Short abstract
Background
Acupuncture and non-steroidal anti-inflammatory drugs (NSAIDs) are used frequently to treat primary dysmenorrhoea. However, it is unclear whether this treatment greatly reduces the risk of primary dysmenorrhoea.
Methods
Eight databases were searched up to January 2018. Pair-wise and network meta-analyses were conducted to synthesize data from eligible studies.
Results
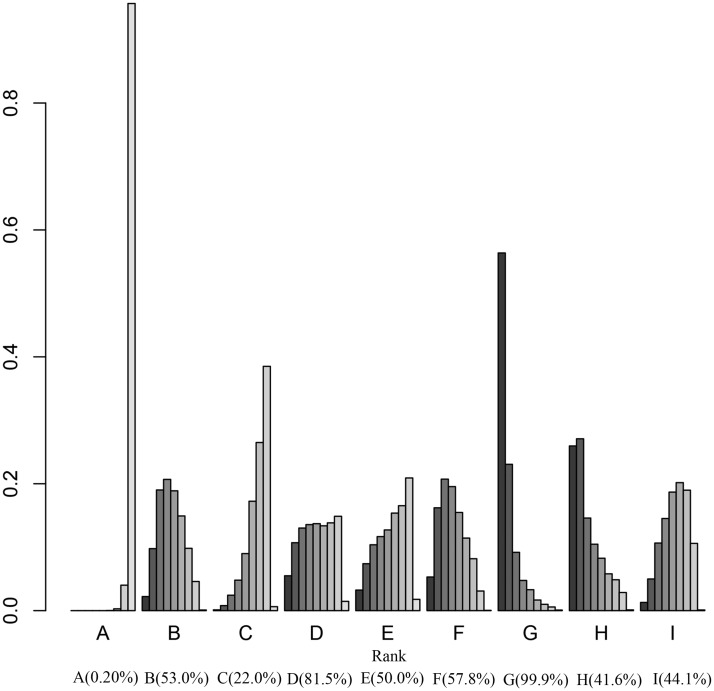
Seventeen randomized controlled trials were included. The following acupuncture types showed more efficacy than NSAIDs in reducing primary dysmenorrhoea risk: traditional acupuncture (odds ratio [OR] = 6.70, 95% confidence interval [CI] 2.60–20.0), eye acupuncture (OR = 3.50, 95% CI 1.40–8.90), wrist–ankle acupuncture (OR = 6.00, 95% CI 1.30–32.0), superficial acupuncture (OR= 5.10, 95% CI 1.20–26.0), moxibustion (OR = 7.70, 95% CI 2.90–25.0), electroacupuncture (OR = 23.0, 95% CI 4.80–130), ear acupuncture (OR = 13.0, 95% CI 2.80–100) and abdominal acupuncture (OR = 5.30, 95% CI 2.10–16.0). Surface under the cumulative ranking curve values were traditional acupuncture (53.0%), eye acupuncture (22.0%), wrist–ankle acupuncture (81.5%), superficial acupuncture (50.0%), moxibustion (57.8%), electroacupuncture (99.9%), ear acupuncture (41.6%) and abdominal acupuncture (44.1%).
Conclusion
Acupuncture is more efficacious than NSAIDs in reducing primary dysmenorrhoea risk. Acupuncture, particularly electroacupuncture, can decrease the risk of primary dysmenorrhoea.
Keywords: Primary dysmenorrhoea, acupuncture, non-steroidal anti-inflammatory drugs, randomized controlled trial, network meta-analysis, electroacupuncture
Introduction
Primary dysmenorrhoea is characterized by the presence of lower abdominal pain and distension in the lower abdomen before and after menstruation in the absence of organic lesions in the reproductive organs. It is one of the most common gynaecological symptoms and can severely affect quality of life.1 Primary dysmenorrhoea accounts for more than 90% of dysmenorrhoea, and is most common in adolescence.2 Dysmenorrhoea is a common problem and can occur in 50% of menstruating women.3 There are many current approaches to treat dysmenorrhoea, such as oral administration of traditional Chinese medicine, external use of traditional Chinese medicine,4 acupuncture5 and non-steroidal anti-inflammatory drugs (NSAIDs).6,7
According to Western medicine, primary dysmenorrhoea is associated with increased levels of prostaglandins.8 Oral pain relief is often prescribed for dysmenorrhoea symptoms, but they are often ineffective or slow-acting.8 NSAIDs are widely used as the first-line therapy for females with dysmenorrhoea.7 The traditional Chinese medicine interpretation of primary dysmenorrhoea is stagnation of qi and blood. By improving qi and blood flow, acupuncture can not only reduce symptoms, but also improve the quality of life of dysmenorrhoea patients.9
Acupuncture and NSAIDs are commonly used to treat primary dysmenorrhoea. Xu et al. found that acupuncture therapy is more efficacious than NSAIDs in reducing the risk of primary dysmenorrhoea.10 However, it is unclear whether all types of acupuncture therapy are efficacious in treating primary dysmenorrhoea, and which acupuncture therapies provide the most efficacy in primary dysmenorrhoea treatment. We conducted a network meta-analysis of randomized controlled trials to determine the efficacy and safety of NSAIDs-controlled acupuncture in primary dysmenorrhoea treatment.
