compared between patients treated using CS plus BP versus CS only.
Results
At 4 months following surgery, significantly better outcomes were shown in the CS plus BP group (n = 24) versus CS only group (n = 21) regarding ROM (120.4 ± 5.2° versus 110 ± 7.1°) and KSS (85.5 ± 4.1 versus 79.7 ± 3.3). At the 12-month follow-up, significantly better outcomes were maintained in the CS plus BP versus CS only group regarding ROM (126.2 ± 7.4° versus 120.5 ± 8.2°) and KSS (88.3 ± 4.6 versus 84.2 ± 4.0). At the final follow-up, all patients had normal fracture healing and no malunion, nonunion or reduction loss.
Conclusions
Fixation with CS plus BP for Hoffa fracture is effective and reliable, and may provide more adequate stability and better outcomes versus CS only.
Keywords: Hoffa fracture, compression screw, buttress plate, comparative study
Introduction
Hoffa fracture is a coronal plane fracture involving the posterior aspect of the femoral condyle, and is often associated with femoral shaft fracture.1,2 First described by Hoffa in 1904,3 this type of femoral fracture has been reported to involve both the lateral and medial condyle. Hoffa fracture has been classified by the Orthopaedic Trauma Association as a Type 33-B3 fracture,4 and typically occurs as a result of falling from a height or a motor vehicle accident,5 however, the specific mechanism remains unclear.
Hoffa fracture is rare and difficult to detect, and although anteroposterior, lateral and oblique view radiographs may be helpful, computed tomography (CT) scan is recommended if there is difficulty in making the diagnosis.6 Conservative treatment often leads to nonunion or loss of knee function, thus, surgical intervention is needed. Published reports indicate that most Hoffa fractures are treated with screws only5 or with plate and screws,7–9 however, the different types of treatment appear to result in different clinical outcomes. To the best of the authors’ knowledge, there is no published study that has evaluated a clinical comparison between the two fixation methods mentioned above. Thus, the aim of the present study was to compare the clinical outcomes of surgical treatment with compression screws and buttress plate (CS plus BP) versus compression screws only (CS) in a consecutive series of Chinese patients with Hoffa fracture.
Patients and methods
Study population
This retrospective case-series study included consecutive Chinese patients with Hoffa fracture who were treated at the Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China between May 2009 and December 2016, by open reduction and internal fixation using CS plus BP or CS only. Inclusion criteria for the study were as follows: (1) Patients aged >18 years or skeletal maturity at the time of surgical revision; (2) Diagnosis of Hoffa fracture; (3) Surgical treatment within 3 weeks of injury; and (4) Followed-up for at least 12 months. Exclusion criteria comprised: (1) Patients aged <18 years; (2) Open fractures; (3) Pathological fractures; (4) follow-up <12 months or incomplete follow-up; (5) insufficient clinical data; and (6) conservative treatment (non-surgical). Data regarding patient demographics, mechanism of injury, Letenneur classification,10 surgical parameters, and clinical outcomes (bone union [shown by radiographs], range of movement [ROM] and Knee Society Scores [KSS]) were collected from patients’ medical records. Surgical intervention was indicated for all selected patients unless, as in very rare cases, the patient was too ill to undergo surgery.
The study was approved by the Xiangya Hospital ethics committee, and written informed consent was obtained from all included participants.
Surgical technique
All surgical procedures were performed by surgeons (YZ and ZYL) in the Department of Orthopaedics, Xiangya Hospital, under general anaesthesia. A posteromedial or posterolateral approach was made according to Hoffa fracture position (medial or lateral). Following lateral or medial parapatellar release and medial or lateral dislocation of the patella, the fractured condyle was fully exposed. With 30° flexion of the knee, the Hoffa fracture fragment was reduced and preliminarily fixed using two Kirschner wires. Based on the fracture fragment and the fracture line, two cannulated lag screws were placed in a posteroanterior or anteroposterior direction. If the Hoffa fracture remained unstable following fixation with two cannulated lag screws, a locking plate was anatomically contoured and placed on the posterior side of the fractured condyle to provide angular stability.
