Short abstract
This series of case reports describes six eyes from five patients that underwent intraocular lens (IOL) exchange with scleral-fixated IOLs for cystoid macular oedema associated with iris-fixated IOLs between 2005 and 2015. Macular oedema was assessed using ocular coherence tomography (OCT). The six eyes in this series were treated by IOL removal and implantation of a scleral-sutured IOL with four points of fixation in the sulcus. Visual acuity improved in all six eyes. On OCT, macular oedema resolved after 3 months in all eyes. There were no surgical complications from the IOL exchange. One eye had a pupilloplasty and another had a diaphragm IOL to treat a major iris impairment from prior surgeries. The cause of cystoid macular oedema in these cases remains controversial but has been well recognized in eyes with iris-sutured IOLs. The absence of sutures with posterior fixation of an iris claw IOL prevents progressive corneal endothelial cell loss but does not prevent macular oedema, even in vitrectomized eyes. In conclusion, macular oedema resolved and visual acuity improved after implant exchange with a secondary scleral-fixated IOL in these cases. This procedure should be considered as a solution to persistent symptomatic cystoid macular oedema from an iris-fixated implant.
Keywords: Iris claw lens, scleral-sutured intraocular lens, cystoid macular oedema, complications, iris-fixated intraocular lenses
Introduction
Multiple solutions exist to treat aphakia in cases of posterior capsular disruption following complicated cataract surgery or trauma, including angle-fixated intraocular lenses (IOL), iris fixation with or without sutures, and scleral fixation. Because of endothelial cell loss related to angle-fixated IOLs, many surgeons prefer the last two options.
Iris-fixated IOLs1 appeared in the early 1980s and rapidly became popular,2 but lost favour to anterior chamber implants until the iris claw IOL was introduced, clipped to the front or more recently to the back of the iris. Vitreoretinal traction and low-grade uveitis are the two common hypotheses to explain recalcitrant cystoid macular oedema that can complicate iris claw IOLs.3,4 In our opinion, low-grade, sub-clinical, anterior uveitis generated by an iris-fixated IOL can lead to chronic and resistant cystoid macular oedema requiring IOL explantation. This current report describes a series of cases that experienced this complication and were treated between 2005 and 2015 by the Department of Ophthalmology, ophthalmologic foundation A. de Rothschild, Paris, France. The report also provides a discussion of their management.
Case reports
Case number 1
In May 1982, a 77-year-old woman had bilateral intracapsular cataract extractions with implantation of iris-fixated Binkhorst 4 loop IOLs. In July 2005, 6 months after a spontaneous mild left vitreous haemorrhage, a sudden decrease of her left visual acuity occurred to 2/10 Snellen with a correction of +14.00 –1.00 × 80° because of luxation of the IOL into the anterior chamber associated with mild stromal corneal oedema. The patient was referred to our emergency service and marked macular oedema was observed. After removal of the dislocated IOL, posterior vitrectomy and insertion of a 28 dioptre scleral-fixated IOL, the visual acuity improved to 10/10 Snellen with a correction of –1.25 –2.00 × 55°.
One year later, the right eye developed decreased vision to 5/10 Snellen from cystoid macular oedema with thickening to 639 microns. Her IOL had one loop fixated to the iris with a prolene suture (standard fixation technique) and was tilting. No inflammation was visible in the anterior chamber. She underwent replacement of the Binkhorst IOL with a 28 dioptre scleral-sutured IOL and vitrectomy. One month later, the right visual acuity was stable at 10/10 Snellen with –3.50 –0.50 × 175° and the macular oedema resolved. At 10-year follow-up, the visual acuity remained unchanged in both eyes.
Case number 2
A 56-year-old man presented 1.5 months after complicated left cataract surgery with a very decentred posterior chamber IOL in June 2010. The IOL was removed and replaced with a posterior iris claw IOL with vitrectomy. Eleven months later, the left visual acuity was 3/10 Snellen with –025 –2.75 × 170°. Ocular coherence tomography (OCT) revealed cystoid macular oedema of 300 microns. The central endothelial cell count was Oculus Dexter (OD) 2432 and Oculus Sinister (OS) 1198 cells/mm2.