Methods
Search strategy
Eligible studies were systematically searched to January 2018 using Medline, Embase, Web of Science, Cochrane Database, Chinese Academic Journals Full-text Database, Chinese Science and Technology Journal Full-text Database, Wanfang Data and Chinese Biomedical Literature Database. The keywords were “Primary Dysmenorrhoea” [MeSH] OR “Menstrual Pains” [MeSH] AND “Acupuncture” [MeSH] OR “Acupuncture Therapy” [MeSH] AND “NSAIDs” [MeSH] OR “Non-Steroidal Anti-Inflammatory Agents” [MeSH] OR “Anti-Inflammatory Analgesics” [MeSH] OR “Aspirin Like Agents” [MeSH].
Inclusion criteria and data extraction
We only included randomized controlled trials written in English, regardless of whether the authors mentioned specific random allocation methods, randomization distribution schemes, or blinding methods. No restriction was placed on date of publication. Subjects in all trials were diagnosed with primary dysmenorrhoea. All studies focused on the effect of acupuncture compared with NSAIDs on primary dysmenorrhoea.
We input the studies retrieved from the database into EndNote and eliminated duplicate documents. We read the titles and abstracts according to the elements in the PICOS approach (participants, interventions, comparators, outcomes and study design) to conduct preliminary screening, and then read the full text. The data were extracted and evaluated by two staff members, who discussed and resolved any differences. All relevant data were recorded for each study, including first author name, publication time, sample size, age, and intervention measures. Quality evaluation was conducted using the Cochrane risk of bias tool.11
Statistical analysis
The risk of primary dysmenorrhoea in each group was compared using the odds ratios (ORs) and the 95% confidence intervals (95% CIs). A summary effect (pooled OR) was produced for each pair-wise comparison using a meta-analytic approach (fixed-effect model). The validity of the fixed-effect model was assessed by examining study heterogeneity in each pair-wise comparison. The degree