Abstract
Background:
Cervical radiculopathy is an important subgroup of neck disorders causing severe pain and disability.
Objectives:
The study assessed the effect of transverse oscillatory pressure (TOP) on pain intensity and functional disability of patients with cervical radiculopathy.
Methods:
Twenty-six individuals with unilateral radiating neck pain were randomly allocated into Group A (8 males and 5 females) and Group B (6 males and 7 females). Participants in the two groups received kneading massage, cryotherapy, and active isometric exercises to the posterior paraspinal muscles, trapezuis, and sternomastoid muscles. TOP was administered to Group A, whereas Group B served as control. Treatment was applied three times per week for 4 weeks, making 12 treatment sessions for each participant. Visual analogue scale and Neck Disability Index were used to assess pain intensity and neck disability, respectively, at baseline, 2 weeks, and 4 weeks. Data were analysed using repeated-measures analysis of variance.
Results:
There was a significant improvement in pain intensity and neck functional disability of patients between baseline, 2nd week, and 4th week of treatment sessions in Groups A and B (p < 0.05). There was a significant reduction in pain intensity in Group A (f = 7.08, p < 0.05) at the 2nd week and 4th week compared with Group B.
Conclusion:
It can be concluded that TOP reduces pain faster in patients with cervical radiculopathy.
Keywords: cervical radiculopathy, neck disability, pain intensity, transverse oscillatory pressure, visual analogue scale
Introduction
Cervical radiculopathy resulting primarily from an inflammation of a cervical nerve root induced by a lesion that reduces the intervertebral foramen formed an important subgroup of neck disorders which lead to more severe pain and disability [1–7]. Cervical radiculopathy is a disease process marked by nerve compression from herniated disc material or arthritic bone spurs which typically produces neck and radiating arm pain or numbness, sensory deficits, or motor dysfunction in the neck and upper extremities [8]. An epidemiologic survey showed the annual age-adjusted incidence of radiculopathy to be 83 per 100,000 persons [1]. Persons reporting radiculopathy were aged between 13 years and 91 years, and men were affected slightly more than women [8]. More than 14% of persons with radiculopathy reported antecedent physical exertion or trauma, and only 21.9% had an accompanying objective disc protrusion on imaging with spondylosis, disc protrusion, or both, which accounted for nearly 70% of cases [8].
The cervical spine has cervical nerve roots that exit above the level of the corresponding pedicle. For instance, the C5 nerve root exits at the C4–C5 disc space, and a C4–C5 disc herniation typically leads to C5 radiculopathy [8]. The exiting nerve root can be compressed by herniated disc material (soft disc herniation) or through encroachment by surrounding degenerative or hypertrophic bony elements (hard disc pathology). In either case, a combination of factors, such as inflammatory mediators (e.g., substance P), changes in vascular response, and intraneural edema, contribute to the development of radicular pain [9]. Pain radiation varies depending on the involved nerve root in which some distributional overlap may exist but absence of radiating extremity pain does not preclude nerve root compression; at times, pain may be isolated to the shoulder girdle [10]. Similarly, sensory or motor dysfunction may be present without significant pain. Symptoms are often exacerbated by extension and rotation of the neck (Spurling sign), which decreases the size of the neural foramen [11].
The main objectives of treatment in patients with cervical radiculopathy are to relieve pain, improve neurologic function, and prevent recurrences [12]. Some investigators have advocated the use of short-term immobilisation (<2 weeks) with either a hard or a soft collar (either continuously or only at night) to aid in pain control [13]. Exercise therapy—including active range-of-motion exercises and aerobic conditioning (walking or use of a stationary bicycle), followed by isometric and progressive-resistive exercises—is typically recommended once pain has subsided in order to reduce the risk of recurrence, although this recommendation is not supported by evidence from clinical trials [12]. Manual techniques are the therapeutic tools therapist uses to assist the body in the repair and adaptation processes [14]. The main aim of manual therapy is to decrease pain and increase functional activity in areas that are limited, whether they are joints, connective tissue, or skeletal muscles [15]. Joint movement and isometric muscle contraction stimulate joint and muscle proprioceptors [16]. This is theorised to produce pain relieve according to the gate-control theory of Melzack and Wall [17], where mechanoreceptor afferents are carried through large-diameter axons to inhibit nociceptive afferents at the dorsal horn of the spinal cord, therefore causing inhibition of pain.
