Abstract
Apixaban is a direct oral anticoagulant that works by inhibiting factor Xa. It has been associated with adverse bleeding outcomes including atraumatic splenic rupture. We present the case of an 86-year-old man who presented with features of left upper abdominal pain and hemorrhagic shock found to have atraumatic splenic rupture and hemoperitoneum on imaging.
Keywords: Apixaban, splenic rupture, atraumatic
Introduction
Apixaban is a direct oral anticoagulant (DOAC) approved by the US Food and Drug Administration (FDA) for use in non-valvular atrial fibrillation for stroke prevention.1 DOACs are associated with an increased risk of bleeding. Recently, atraumatic splenic rupture has been reported with their increasing use.2–8 We present a case of a spontaneous splenic rupture with hemorrhagic shock requiring emergent splenic artery embolization and splenectomy in the setting of apixaban use.
Case description
An 86-year-old gentleman presented to the emergency department (ED) after a fall due to orthostatic syncope. He had complained of left upper quadrant abdominal pain the night prior. According to his wife, he was restless overnight and had gone to the bathroom that morning when she heard him fall. The patient denied trauma prior to the onset of abdominal pain, recent sore throat, fever, chills, night sweats, weight loss, fatigue, reflux, or recent travel. His history was significant for atrial fibrillation, coronary artery disease, hypertension, hyperlipidemia, and type II diabetes mellitus. He did not have a history of bleeding or clotting disorders. His home medications included apixaban 5 mg two times daily, aspirin 81 mg daily, atorvastatin 40 mg daily, carvedilol 12.5 mg two times daily, hydrochlorothiazide 25 mg daily, lisinopril 10 mg daily, and metformin 500 mg two times daily. He was not on any medications with CYP3A4 or P-gp-inhibiting activity. On presentation, his temperature was 36.7°C (98.1°F), blood pressure was 107/67 mm Hg with nadir of 74/46 mm Hg, heart rate was 65/min, and respiratory rate was 16 breaths per minute. Physical examination was significant for diffuse bilateral abdominal tenderness without any guarding or rebound tenderness. He was lethargic and slow to follow commands. The remainder of the physical examination was normal.
Serologic testing revealed his hemoglobin was 11.8 g/dL (reference range: 14.0–17.5 g/dL), down from a baseline of 14 g/dL. Coagulation panel revealed international normalized ratio (INR) of 1.2 (reference range: 0.9–1.1), prothrombin time (PT) of 14.9 s (reference range: 11.7–14.1 s), activated partial thromboplastin time (aPTT) of 28 s (reference range: 23–34 s), and platelets 146,000/µL (reference range: 130,000–400,000/µL). His random blood sugar was 268 mg/dL (reference range: 70–99 mg/dL). Computed tomography (CT) of the abdomen/pelvis with contrast showed active extravasation from the spleen with a large subcapsular hematoma and hemoperitoneum (Figure 1). CT head with cervical spine was negative for acute intracranial mass or hemorrhage, fracture, or focal bony lesions. He was given 2.5 L of normal saline to maintain his systolic blood pressure over 100 mg Hg. He received a unit of prothrombin complex concentrate (PCC), 2 units of packed red blood cells (PRBCs), and 2 units of fresh frozen plasma (FFP) in the ED to reverse his coagulopathy. The patient was taken for emergent splenic arteriography and embolization. Embolization was initially pursued to avoid the need for an exploratory laparotomy as his blood pressures stabilized with initial volume resuscitation. Images after contrast injection demonstrated a small area of extravasation from the inferior tip of the spleen in the area of the abnormality seen on CT scan. The proximal third of the splenic artery was successfully embolized with a 10-mm Amplatzer 2 plug device. Post procedure, the patient’s blood pressure improved to 154/47 mm Hg. He was then admitted to the surgical intensive care unit for close monitoring. Over the course of hours, the patient again deteriorated and was hypotensive with systolic blood pressure in the 80s. He was short of breath. Bedside focused assessment with sonography for trauma (FAST) scan showed a flat inferior vena cava and a large hemoperitoneum. With concern for ongoing bleed, the patient was transfused 2 units of PRBCs and was taken to the operating room for exploratory laparotomy and splenectomy for a ruptured subcapsular splenic hematoma. Around 1500 mL of bloody fluid was removed from the peritoneum. No retroperitoneal hematoma was noted. Splenic pathology revealed capsular disruption with associated subcapsular and intra-parenchymal hemorrhage, and numerous macrophages within the splenic parenchyma likely secondary to a reactive phenomenon. His hematoma was thought to be related to apixaban use in the absence of trauma or splenic pathology. Patient’s postoperative hospital stay was unremarkable. His hemoglobin was stable at 11.7 g/dL. He was discharged on day 5 with recommendations to resume apixaban and aspirin.