of heterogeneity was quantified using Cochran’s Q and I2 statistics. If the P value of Cochran’s Q test statistic is less than 0.05 or the I2 statistic is larger than 50%, this indicates significant heterogeneity among included studies for each pair-wise comparison. As a result, the fixed-effect model may not be appropriate for synthesizing direct evidence and the random-effects model should be used instead.
We conducted a network meta-analysis (Bayesian approach) that included both direct and indirect evidence in the network. Acupuncture types were ranked based on the surface under the cumulative ranking curve (SUCRA) values. Adjuvant treatments with greater SUCRA values are considered preferable. The presence of small study effects or publication bias was visually assessed using funnel plots.
Results
Literature search results
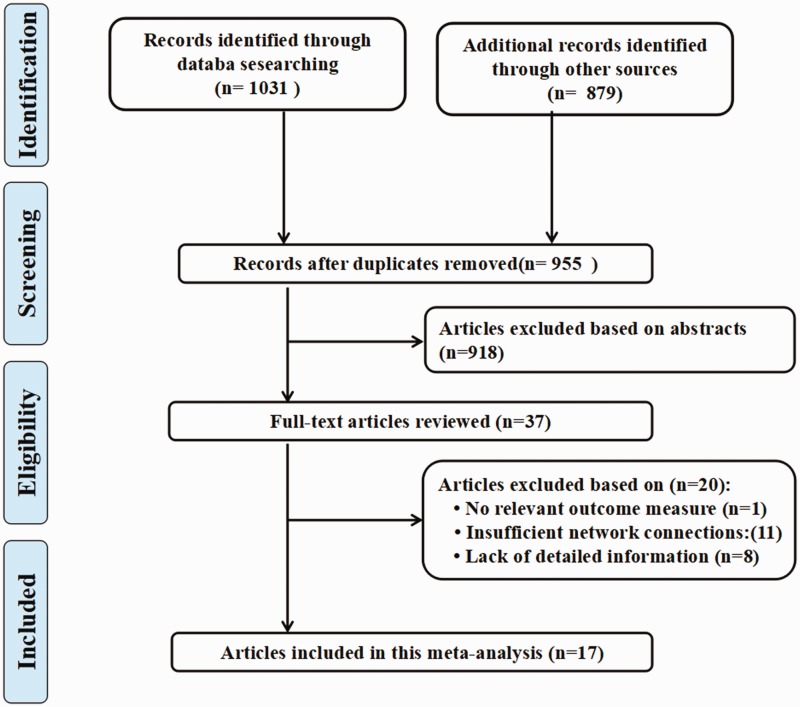
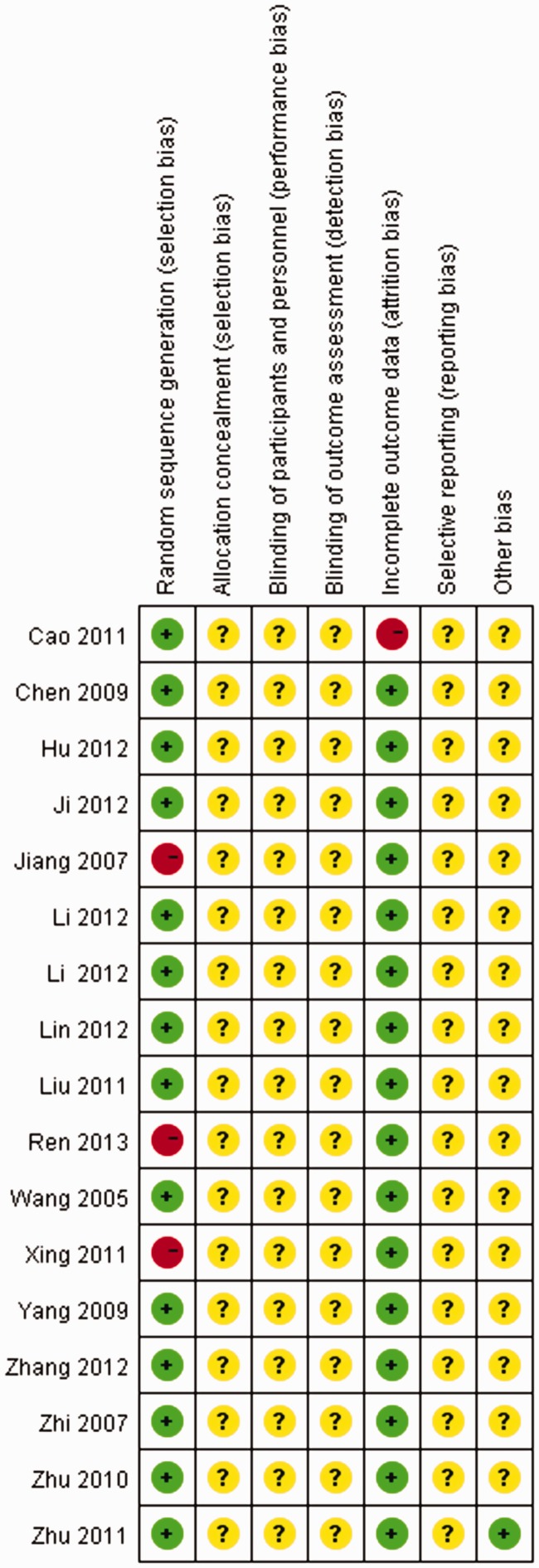
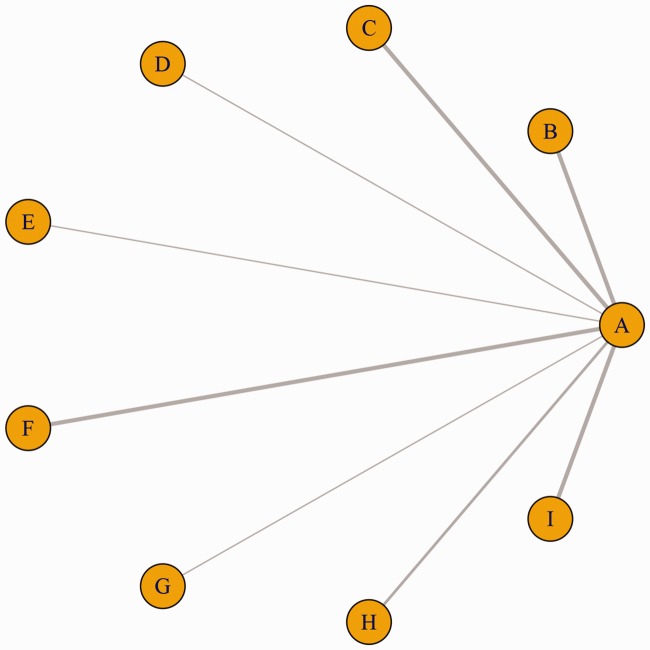
After removing duplicated studies, 955 studies were identified from the eight databases. After reviewing their titles and abstracts, 918 citations were excluded. The remaining 37 citations were assessed in more detail for eligibility by reading the full text. Of these, 1 study was excluded owing to lack of a relevant outcome measure, 11 studies were excluded because of insufficient network connections and 8 studies were excluded owing to a lack of detailed information. A total of 17 studies were used for the final data synthesis. The flow chart of the literature search is shown in Figure 1. The risk of bias of the 17 studies included in this meta-analysis is summarized in Figure 2. The characteristics of the included studies are shown in Table 1.12–28 The pattern of evidence in the network is displayed in Figure 3.
Figure 1.
Flow diagram of the study selection process.
Figure 2.
Risk of bias of the included randomized controlled trials (review authors’ judgments about each risk of bias item for each included study. + indicates low risk; − indicates high risk; ? indicates unclear risk).
Table 1.
