Abstract
Background:
Rehabilitation of subacute stroke patients represents a major challenge.
Objective:
This study was conducted to examine the effects of mirror therapy on balance ability among subacute stroke patients.
Methods:
The patients were assigned to a mirror therapy group (n = 17) or a sham therapy group (n = 17). Participants in the experimental group received mirror therapy and conventional rehabilitation therapy for a total of 60 minutes (mirror therapy: 30 minutes; conventional rehabilitation therapy: 30 minutes) per day, with a 10 minute rest period halfway through the session. Participants in the experimental group received training 5 days/week for 4 weeks. Participants in the control group received sham therapy and conventional rehabilitation therapy for a total of 60 minutes (sham therapy: 30 minutes, conventional rehabilitation therapy: 30 minutes) per day on the same day. Balance Index (BI) scores were obtained using a balance measurement system.
Results:
A significant difference in post-training gains for the overall stability index and medial and lateral stability index was observed between the experimental group and the control group (p < 0.05).
Conclusion:
We conclude that mirror therapy may be beneficial in improving balance ability among subacute stroke patients.
Keywords: balance, mirror therapy, subacute stroke
Introduction
Stroke, the number one cause of neurological disability worldwide, is characterised by both cognitive and motor impairments, as well as balance impairment, which may lead to functional dependence and reduced quality of life [1].
In particular, because of abnormal muscle tone, coordination disorder, and associated reactions, hemiplegic patients experience a considerable decrease of motor function in affected limbs [1]. The impaired lower extremity motor function commonly leads to functional limitations and disability [2].
Damage to balance ability after a stroke decreases stability in the standing position, causing difficulty in walking and performing functional activities. Hence, balance ability is the basis for independent movement and functional performance [3].
Treatments to improve function of stroke patients include constraint-induced therapy [4], mental imagery training [5], and robotic-assisted rehabilitation [6]. However, most intervention protocols are labour intensive, making the provision of intensive treatment for all patients difficult.
Mirror therapy, with its low cost and simplicity, may be a suitable alternative [7,8]. Ramachandran and Rogers-Ramachandran [9] introduced the use of visual illusions created by a mirror as a treatment for phantom pain.
A mirror is placed in the patient’s midsagittal plane, with the unaffected limb in front of it, so that the affected limb is blocked and the patient can only see the reflection of the intact limb [10]. Movement of the intact limb gives the patient the illusion in which inputs are perceived through the affected limb behind the mirror.
Studies on the effectiveness of mirror therapy in stroke patients, including a 2012 Cochrane analysis [11], identified methodologically appropriate randomised controlled trials [12]. In addition, Altschuler et al [13] implemented mirror therapy with stroke patients and proved the beneficial effects of mirror therapy on the range of motion of upper extremity joints, motion velocity, and accuracy. Sathian et al [8] found that, after 2 weeks of mirror therapy, a chronic stroke patient recovered hand function and grip strength in the paretic limb.
In previous research, mirror therapy focused mainly on the upper limb functions. However, since damage to lower limb function after stroke affects the independent daily functions, more studies are required to explore the issue of mirror therapy and balance ability which is very much related to the lower limb functions.
This study was conducted to examine the effect of mirror therapy on balance ability in subacute patients (onset within 6 months after a stroke).
Methods
Participants
Patients (n = 60) with stroke were screened for this study from March 2014 to August 2014. The inclusion criteria were: (1) sufficient cognitive ability to follow instructions (Mini-Mental State Examination score ≥ 24) [14]; (2) only mild spasticity in all joints of the affected limb (Modified Ashworth Scale score < 3) [15]; and (3) a higher than fair score on the Manual Muscle test [16].
The exclusion criteria were: (1) muscular-skeletal disorder and operation of the lower extremities; (2) limited range of motion of the lower extremity; (3) unilateral neglect, hemianopsia, or apraxia; and (4) psychological or emotional problems.
