Abstract
Background:
Obvious functional deterioration is demonstrated in elderly people aged 75 years and older. However, there is only little objective evidence relating to falls in these individuals.
Objective:
This cross-sectional study compared functional abilities and health status in the elderly age at least 75 years with no fall, single fall (1 fall), and multiple falls (≥2 falls) during the past 6 months. Furthermore, the study describes fall information of the participants.
Methods:
Ninety participants (30 individuals/group) were interviewed for their health status and fall history within the past 6 months. Then they were objectively assessed in terms of their functional ability to conduct daily activities independently.
Results:
The findings indicated that the functional abilities of participants with multiple falls were significantly poorer, with the number of those requiring a walking device significantly greater than that in the other groups. These individuals reported loss of balance as a major factor for falls, whereas individuals with a single fall reported an environmental hazard as a common cause of falls.
Conclusion:
Although the cross-sectional findings may be unable to clearly confirm the causal relationship of the outcomes, the data support the influence of intrinsic impairments and can be used to promote functional ability and minimise fall risk in these individuals.
Keywords: balance, endurance, fall, functional test, older adult
Introduction
Approximately 30% of elderly people experience a fall in a year, and each fall can cause physical and psychological consequences that subsequently reduce quality of life such as fracture and decreased self-confidence and ability to conduct productive activities [1–4]. It is a complex causal event that relates to both intrinsic and extrinsic factors in which a single fall mostly involves extrinsic factors, whereas multiple falls are likely to be related to intrinsic impairments [5–8]. Thus having multiple falls is more clinically important, particularly with advancing age [5–7]. However, these findings were derived from subjective data or some aspects of functional ability in early age elderly. Although advancing age introduces changes in age-related functional decline of many body systems, the obvious functional deterioration is demonstrated in those aged at least 75 years [9]. Therefore, investigation of data relating to falls in these individuals is important to minimise the number of dependent persons, particularly in current times as the number of elderly and their life expectancy have dramatically increased.
Important contributors to an independent lifestyle for the elderly include safe and efficient ambulatory status, good static and dynamic balance, adequate lower extremity muscle strength (LEMS), and good functional endurance [10,11]. These abilities can be quantified using the 10-Meter Walk Test (10MWT), Timed Up and Go Test (TUG), Five Times Sit-to-Stand Test (FTSST), and 6-Minute Walk Test (6MWT) [11,12]. These tests are valid, reliable, and feasible in assessment of the functional ability of the elderly in both clinics and communities [11–14]. In addition, the findings of these tests can be used to direct the process of decision-making to improve the effectiveness of rehabilitation strategies for these individuals [11,12]. Therefore, this study primarily compared functional abilities and health status in the elderly, aged at least 75 years, with a history of having had no fall, a single fall (1 fall), and multiple falls (≥2 falls) during the 6 months prior to taking part in this study. The study also secondarily investigated fall information of individuals who fell.
Materials and methods
Study design and population
The data were cross-sectional, and were collected from several rural communities in Thailand. The sample size was calculated using a formula for data comparison of a major outcome (10MWT) [15,16]. When the power of test was set at 0.8 with an α level at 0.05 and effect size of 0.24 (data from a pilot study using 10 individuals/group), the study required 30 individuals/group or 90 participants in total. The elderly individuals were recruited if they were at least 75 years old with a body mass index (BMI) between 18.5 and 29.9 kg/m2. In addition, they needed to have intact cognitive functions [Mini-Mental State Examination (Thai version 2002) ≥ 22 points based on education level [17], good communication, and the ability to understand simple commands for the tests. The exclusion criteria were having (1) pain (at rest and with movement) in the musculoskeletal system of more than 5 out of 10 on a visual analogue scale; (2) sequelae of neuromuscular diseases (e.g., Parkinson’s disease and stroke) that affected balance and walking abilities; (3) other signs and symptoms that might influence the tests used in this study such as dizziness, acute illness or injury, unstable heart diseases (e.g., angina) and uncontrolled hypertension. The protocol of the study was approved by the local ethics committee (HE542091), and eligible individuals signed a written informed consent prior to their participation in the study.