A posterior vitrectomy was performed through separate pars plana incisions. During surgery, it was observed that the iris claw was clipped on one side to the ciliary body and on the other side to the residual lens capsule. The iris claw IOL was removed through a temporal 7 mm incision on bare sclera, 3 mm behind the limbus, followed by tunnelling anteriorly with a crescent knife to create a corneo-scleral flap. Then the anterior chamber was entered through clear cornea under the flap with a 3.2 mm knife to enlarge to 11 mm, necessary to allow implantation of a 22 dioptre diaphragm IOL with 10 mm narrowest diameter. The implant was sewn into the sulcus with four prolene 10/0 sutures, two for each haptic, tied on bare sclera (two sutures for the inferior haptic and two for the superior haptic). Correct localization in the sulcus was assured by transillumination using an endocular fibre optic illuminator that shows the sulcus as a white line between two darker lines corresponding to the iris root anteriorly and ciliary body posteriorly. The diaphragm IOL corrected pre-existent iris damage.
One month after surgery, the visual acuity improved to 10/10 Snellen. OCT showed a normal macular profile of 239 microns thick.
Case number 3
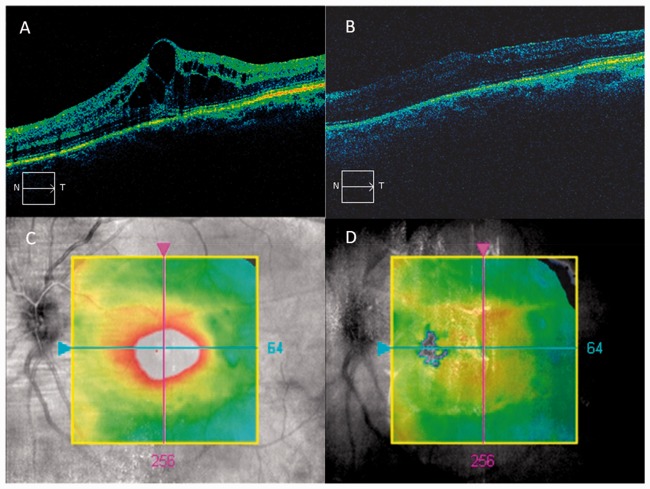
The right eye of a 72-year-old man with previous scleral buckling for a retinal detachment underwent cataract surgery with implantation of an anterior iris claw IOL in November 1997. One year later, a vitrectomy with epiretinal membrane peeling was performed because of reduced vision to 1/10 Snellen. Postoperatively, the right visual acuity oscillated between 2/10 and 8/10 Snellen with –5.50 –0.75 × 165° because of persistent macular oedema. In February 2012, the right corrected visual acuity was at 4/10 Snellen and the iris claw lens was decentred causing monocular diplopia. OCT revealed increased cystoid macular oedema. Replacement of the iris claw with a scleral-sutured IOL was performed with complete visual recovery (10/10 Snellen) with plano –2.50 × 135° after a few months (Figure 1).
Figure 1.
Macular ocular coherence tomography of the right eye of a 72-year-old man (case number 3) preoperatively (A) showing cystoid macular oedema with loss of the foveal depression and intra-retinal cysts in the outer and inner nuclear layer of the retina; and 6 months postoperatively (B) showing restoration of the normal foveal depression and macular anatomy. The images of the macula shown in C and D confirm that the images shown in A and B were taken through the fovea at the same retinal point. Macular oedema resolved considerably by the 6-month postoperative follow-up examination. Note the colour scale highlighting the macular oedema (red and white) (C) and the restoration to a normal macular profile (green and red) at 6 months postoperatively (D).
Case number 4
A 77-year-old woman's left eye underwent cataract surgery in November 2013 with ruptured capsular bag and an anterior iris claw IOL. In early 2014, her left visual acuity oscillated between 3/10 and 6/10 Snellen due to persistent cystoid macular oedema (645 microns in September 2015) unresponsive to medical therapy. After removal of her iris claw IOL and implantation of an acrylic hydrophobic 28 dioptre scleral-sutured implant, the left visual acuity improved to 9/10 Snellen with +0.75 –1.75 × 90° and the fovea was normal on OCT (239 microns).
Case number 5
A 65-year-old myopic male patient underwent right retinal detachment surgery in August 2003 and uncomplicated cataract surgery with in-the-bag IOL in June 2004. Postoperative visual acuity was 10/10 Snellen with –1.50 –2.00 × 175°. In October 2014, bag luxation occurred with superior zonulolysis, which was treated with vitrectomy and implantation of an anterior iris claw IOL. Cystoid macular oedema following this surgery was resistant to steroidal and non-steroidal anti-inflammatory drops as well as multiple anti-vascular endothelial growth factor injections. Ultimately, an intravitreal steroid implant (Ozurdex®) was performed; however, the iris claw lens was unstable with eye movement and macular thickness was 507 microns with corrected visual acuity of counting fingers. In October 2015, the iris claw IOL was removed and replaced with an acrylic hydrophobic scleral-sutured implant. One month later, macular OCT showed a normal fovea but visual acuity was limited to 2/10 Snellen because of corneal oedema.