An extensive literature review carried out by Haldeman et al [6] found that transverse oscillatory pressure (TOP), which is one of the techniques of manipulation, provides some benefit in the treatment of chronic mechanical neck pain. Empirical observations of Maitland [18] reported that TOP was recommended for unilaterally distributed symptoms of cervical origin. Egwu [19] studied the manual forces applied during vertebral mobilisation to the cervical spine and found that less time was spent in the use of anterior posterior unilateral pressure and posterior anterior unilateral pressure; he also noted that significantly more patients were pain-free with the use of these techniques when compared to cervical oscillatory rotation and TOP. TOP, originated by Nwuga [20], although one of the frequently used manipulative techniques by physiotherapists, has been claimed to be effective in amelioration of pain intensity especially radiating pain in cervical, thoracic, and lumbar regions [20,21]. It involves mobilisation of the spinous process of the vertebrae in the region of the spine that had mechanical pain [21]. This technique was reported to be useful when pain has a unilateral distribution, whether localised to the neck or referred to the upper limb [21]. However, there was dearth of documenting evidence on the efficacy of TOP in the management cervical radiculopathy. Therefore, the aim of the study was to examine the effect of TOP on pain intensity and the Neck Disability Index (NDI) of participants with cervical radiculopathy.
Methods
The participants for this study were 26 (14 males, 12 females) individuals referred for physiotherapy at the Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife, Nigeria, with cervical radiculopathy in either right or left upper limbs. They were recently diagnosed patients from the orthopaedic clinic of the same hospital.
All participants had cervical radiculopathy with a symptom of radiating neck pain of not less than 6 weeks’ duration with no history of vertebrobasilary artery insufficiency. From the patients’ history, the primary complaint was left-sided neck pain that radiated distally down the left arm to the elbow in 16 patients, whereas 10 patients reported radiation toward the right upper limb. Their pain started ~6–7 weeks prior to the study. No patient can recall a specific injury that precipitated his/her symptoms. The majority reported that they just woke up with neck and arm pain, and some discovered it while they were doing their daily activities. Pains were described in various forms, but a large percentage described the pain as a burning in the neck and a deep ache into the left arm that was aggravated by activities at work. Five patients reported numbness of some fingers in addition to the radiating pain.
Patients with unilateral radiating neck pain that were not of mechanical origin and patients with recent major trauma or fracture of the cervical spine, patients whose primary complaint was that of headaches or facial pain associated with unilateral radiating neck pain, and any patient who had received manual therapy of the cervical region in the past 3 months were excluded from the study.
Ethical approval (HREC NO: IPHOAU/12/33) was obtained from the Health Research Ethic Committee of Institute of Public Health, College of Health Sciences, Obafemi Awolowo University Ile Ife, Nigeria. On arrival at the clinic, the purpose and procedure of the study were explained to each participant, and consent was obtained prior to the research. Each participant’s blood pressure (in mmHg), height (m) and weight (kg) were measured. Active range of motion of the neck elicited pain, especially flexion towards the side of radiculopathy. Participants in both groups have not received physiotherapy intervention since the onset of their problem. Skin rolling test according to Bansevicius and Pareja [19] to the cervical region produced pain between the fourth cervical to seventh cervical vertebrae in all patients. Spurling's, distraction and Valsalva tests were carried out according to Konin et al [23] and were found positive.
Individuals found suitable for the study were randomly allocated into two groups. Twenty-six pieces of paper with inscription of TOP on 13 and CON on 13 were wrapped in an opaque envelope. Each participant picked a paper, and individuals who picked TOP were placed in Group A (8 males and 5 females) and the other participants were placed in Group B (6 males and 7 females). Two participants reported numbness on the index and middle fingers in Group A, and three participants reported numbness on the little and ring fingers in Group B.
Each participant in Groups A and B was treated three times per week. The maximum experimental treatment period for a participant was 4 weeks, after which the treatment time was estimated from the patient’s record. This cumulated to 12 treatment sessions for each participant in both groups. Present pain perception and neck functional disability were measured using visual analogue scale (VAS) and NDI, respectively.
Outcome measures
Patients were introduced to a 10-point VAS with instructions not to over- or underestimate the pain. VAS is a continuous scale comprised of a horizontal or vertical line, usually 10 cm (100 mm) in length, anchored by two verbal descriptors, one for each symptom extreme. The scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” (score of 100; 100-mm scale) [24]. Each participant was asked to point to the number corresponding to the pain intensity, which was recorded.