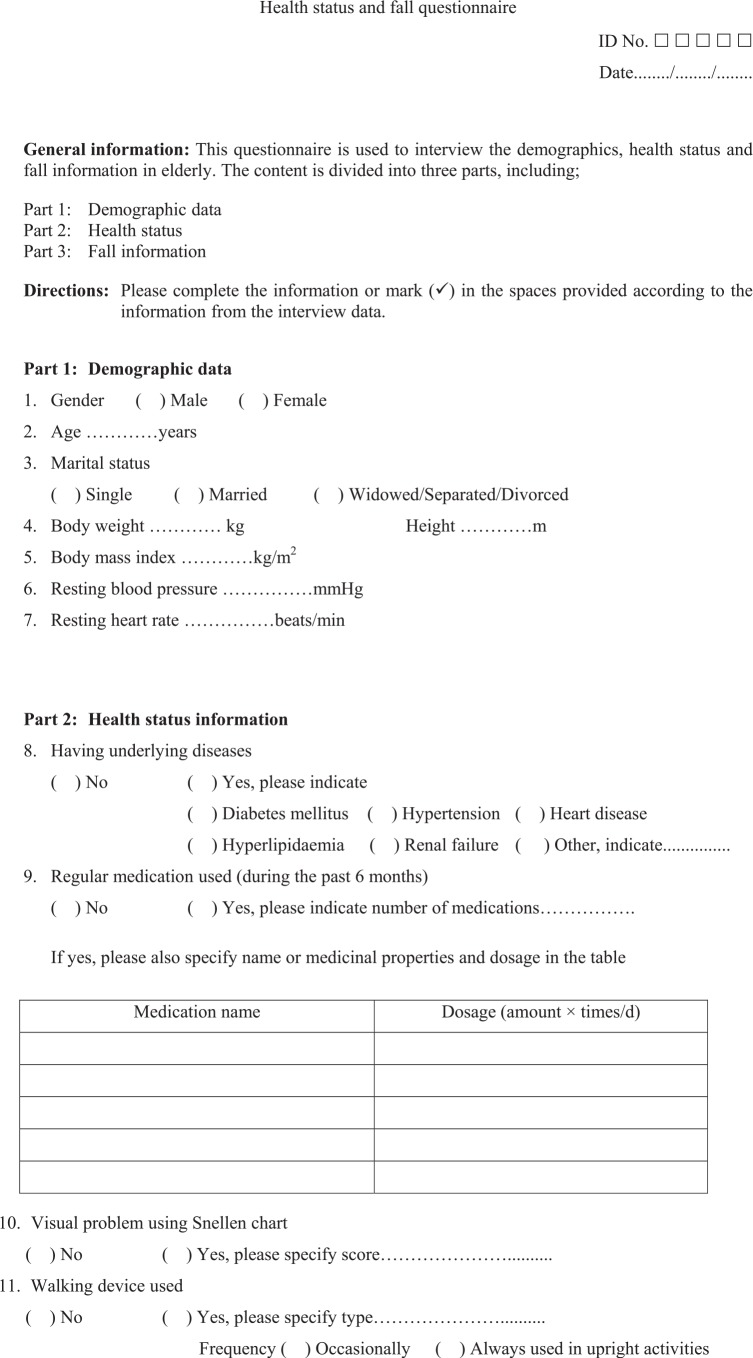
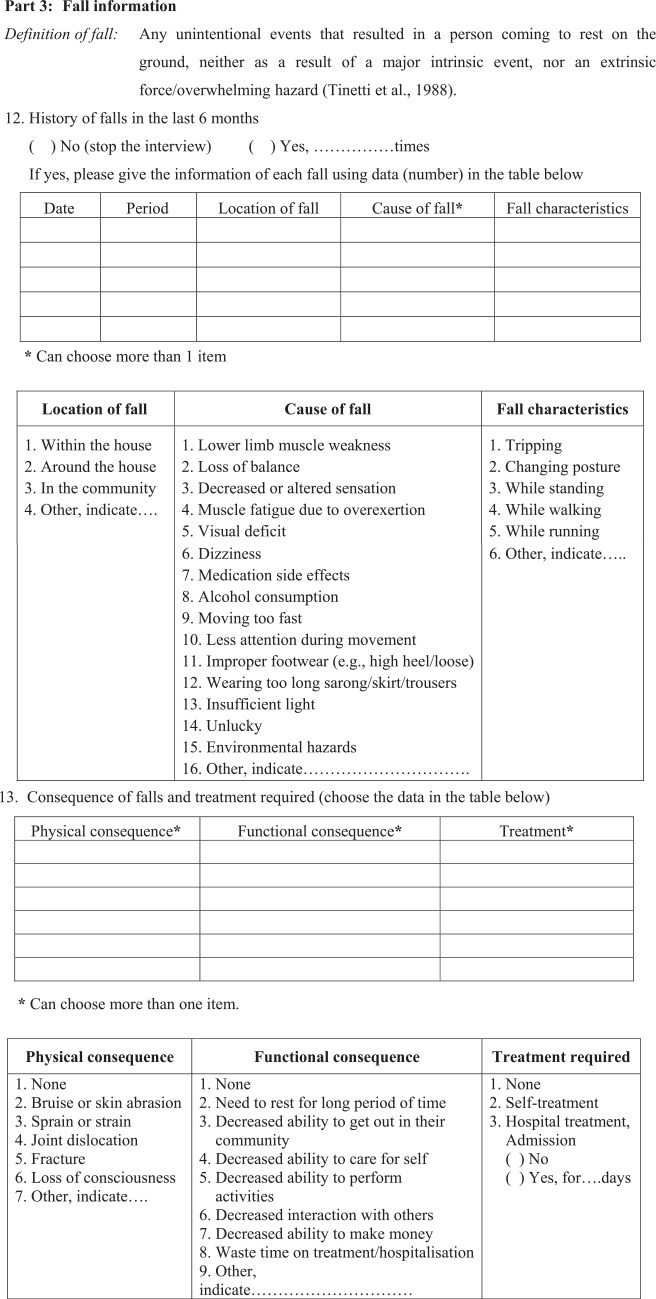
Questionnaire development
This study used a questionnaire to interview for baseline data, health status and fall information (please see Appendix 1). It was developed based on consolidation of data from previous studies [5,8,18,19]. Thereafter, it was verified for the content validity through the method of expert panel discussion using four rehabilitation professionals (3 physical therapists and a nurse) who had good clinical experience with the elderly population. Next, it was preliminarily used in 15 elderly people. Then, some items were modified, rearranged, or deleted in order to improve the conciseness, clarity, and completeness of the questionnaire. After all revisions have been made, the questionnaire was divided into three parts: (1) demographic information, (2) health status information, and (3) fall information (Appendix 1). The interview process took approximately 15–20 min/participant.
Study protocols
The eligible individuals were interviewed for their demographics, health status, and their history of falls within the past 6 months using a questionnaire (Appendix 1). The findings were used to classify the participants into three groups including nonfaller, single-faller (1 fall), and multiple-faller (≥2 falls) groups. A fall in this study was defined as any unintentional events that resulted in a person coming to rest on the ground, neither as a result of a major intrinsic event such as stroke or syncope, nor an extrinsic force/overwhelming hazard such as forcefully being pushed down or having a road traffic accident [20].
After sufficient rest, participants were assessed for their level of ability including ambulatory status, static and dynamic balance, LEMS, and functional endurance using four functional tests, including the 10MWT, TUG, FTSST, and 6MWT, in random order. The examiners were blinded to the participants’ history of falls, and had sufficient discussion and practice with the methods of measurements to minimise errors of the findings. The procedures used for the tests were as follows.
10MWT
The 10MWT measured ambulatory status in terms of walking speed [11]. This test was performed using a flying start in which participants walked at a comfortable pace along a 10-m walkway, and the time was recorded during the middle 3 m of the walkway [13,21]. Then, the average finding of the two trials was converted to walking speed in meters/second (m/s).
TUG test
The TUG test was widely used to measure balance ability while changing posture and walking [11,13,22]. This test recorded the time required to complete the tasks of standing up from a chair (without using arms), walking around a traffic cone that was placed 3 m from the chair, and returning to sit down at a maximum and safe speed. The average findings of two trials were recorded in seconds [11,22].