Follow-up, evaluation and rehabilitation
All patients were reviewed at 4 and 12 months following surgery. During each review assessment, a physical examination and X-ray were performed. All patients were clinically, radiologically and functionally evaluated using ROM, bone union and Knee Society Score (KSS). A systematic guideline of rehabilitation was followed by each patient, under the supervision of a physiotherapist (ZWL) or clinician (BBL and SSZ) to regain good function of the injured knee joint. Briefly, a continuously passive motion system for knee joint exercises was used in all patients from three days following surgery. From 2 weeks post-surgery, based on different degrees of patient knee pain, the continuous passive movement range was gradually increased from 20–40° to 0–100°. During the 2–6-week postoperative period, patients began practicing non-weight-bearing exercise with the help of heel props, resistance bands or strengthening exercises on the bed. During the next 2 weeks, patients were encouraged to practice non-weight-bearing walking with the help of crutches. From 8 weeks following surgery, patients were allowed to progress to partial weight-bearing walking exercises. Elastic resistance was used for muscle strengthening. As long as bone union was indicated by X-ray examination, full weight-bearing was allowed from 4 months post-surgery.
Following hospital discharge, patients underwent a self-administered rehabilitation program under the guidance of a physiotherapist (ZWL) or clinician (BBL and SSZ) via telephone or WeChat app (Tencent Co. Ltd., Shenzhen, China).
Statistical analyses
Statistical analyses were performed using SPSS, version 12.0 (SPSS Inc, Chicago, IL, USA) for windows. Data are presented as mean ± SE, except where indicated otherwise. Continuous variables were analysed between groups using independent samples t-test while categorical data were analysed using χ2-test. A P value <0.05 was considered to be statistically significant.
Results
A total of 45 consecutive patients with Hoffa fracture were treated by open reduction and internal fixation, comprising 27 males and 18 females, aged from 19 to 57 years (Table 1). The mechanism of injury was motor or vehicle accident in 32 patients and falling in 13 patients. According to Letenneur classification,10 the number of patients with type I, type II and type III fractures was 15, 12, and 18, respectively. A total of 24 patients were treated using CS plus BP (15 males and 9 females, aged 25–53 years) and 21 patients were treated using CS only (12 males and 9 females, aged 19–57 years).
Table 1.
Demographic and clinical data of patients with Hoffa fracture at presentation.
|
Treatment group |
||
|---|---|---|
| Compression screws and plate | Compression screws only | |
| Characteristic | n = 24 | n = 21 |
| Age, years | 37.2 (25–53) | 32.6 (19–57) |
| Sex | ||
| Male | 15 | 12 |
| Female | 9 | 9 |
| Anatomical side | ||
| Left | 10 | 7 |
| Right | 14 | 14 |
| Letenneur Classification | ||
| I | 8 | 7 |
| II | 6 | 6 |
| III | 10 | 8 |
| Mechanism of injury | ||
| Vehicle | 17 | 15 |
| Falling | 7 | 6 |
Data presented as mean (range), or n patient prevalence.
There were no statistically significant between-group differences (P > 0.05).
There were no statistically significant differences between patients treated with CS plus BP and those treated with CS only in terms of age, sex, anatomical side of fracture, Letenneur classification and mechanism of fracture (Table 1). All participants were treatment compliant and there were no missing clinical data. Mean duration of surgery and mean blood loss were significantly higher in the CS plus BP group than the CS only group (mean duration of surgery, 88 [range, 72–113] min versus 72 [69–89] min, P = 0.03; mean blood loss, 93.0 [range, 73–121] ml versus 78.3 [69–89] ml, P = 0.02, CS plus BP versus CS only; Table 2). There was no statistically significant difference between the two groups in terms of screw direction (anterior to posterior, 10/24 versus 9/21, CS plus BP versus CS only). A search of the published literature regarding Hoffa fracture treatment revealed several similar studies, which are summarized in Table 3 and reviewed in the discussion.