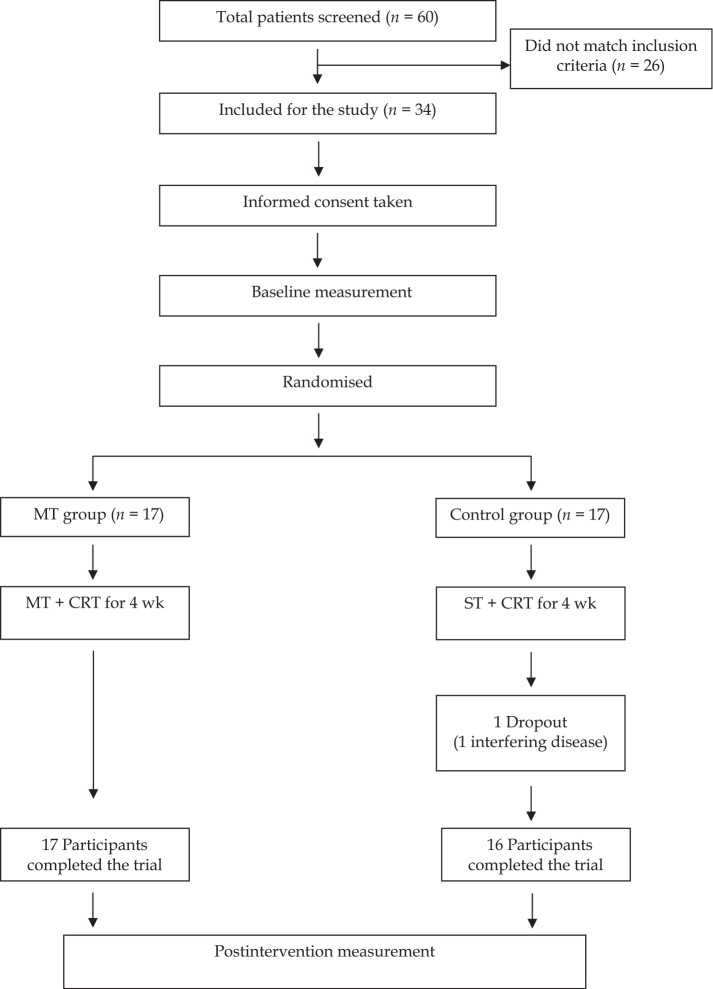
Thirty four patients with stroke met the criteria (Figure 1). The Research Ethics Committee of Eulji University Hospital approved the study, and all participants provided written informed consent prior to inclusion in the study. After completion of the initial assessment, the participants were randomly assigned to an experimental group (n = 17) or a control group (n = 17). For randomisation, sealed envelopes were prepared in advance and marked inside with A or B, indicating the experimental group or the control group respectively. The randomisation was done by a third party who was completely unaware of the study content. The participants’ characteristics and all outcome measures before and after the treatment were assessed by Physician 1, who was blinded to the treatment allocations. The mirror therapy and sham therapy were performed by Physician 2, who was not involved in the assessment of the participants, in a closed room. Both physicians were instructed not to communicate with the participants about the possible goals or the rationale of either treatment.
Figure 1.
Study flowchart. CRT = conventional rehabilitation therapy; MT = mirror therapy; ST = sham therapy.
Intervention
Participants in the experimental group received mirror therapy and conventional rehabilitation therapy for a total of 60 minutes (mirror therapy: 30 minutes; conventional rehabilitation therapy: 30 minutes) per day, with a 10 minutes rest period halfway through the session. Participants in the experimental group received training 5 days/week for 4 weeks. Conventional rehabilitation therapy consists of neurodevelopmental facilitation techniques. Subjects in the control group received sham therapy and conventional rehabilitation therapy for a total of 60 minutes (sham therapy: 30 minutes, conventional rehabilitation therapy: 30 minutes) per day on the same day.