Figure 1.
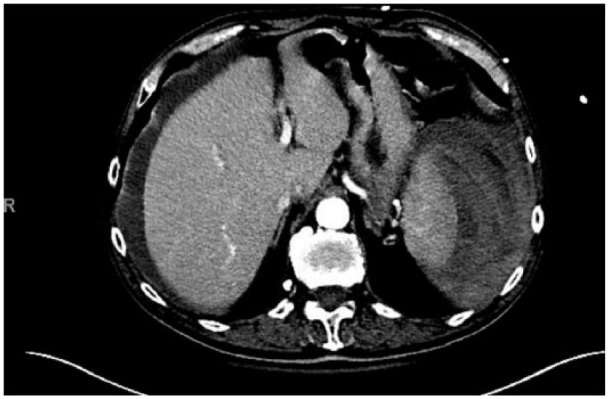
CT scan of the abdomen/pelvis showing large subcapsular hematoma and active extravasation from the spleen with associated hemoperitoneum.
Discussion
Spontaneous splenic rupture is a rare entity but has been noted to occur with infections such as infectious mononucleosis; hematologic neoplasms such as leukemia and lymphoma; non-infectious, inflammatory disorders such as amyloidosis and polyarteritis nodosa; medications; dialysis; and pregnancy.9,10 Orloff and Peskin11 established four criteria for spontaneous rupture of the normal spleen to which a fifth criterion was later added by Crate and Payne.12 In our case, the biopsy was negative for infiltrating atypical lymphocytes or monocytes that would be suggestive of infection, neoplasm, or inflammatory disorders. His renal function was unremarkable. Although he had a fall, this was preceded by left upper quadrant pain. Thus, we believe that his orthostatic syncope was a manifestation of low intravascular volume status from preceding splenic hemorrhage. We were not able to find an etiology for splenic rupture other than apixaban use.
DOACs, apixaban, rivaroxaban, and dabigatran have all been associated with atraumatic splenic rupture in previous literature.2–8 This is the third case related to apixaban.7,8 Apixaban has anticoagulant properties by inhibiting free and bound form of factor Xa.1 Lowry and Goldner7 suggest that apixaban may worsen previously undetected microtrauma that may lead to splenic hemorrhage. Concomitant use of antiplatelets, p-glycoprotein, and CYP3A4-inhibiting medications and poor renal function all increase the risk of bleeding with DOACs.2 Our patient was not on any medications that were associated with p-glycoprotein and CYP3A4-inhibiting activity. Atraumatic splenic rupture was noted early after initiation of a DOAC. Splenic rupture was reported 1 day, 2 days, and 2 months after initiation of dabigatran,6 apixaban,8 and rivaroxaban,4 respectively. Left-sided abdominal pain that may radiate to the shoulder, declining hemoglobin levels, hypotension, and features of hemorrhagic shock all suggest splenic hemorrhage.6,7 Due to its non-specific clinical picture, it can easily be mistaken for peptic ulcer disease or cardiac disease in the absence of trauma. Diagnosis should especially be considered in a patient who is on anticoagulation.7
Besides ultrasound can be urgently performed in these patients for rapid diagnosis,8 it can detect free fluid with 90% sensitivity and 99% specificity13 and can aid in early diagnosis and urgent consultations and guide treatment plans in cases with undifferentiated hypotension.14 CT scan is a recommended imaging modality for diagnosis, staging, and decision on surgical management.8 Initial management includes discontinuation of anticoagulants, volume resuscitation, and, if available, reversal of anticoagulation. Volume resuscitation with intravenous isotonic crystalloids offers the same benefit as colloids.15 PCC, FFP, and recombinant activated factor VII can be used in this setting despite lack of evidence.3 Current guidelines recommend RBC transfusion, platelet, and cryoprecipitate transfusion to maintain target hemoglobin >7 g/dL, platelet count >50,000/µL, and fibrinogen >100 mg/dL, respectively.15 With andexanet alfa being approved by FDA for reversal of anticoagulation in life-threatening or uncontrolled bleeding,16 it will be interesting to know its efficacy in patients with splenic hemorrhage. Surgical options for splenic rupture include conservative transcatheter arterial embolization and open surgical exploration.9 Spontaneous splenic hemorrhage can be managed conservatively with close monitoring if the patient is hemodynamically stable without signs of active hemorrhage or peritonitis.6,7 Embolization can be tried in hemodynamically stable patients with active contrast extravasation noted in CT angiography.17 Emergent laparotomy with splenectomy should be performed in hemodynamically unstable patients.7
Conclusion
Atraumatic splenic hemorrhage is life-threatening, and high index of suspicion for this should be maintained in patients presenting with abdominal pain, features of hypotension, and hemorrhagic shock while on apixaban. We hope this case will bring forward more similar reports in the future.