Characteristics of included studies.
| Author (year) | No. of Participants | Treatments |
|||||
|---|---|---|---|---|---|---|---|
| Treatments 1 | Age (year) | Case/n | Treatments 2 | Age (year) | Case/n | ||
| Zhang et al. (2012) | 90 | Traditional acupuncture | 13–27 | 42/45 | Indometacin | 11–25 | 32/45 |
| Lin et al. (2012) | 140 | Eye acupuncture | 15–30 | 76/80 | Ibuprofen | 15–30 | 48/60 |
| Hu et al. (2012) | 110 | Eye acupuncture | 15–30 | 57/60 | Ibuprofen | 15–29 | 41/50 |
| Cao (2011) | 59 | Wrist–ankle acupuncture | 15–29 | 25/29 | Ibuprofen | 20–28 | 16/30 |
| Zhi (2007) | 120 | Superficial acupuncture | 19.60 ± 3.20 | 56/60 | Indometacin | 18.93 ± 2.60 | 45/60 |
| Ren (2013) | 80 | Moxibustion | 16–28 | 36/40 | Ibuprofen | 16–27 | 34/40 |
| Zhu et al. (2010) | 102 | Moxibustion | 18–26 | 47/51 | Indometacin | 19–25 | 39/57 |
| Li (2012) | 60 | Electroacupuncture | 19–30 | 24/30 | Fenbid | 19–25 | 5/30 |
| Wang et al. (2005) | 58 | Ear acupuncture | 16–28 | 29/30 | Indometacin | 15–24 | 18/28 |
| Yang (2009) | 72 | Abdominal acupuncture | 14–28 | 34/36 | Indometacin | 13–27 | 29/36 |
| Chen et al (2006) | 58 | Abdominal acupuncture | 16–28 | 29/30 | Indometacin | 15–24 | 18/28 |
| Liu et al. (2011) | 80 | Moxibustion | 21.22 ± 5.86 | 39/40 | Fenbid | 20.96 ± 6.12 | 29/40 |
| Zhu et al. (2011) | 40 | Traditional acupuncture | 17–28 | 19/20 | Indometacin | 18–27 | 16/20 |
| Li et al. (2012) | 200 | Traditional acupuncture | 13–30 | 96/100 | Ibuprofen | 14–35 | 77/100 |
| Jiang (2007) | 68 | Ear acupuncture | 19.35 ± 4.33 | 33/34 | Indometacin | 20.55 ± 4.51 | 29/34 |
| Xing (2011) | 114 | Abdominal acupuncture | 15–27 | 55/60 | Indometacin | 16–32 | 42/54 |
| Ji et al. (2012) | 60 | Moxibustion | 22 ± 3 | 29/30 | Indometacin | 22 ± 2 | 25/30 |
Figure 3.
Network of randomized controlled trials comparing different acupuncture therapies for primary dysmenorrhoea treatment. The thickness of the connecting lines represents the number of trials between each comparator, and the size of each node corresponds to the number of subjects who received the same pharmacological agent (sample size). (A: Non-steroidal anti-inflammatory drugs [NSAIDs]; B: Traditional acupuncture; C: Eye acupuncture; D: Wrist–ankle acupuncture; E: Superficial acupuncture; F: Moxibustion; G: Electroacupuncture; H: Ear acupuncture; I: Abdominal acupuncture).
Results of pair-wise meta-analysis
Table 2 shows the results of the pair-wise meta-analysis. The following types of acupuncture appeared to show more efficacy than NSAIDs in reducing the risk of primary dysmenorrhoea: traditional acupuncture (OR = 7.10, 95% CI 2.80–21.0), eye acupuncture (OR = 3.90, 95% CI 1.50–9.10), wrist–ankle acupuncture (OR = 5.60, 95% CI 1.30–31.0), superficial acupuncture (OR = 5.10, 95% CI 1.20–24.0), moxibustion (OR = 7.60, 95% CI 2.80–27.0), electroacupuncture (OR = 22.0, 95% CI 4.50–120), ear acupuncture (OR = 13.0, 95% CI 2.70–130), and abdominal acupuncture (OR = 5.50, 95% CI 2.10–16.0). In addition, there was low heterogeneity among studies (P-heterogeneity > 0.05 and I2 < 50%) (Table 2).
Table 2.
Summary odds ratios of acupuncture and heterogeneity for each direct comparison.
| Comparison | OR (95% CI) | P-heterogeneity | I-squared | Tau-squared |
|---|---|---|---|---|
| Traditional acupuncture vs. NSAIDs | 7.10 (2.80, 21.0) | 0.697 | <0.01% | <0.001 |
| Eye acupuncture vs. NSAIDs | 3.90 (1.50, 9.10) | 0.790 | <0.01% | <0.001 |
| Wrist–ankle acupuncture vs. NSAIDs | 5.60 (1.30, 31.0) | 0.723 | <0.01% | <0.001 |
| Superficial acupuncture vs. NSAIDs | 5.10 (1.20, 24.0) | 0.146 | 5.90% | <0.001 |
| Moxibustion vs. NSAIDs | 7.60 (2.80, 27.0) | 0.811 | <0.01% | <0.001 |
| Electroacupuncture vs. NSAIDs | 22.0 (4.50, 120) | 0.887 | <0.01% | <0.001 |
| Ear acupuncture vs. NSAIDs | 13.0 (2.70, 130) | 0.730 | <0.01% | <0.001 |
| Abdominal acupuncture vs. NSAIDs | 5.50 (2.10, 16.0) | 0.814 | <0.01% | <0.001 |
OR: odds ratio; CI: confidence interval; NSAIDs: non-steroidal anti-inflammatory drugs.