Discussion
This current report presents a series of six eyes from five patients treated consecutively between 2005 and 2015 with iris-fixated IOLs, four iris claw and two Binkhorst four loop IOLs, all with important visual acuity impairment from cystoid macular oedema resistant to medical therapy. After exchange of the iris-fixated IOL with a scleral-sutured IOL and thorough posterior vitrectomy if not already performed, all six eyes had rapid resolution of macular oedema with good visual improvement (pre- and postoperative overview presented in Tables 1 and 2). This short series illustrates the association of iris-fixated IOLs with chronic cystoid macular oedema and the benefit on visual acuity of IOL exchange even with longstanding macular oedema. Interestingly, even in the case of chronic macular oedema, visual acuity increased to 10/10 Snellen, except in one case, highlighting the limited damage of the photoreceptors.
Table 1.
Demographic and clinical data of the five cases described in this report.
| Case | Age, years | Implant type | Preoperative visual acuity | Postoperative visual acuity |
|---|---|---|---|---|
| 1 OS | 77 | Binkhorst with four loops | 0.25 | 1 |
| 1 OD | 77 | Binkhorst with four loops | 0.5 | 1 |
| 2 OS | 56 | Iris claw | 0.32 | 1 |
| 3 OS | 72 | Iris claw | 0.4 | 1 |
| 4 OD | 77 | Iris claw | 0.3 | 0.6 |
| 5 OD | 65 | Iris claw | 0.05 | 0.16 |
OS, oculus sinister; OD, oculus dexter.
Table 2.
Vitreous status and evolution of cystoid macular oedema before and after iris-fixated lens removal based on ocular coherence tomography assessment of the five cases.
| Case | Previous vitrectomy | Implant: type, diameter and power | Preoperative ocular coherence tomography | Postoperative ocular coherence tomography | Preoperative astigmatism | Postoperative astigmatism |
|---|---|---|---|---|---|---|
| 1 left eye | – | PMMA7 mm28D | 420 µm | 270 µm | 1D | 1.25D |
| 1 right eye | – | PMMA7 mm28D | 450 µm | 270 µm | 2D | 1.5D |
| 2 | + | Diaphragm IOL10 mm16,5 | 300 µm | 240 µm | 1.25D | 2.25D |
| 3 | + | PMMA7 mm11D | 450 µm | 240 µm | 1.25D | 2.25D |
| 4 | + | Acrylic hydrophobic28D | 470 µm | 250 µm | 2.25D | 2.00D |
| 5 | + | Acrylic hydrophobic16,5D | 507 µm | 260 µm | 2.00D | 1.00D |
PMMA, Polymethyl Methacrylate; IOL, intraocular lens.
One explanation of the macular oedema in these cases could be chronic low-grade irritation of the iris. Although there was no evidence of inflammatory cells or flare (i.e. foggy appearance of the aqueous humor due to protein leaking from inflamed blood vessels) in the anterior chamber, it was not possible to exclude subclinical low-grade inflammation. If there is, in fact, no direct inflammatory mediator passing through the vitreous perhaps there is an inflammatory connection between the uveal tissue of the iris and choroid. Low-grade anterior uveitis in such cases has three likely origins: first, a lack of IOL stability causing movement of the IOL against the iris because insufficient iris tissue is captured in the claw or from iris progressive atrophy in the claw; secondly, microscopic imperfections in the surface of the IOL rubbing on the iris; and thirdly, malposition of the iris claw on the ciliary body. The stability of an iris-fixated implant depends on the quality of the grip of its claws.5,6 This can be appreciated with fixation on the anterior iris surface of the iris but is less evident with posterior surface iris fixation. Our first case, with a large iris defect, illustrates this with the posterior claw lens clipped on the ciliary body and a capsule remnant. Technical difficulty, insufficient trapped iris tissue or trapping of the ciliary body with posterior fixation, may partially explain the reported rates of cystoid macular oedema as high as 25%.7–10 Luxation of iris claw IOLs occurs with a rate between 6.0% and 8.7%.11,12 Another explanation for chronic, resistant cystoid macular oedema with iris-fixated IOLs is persistent vitreous traction after incomplete vitrectomy. This is supported by a lower cystoid macular oedema rate with posterior fixation of iris claw lenses in previously vitrectomized eyes.13 See literature review on cystoid macular oedema and luxation rate in Table 3.8–12,14 In this current series, four eyes had a posterior vitrectomy when the iris claw IOL was explanted and none of our patients had vitreomacular traction syndrome. The relationship between cystoid macular oedema and luxation or subluxation of iris claw lenses has been investigated but no clear conclusion could be established.3 In this current series, one implant was dislocated in the anterior chamber, two implants were slightly displaced due to a perforation of the iris by a claw, and one implant was stable on the iris plane but with marked iridodonesis. The Binkhorst IOL in case 1 of the current series had only one loop fixated by suture to the iris. In all of these current cases, the iris claw implant was generating micro-trauma to the iris and probably causing low-grade uveitis.