The NDI utilised in the study was in the English language. NDI is a commonly utilised outcome measure to capture perceived disability in patients with neck pain [25]. The NDI contains 10 items: seven related to activities of daily living, two related to pain, and one related to concentration [26]. Each item is scored from 0 to 5, and the total score is expressed as a percentage, with higher scores corresponding to greater disability [26]. The NDI has demonstrated moderate test–retest reliability and has been shown to be a valid health outcome measure in a patient population with cervical radiculopathy. Westaway et al [27] identified the minimum detectable change as 5 (10 percentage points) in a group of 31 patients with neck pain. Stratford and colleagues [28] identified the minimal detectable change also to be 5 (10 percentage points) in a group of 48 patients with neck pain and arm pain.
Interventions
Exercise therapy
During each appointment, participants in the two groups underwent exercises. All participants performed cervical spine retraction, rotation in each direction especially away from the direction of pain, extension, and contralateral side-bending stretching exercises. Deconditioning of cervical deep neck flexors was also addressed through exercise according to Ylinen et al [29]. The exercises also included passive stretching and isometric exercises to the posterior neck muscles. Isometric exercise was administered according to Kisner and Colby [30] to the posterior neck muscles for 10 seconds in 10 rounds, in which the contraction was against resistance of the physiotherapist’s hand. Ice chips were packed in a towel and applied to the cervical region for 7 minutes, then kneading massage was applied with methyl salicylate ointment for 3 minutes.
TOP
For participants in Group A, in addition to the exercise therapy, cryotherapy, and massage with methyl salicylate ointment were also applied. TOP was administered with the patient lying prone on a couch with the forehead placed on the backs of her fingers. Standing on the side of the patient, the therapist placed the pad of the thumbs against the left side (or the right side depending on the location of the pain) of the spinous process of the vertebrae to be moved. The fingers are spread out on the neck and the upper thoracic region. Pressure is directed horizontally through the thumbs to the side of the spinous process. TOP is executed by a pressure-relaxed sequence on the spinous process. Movement is initiated from the trunk and transmitted down the arm to the thumbs [21]. Treatment is effected by a push–relax sequence on the spinous process using the thumbs to produce an oscillatory movement. Transverse pressure was directed towards the side of pain on the cervical vertebrae. The oscillation is done rhythmically for a period of 20 seconds. This was repeated three times with a rest period of 2 minutes for a session per day [21].
Treatment was administered three times per week for 4 weeks and cumulated to 12 treatment sessions. Patient response was assessed after each third treatment session using VAS and NDI. Patients were advised not to involve in any other intervention without consulting the corresponding author of this article.
Data analysis
SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used to analyse the data. Descriptive and inferential statistics were used to summarise the result. An independent t test was used to compare each of the physical characteristics of the participants in Groups A and B. Repeated-measures analysis of variance (ANOVA) testing was used to compare the pretreatment, 2nd week, and 4th week values of present pain intensity and NDI of participants in Groups A and B. Repeated-measures ANOVA was also used to compare pretreatment, 2nd week, and 4th week values of the outcome measures between Groups A and B. Post hoc analysis using Tukey’s highest significant difference was carried out to examine which variables were significantly different from each other. An alpha level of 0.05 was set as level of significant.