Network meta-analysis
Table 3 shows the results of the network meta-analysis. The following types of acupuncture appeared to show more efficacy than NSAIDs in reducing the risk of primary dysmenorrhoea: traditional acupuncture (OR = 6.70, 95% CI 2.60–20.0), eye acupuncture (OR = 3.50, 95% CI 1.40–8.90), wrist–ankle acupuncture (OR = 6.00, 95% CI 1.30–32.0), superficial acupuncture (OR = 5.10, 95% CI 1.20–26.0), moxibustion (OR = 7.70, 95% CI 2.90–25.0), electroacupuncture (OR = 23.0, 95% CI 4.80–130), ear acupuncture (OR = 13.0, 95% CI 2.80–100), and abdominal acupuncture(OR = 5.30, 95% CI 2.10–16.0).
Table 3.
Network meta-analysis comparisons.
| NSAIDs | Traditional acupuncture | Eye acupuncture | Wrist–ankle acupuncture | Superficial acupuncture | Moxibustion | Electroacupuncture | Ear acupuncture | Abdominal acupuncture | |
|---|---|---|---|---|---|---|---|---|---|
| NSAIDs | 1 | 0.15 (0.05,0.40) |
0.29 (0.11,0.72) |
0.16 (0.03,0.80) |
0.19 (0.04,0.84) |
0.13 (0.04,0.36) |
0.04 (0.01,0.21) |
0.08 (0.01,0.37) |
0.19 (0.06,0.51) |
| Traditional acupuncture |
6.70
(2.60,20.0) |
1 | 2.00 (0.51,8.00) |
1.10 (0.15,7.40) |
1.30 (0.20,7.70) |
0.86 (0.19,3.60) |
0.29 (0.04,2.00) |
0.51 (0.05,3.40) |
1.30 (0.29,5.20) |
| Eye acupuncture |
3.50
(1.40,8.90) |
0.51 (0.12,2.10) |
1 | 0.57 (0.08,3.60) |
0.64 (0.11,4.00) |
0.44 (0.10,1.80) |
0.15 (0.02,0.95) |
0.26 (0.03,1.70) |
0.65 (0.15,2.60) |
| Wrist–ankle acupuncture |
6.00
(1.30,32.0) |
0.91 (0.14,6.60) |
1.70 (0.28,12.0) |
1 | 1.20 (0.13,11.0) |
0.76 (0.10,5.60) |
0.25 (0.02,2.60) |
0.45 (0.03,4.90) |
1.10 (0.16,7.40) |
| Superficial acupuncture |
5.10
(1.20,26.0) |
0.77 (0.12,5.20) |
1.50 (0.26,9.90) |
0.80 (0.09,8.10) |
1 | 0.64 (0.10,4.30) |
0.21 (0.02,2.10) |
0.38 (0.03,3.80) |
0.95 (0.15,6.10) |
| Moxibustion |
7.70
(2.90,25.0) |
1.10 (0.27,5.50) |
2.20 (0.56,10.0) |
1.30 (0.18,9.60) |
1.50 (0.24,11.0) |
1 | 0.34 (0.05,2.50) |
0.58 (0.06,4.50) |
1.50 (0.32,6.90) |
| Electroacupuncture |
23.0
(4.80,130) |
3.30 (0.48,24.0) |
6.50
(1.10,49.0) |
3.80 (0.37,41.0) |
4.10 (0.46,40.0) |
2.80 (0.39,22.0) |
1 | 1.70 (0.13,17.0) |
4.20 (0.61,30.0) |
| Ear acupuncture |
13.0
(2.80,100) |
2.00 (0.29,20.0) |
3.80 (0.57,35.0) |
2.20 (0.21,29.0) |
2.60 (0.27,35.0) |
1.60 (0.22,16.0) |
0.53 (0.05,7.20) |
1 | 2.40 (0.34,29.0) |
| Abdominal acupuncture |
5.30
(2.10,16.0) |
0.79 (0.19,3.50) |
1.60 (0.41,6.60) |
0.85 (0.13,6.20) |
1.00 (0.16,6.60) |
0.70 (0.14,3.30) |
0.23 (0.03,1.60) |
0.39 (0.04,2.90) |
1 |
NSAIDs: non-steroidal anti-inflammatory drugs. Italicized values are significant at P < 0.05.
The corresponding SUCRA values are shown in Figure 4. The corresponding rankings based on SUCRA values were as follows: traditional acupuncture (53.0%), eye acupuncture (22.0%), wrist–ankle acupuncture (81.5%), superficial acupuncture (50.0%), moxibustion (57.8%), electroacupuncture (99.9%), ear acupuncture (41.6%), and abdominal acupuncture (44.1%). The use of acupuncture, particularly electroacupuncture, was significantly associated with a decreased risk of primary dysmenorrhoea.
Figure 4.