Mirror therapy was performed using a modified version of that described in the study by Sütbeyaz et al [18] was modified. The participants performed the following actions: placing a chair in front of a full-length mirror and sitting and standing up from the chair, and standing while keeping feet in parallel back and forth. The control group performed the identical training in a space without a mirror.
Outcome measurement
Balance Index
Balance Index (BI) scores were obtained using a balance measurement system (Balance System SD, Biodex, NY, USA), which incorporates a specific monitor and a movable force platform, which provides up to 20 ° of surface tilt in a 360 ° range of motion, with a visual feedback system. BI refers to the participant’s ability to maintain the vertical axis of the body within a suitable range of the balance centre of the platform’s angle of tilt. A low BI score implies excellent balance ability [19].
In evaluation of balance ability, overall index captures the change of overall movement, anterior/posterior stability index captures the change on the sagittal plane, and medial/lateral stability index captures the change on the frontal plane. That is, the stability index means the movement change of the platform, where a higher value indicates more movement during the test.
The BI has a strong internal consistency, and acceptable intrarater (r = 0.82) and interrater (r = 0.70) reliability [19].
Statistical analysis
The general characteristics of the participants were tested for homogeneity using the independent t test. Paired t tests were used to verify statistical significance in performances before and after the experiment. An independent t test was performed for comparison between groups. The statistical significance level was set at α = 0.05.
Results
As shown in the summary of clinical and demographic features of the sample (n = 34) in Table 1, there were no significant differences in the baseline characteristics between the two groups (p > 0.05). One participant in the control group gave up the training due to extremely poor health. Therefore, 17 participants (experimental) and 16 participants (control) in each group completed this experiment. A significant difference in post-training gains for the overall stability index and medial and lateral stability index was observed between the experimental group and the control group (p < 0.05) (Table 2).
Table 1.
General and medical characteristics of participants (n = 34).
| EG (n = 17) | CG (n = 17) | t/X2 | p | |
|---|---|---|---|---|
| Age (y) | 52.4 (7.2) | 54.6 (10.2) | −0.548 | 0.453 |
| Height (cm) | 165.6 (6.4) | 165.3 (7.1) | 0.315 | 0.882 |
| Weight (kg) | 65.6 (9.3) | 67.7 (6.9) | −0.432 | 0.478 |
| Since onset (mo) | 4.7 (1.3) | 4.5 (1.1) | 0.443 | 0.663 |
| Sex (male/female) (n) | 8/9 | 7/10 | −0.336 | 0.739 |
| Affected side (left/right) (n) | 8/9 | 10/7 | 0.671 | 0.507 |
| Type of stroke (ischaemia/haemorrhage) (n) | 12/5 | 14/3 | 0.792 | 0.434 |
| MMSE-K (score) | 26.8 (2.2) | 26.5 (1.9) | 0.427 | 0.681 |
CG = control group; EG = experimental group; MMSE-K = Korean version of the Mini-Mental State Examination.
Values are presented as mean (SD) unless indicated otherwise.
Table 2.
Comparison of balance within and between groups (n = 33) (unit: degree).
| EG (n = 17) | CG (n = 16) | t | p | |||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | CWG | Pre | Post | CWG | |||
| Overalla | 5.29 (0.79) | 4.32 (1.12) | 0.97 (0.59–1.34)* | 5.31 (0.87) | 5.08 (0.88) | 0.23 (0.19–0.45)* | −2.155 | 0.038 |
| A/P | 4.42 (0.43) | 4.10 (0.51) | 0.32 (0.10–0.54)* | 4.43 (0.45) | 4.27 (0.51) | 0.16 (0.01–0.31)* | −0.983 | 0.333 |
| M/La | 4.27 (0.42) | 3.33 (0.67) | 0.94 (0.67–1.21)* | 4.06 (0.44) | 3.89 (0.45) | 0.17 (0.37–0.30)* | −2.816 | 0.008 |
Values are presented as mean (SD) except for changes within groups, which are expressed as mean differences (95% confidence intervals).