Results
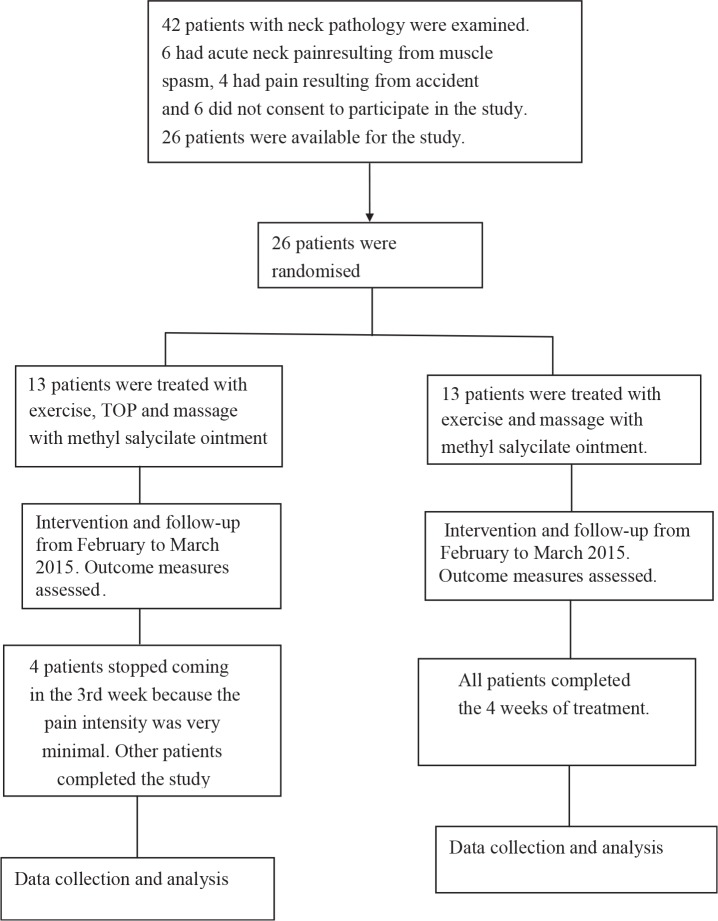
The study was designed to assess the effect of TOP in the management of cervical radiculopathy. Figure 1 illustrates the flow of patients through the study. Overall, 42 patients with neck pathology were examined. Six patients had acute neck pain resulting from muscle spasm, four patients had pain resulting from accidents, and six patients did not consent to participate in the study, leaving 26 patients available for the study. The 26 patients were randomly assigned into two groups. TOP, exercise, and massage with methyl salicylate ointment were given to Group A, whereas exercise and massage with methyl salicylate ointment only were provided to Group B, which served as the control group. Individuals in the two groups received range of motion exercise, stretching and strengthening exercise, and cryotherapy three times a week for 4 weeks, making 12 treatment sessions. TOP was applied in addition to exercise for Group A, whereas Group B served as control.
Figure 1.
Flow chart for the randomised controlled trial.
The physical characteristics of participants in the two groups are presented in Table 1. The mean values of physical characteristics of participants in Group A were not significantly different from those of their Group B counterparts.
Table 1.
Physical characteristics of participants (N = 26).
| Variables | Mean ± SD | T | p | |
|---|---|---|---|---|
| Group A | Group B | |||
| Age (y) | 55.67 ± 5.35 | 59.50 ± 2.646 | 3.01 | 0.08 |
| Weight (kg) | 73.13 ± 13.010 | 71.25 ± 5.377 | 0.05 | 0.95 |
| Height (m) | 1.63 ± 0.12 | 1.65 ± 0.026 | 0.09 | 0.92 |
| BMI (kg/m2) | 26.83 ± 4.43 | 26.02 ± 2.041 | 0.15 | 0.86 |
BMI = body mass index; SD = standard deviation.
Table 2 compares the pretreatment, 2nd week, and 4th week pain intensity values of Group A. There was a significant difference between the pretreatment, 2nd week, and 4th week values of pain intensity (f = 37.881; p < 0.001) and NDI (f = 23.156; p < 0.001) in the group. The difference in pain intensity between the pretreatment and the 2nd week was 2.8, and that between the 2nd week and 4th week was 2.17. Moreover, the difference in NDI between pretreatment and the 2nd week was 19.66, and that between the 2nd week and 4th week was 22.67.
Table 2.
Repeated-measures ANOVA comparing the outcome measures of pretreatment, 2nd week, and 4th week sessions in Group A (N = 13).
| Variables | Mean ± SD | F | p | |
|---|---|---|---|---|
| Pain intensity | Pretreatment | 7.63 ± 2.98 | ||
| 2nd wk | 4.83 ± 0.75 | 37.881 | <0.001* | |
| 4th wk | 2.66 ± 0.81 | |||
| Neck Disability Index | Pretreatment | 58.66 ± 8.91 | ||
| 2nd wk | 39.00 ± 17.46 | 23.156 | <0.001* | |
| 4th wk | 16.33 ± 9.75 | |||
Significant at p < 0.001.
ANOVA = analysis of variance; SD = standard deviation.
Table 3 compares the pretreatment, 2nd week, and 4th week pain intensity values of Group B. There was a significant difference between the pretreatment, 2nd week, and 4th week values of pain intensity (f = 34.40; p < 0.001) and NDI (f = 24.54; p < 0.001) in the group. The difference in pain intensity between pretreatment and the 2nd week was 1.5, and that between the 2nd week and 4th week was 2.59. Meanwhile, the difference in NDI between pretreatment and the 2nd week was 19.51, and that between the 2nd week and the 4th week was 12.32.