FTSST
The FTSST reflected functional LEMS during changing from sitting to standing postures [23]. The test recorded the time required to complete five chair-rise cycles at a maximum and safe speed without using the arms. Then the average findings of the two trials were recorded in seconds.
6MWT
The 6MWT evaluated functional endurance using the longest distance walked in 6 minutes [24]. The test was performed along a square walkway marked in 1-m intervals with an orange traffic cone placed at each corner. During the test, an examiner walked alongside the participant to ensure safety and inform the participant about the time left every minute. Participants were able to take a period of rest as needed during the test without losing time. Then the total distance covered after 6 minutes was recorded in meters [21].
During the tests, an examiner walked alongside or was beside the participant without interruption in order to ensure the participant’s safety and improve the accuracy of the outcomes. The participants wore the proper size of sandal sport shoes that were prepared by the researchers, and were given a practice session so they could familiarise themselves with the shoes. They were able to take a period of rest during participation in the study as needed.
Statistical analysis
Descriptive statistics were applied to explain baseline characteristics, health status, and fall information of the participants. The findings among the three groups (nonfaller, single-faller, and multiple-faller) were compared using one-way analysis of variance for continuous variables and chi-square test for categorical variables. Then, the post hoc (Scheffe) test was used to identify the differences in the continuous data for each pairwise condition. All data were analysed using the SPSS software (SPSS Statistic 17.0, IBM Corporation, Armonk, NY, USA; serial number: 5068054) with the level of statistical significance at less than 0.05.
Results
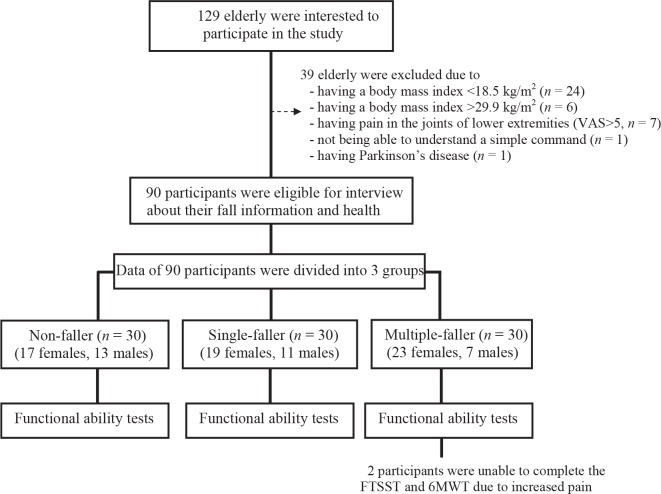
One hundred and twenty-nine elderly agreed to participate in the study; however, 39 of them were excluded for reasons shown in Figure 1. Therefore, 90 participants were involved in the study (30 individuals/group; Figure 1). Most participants in each group were women, and fallers were slightly older than their nonfaller counterparts (Table 1). In addition, the number of multiple-fallers (range 2–4 falls) who required a walking device was significantly greater than those in the other groups (p < 0.001, Table 1). Two individuals in this group were unable to complete the FTSST and 6MWT because of increased pain in the lower extremities. The 10MWT, TUG, and FTSST of these individuals were significantly poorer than those in the other groups (p < 0.001, Table 2). For the 6MWT, fallers could cover a distance significantly shorter than nonfallers (p < 0.001, Table 2).
Figure 1.
Participation flowchart of study participants.
Table 1.