Table 3.
Literature review regarding cystoid macular oedema and luxation rate in the presence of an iris claw.
| Author | Year of publication | Number of eyes | Mean follow-up time, months | CMO | IOL subluxation |
|---|---|---|---|---|---|
| Mohr A et al.14 | 2002 | 48 | 12 | 6.2% | 0% |
| Acar N et al.11 | 2010 | 12 | 16 | 8.3% | 8.3% |
| De Silva SR et al.12 | 2011 | 116 | 22 | 7.7% | 6% |
| Gonnermann J et al.9 | 2012 | 137 | 5 | 8.7% | 8.7% |
| Guëll JL et al.8 | 2014 | 128 | 42 | 4.3% | 1% |
| Labeille E et al.10 | 2014 | 32 | 6 | 25% | 0% |
CMO, cystoid macular oedema; IOL: intraocular lens.
Visual acuity has been reported to be decreased in up to 23% of patients with iris claw lenses.14 Usually, this visual loss is transient and only a few patients suffer from chronic macular oedema (0.8%).12,15
The role of vitrectomy in the treatment of the cystoid macular oedema is well established.16–18 Four of the current cases were previously vitrectomized, therefore it is possible that explantation of the iris-fixated implant was sufficient to resolve the macular oedema as suggested by Gelender in 1984.4
Replacement of an iris-clipped IOL with a scleral-sutured implant in cases of chronic and resistant macular oedema should be strongly considered. The scleral-sutured implant has a long history.19,20 The major complication of this technique is the secondary luxation.21 To overcome this complication, a glued IOL technique was proposed some years ago.22,23 A comparative study of these two techniques has shown a similar rate of transient cystoid macular oedema.24,25 We have not experienced secondary luxation with prolene four suture fixation, attaching the sutures around a poly(methyl methacrylate) IOL haptic or soft hydrophobic acrylic IOL haptic so no sharp edge can harm the suture. In this current case series, the postoperative induced astigmatism was very low considering the size of the incision. Table 2 shows the effect of surgery on macular thickness assessed by OCT depending on the vitreous status and ocular astigmatism assessed by subjective refraction.
Limitations of this current case series are the retrospective nature of the study and the small size of the series.
In conclusion, this small case series demonstrates the complication of chronic, medication-resistant, cystoid macular oedema from iris-fixated IOLs. The removal of the iris-fixated implant was effective and associated with functional and anatomical recovery. While some feel a higher level of skill and experience is required to perform scleral fixation, we prefer this technique in cases where in the capsular bag or sulcus fixation is not felt to be safe.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Worst JG. Iris claw lens. J Am Intraocul Implant Soc 1980; 6: 166–167. [DOI] [PubMed] [Google Scholar]
- 2.Menezo JL, Martinez MC, Cisneros AL. Iris-fixated Worst claw versus sulcus-fixated posterior chamber lenses in the absence of capsular support. J Cataract Refract Surg 1996; 22: 1476–1484. [DOI] [PubMed] [Google Scholar]
- 3.Pendergast SD, Margherio RR, Williams GA, et al. Vitrectomy for chronic pseudophakic cystoid macular edema. Am J Ophthalmol 1999; 128: 317–323. [DOI] [PubMed] [Google Scholar]
- 4.Gelender H. Corneal endothelial cell loss, cystoid macular edema, and iris-supported intraocular lenses. Ophthalmology 1984; 91: 841–846. [DOI] [PubMed] [Google Scholar]
- 5.Salchow DJ, Sinard J. Management of lens dislocation and iris cyst after iris sutured intraocular lens implantation in children with Marfan syndrome. J Pediatr Ophthalmol Strabismus 2013; 50 Online: e8–e10. [DOI] [PubMed] [Google Scholar]