Acknowledgments
This study was accepted for poster presentation at the “Society of Hospital Medicine 2018 Annual Meeting.”
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Sijan Basnet  https://orcid.org/0000-0002-8324-2827
https://orcid.org/0000-0002-8324-2827
References
- 1. 202155s000lbl.pdf, https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202155s000lbl.pdf (accessed 5 November 2018). [Google Scholar]
- 2. Hattab YA, Speredelozzi D, Bajwa O. Rivaroxaban causing spontaneous splenic rupture C52. Illustrative disease presentations in critical care I, https://www.atsjournals.org/doi/pdf/10.1164/ajrccm-conference.2015.191.1_MeetingAbstracts.A4632 (accessed 5 November 2018).
- 3. Nagaraja V, Cranney G, Kushwaha V. Spontaneous splenic rupture due to rivaroxaban. Drug Ther Bull 2018; 56(11): 136–139. [DOI] [PubMed] [Google Scholar]
- 4. Gonzva J, Patricelli R, Lignac D. Spontaneous splenic rupture in a patient treated with rivaroxaban. Am J Emerg Med 2014; 32(8): 950e3. [DOI] [PubMed] [Google Scholar]
- 5. Amin A, Safaya A, Ronny F, et al. Hemorrhagic shock from spontaneous splenic rupture requiring open splenectomy in a patient taking rivaroxaban. Am Surg 2016; 82(2): E54–E15. [PubMed] [Google Scholar]
- 6. Carey R, Nelatur V. Spontaneous splenic rupture secondary to dabigatran: the last in a series of unfortunate events. Clin Med 2018; 18(5): 406–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lowry LE, Goldner JA. Spontaneous splenic rupture associated with apixaban: a case report. J Med Case Rep 2016; 10(1): 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Abdelhady A, Ahmed A, Mohamed Y, et al. Apixaban-associated spontaneous splenic rupture: a case report. Irish Med J, http://imj.ie/july-august-2018-c-r2-apixaban-associated-spontaneous-splenic-rupture/ (accessed 5 November 2018). [PubMed]
- 9. Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009; 96(10): 1114–1121. [DOI] [PubMed] [Google Scholar]
- 10. Debnath D, Valerio D. Atraumatic rupture of the spleen in adults. J R Coll Surg Edinb 2002; 47(1): 437–445. [PubMed] [Google Scholar]
- 11. Orloff MJ, Peskin GW. Spontaneous rupture of the normal spleen; a surgical enigma. Int Abstr Surg 1958; 106(1): 1–11. [PubMed] [Google Scholar]
- 12. Crate ID, Payne MJ. Is the diagnosis of spontaneous rupture of a normal spleen valid. J R Army Med Corps 1991; 137(1): 50–51. [DOI] [PubMed] [Google Scholar]
- 13. Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma 1995; 38(6): 879–885. [DOI] [PubMed] [Google Scholar]
- 14. Shokoohi H, Boniface KS, Pourmand A, et al. Bedside ultrasound reduces diagnostic uncertainty and guides resuscitation in patients with undifferentiated hypotension. Crit Care Med 2015; 43(12): 2562–2569. [DOI] [PubMed] [Google Scholar]
- 15. Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American College of Cardiology Task Force on expert consensus decision pathways. J Am Coll Cardiol 2017; 70(24): 3042–3067. [DOI] [PubMed] [Google Scholar]
- 16. Research C for BE and approved products—ANDEXXA (coagulation factor Xa (recombinant), inactivated-zhzo), https://www.fda.gov/biologicsbloodvaccines/cellulargenetherapyproducts/approvedproducts/ucm606681.htm (accessed 6 November 2018).
- 17. Raikhlin A, Baerlocher MO, Asch MR, et al. Imaging and transcatheter arterial embolization for traumatic splenic injuries: review of the literature. Can J Surg 2008; 51(6): 464–472. [PMC free article] [PubMed] [Google Scholar]