Table 3.
Repeated-measures ANOVA comparing the outcome measures of pretreatment, 2nd week, and 4th week sessions in Group B (N = 13).
| Variables | Mean ± SD | F | p | |
|---|---|---|---|---|
| Pain intensity | Pretreatment | 7.75 ± 0.96 | ||
| 2nd wk | 6.25 ± 0.95 | 34.400 | <0.001* | |
| 4th wk | 3.66 ± 0.81 | |||
| Neck Disability Index | Pretreatment | 53.33 ± 11.30 | ||
| 2nd wk | 33.82 ± 1.67 | 24.540 | <0.001* | |
| 4th wk | 21.50 ± 5.00 | |||
Significant at p < 0.001.
ANOVA = analysis of variance; SD = standard deviation.
Table 4 shows the results of repeated-measures ANOVA and post hoc analysis using Tukey’s highest significant difference comparing the pain intensity of Group A and Group B during pretreatment, 2nd week, and 4th week treatment session. A significant reduction was observed between Groups A and B at the 2nd week (f = 31.240; p < 0.05) and the 4th week (f = 31.240, p < 0.05). The difference in pain intensity in the 2nd week and 4th week between Groups A and B were 1.42 and 2.01, respectively.
Table 4.
Repeated-measures ANOVA with post hoc comparing the pain intensity of Groups A and B at pretreatment, 2nd week, and 4th week sessions (N = 26).a
| Variables | Mean ± SD | f | p | |
|---|---|---|---|---|
| Group A (13) | Group B (13) | |||
| Pretreatment | 7.63 ± 2.98a | 7.75 ± 0.96a | ||
| 2nd wk | 4.83 ± 0.75b | 6.25 ± 0.95c | 31.240 | 0.003* |
| 4th wk | 2.66 ± 0.81d | 4.67 ± 0.81e | ||
Significant at p < 0.05.
ANOVA = analysis of variance; SD = standard deviation.
Post hoc Tukey’s highest significant difference. Superscript letters within the table: mean mode with the same superscript letters indicate no significant difference between means. Mean mode with different superscript letters indicate significant difference.
Table 5 presents the results of repeated-measures ANOVA comparing the pretreatment, 2nd week, and 4th week NDI values in Groups A and B. There was no significant difference between the pretreatment, 2nd week, and 4th week NDI in Groups A and B (f = 1.46; p > 0.05).
Table 5.
Repeated-measures ANOVA comparing the NDI of Groups A and B at pretreatment, 2nd week, and 4th week sessions (N = 26).a
| Variables | Mean ± SD | F | p | |
|---|---|---|---|---|
| Group A (13) | Group B (13) | |||
| Pretreatment | 58.66 ± 8.91a | 53.33 ± 11.30a | ||
| 2nd wk | 39.00 ± 17.46b | 33.82 ± 1.67b | 1.46 | 0.46 |
| 4th wk | 16.33 ± 9.75c | 21.50 ± 5.00c | ||
* Significant at p < 0.05.
ANOVA = analysis of variance; NDI = Neck Disability Index; SD = standard deviation.
Superscript letters within the table: mean mode with the same superscript letters indicate no significant difference between means. Mean mode with different superscript letters indicate significant difference.
Discussion
The purpose of this study was to examine the therapeutic efficacy of TOP in the management of pain intensity and functional disability of patients with cervical radiculopathy. TOP was found to induce a significant reduction on clinical outcome measures especially in Group A. The mean difference between the pretreatment and 2nd week values of pain intensity in Group A was greater than that of Group B. Also, the mean difference of NDI at the 4th week in Group A was greater than that of Group B, an indication that TOP has a significant therapeutic effect in the management of cervical radiculopathy. Manual therapy including TOP may alter segmental biomechanics by releasing trapped meniscoids, releasing adhesions, or by diminishing distortion in the intervertebral disc [31–33]. Also, individual motion segments are thought capable of buckling, thereby producing relatively large vertebral motions that achieve a new position of stable equilibrium [34]. The manipulative impulse may provide sufficient energy to restore a buckled segment to a lower energy level, thus reducing mechanical stress or strain on soft and hard spinal tissues [35]. Gillette [36] proposed that spinal manipulation activates all known mechanosensitive, somatosensory receptors because they all possess mechanical thresholds lower than the peak force delivered during a manipulation, and because the receptor types are responsive to dynamic and/or static components of a mechanical stimulus.