- 6.Mertens E, Tassignon MJ. Detachment of iris claw haptic after implantation of phakic worst anterior chamber lens: case report. Bull Soc Belge Ophtalmol 1998; 268: 19–22. [PubMed] [Google Scholar]
- 7.Hirashima DE, Soriano ES, Meirelles RL, et al. Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome. Ophthalmology 2010; 117: 1479–1485. [DOI] [PubMed] [Google Scholar]
- 8.Guëll JL, Verdaguer P, Elies D, et al. Secondary iris-claw anterior chamber lens implantation in patients with aphakia without capsular support. Br J Ophthalmol 2014; 98: 658–663. [DOI] [PubMed] [Google Scholar]
- 9.Gonnermann J, Klamann MK, Maier AK, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg 2012; 38: 2139–2143. [DOI] [PubMed] [Google Scholar]
- 10.Labeille E, Burillon C, Cornut PL. Pars plana vitrectomy combined with iris-claw intraocular lens implantation for lens nucleus and intraocular lens dislocation. J Cataract Refract Surg 2014; 40: 1488–1497. [DOI] [PubMed] [Google Scholar]
- 11.Acar N, Kapran Z, Altan T, et al. Secondary iris claw intraocular lens implantation for the correction of aphakia after pars plana vitrectomy. Retina 2010; 30: 131–139. [DOI] [PubMed] [Google Scholar]
- 12.De Silva SR, Arun K, Anandan M, et al. Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg 2011; 37: 1667–1672. [DOI] [PubMed] [Google Scholar]
- 13.Gonnermann J, Torun N, Klamann MK, et al. Posterior iris-claw aphakic intraocular lens implantation in subluxated lenses due to Marfan syndrome. Eur J Ophthalmol 2014; 24: 352–357. [DOI] [PubMed] [Google Scholar]
- 14.Mohr A, Hengerer F, Eckardt C. Retropupillary fixation of the iris claw lens in aphakia. 1 year outcome of a new implantation techniques. Ophthalmologe 2002; 99: 580–583 [in German, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 15.Michelson JB, Friedlaender MH, Nozik RA. Lens implant surgery in pars planitis. Ophthalmology 1990; 97: 1023–1026. [DOI] [PubMed] [Google Scholar]
- 16.Schepens CL, Avila MP, Jalkh AE, et al. Role of the vitreous in cystoid macular edema. Surv Ophthalmol 1984; 28: 499–504. [DOI] [PubMed] [Google Scholar]
- 17.Tranos P, Scott R, Zambarakji H, et al. The effect of pars plana vitrectomy on cystoid macular oedema associated with chronic uveitis: a randomised, controlled pilot study. Br J Ophthalmol 2006; 90: 1107–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ikeda T, Sato K, Katano T, et al. Vitrectomy for cystoid macular oedema with attached posterior hyaloid membrane in patients with diabetes. Br J Ophthalmol 1999; 83: 12–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malbran ES Malbran E Jr.andNegri Aranguren A.. Scleral-fixated intraocular lenses. Arch Ophthalmol 1988; 106: 1347–1348. [DOI] [PubMed] [Google Scholar]
- 20.Kjeka O, Bohnstedt J, Meberg K, et al. Implantation of scleral-fixated posterior chamber intraocular lenses in adults. Acta Ophthalmol 2008; 86: 537–542. [DOI] [PubMed] [Google Scholar]
- 21.Balta FN. Surgical technique for repositioning subluxated previously scleral-fixated intraocular lenses. Am J Ophthalmol 2004; 138: 676–677. [DOI] [PubMed] [Google Scholar]
- 22.Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg 2007; 33: 1851–1854. [DOI] [PubMed] [Google Scholar]
- 23.Scharioth GB, Prasad S, Georgalas I, et al. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg 2010; 36: 254–259. [DOI] [PubMed] [Google Scholar]
- 24.Sindal MD, Nakhwa CP, Sengupta S. Comparison of sutured versus sutureless scleral-fixated intraocular lenses. J Cataract Refract Surg 2016; 42: 27–34. [DOI] [PubMed] [Google Scholar]
- 25.Le Quoy O, Papaefthymiou Y. Sclerally fixated intraocular lens implant associated with vitrectomy: a study of 50 cases. J Fr Ophtalmol 2003; 26: 1051–1058 [in French, English Abstract]. [PubMed] [Google Scholar]