Demographics and health status of the participants.
| Variable | Group (30 individuals/group) | p | |||
|---|---|---|---|---|---|
| Non-faller | Single-faller | Multiple-faller | |||
| Agea (y) | 77.6±2.2 (76.8–78.4) | 79.1±4.1 (77.6–80.9) | 79.5±4.2 (78.0–81.1) | 0.099 | |
| Body mass indexa (kg/m2) | 21.2±2.4 (20.3–22.1) | 22.2±2.6 (21.2–23.2) | 21.4±2.5 (20.5–22.4) | 0.281 | |
| Sexb, c: female, n (%) | 17 (56.7) | 19 (63.3) | 23 (76.7) | 0.252 | |
| Underlying diseases,b n (%) | None | 16 (53.4) | 21 (70.1) | 10 (33.3) | 0.223 |
| Diabetes mellitus | 3 (10.0) | 4 (13.3) | 8 (26.7) | ||
| Hypertension | 6 (20.0) | 4 (13.3) | 8 (26.7) | ||
| Hyperlipidaemia | 3 (10.0) | — | 3 (10.0) | ||
| Renal failure | 1 (3.3) | 1 (3.3) | 1 (3.3) | ||
| Heart disease | 1 (3.3) | — | — | ||
| Number of medications,b n (%) | 0 | 19 (63.3) | 21 (70.0) | 19 (63.3) | 0.429 |
| 1 | 8 (26.7) | 7 (23.3) | 4 (13.3) | ||
| 2–3 | 3 (10.0) | 2 (6.7) | 6 (20.0) | ||
| ≥4 | — | — | 1 (3.3) | ||
| Visual problems,d n (%) | 27 (90.0) | 29 (96.7) | 30 (100.0) | 0.160 | |
| Device usedc: Yes, n (%) | — | 2 (6.7) | 12 (40.0) | <0.001* | |
Indicates significant difference.
Data are presented using mean±standard deviation (95% confidence intervals) and the comparisons among the groups were executed using the one-way analysis of variance.
These variables were categorised as follows: sex: female/male, device used: yes/no.
The comparisons among the groups were performed using the chi-square test.
The Snellen chart 6/6 vision was applied.
Table 2.
Functional abilities of the participants.
| Variable | Group (30 individuals/group) | pa | ||
|---|---|---|---|---|
| Non-faller | Single-faller | Multiple-faller | ||
| 10MWT (m/s) | 1.1 | 1.0 | 0.8N,S | <0.001 |
| 1.1–1.2 | 1.0–1.1 | 0.8–0.9 | ||
| TUG (s) | 10.4 | 11.8 | 13.5N,S | <0.001 |
| 9.9–10.9 | 10.8–12.8 | 12.2–14.8 | ||
| FTSSTb (s) | 12.7 | 14.1 | 16.6N,S | <0.001 |
| 12.1–13.3 | 13.2–15.0 | 14.8–18.3 | ||
| 6MWTb (m) | 356.0 | 298.6N | 264.8N | <0.001 |
| 338.5–373.5 | 262.3–327.8 | 231.5–298.0 | ||
Data are presented using mean and 95% confidence intervals.
6MWT = 6-Minute Walk Test (meters); 10MWT = 10-Meter Walk Test (meters/second); FTSST = Five Times Sit-to-Stand (seconds); TUG = Timed Up & Go Test (seconds).
p value from the one-way analysis of variance and every pairwise comparison were further analysed using the post hoc (Scheffe) analysis. Superscripts indicate the group(s) with significant differences from the indicated groups, where N = Non-faller; S = Single-faller.
Only 28 multiple-faller individuals could complete the FTSST and 6MWT.
Most falls occurred while they were walking in a community, particularly during rainy season (Table 3). Multiple-fallers indicated loss of balance as a major cause of falls, whereas an environmental hazard was an important cause of a single fall. After falls, most multiple-fallers experienced physical consequences, in which two of them had wrist fractures. Nearly half of all falls also induced functional consequences and required medical attention (Table 3).
Table 3.
Fall information of participants who fell in the last 6 months.