Our study showed further that there was a significant reduction in pain intensity at the 2nd week of the study in Group A compared to Group B, an indication that patients will have faster pain relief with TOP. Haldeman et al [6] found that TOP provides some benefit in the treatment of chronic mechanical neck pain. Empirical observations of Maitland [18] also reported that TOP was recommended for unilaterally distributed symptoms of cervical origin. Our findings are in agreement with these studies. Moreover, Hurwitz et al [37] supported the use of manual therapy and exercises for neck pain in comparison to alternative treatments and suggested a lack of research in patients experiencing neck pain with radicular symptoms.
The study demonstrated significant reduction in pain intensity and NDI scores over a period of 4 weeks for the experimental and control groups. This is an indication that pain of cervical radiculopathy and NDI can be reduced when treated with a combination of exercise, massage, and cryotherapy. The improvement of outcome measures in Group B is in line with the observation of Radhakrishnan et al [1]. They reported that conservative treatment is generally believed to alleviate symptoms of cervical radiculopathy, at least for the short term, and the long-term prognosis remains unknown. In their study, Gupta et al [38] compared postisometric relaxation and isometric exercise in nonspecific neck pain and reported a significant improvement in pain intensity and NDI in two groups. The study also reported that exercise therapy—including active range-of-motion exercises and aerobic conditioning (walking or use of a stationary bicycle), followed by isometric and progressive–resistive exercises—is typically recommended in a case of cervical radiculopathy once pain has subsided in order to reduce the risk of recurrence [12]. Exercise appears to improve pain and function over the long term [39]. Studies have examined the effect of isometric exercise on the contracting body part, as well as on the contralateral and a distant body part to the contracting one [40–43]. Importantly, the hypoalgesic effect of isometric exercise was multisegmental and not isolated to the contracting muscle. Moreover, the pain-reducing effects of isometric exercise on the contralateral and distant body parts were similar in magnitude to the local body part. These results suggest that a central widespread inhibitory mechanism is activated by static muscle contractions. As discussed by Kosek and Lundberg, these central mechanisms may include increased secretion of β-endorphins, attention mechanisms, activation of diffuse noxious inhibitory controls, or an interaction of the cardiovascular and pain regulatory systems [41].
The effect of kneading massage in this study is explained by researchers who documented that massage has traditionally been used to relieve pain in producing short-lived analgesia by activating the “pain gate” mechanism [44]. Cutaneous mechanoreceptors are stimulated by touch and transmit information within large nerve fibres to the spinal cord [45,46]. These impulses block the passage of painful stimuli entering the same spinal segment along small, slowly conducting neurons [47]. Massage is a potent mechanical stimulus and a particularly effective trigger for the pain gate process which can reinforce a naturally occurring discomfort, cause much greater release of opiates, and achieve more profound pain suppression [48]. On muscle fibres, massage reduces discomfort, relieves the associated muscle spasm, and permits improved function [49].
The contribution of cryotherapy in the relief of pain has been reported in studies noting that cryotherapy may be most effective when combined with exercise [50,51]. Adequate cooling can reduce pain, spasm, and neural inhibition, thereby allowing for earlier and more aggressive exercises. Cryotherapy can increase pain tolerance and pain threshold and decrease nerve conduction velocity [51].
Conclusion
It could be concluded from the study that there was an overall improvement in pain intensity and NDI scores over 4 weeks of treatment regardless of the intervention (ice therapy, exercise, and TOP). The study revealed that addition of TOP in the management of cervical radiculopathy reduced pain intensity faster compared with cryotherapy, massage, and exercise only.
Footnotes
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding/support: No financial or grant support was received from governmental or private organizations for the work described in this article.