Table 2.
Clinical outcomes in patients with Hoffa fracture treated with compression screws and plate or compression screws only.
|
Treatment group |
|||
|---|---|---|---|
| Characteristic | Compression screws and platen = 24 | Compression screws onlyn = 21 | Statistical significance |
| Duration of surgery, min | 88.1 (72–113) | 72.0 (59–86) | P = 0.03 |
| Blood loss, ml | 93.0 (73–121) | 78.3 (69–89) | P = 0.02 |
| Screw direction | |||
| AP | 10 | 9 | NS |
| PA | 14 | 12 | NS |
| Knee ROM, ° | |||
| 4 months | 120.4 ± 5.2 | 110 ± 7.1 | P < 0.01 |
| 12 months | 126.2 ± 7.4 | 120.5 ± 8.2 | P < 0.05 |
| KSS points | |||
| 4 months | 85.5 ± 4.1 | 79.7 ± 3.3 | P < 0.01 |
| 12 months | 88.3 ± 4.6 | 84.2 ± 4.0 | P < 0.01 |
| Stability | |||
| Yes | 24 | 21 | NS |
| No | 0 | 0 | NS |
| Time to bone union, months | 3.5 ± 1.1 | 4 ± 1.3 | NS |
Data presented as mean (range), n prevalence or mean ± SE.
AP, anterior to posterior; PA, posterior to anterior; ROM, range of movement; KSS, Knee Society Score.
NS, no statistically significant between-group difference (P > 0.05).
Table 3.
Demographic and clinical outcome data in recently published studies concerning surgical treatment of patients with Hoffa fracture.
| First author | Publication year | Study period | Patients (M/F) |
Letenneur classification |
Mean Age (years) | Treatment | Screw direction | Mean follow-up (months) | Mean time to bone union (weeks) | Mean ROM | Mean KSS | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | |||||||||||
| Onay9 | 2018 | January 2000–December 2010 | 13 (11/2) | 7 | 3 | 3 | 27.5 | Two screws | AP/PA | 93 | N/A | 110° | 78.4 |
| Singh18 | 2017 | 2011–2014 | 7 (5/2) | N/A | N/A | N/A | 39.8 | Two screws | AP | 28 | N/A | 111° | 87.5 |
| Trikha16 | 2017 | January 2010–March 2015 | 32 (25/7) | N/A | N/A | N/A | 34.7 | Two screws or two screws and plate | AP | >12 | 11.6 | 116° | 83.2 |
| Xu14 | 2016 | April 2004–July 2013 | 11 (8/3) | 7 | 0 | 4 | 38.5 | Three screws | AP/Cross | 27.1 | 11.4 | N/A | 88.8 |
| 16 (11/5) | 10 | 0 | 6 | 38.2 | Two screws | AP | 11.9 | N/A | 87.9 | ||||
| Zhao8 | 2016 | May 2006–May 2014 | 17 (13/4) | 8 | 4 | 5 | 32.5 | Two or three screws and plate | PA | 14.6 | 20.1 | N/A | 91.1 |
| Gao7 | 2015 | February 2005–February 2013 | 13 (8/5) | 3 | 6 | 4 | 49 | One or two screws and plate | PA | 23.5 | 15.2 | 124.6° | 85.6 |
| Current study | 2018 | May 2009–December 2016 | 24 (15/9) | 8 | 6 | 10 | 37.2 | Two screws and plate | AP/PA | 12 | 15 | 126.2° | 88.3 |
| 21 (12/9) | 7 | 6 | 8 | 32.6 | Two screws | AP/PA | 12 | 17.1 | 120.5° | 84.2 | |||
Data presented as n prevalence or mean value.
M, male; F, female; AP, anterior to posterior; PA, posterior to anterior; ROM, range of movement; KSS, Knee Society Score.