| Fall dataa | Group (30 individuals/group) | p* | |
|---|---|---|---|
| Single-faller, n (%) | Multiple-fallerb, n (%) | ||
| Period of fall | |||
| Rainy season | 17 (56.7) | 40 (51.9) | 0.843 |
| Summer | 8 (26.7) | 25 (32.5) | |
| Winter | 5 (16.7) | 12 (15.6) | |
| Location of fall | |||
| In the community | 18 (60.0) | 32 (41.6) | 0.129 |
| Around the house | 7 (23.3) | 34 (44.2) | |
| Within the house | 5 (16.7) | 11 (14.3) | |
| Causes of fall as perceived by the participants | |||
| Environmental hazard | 15 (37.5) | 21 (18.4) | 0.001 |
| Loss of balance | 4 (10.0) | 41 (36.0) | |
| Less attention during movement | 13 (32.5) | 20 (17.5) | |
| Dizziness | 3 (7.5) | 16 (14.0) | |
| Lower limb muscle weakness | 2 (5.0) | 14 (12.3) | |
| Moving too fast | 3 (7.5) | 2 (1.8) | |
| Fall behaviour | |||
| While walking | 21 (70.0) | 48 (62.3) | 0.789 |
| Changing posture | 6 (20.0) | 17 (22.1) | |
| Tripping | 2 (6.7) | 10 (13.0) | |
| While running | 1 (3.3) | 2 (2.6) | |
| Consequences of fall | |||
| Physical consequences | |||
| None | 16 (50.0) | 23 (28.0) | 0.115 |
| Bruise or skin abrasion | 11 (34.4) | 40 (48.8) | |
| Sprain | 3 (9.4) | 17 (20.7) | |
| Fracture | 2 (6.3) | 2 (2.4) | |
| Functional consequences | |||
| None | 23 (65.7) | 53 (53.5) | 0.626 |
| Need to rest for a long period | 4 (11.4) | 16 (16.2) | |
| Decreased ability to get out in their community | 3 (8.6) | 11 (11.1) | |
| Decreased ability to care for self | 3 (8.6) | 5 (5.1) | |
| Decreased ability to perform their activities | 2 (5.7) | 12 (12.1) | |
| Decreased ability to make money | — | 2 (2.0) | |
| Treatment | |||
| None | 26 (74.3) | 39 (44.8) | 0.005 |
| Self-treatment (such as taking medication, cold packs) | 3 (8.6) | 30 (34.4) | |
| Hospital treatment (both hospitalisation and medical treatments) | 6 (17.1) | 18 (20.7) | |
p value from the chi-square test.
n = number of situations.
The data were subjectively reported by the participants.
The number of falls ranged from 2 to 4 times/individual—thus, the total number of falls was 77 and the data are reported as the number of falls (percentage of total falls).
Discussion
This study compared functional abilities necessary for daily activities and health status among participants aged 75 years and older. They were classified into three groups according to history of fall: no fall, single fall, and multiple falls. The results revealed no significant differences among the groups in terms of baseline data, except for the walking device used. The number of multiple-fallers who required a walking device was significantly greater (p < 0.001, Table 1), and they had significantly poorer functional ability than those in the other groups (p < 0.001, Table 2). For the 6MWT, the data indicated that individuals with falls, both single and multiple falls, had significantly poorer functional endurance than those without falls (p < 0.001, Table 2).
Although the rainy season leads to slippery floors that introduce environmental hazards and risk of falls in the elderly, the data on functional tests indicates significantly greater deficits among multiple-faller individuals when compared to individuals in the other groups (Table 2). In addition, nearly half of these individuals required a walking device for daily walking (Table 1). In general, a walking device is prescribed to promote walking ability, balance control, and level of independence of the elderly [25,26]. Although a cross-sectional study cannot indicate the causal relationship for the given data, the findings may confirm the important consequences of intrinsic impairments on the risk of multiple falls in the participants.
Data in functional tests support this assumption. The findings indicate that multiple-fallers had significantly poorer functional ability, as measured using the 10MWT, TUG, and FTSST, than those in the other groups (p < 0.001, Table 2). Many studies have reported that outcomes of the 10MWT, TUG, and FTSST reflect ambulatory status, balance control, and lower extremity motor strength Table 2). In general, the 6MWT is used to evaluate the global and integrated responses of the systems involved in the activity including the pulmonary and cardiovascular systems, systemic circulation, neuromuscular units, and muscle metabolism [30]. Thus, the results of the test reflect the overall functional tolerance in daily activities, and the test has been recommended as a good indicator of habitual walking [30,31]. Hausdorff and colleagues [32] found that, while performing the 6MWT, faller elderly showed significantly greater gait variability than nonfaller elderly, from which gait unsteadiness or variability is an important predictor to increase risk of falls in the elderly. Thus, these findings may explain the significant differences in the 6MWT data of participants with and without falls during the 6 months prior to participation in this study.