References
- [1]. Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy: a population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994;117:325–335. [DOI] [PubMed] [Google Scholar]
- [2]. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J 2007;16:307–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2008;38:A1–A34. [DOI] [PubMed] [Google Scholar]
- [4]. Tsakitzidis G, Remmen R, Peremans L, Van Royen P, Duchesnes C, Paulus D, et al. Non-specific neck pain: diagnosis and treatment. KCE Reports. 2009. 119C [Google Scholar]
- [5]. Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine 2003;28:2030–2035. [DOI] [PubMed] [Google Scholar]
- [6]. Haldeman S, Carroll L, Cassidy JD, Schubert J, Nygren A. The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its Associated Disorders: executive summary. Spine 2008; 33(2 Suppl.):S5–7. [DOI] [PubMed] [Google Scholar]
- [7]. Manchikanti L, Singh V, Kloth DS, Slipman CW, Jasper JF, Trescot AM, et al. Interventional techniques in the management of chronic pain: Part 2.0. Pain Physician 2001;4:24–96. [PubMed] [Google Scholar]
- [8]. Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. Am Fam Physician 2010;81:33–40. [PubMed] [Google Scholar]
- [9]. Levine MJ, Albert TJ, Smith MD. Cervical radiculopathy: diagnosis and nonoperative management. J Am Acad Orthop Surg 1996;4:305–316. [DOI] [PubMed] [Google Scholar]
- [10]. Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg 2007;15:486–494. [DOI] [PubMed] [Google Scholar]
- [11]. Polston DW. Cervical radiculopathy. Neurol Clin 2007;25:373–385. [DOI] [PubMed] [Google Scholar]
- [12]. Wolff MW, Levine LA. Cervical radiculopathies: conservative approaches to management. Phys Med Rehabil Clin N Am 2002;13:589–608. [DOI] [PubMed] [Google Scholar]
- [13]. Redford JB, Patel A. Orthotic devices in the management of spinal disorders. Phys Med Rehabil 1995;9:709–724. [Google Scholar]
- [14]. Ledeman E. The science & practice of manual therapy. 2nd ed Edinburgh: Churchill Livingstone; 2005. [Google Scholar]
- [15]. Korr IM. Neurobiologic mechanisms in manipulative therapy. New York: Plenum Press; 1978; p. xv–vii. [Google Scholar]
- [16]. Fryer G. Muscle energy concepts — a need for change. J Osteopathic Med 2000;3:54–59. [Google Scholar]
- [17]. Melzack R, Wall PD. Pain mechanisms: a new theory. Science 1965;150:971–979. [DOI] [PubMed] [Google Scholar]
- [18]. Maitland GD. Vertebral manipulation. 5th ed Boston: Butterworth-Hienemann; 2003. p. 201–212. [Google Scholar]
- [19]. Egwu MO. Relative therapeutic efficacy of some vertebral mobilization techniques in the management of unilateral cervical spondylosis: a comparative study. J Phys Ther Sci 2008;20:103–108. [Google Scholar]
- [20]. Nwuga VCB. Techniques of spinal manipulation In: Nwuga VC, editor. Manipulation of the spine. Baltimore, MD: William and Wilkins Company; 1975. p. 53. [Google Scholar]
- [21]. Nwuga VCB. Techniques of spinal manual therapy In: Nwuga VC, editor. Manual treatment of back pain. 2nd ed William and Wilkins, 2007. p. 115 [Google Scholar]
- [22]. Bansevicius D, Pareja JA. The “skin roll” test: a diagnostic test for cervicogenic headache?. Funct Neurol 1998;13:125–133. [PubMed] [Google Scholar]
- [23]. Konin JG, Wiksten DL, Isear JA Jr., Brader H. Cervical spine. Special test for orthopedic examination. 3rd ed Thorofare, NJ: Slack; 2006. p. 13–17. [Google Scholar]
- [24]. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain. Arthritis Care Res 2011;63:s240–s252. [DOI] [PubMed] [Google Scholar]
- [25]. Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine 2002;5:515–522. [DOI] [PubMed] [Google Scholar]
- [26]. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipul Physiol Ther 1991;14:409–415. [PubMed] [Google Scholar]
- [27]. Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: validation of its use in persons with neck dysfunction. J Orthop Sports Phys Ther 1998;27:331–338. [DOI] [PubMed] [Google Scholar]
- [28]. Stratford PW, Riddle DL, Binkley JM, Spadoni G, Westaway MD, Padfield B. Using the neck disability index to make decisions concerning individual patients. Physiother Can 1999;51:107–112. [Google Scholar]
- [29]. Ylinen J, Takala EP, Nykanen M. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA 2003;289:2509–2516. [DOI] [PubMed] [Google Scholar]
- [30]. Kisner C, Colby LA. Resisted exercise for impaired muscle performance In: Therapeutic exercise foundation and techniques. 5th ed Philadelphia: F.A. Davis Company; 2007. p. 169. [Google Scholar]
- [31]. Farfan HF. The scientific basis of manipulation procedures In: Buchanan WW, Kahn MF, Laine V, Rodnan GP, Scott JT, Zvaifler NJ, et al., editors. Clinics in rheumatic diseases. London: W.B. Saunders Company; 1980. p. 159–177. [Google Scholar]
- [32]. Giles LGF. Anatomical basis of low back pain. Baltimore: Williams & Wilkins; 1989. [Google Scholar]
- [33]. Vernon H. Biological rationale for possible benefits of spinal manipulation Cherkin DC, Mootz RD. Chiropractic in the United States: training, practice and research. AHCPR Publication No. 98-N002; 1997. 105–115.