After 4 months following surgery, mean ROM was 120.4 ± 5.2° in the CS plus BP group and 110 ± 7.1° in CS only group (P < 0.01), and mean KSS was 85.5 ± 4.1 in the CS plus BP group and 79.7 ± 3.3 in CS only group (P < 0.01), indicating that patients treated using CS plus BP had greater ROM and KSS values. At the 12-month follow-up, there remained a significant difference in ROM (126.2 ± 7.4° versus 120.5 ± 8.2°, P < 0.05) and KSS (88.3 ± 4.6 versus 84.2 ± 4.0, P < 0.01) between the CS plus BP group and CS only group. Postoperative radiographs showed that all patients had anatomic reduction with stable fixation (P > 0.05). At the final follow-up, all patients had normal fracture healing and no malunion, delayed union, nonunion or reduction loss. No statistically significant difference was found in time to bone union between the two treatment groups (P > 0.05).
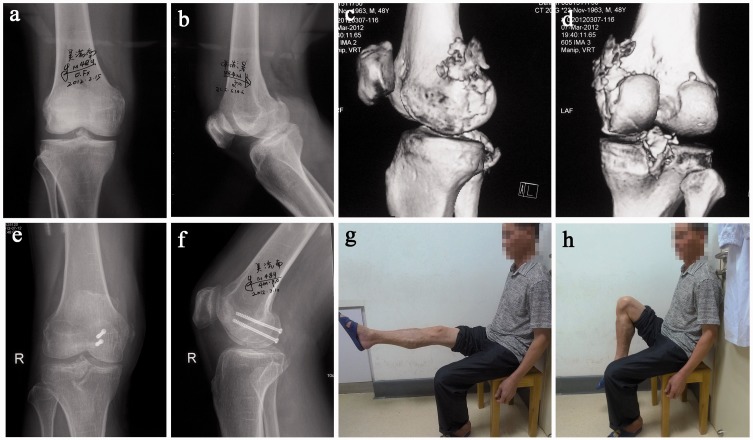
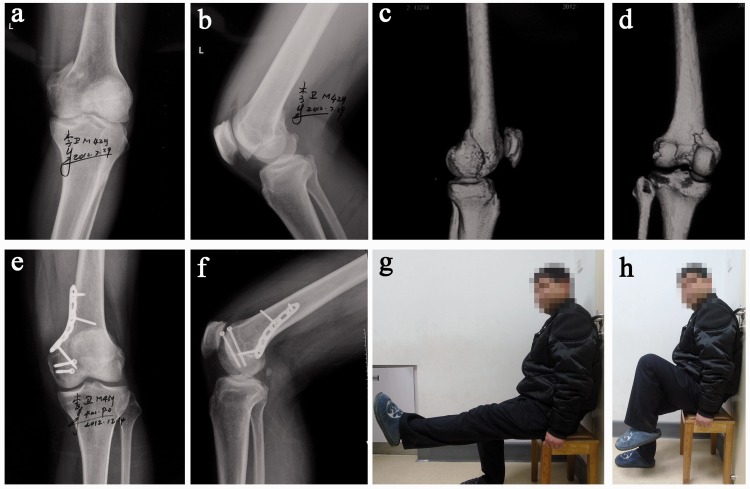
Two cases included in the current study are highlighted as representative examples. Case 1, a 48-year-old male patient, acquired a type II Hoffa fracture of the right knee (Figure 1 a–d) due to a fall. Under general anaesthesia, two cannulated lag screws were placed at the posteromedial distal femoral condyle in the posteroanterior direction. At four months following surgery, radiographs showed that there was no secondary displacement and the fracture line was obscure (Figure 1 e–f). At the 12-month follow-up, right knee ROM was 0–120° and the patient had attained a stable and functional knee (Figure 1 g–h). Case 2, a 42-year-old male patient, acquired a type III Hoffa fracture of the left knee (Figure 2 a–d) due to a motor vehicle accident. A buttress plate and two cannulated lag screws were placed as shown in Figure 2 e–f. At four months following surgery, X-ray images showed that the fracture line in this patient was also obscure. At the one-year follow-up, the patient had completely recovered and knee ROM was 0–125° (Figure 2 g–h).