Overall = overall stability index; A/P = anterior and posterior stability index; M/L = medial and lateral stability index; CG = control group; CWG = changes within groups; EG = experimental group.
Significant difference in gains between two groups, p < 0.05.
Discussion
This study was conducted to investigate the effect of mirror therapy on the balance in patients with subacute stroke. According to the results, the treatment group showed a significant decrease of degree in overall stability index and in-and-out stability index after treatment compared to the control group, implying that mirror therapy is effective in improving balance ability.
Several underlying mechanisms have been suggested for the effect of mirror therapy on motor recovery after stroke. Stevens and Stoykov [20] suggested that mirror therapy is related to motor imagery and that the mirror provides visual feedback of the successful performance of the imagined action with the affected limb. Motor imagery itself, the mental performance of a movement without overt execution of this movement, has proven to be beneficial in the rehabilitation of stroke patients [21].
The effect of mirror therapy on brain activity has been investigated in a number of studies. Galeazzi et al [22] reported improvement of balance ability in stroke patients who performed exercise training in front of a full-length mirror. Lynch [23] argued that instant self-analysis and correction for the patients are possible, as they visually confirm their own physical alignment through mirrors. Sütbeyaz et al [17] randomly assigned 40 stroke patients to a mirror therapy group and a control group. The participants repeatedly performed dorsiflexion of the ankles with the non-affected lower limb placed in front of a mirror. In measurement of their functional ambulation categories, the mirror therapy group achieved a statistically significant higher level of improvement in gait ability than the control group.
Functional magnetic resonance imaging (fMRI) images related to mirror therapy found that the primary motor cortex, which is involved in the movements of the other side extremities, was excited by only observing the moving extremities in mirrors [24–26]. This finding shows that the functional organisation of motor systems is achieved not only by the active movements of the ipsilateral extremities, but also by passive observation of the movements of the contralateral extremities [25,26].
In another study, Altschuler et al [27] reported that application of mirror therapy to chronic stroke patients caused an increase in range of motion and moving speed of upper limbs, along with minute improvement of task performance ability that uses fingers. Cacchio et al [28], who applied mirror therapy to stroke patients, reported significant improvement of upper limb functions, as indicated by the Motor Activity Log and Wolf motor function test scores. Feltham et al [29] showed that visual feedback treatment using a mirror has positive effects on the bilateral coordination ability and neuromuscular activity among spastic hemiplegic patients.
These findings are generally in line with the results of the current study. As a cognitive intervention method, mirror therapy causes activation of the frontal or parietal lobe in the corresponding motor region, an area known as the mirror neurons, through only observing the behaviour of others [30].
Among the assumptions regarding the functional role of mirror neuron, the first one is expressing actions related to those entered into visual and auditory sense in exercise. This means understanding of the observed exercise goal and projecting it in exercise. The ventral premotor cortex and inferior parietal lobe control these reactions. The second assumption is about is realising the conceived emotional situation into motor reaction. Insula and rostral cingulate control these reactions [30].
Therefore, mirror therapy could play an important role in learning a new skill or understanding the behaviour of others, which can be used to motivate stroke patients [17]. Mirror therapy is performed on the non-paralysed side by moving the limbs of stroke patients; the movement of paralysed limbs through the reflection in the mirror shows a visual illusion of normal movement. This method for treating a brain injury is based on the principle of synaptic plasticity [17].
The current study has some limitations. First, the small sample size may have influenced the results. Second, the absence of follow-up after the end of the mirror therapy does not allow for determination of the durability of the effect of this therapy. Third, individual musculoskeletal and neurologic variations, which is important in patient evaluation, was not considered. This can be a significant factor affecting the research results regarding the improvement of balance ability. Finally, the study does not include diverse evaluation of the walking ability and independent daily routine which are important in quality of life. Therefore, these results can be generalised to subacute stroke patients. Further studies, including a long-term follow-up assessment, are needed to evaluate the long-term benefits of mirror therapy.