Surface under the cumulative ranking curve (SUCRA), expressed as percentages, ranking the therapeutic effects and safety of treatments for primary dysmenorrhoea. For efficacy and safety assessment, the pharmacological agent with the highest SUCRA value is assumed to be the safest, most efficacious treatment. (A: Non-steroidal anti-inflammatory drugs [NSAIDs]; B: Traditional acupuncture; C: Eye acupuncture; D: Wrist–ankle acupuncture; E: Superficial acupuncture; F: Moxibustion; G: Electroacupuncture; H: Ear acupuncture; I: Abdominal acupuncture).
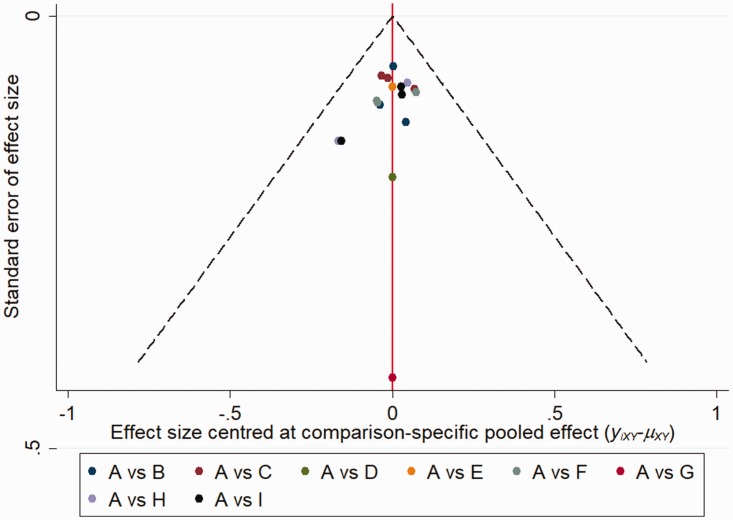
Publication bias
The comparison-adjusted funnel plots did not reveal any evidence of apparent asymmetry (Figure 5). No significant publication bias was observed.
Figure 5.
Comparison-adjusted funnel plot for the network meta-analysis. The red line suggests the null hypothesis that the study-specific effect sizes do not differ from the respective comparison-specific pooled effect estimates. Different colors represent different comparisons. (A: Non-steroidal anti-inflammatory drugs [NSAIDs]; B: Traditional acupuncture; C: Eye acupuncture; D: Wrist–ankle acupuncture; E: Superficial acupuncture; F: Moxibustion; G: Electroacupuncture; H: Ear acupuncture; I: Abdominal acupuncture).
Discussion
Ancient traditional Chinese medicine literature records that acupuncture can be used to treat dysmenorrhoea by moving the qi and blood and resolving stasis, indicating an early understanding of dysmenorrhoea.29 Clinically, traditional Chinese medicine categorizes the causes of dysmenorrhoea into five types: stagnation of qi and blood, stagnation of liver and dampness, stagnation of cold and dampness, deficiency of liver and kidney, and deficiency of qi and blood. In contrast, Western medicine considers the occurrence of primary dysmenorrhoea to be closely related to the increase of prostaglandin and interleukin.30 The main pathogenesis of dysmenorrhoea is spastic contraction of the uterine smooth muscle, manifested as increased uterine muscle tension, resulting in reduced uterine blood flow and uterine hypoxia-ischaemia.1 The increase of interleukin causes the spasmodic contraction of the smooth muscle of the uterus and results in dysmenorrhoea.30,31 Moreover, dysmenorrhoea is most severe in the first 2 days of menstruation, when the concentration of prostaglandin F2α (PGF2α) and PGF2α/PGE2 increases significantly in the endometrium.32 Acupuncture can greatly reduce PGF2α/PGE2 in dysmenorrhoea patients, effectively inhibit uterine smooth muscle spasmodic contraction, and increase uterine blood flow. This reduces local ischaemia and hypoxia and generates an analgesic effect.33
A previous meta-analysis of 42 randomized controlled trials reported an association between acupuncture and dysmenorrhoea risk, and found that acupuncture was effective in treating primary dysmenorrhoea.5 Furthermore, Yang et al. found that acupuncture therapy is more efficacious than NSAIDs in reducing the risk of primary dysmenorrhoea.10 However, no previous studies have examined whether all acupuncture therapy methods are efficacious in treating primary dysmenorrhoea, or have clarified which type of acupuncture therapy shows most efficacy in primary dysmenorrhoea treatment.
In this network meta-analysis, we compared the efficacy of acupuncture therapies for primary dysmenorrhoea and examined which acupuncture therapy showed most efficacy for primary dysmenorrhoea compared with NSAIDs. The results suggest that traditional acupuncture, eye acupuncture, wrist–ankle acupuncture, superficial acupuncture, moxibustion, electroacupuncture, ear acupuncture, and abdominal acupuncture are more efficacious than NSAIDs in reducing the risk of primary dysmenorrhoea, and that the use of acupuncture, particularly electroacupuncture, is significantly associated with a decreased risk of primary dysmenorrhoea. The SUCRA ranking scheme ranked wrist–ankle acupuncture lower than electroacupuncture. The use of clinical syndromes to diagnose patients means that traditional Chinese medicine can tailor the prescription to the patient, and a good curative effect is often obtained.