Figure 1.
Representative case from the current study of a 48-year-old male patient with a type II Hoffa fracture acquired following a fall: (a) anteroposterior and (b) lateral knee radiographs showed a Hoffa fracture which was not detected by healthcare professionals; (c and d) computed tomography reconstructions clearly demonstrating the fracture; (e) anteroposterior and (f) lateral radiographs at four months following surgery, showing that the fracture had adequate stability and no displacement; (g and h) representative images at 12 months following surgery, showing the patient with a stable and functional knee.
Figure 2.
Representative case from the current study of a 42-year-old male patient with type III Hoffa fracture acquired during a motor vehicle accident: (a) anteroposterior and (b) lateral knee radiographs, and (c and d) computed tomography reconstructions showing the Hoffa fracture; (e and f) radiographs showing a buttress plate and two cannulated lag screws placed during surgical treatment; and (g and h) representative images at the final 12-month follow-up, at which the patient had completely recovered knee function.
Discussion
Hoffa fracture is well known as an intra-articular coronal fracture of the distal femur, yet it remains one of the most difficult fractures to treat.11 Conservative management has shown unsatisfactory results and nonunion,12,13 thus, open reduction with internal fixation is mandatory for good clinical outcomes.11 Screw fixation is generally accepted as a standard method for treating Hoffa fractures,11,14 with the internal fixation method undergoing continual improvement. At least two screws should be used to provide biomechanical stability,5,14,15 and the screws must vertically cross the fracture line to achieve compression between the fragments. Results from several studies have shown that Hoffa fracture treated with screws from anterior to posterior or the opposite direction are associated with different clinical outcomes (Table 3).5,7,9,14 In addition, a few trials have reported that Hoffa fracture treated with screws and plate also provides good clinical results (Table 3).7,8,16
A relatively new fixation method for Hoffa fracture, that involved using intercondylar screw and crossed screws, was shown to be as effective as conventional methods and may provide a new way to treat Hoffa fractures.14 In several studies that were reviewed, Hoffa fractures were reported to be treated with different sizes and numbers of screws,9,14,17,18 and the clinical outcomes were acceptable. However, due to the shear stress required to displace the fragment,19 the stability of the screws may be mechanically insufficient in flexion,20 particularly in the early stage of rehabilitation.21
Fixation stability is an important factor for fracture healing.22–24 To get more purchase for fixation, favorable biomechanical and clinical studies demonstrated that a buttress plate could provide more stability to the Hoffa fracture and was associated with good clinical outcomes.8,25–28 One study reported on 10 cases of Hoffa fracture that were treated by posterior screw combined with anti-sliding plate. All the fractures had healed at the final follow-up and, according to Letenneur score for knee function,29 the excellent-to-good rate was 90%. In another study that included 12 cases of lateral Hoffa fractures treated with a locking plate and cannulated or lag screw,15 bony union was achieved in all patients and no loss of reduction and fixation was found. According to the KSS, all patients in the study had excellent-to-good results.15 In a retrospective cohort study, which included 13 Hoffa fractures treated with open reduction and internal fixation using a locking plate combined with cannulated or lag screws,7 clinical outcomes were as good as the study conducted by Shi et al.15
A search of the relevant literature revealed no clinical comparative study of CS plus BP and CS only to treat Hoffa fracture. Most of the published clinical trials reported that Hoffa fractures were treated by either screws only or plate combined with screws. To the best of the present authors’ knowledge, this is the first clinical comparison of the efficacy of CS plus BP and CS only for treatment of Hoffa fracture. A total of 45 participants were included in the present study and there was no statistically significant difference between the two patient groups in terms of baseline demographic and clinical characteristics. The duration of surgery, and levels of blood loss were significantly higher in the CS plus BP group than in the CS only group. This was because more time and a larger incision were needed to place the plate during surgery, which resulted in a longer operating time and higher levels of blood loss. Patients in the CS plus BP group had better outcomes in terms of ROM and KSS values at the 4- and 12-month follow-ups, however, the difference between the two groups reduced between the 4- and 12-month follow-ups. The patients may have attained better outcomes due to the plate providing greater stability, which could prevent the fragment from moving upward, thus maintaining postoperative stability.15 At the final follow-up in the present study, all patients displayed normal fracture healing, however, patients in the CS plus BP group had better outcomes in terms of ROM and KSS. These data suggest that adding a plate when treating Hoffa fracture may provide firmer fixation stability resulting in better outcomes.