Conclusion
Mirror therapy may be beneficial in increasing the balance ability of subacute stroke patients. The data should be interpreted with caution due to the small sample size. A large-scale randomised controlled trial is required in order to confirm our findings and further evaluate the long-term effects of mirror therapy in patients after stroke.
Footnotes
Conflicts of interest: All contributing authors declare that they have no conflicts of interest.
Funding/support: No financial or material support of any kind was received for the work described in this article.
References
- [1]. Erkinjuntti T, Bowler JV, DeCarli CS, Fazekas F, Inzitari D, O’Brien JT, et al. Imaging of static brain lesions in vascular dementia: implications for clinical trials. Alzheimer Dis Assoc Disord 13(Suppl. 3): 1999; S81–90. [PubMed] [Google Scholar]
- [2]. Luke C, Dodd KJ, Brock K. Outcomes of the Bobath concept on upper limb recovery following stroke. Clin Rehabil 2004;18:888–898. [DOI] [PubMed] [Google Scholar]
- [3]. Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 1992;73:1073–1080. [PubMed] [Google Scholar]
- [4]. Page SJ, Sisto S, Johnston MV, Levine P, Hughes M. Modified constraint-induced therapy in subacute stroke: a case report. Arch Phys Med Rehabil 2002;83:286–290. [DOI] [PubMed] [Google Scholar]
- [5]. Liu H, Song L, Zhang T. Changes in brain activation in stroke patients after mental practice and physical exercise: a functional MRI study. Neural Regen Res 2014;9:1474–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Masiero S, Celia A, Rosati G, Armani M. Robotic-assisted rehabilitation of the upper limb after acute stroke. Arch Phys Med Rehabil 2007;88:142–149. [DOI] [PubMed] [Google Scholar]
- [7]. Michielsen ME, Selles RW, van der Geest JN, Smits M, Ribbers GM, Bussmann JB. Motor recovery and cortical reorganization after mirror therapy in chronic stroke patients: a phase II randomized controlled trial. Neurorehabil Neural Repair 2011;25:223–233. [DOI] [PubMed] [Google Scholar]
- [8]. Sathian K, Greenspan AI, Wolf SL. Doing it with mirrors: a case study of a novel approach to neurorehabilitation. Neurorehabil Neural Repair 2000;14:73–76. [DOI] [PubMed] [Google Scholar]
- [9]. Ramachandran, Rogers-Ramachandran D. Synaesthesia in phantom limbs induced with mirrors. Proc R Soc Lond B Bilo Sci 1996;263:377–386. [DOI] [PubMed] [Google Scholar]
- [10]. Dohle C, Pullen J, Nakaten A, Küst J, Rietz C, Karbe H. Mirror therapy promotes recovery from severe hemiparesis: a randomized controlled trial. Neurorehabil Neural Repair 2009;23:209–217. [DOI] [PubMed] [Google Scholar]
- [11]. Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror therapy for improving motor function after stroke. Cochrane Database Syst Rev 2012;3:CD008449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Lee MM, Cho HY, Song CH. The mirror therapy program enhances upper-limb motor recovery and motor function in acute stroke patients. Am J Phys Med Rehabil 2012;91:689–700. [DOI] [PubMed] [Google Scholar]
- [13]. Altschuler EL, Sidney B, Wisdom SL, Foster C, Galasko D, Llewellyn DM, et al. Rehabilitation of hemiparesis after stroke with a mirror. Lancet 1999;353:2035–2036. [DOI] [PubMed] [Google Scholar]