Acupuncture is simple, efficient, and safe, and plays an important role in the treatment of primary dysmenorrhoea. Electroacupuncture is one of the most widely used acupuncture methods in clinical practice. Endogenous opioid receptors mediate the analgesic effects of electroacupuncture.34 In one study, electroacupuncture was used to stimulate the acupuncture point SP6, which resulted in an increase of beta-endorphins in the rat uterus and consequent analgesia.34 Hypoimmunity is a typical manifestation of primary dysmenorrhoea.35 Electroacupuncture can lead to the release of interleukin-1 and interleukin-6 and increase the activity of natural killer cells in rats with primary dysmenorrhoea.36 Additionally, electroacupuncture can effectively improve blood flow in the uterus of patients with dysmenorrhoea, reducing local ischaemia and hypoxia.37
This meta-analysis had some limitations. The statistical tests used to examine heterogeneity in the randomized controlled trials lacked power, and there was limited evidence of a dose-dependent association between acupuncture therapy and dysmenorrhoea; therefore, we can have only limited confidence in the study findings. Second, standardized treatment methods were not used across the trials. The difference between trials means that the results should be interpreted with caution. Third, the study durations were short and the participants may not be representative of the general population. Fourth, these findings may not be generalizable to other groups of patients, as randomized controlled trials tend to exclude some participants. Fifth, the overall study sample sizes were small, and the overall quality of acupuncture and moxibustion treatment was not high, which may have affected the evaluation results.
Our findings indicate that acupuncture is more efficacious than NSAIDs in reducing the risk of primary dysmenorrhoea. The use of acupuncture, particularly electroacupuncture, seems to be strongly associated with a decreased risk of primary dysmenorrhoea. Future research requires large-scale and ongoing trials to validate the effect identified in this meta-analysis.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Dawood MY. Dysmenorrhea. Clin Obstet Gynecol 1983; 26: 719–727. [PubMed] [Google Scholar]
- 2.Ylikorkala O, Dawood MY. New concepts in dysmenorrhea. Am J Obstet Gynecol 1978; 130: 833–847. [DOI] [PubMed] [Google Scholar]
- 3.Harel Z. Dysmenorrhea in adolescents and young adults: from pathophysiology to pharmacological treatments and management strategies. Expert Opin Pharmacother 2008; 9: 2661–2672. [DOI] [PubMed] [Google Scholar]
- 4.Zhu X, Proctor M, Bensoussan A, et al. Chinese herbal medicine for primary dysmenorrhoea. Cochrane Database Syst Rev 2008: 2: CD005288. [DOI] [PubMed] [Google Scholar]
- 5.Smith CA, Armour M, Zhu X, et al. Acupuncture for dysmenorrhoea. Cochrane Database Syst Rev 2016; 4: CD007854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dawood MY. Nonsteroidal anti-inflammatory drugs and changing attitudes toward dysmenorrhea. Am J Med 1988; 84: 23–29. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan O, Naziroglu M, Guney M, et al. Non-steroidal anti-inflammatory drug modulates oxidative stress and calcium ion levels in the neutrophils of patients with primary dysmenorrhea. J Reprod Immunol 2013; 100: 87–92. [DOI] [PubMed] [Google Scholar]
- 8.Marjoribanks J, Proctor M, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev 2010: 7: CD001751. [DOI] [PubMed] [Google Scholar]
- 9.Yang H, Liu CZ, Chen X, et al. Systematic review of clinical trials of acupuncture-related therapies for primary dysmenorrhea. Acta Obstet Gynecol Scand 2008; 87: 1114–1122. [DOI] [PubMed] [Google Scholar]
- 10.Xu Y, Zhao W, Li T, et al. Effects of acupoint-stimulation for the treatment of primary dysmenorrhoea compared with NSAIDs: a systematic review and meta-analysis of 19 RCTs. BMC Complement Altern Med 2017; 17: 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu YL, Lin Q, Li Y, et al. Effect of eye acupuncture on plasma PGF 2α in patients of primary dysmenorrhea. World J Acupuncture-Moxibustion 2012; 22: 17–22. [Google Scholar]
- 13.Zhang LM, Yang HY. The 45 cases on single acupuncture treatment for primary dysmenorrhea. Fujian J TCM 2012; 43: 25–26. [Google Scholar]
- 14.Lin Q, Chen WZ, Li Y, et al. Effect of eye acupuncture on uterine artery blood flow in patients with primary dysmenorrhea. Shanghai J Acupunct Moxibustion 2012; 31: 885–887. [Google Scholar]