After falls, most of the individuals with multiple falls also encountered physical consequences, and two of them had wrist fractures that subsequently required medical attention and resulted to limited ability to perform productive activities (Table 3). The findings were consistent with data from a previous study that reported that multiple-faller elderly also needed extra medical attention because they generally had a worse health status and more internal deterioration than those with a single fall [8].
The findings of the current study confirm the contribution of intrinsic impairments, and direct the process of decision-making to promote functional ability and reduce risk of multiple falls in elderly aged 75 years and older. However, there are several noteworthy limitations of the study. First, this study did not aim to explore the incidence of falls of the participants but applied the data from other studies [33,34]. A further study that explores this information specifically for the community-dwelling elderly from a developing country would provide an important database for further management. Second, apart from functional ability, there are other factors necessary for the ability to lead an independent lifestyle such as personal, social, and environmental factors. In addition, balance and walking ability can possibly be affected by BMI, so the study included individuals with a BMI between 18.5 and 29.9 kg/m2 in order to minimise these confounding factors on the outcomes. However, this may limit the generalisability of the findings. Third, the participants needed to complete the four functional tests, so their average age was younger than 80 years, which may not truly represent the late-age elderly. Third, the fall information was gathered retrospectively, which might increase the chance of recall bias, particularly in the older elderly. However, Mackenzie and colleagues [35] reported that the accuracy of fall recall was as high as 84%. In addition, the researchers recruited only individuals with intact cognitive functions (based on Mini-Mental State Examination scores) in order to minimise errors of the findings. Moreover, the cross-sectional data collection in this study cannot indicate the causal relationship of the findings. A further prospective study with a larger number of participants and consideration of other factors influencing the ability to lead an independent lifestyle using multiple regression analysis may thoroughly confirm the factors associated with multiple falls in these individuals.
Acknowledgements
The researchers thank Mr Ian Thomas for his help with manuscript preparation.
Appendix
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding/support: This research was supported by the Faculty of Associated Medical Sciences (02-56), and the Improvement of Physical Performance and Quality of Life (IPQ) Research Group, Khon Kaen University, Khon Kaen, Thailand.
References
- [1]. Chu LW, Chi I, Chiu AY, . Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore 2005;34:60–72. [PubMed] [Google Scholar]
- [2]. Moylan KC, Binder EF. Falls in older adults: risk assessment, management and prevention. Am J Med 2007;120:493–497. [DOI] [PubMed] [Google Scholar]
- [3]. Resnick B, Junlapeeya P. Falls in a community of older adults: findings and implications for practice. Appl Nurs Res 2004;17:81–91. [DOI] [PubMed] [Google Scholar]
- [4]. Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther 2009;89:324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Toraman A, Yildirim NU. The falling risk and physical fitness in older people. Arch Gerontol Geriatr 2010;51:222–226. [DOI] [PubMed] [Google Scholar]
- [6]. Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. J Am Med Assoc 1989;261:2663–2668. [PubMed] [Google Scholar]
- [7]. Nickens H. Intrinsic factors in falling among the elderly. Arch Intern Med 1985;145:1089–1093. [PubMed] [Google Scholar]
- [8]. Tromp AM, Pluijm S.M.F, Smit JH, Deeg D.J.H, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 2001;54:837–844. [DOI] [PubMed] [Google Scholar]
- [9]. Hebert R, Brayne C, Spiegelhalter D. Incidence of functional decline and improvement in a community-dwelling, very elderly population. Am J Epidemiol 1997;145:935–944. [DOI] [PubMed] [Google Scholar]