The results of the present study may be limited by several factors. First, due to a very low incidence of Hoffa fracture, the sample size in this trial was relatively small. Secondly, the outcomes in patient subgroups characterized by fracture classification were not analysed, due to the small sample size. Type II fracture, for example, may be a completely intra-articular fracture, and the condylar fragment has no soft tissue attachment,10 thus, to prevent nonunion of the fracture, strong fixation is needed.7,15 The patients with Type II Hoffa fracture should, therefore, have better outcomes in the CS plus BP group. Thirdly, this was a retrospective study, and selection bias may have produced distorted results. Prospective randomized trials are needed to further evaluate the relative efficacy of CS plus BP versus CS only in treating patients with Hoffa fracture.
In summary, fixation with compression screws and buttress plate for Hoffa fracture was shown to be an effective and reliable treatment procedure in patients with Hoffa fracture, and may provide greater stability and better outcomes, in terms of ROM and KSS, than screws only. More high-quality randomized clinical trials are needed to verify the present results.
Declaration of conflicting interests
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by Hunan Provincial Natural Science Foundation (2016JJ6165).
References
- 1.Nork SE, Segina DN, Aflatoon K, et al. The association between supracondylar-intercondylar distal femoral fractures and coronal plane fractures. J Bone Joint Surg Am 2005; 87: 564–569. [DOI] [PubMed] [Google Scholar]
- 2.Vaishya R, Singh AP, Dar IT, et al. Hoffa fracture with ipsilateral patellar dislocation resulting from household trauma. Can J Surg 2009; 52: E3–E4. [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffa A. Lehrbuch der Frankturen und Luxationen. Stuttgart: Ferdinand Enke-Verlag, 1904, pp. 451–453 [In German]. [Google Scholar]
- 4.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007; 21(10 Suppl): S1–S133. [DOI] [PubMed] [Google Scholar]
- 5.Gavaskar AS, Tummala NC, Krishnamurthy M. Operative management of Hoffa fractures–a prospective review of 18 patients. Injury 2011; 42: 1495–1498. [DOI] [PubMed] [Google Scholar]
- 6.Holmes SM, Bomback D, Baumgaertner MR. Coronal fractures of the femoral condyle: a brief report of five cases. J Orthop Trauma 2004; 18: 316–319. [DOI] [PubMed] [Google Scholar]
- 7.Gao M, Tao J, Zhou Z, et al. Surgical treatment and rehabilitation of medial Hoffa fracture fixed by locking plate and additional screws: A retrospective cohort study. Int J Surg 2015; 19: 95–102. [DOI] [PubMed] [Google Scholar]
- 8.Zhao LL, Tong PJ, Xiao LW. Internal fixation with lag screws plus an anti-sliding plate for the treatment of Hoffa fracture of the lateral femoral condyle. Zhongguo Gu Shang 2016; 29: 266–269 [in Chinese, English abstract]. [PubMed] [Google Scholar]
- 9.Onay T, Gulabi D, Colak I, et al. Surgically treated Hoffa fractures with poor long-term functional results. Injury 2018; 49: 398–403. [DOI] [PubMed] [Google Scholar]
- 10.Letenneur J, Labour PE, Rogez JM, et al. Hoffa's fractures. Report of 20 cases (author's transl). Ann Chir 1978; 32: 213–219 [in French, English abstract]. [PubMed] [Google Scholar]
- 11.Tetsunaga T, Sato T, Shiota N, et al. Posterior buttress plate with locking compression plate for Hoffa fracture. J Orthop Sci 2013; 18: 798–802. [DOI] [PubMed] [Google Scholar]