- 15.Cao Y. Acupuncture clinical analysis of primary dysmenorrhea. Heilongjiang Chin Med College 2011: 3: 26–29. [Google Scholar]
- 16.Zhi LX. Randomized controlled study on superficial needling for treatment of primary dysmenorrhea. Zhongguo Zhen Jiu 2007; 27: 18–21. [PubMed] [Google Scholar]
- 17.Ren XL. Clinical study on the treatment of primary dysmenorrhea with moxibustion. Global Traditional Chin Med 2013; 6: 431–432. [Google Scholar]
- 18.Zhu Y, Chen RL, Le JI, et al. Efficacy observation of primary dysmenorrhea treated with isolated-herbal moxibustion on Shenque (CV8). Zhongguo Zhen Jiu 2010; 30: 453–455. [PubMed] [Google Scholar]
- 19.Li JM. Clinical study of electro—acupuncture treatment of primary dysmenorrhea Ci Liao acupoints. Guangzhou Chin Med College 2012; 6: 18–21. [Google Scholar]
- 20.Wang K, Pan WY, Duan YH. Clinical study on the treatment of primary dysmenorrhea with auricular acupuncture. Guangdong Med J 2005; 26: 1728–1730. [Google Scholar]
- 21.Yang M. The clinical observation of 36 cases on dysmenorrhea moxibustion treatment of primary dysmenorrhea. Hainan Med J 2009; 20: 226–227. [Google Scholar]
- 22.Chen LW. The clinical observation of primary dysmenorrhea treated with the Chinese native medicine sticks on the acupuncture point. Guangzhou Chin Med College 2006: 6: 20–22. [Google Scholar]
- 23.Liu C, Zhang HY. Therapeutic effect of moxibustion on primary dysmenorrhea due to damp-cold retention. World J Acupuncture-Moxibustion 2011; 21: 1–4. [Google Scholar]
- 24.Zhu C. Clinical study on the treatment of haemorrheological nature blood stasis type of primary dysmenorrhea with moxibustion. Hubei J TCM 2011; 33: 65–66. [Google Scholar]
- 25.Li ZL, Li YQ, Pan FQ, et al. Clinical observation on Chinese herbs acupoint of Yugui wenjing decoction stick to treat haemorrheological nature blood stasis type of primary dysmenorrhea. Modern J Integrated Traditional Chinese Western Med 2012; 21: 483–484. [Google Scholar]
- 26.Jiang LY. Clinical experience of acupuncture for treatment of 34 cases in primary dysmenorrhea. J Emerg Tradit Chin Med 2007; 16: 620–621. [Google Scholar]
- 27.Xing QX. Observation on the therapeutic effect of pricking bloodletting at ear points on primary dysmenorrhea. Shanghai Zhenjiu Zazhi 2011; 30: 235–236. [Google Scholar]
- 28.Ji L, Chen RL, Deng PY, et al. Treatment effect of herb-partitioned moxibustion for dysmenorrhea of cold stagnation type and its effect on PGF2α and PGE2. Shanghai J Acupunct Moxibustion 2012; 31: 882–884. [Google Scholar]
- 29.Zhang YZ. Chinese gynecology. Beijing: China Traditional Chinese Medicine Press, 2002, p.131. [Google Scholar]
- 30.Harel Z. Dysmenorrhea in adolescents and young adults: from pathophysiology to pharmacological treatments and management strategies. Expert Opin Pharmacother 2008; 9: 2661–2672. [DOI] [PubMed] [Google Scholar]
- 31.Abu JI, Konje JC. Leukotrienes in gynaecology: the hypothetical value of anti-leukotriene therapy in dysmenorrhoea and endometriosis. Hum Reprod Update 2000; 6: 200–205. [DOI] [PubMed] [Google Scholar]
- 32.Dingfelder JR. Primary dysmenorrhea treatment with prostaglandin inhibitors: a review. Am J Obstet Gyecol 1981; 140: 874–879. [DOI] [PubMed] [Google Scholar]
- 33.Xu T, Hui L, Juan YL, et al. Effects of moxibustion or acupoint therapy for the treatment of primary dysmenorrhea: a meta-analysis. Altern Ther Health Med 2014; 20: 33–42. [PubMed] [Google Scholar]
- 34.Miao EY, Miao MY, Kildea DG, et al. Effects of electroacupuncture and electroacupuncture plus Tao Hong Si Wu Wan in treating primary dysmenorrhea. J Acupunct Meridian Stud 2014; 7: 6–14. [DOI] [PubMed] [Google Scholar]
- 35.Ma YX, Ma LX, Liu XL, et al. A comparative study on the immediate effects of electroacupuncture at Sanyinjiao (SP6), Xuanzhong (GB39) and a non-meridian point, on menstrual pain and uterine arterial blood flow, in primary dysmenorrhea patients Pain Med. 2010; 11: 1564–1575. [DOI] [PubMed] [Google Scholar]
- 36.Li CH, Ren XX, Guo MW, et al. Effect of electroacupuncture at different acupoints on plasma TXB2 and 6-keto-PGF(1alpha), contents in dysmenorrhea rats Zhen Ci Yan Jiu. 2011; 36: 347–352. [PubMed] [Google Scholar]
- 37.Li CH, Zhao YF, Ji B, et al. Effect of electroacupuncture on the uterine microcirculation in dysmenorrhea rats. Zhen Ci Yan Jiu 2011; 36: 12–17. [PubMed] [Google Scholar]