- [10]. El Haber N, Erbas B, Hill KD, Wark JD. Relationship between age and measures of balance, strength and gait: linear and non-linear analyses. Clin Sci 2008;114:719–727. [DOI] [PubMed] [Google Scholar]
- [11]. Lusardi MM, Pellecchia GL, Schulman M. Functional performance in community living older adults. J Geriatr Phys Ther 2003; 2614–2622. [Google Scholar]
- [12]. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther 2002;82:128–137. [DOI] [PubMed] [Google Scholar]
- [13]. Langley FA, Mackintosh S. Functional balance assessment of older community dwelling adults: a systematic review of literature. Internet J Allied Health Sci Pract 2007;5:1–11. [Google Scholar]
- [14]. Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing 2008;37:430–435. [DOI] [PubMed] [Google Scholar]
- [15]. Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc 2007;55:1727–1734. [DOI] [PubMed] [Google Scholar]
- [16]. Chirawatkul A. Statistics for health science research. 2nd ed. Bangkok: Witthayaphat Company; 2010. [Google Scholar]
- [17]. Institute of Geriatric Medicine. Department of Medical Services, Ministry of Public Health. Bangkok, Thailand: Mini-Mental State Examination—Thai 2002; 2002. Author. [Google Scholar]
- [18]. Phonthee S, Saengsuwan J, Siritaratiwat W, Amatachaya S. Incidence and factors associated with falls in independent ambulatory individuals with spinal cord injury: a 6-month prospective study. Phys Ther 2013;93:1061–1072. [DOI] [PubMed] [Google Scholar]
- [19]. Wannapakhe J, Arrayawichanon P, Saengsuwan J, Amatachaya S. Medical complications and falls in patients with spinal cord injury during the immediate phase after completing a rehabilitation program. J Spinal Cord Med 2013: 11 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New Engl J Med 1988;319:1701–1707. [DOI] [PubMed] [Google Scholar]
- [21]. Amatachaya S, Thaweewannakij T, Srisim K, Wongsa S, Phiwjinda K, Mato L, et al. . Sufficient activity is important for mobility of well-functioning elderly. Chula Med J 2011;55:221–231. [Google Scholar]
- [22]. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000;80:896–903. [PubMed] [Google Scholar]
- [23]. Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills 1995;80:163–166. [DOI] [PubMed] [Google Scholar]
- [24]. Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil 1999;80:837–841. [DOI] [PubMed] [Google Scholar]
- [25]. Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil 2005;86:134–145. [DOI] [PubMed] [Google Scholar]
- [26]. Bradley SM, Hernandez CR. Geriatric assistive devices. Am Fam Phys 2011;84:405–411. [PubMed] [Google Scholar]
- [27]. Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. . Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc 2005;53:1675–1680. [DOI] [PubMed] [Google Scholar]
- [28]. Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. . Identifying a cut-off point for normal mobility: a comparison of the timed ’up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing 2003;32:315–320. [DOI] [PubMed] [Google Scholar]
- [29]. Etnyre B, Thomas DQ. Event standardization of sit-to-stand movements. Phys Ther 2007;87:1651–1666. [DOI] [PubMed] [Google Scholar]
- [30].American Thoracic Society. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–117. [DOI] [PubMed] [Google Scholar]
- [31]. Gijbels D, Alders G, Van Hoof E, Charlier C, Roelants M, Broekmans T. Predicting habitual walking performance in multiple sclerosis: relevance of capacity and self-report measures. Multiple Scler J 2010;16:618–626. [DOI] [PubMed] [Google Scholar]
- [32]. Hausdorff JM, Edelberg HK, Mitchell SL, Goldberger AL, Wei JY. Increased gait unsteadiness in community-dwelling elderly fallers. Arch Phys Med Rehabil 1997;78:278–283. [DOI] [PubMed] [Google Scholar]
- [33]. Assantachai P, Praditsuwan R, Chatthanawaree W, Pisalsarakij D, Thamlikitkul V. Risk factors for falls in the Thai elderly in an urban community. J Med Assoc Thai 2003;86:124–130. [PubMed] [Google Scholar]
- [34]. Jitapunkul S, Songkhla MN, Chayovan N, Chirawatkul A, Choprapawon C, Kachondham Y, et al. . Falls and their associated factors: a national survey of the Thai elderly. J Med Assoc Thai 1998;81:233–242. [PubMed] [Google Scholar]
- [35]. Mackenzie L, Byles J, D’Este C. Validation of self-reported fall events in intervention studies. Clin Rehabil 2006;20:331–339. [DOI] [PubMed] [Google Scholar]