- 12.Ozturk A, Ozkan Y, Ozdemir RM. Nonunion of a Hoffa fracture in an adult. Chir Organi Mov 2009; 93: 183–185. [DOI] [PubMed] [Google Scholar]
- 13.Singh AP, Dhammi IK, Vaishya R, et al. Nonunion of coronal shear fracture of femoral condyle. Chin J Traumatol 2011; 14: 143–146. [PubMed] [Google Scholar]
- 14.Xu Y, Li H, Yang HH, et al. A comparison of the clinical effect of two fixation methods on Hoffa fractures. Springerplus 2016; 5: 1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shi J, Tao J, Zhou Z, et al. Surgical treatment of lateral Hoffa fracture with a locking plate through the lateral approach. Eur J Orthop Surg Traumatol 2014; 24: 587–592. [DOI] [PubMed] [Google Scholar]
- 16.Trikha V, Das S, Gaba S, et al. Analysis of functional outcome of Hoffa fractures: a retrospective review of 32 patients. J Orthop Surg (Hong Kong) 2017; 25: 2309499017718928. [DOI] [PubMed] [Google Scholar]
- 17.Cai CY, Dong YL, Huang YJ, et al. Treatment of Hoffa fracture using hollow lag screw. Zhongguo Gu Shang 2012; 25: 435–437 [in Chinese, English abstract]. [PubMed] [Google Scholar]
- 18.Singh R, Singh RB, Mahendra M. Functional outcome of isolated Hoffa fractures treated with cannulated cancellous screw. Malays Orthop J 2017; 11: 20–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang L, Xia Z, Luo Z, et al. Low plasma PDGF-BB levels are associated with estradiol in postmenopausal osteoporosis: PDGF-BB mediated by estradiol in women. J Int Med Res 2017; 45: 1332–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Long H, Lin Z, Lu B, et al. Percutaneous compression plate versus dynamic hip screw for treatment of intertrochanteric hip fractures: a overview of systematic reviews and update meta-analysis of randomized controlled trials. Int J Surg 2016; 33(Pt A): 1–7. [DOI] [PubMed] [Google Scholar]
- 21.Shi Y, He G, Lee WC, et al. Gli1 identifies osteogenic progenitors for bone formation and fracture repair. Nat Commun 2017; 8: 2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Long HT, Deng ZH, Zou M, et al. Effects of the acetabular fracture index and other factors of posterior wall acetabular fracture on functional outcome. J Int Med Res 2017; 45: 1394–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo Y, Zhou HD, Feng YZ. Effects of hybrid coat on shear bond strength of five cements: an in vitro study. J Adv Prosthodont 2017; 9: 447–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng L, Long HT, Sun BH, et al. The efficacy of a multimodal analgesia protocol in preventing heterotopic ossification after acetabular fractures surgery. Int J Clin Pharm 2017; 39: 826–830. [DOI] [PubMed] [Google Scholar]
- 25.Greiwe RM, Archdeacon MT. Locking plate technology: current concepts. J Knee Surg 2007; 20: 50–55. [DOI] [PubMed] [Google Scholar]
- 26.Tejwani NC, Guerado E. Improving fixation of the osteoporotic fracture: the role of locked plating. J Orthop Trauma 2011; 25(Suppl 2): S56–S60. [DOI] [PubMed] [Google Scholar]
- 27.Jarit GJ, Kummer FJ, Gibber MJ, et al. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma 2006; 20: 273–276. [DOI] [PubMed] [Google Scholar]
- 28.Dare AJ, Hu G. China's evolving fracture burden. Lancet Glob Health 2017; 5: e736–e737. [DOI] [PubMed] [Google Scholar]
- 29.Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br 1989; 71: 118–120. [DOI] [PubMed] [Google Scholar]