- [14]. Skidmore ER, Whyte EM, Holm MB, Becker JT, Butters MA, Dew MA, et al. Cognitive and affective predictors of rehabilitation participation after stroke. Arch Phys Med Rehabil 2010;91:203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Bohannon RW, Smith MB. Interrater reliability of a modified ashworth scale of muscle spasticity. Phys Ther 1987;67:206–207. [DOI] [PubMed] [Google Scholar]
- [16]. Aitkens S, Lord J, Bernauer E, Fowler WM Jr., Lieberman JS, Berck P. Relationship of manual muscle testing to objective strength measurements. Muscle Nerve 1989;12:173–177. [DOI] [PubMed] [Google Scholar]
- [17]. Sütbeyaz S, Yavuzer G, Sezer N, Koseoglu BF. Mirror therapy enhances lower-extremity motor recovery and motor functioning after stroke: a randomized controlled trial. Arch Phys Med Rehabil 2007;88:555–559. [DOI] [PubMed] [Google Scholar]
- [18]. Vaillant J, Vuillerme N, Janvy A, Louis F, Juvin R, Nougier V. Mirror versus stationary cross feedback in controlling the center of foot pressure displacement in quiet standing in elderly subjects. Arch Phys Med Rehabil 2004;85:1962–1965. [DOI] [PubMed] [Google Scholar]
- [19]. Srivstava A, Taly AB, Gupta A, Kumar S, Murali T. Post-stroke balance training : role of force platform with visual feedback technique. J Neurol Sci 2009;287:89–93. [DOI] [PubMed] [Google Scholar]
- [20]. Stevens JA, Stoykov ME. Using motor imagery in the rehabilitation of hemiparesis. Arch Phys Med Rehabil 2003;84:1090–1092. [DOI] [PubMed] [Google Scholar]
- [21]. Sharma N, Pomeroy VM, Baron JC. Motor imagery: a backdoor to the motor system after stroke?. Stroke 2006;37:1941–1952. [DOI] [PubMed] [Google Scholar]
- [22]. Galeazzi GM, Monzani D, Gherpelli C, Covezzi R, Guaraldi GP. Posturographic stabilisation of healthy participants exposed to full-length mirror image is inversely related to body-image preoccupations. Neurosci Lett 2006;410:71–75. [DOI] [PubMed] [Google Scholar]
- [23]. Lynch JA. The effect of mirror feedback in learning a frontal plane motor skill on students in a pilates mat program. Western Washington University; 2006. [Google Scholar]
- [24]. Luft AR, Smith GV, Forrester L, Whitall J, Macko RF, Hauser TK, et al. Comparing brain activation associated with isolated upper and lower limb movement across corresponding joints. Hum Brain Mapp 2002;17:131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Lipert J, Dettmers C, Terborg C, Weiller C. Inhibition of ipsilateral motor cortex during phasic generation of low force. Clin Neurophysiol 2001;112:114–121. [DOI] [PubMed] [Google Scholar]
- [26]. Muellbacher W, Ziemann U, Boroojerdi B, Cohen L, Hallett M. Role of the human motor cortex in rapid motor learning. Exp Brain Res 2001;136:431–438. [DOI] [PubMed] [Google Scholar]
- [27]. Altschuler EL, Wisdom SB, Stone L, Foster C, Galasko D, Llewellyn DM, et al. Rehabilitation of hemiparesis after stroke with a mirror. Lancet 1999;353:2035–2036. [DOI] [PubMed] [Google Scholar]
- [28]. Cacchio A, De blasis E, De Blasis V, Santilli V, Spacca G. Mirror therapy in complex regional pain syndrome type 1 of the upper limb in stroke patients. Neurorehabil Neural Repair 2009;23:792–799. [DOI] [PubMed] [Google Scholar]
- [29]. Feltham MG, Ledebt A, Deconinck FJ, Savelsbergh GJ. Mirror visual feedback induces lower neuromuscular activity in children with spastic hemiparetic cerebral palsy. Res Dev Disabil 2010;31:1525–1535. [DOI] [PubMed] [Google Scholar]
- [30]. Gallese V, Keysers C, Rizzolatti GA. Unifying view of the basis of social cognition. Trends Cogn Sci 2004;8:396–403. [DOI] [PubMed] [Google Scholar]