- [34]. Wilder DG, Pope MH, Frymoyer JW. The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord 1988;1:16–32. [PubMed] [Google Scholar]
- [35]. Triano J. The mechanics of spinal manipulation In: Herzog W, editor. Clinical biomechanics of spinal manipulation. New York: Churchill Livingstone; 2001. p. 92–190. [Google Scholar]
- [36]. Gillette RG. A speculative argument for the coactivation of diverse somatic receptor populations by forceful chiropractic adjustments. Manual Med 1987;3:1–14. [Google Scholar]
- [37]. Hurwitz EL, Carragee JEJ, van der Velde G, Carroll LJ, Nordin M, Guzman J. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33:S123–S152. [DOI] [PubMed] [Google Scholar]
- [38]. Gupta S, Jaiswal P, Chhabra D. A comparative study between postisometric relaxation and isometric exercise in non-specific neck pain. J Exerc Sci Physiother 2008;4:88–94. [Google Scholar]
- [39]. Kay T, Rutherford S, McCall R, Voth S, Gross AR, Santaguida L. Exercises for mechanical neck disorders: a Cochrane review update. Orthopaedic Symposium 2008.
- [40]. Kadetoff D, Kosek E. The effects of static muscular contraction on blood pressure, heart rate, pain ratings and pressure pain thresholds in healthy individuals and patients with fibromyalgia. Eur J Pain 2007;11:39–47. [DOI] [PubMed] [Google Scholar]
- [41]. Kosek E, Lundberg L. Segmental and plurisegmental modulation of pressure pain thresholds during static muscle contractions in healthy individuals. Eur J Pain 2003;7:251–258. [DOI] [PubMed] [Google Scholar]
- [42]. Lannersten L, Kosek E. Dysfunction of endogenous pain inhibition during exercise with painful muscles in patients with shoulder myalgia and fibromyalgia. Pain 2010;151:77–86. [DOI] [PubMed] [Google Scholar]
- [43]. Staud R, Robinson M, Price D. Isometric exercise has opposite effects on central pain mechanisms in fibromyalgia patients compared to normal controls. Pain. 2005;118:176–184. [DOI] [PubMed] [Google Scholar]
- [44]. Jacobs M. Massage for the relief of pain: anatomical and physiological considerations. Phys Ther Rev 1960;40:93–98. [DOI] [PubMed] [Google Scholar]
- [45]. Bowsher D. Modulation of nociceptive input In: Wells PE, Frampton V, Bowsher D, editors. Pain: management and control in physiotherapy. London, UK: Heinemann Medical; 1988. Chapter 13. [Google Scholar]
- [46]. Watson J. Pain mechanisms: a review: 1. Characteristics of the peripheral receptors. Aust J Physiother 1981;27:135–143. [DOI] [PubMed] [Google Scholar]
- [47]. Goats GC. Massage — the scientific basis of an ancient art: Part 2. Physiological and therapeutic effects. Br J Sports Med 1994;28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48]. Nordschow M, Bierman W. Influence of manual massage on muscle relaxation: effect on trunk flexion. Phys Ther 1962;42:653. [DOI] [PubMed] [Google Scholar]
- [49]. Knight K. Cryotherapy in sports injury management. Int Perspect Physiother 1989;4: 163–185. [Google Scholar]
- [50]. Knight KL, Brucker JB, Stoneman PD. Muscle injury management with cryotherapy. Athletic Ther Today 2000;5:26–30. [Google Scholar]
- [51]. Algafly AA, George KP. The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. Br J Sports Med 2007;41:365–369. 10.1136/bjsm.2006.031237. [DOI] [PMC free article] [PubMed] [Google Scholar]