Short abstract
The use of artificial intelligence (AI) has been rapidly progressing in medicine, particularly in radiology. AI has also been the source of great innovation and a prominent topic of discussion within radiology societies and ground-breaking research in recent years.
Despite the risks and quality assurance issues involved in AI, it offers tremendous opportunities for changing how radiological services are delivered. Moreover, it is conceivable that AI could become a reliable, hard-working friend to the radiologist rather than a foe, in addition to being a useful training tool for radiologist trainees.
Keywords: Artificial intelligence, radiology, radiologists, information technology
Introduction
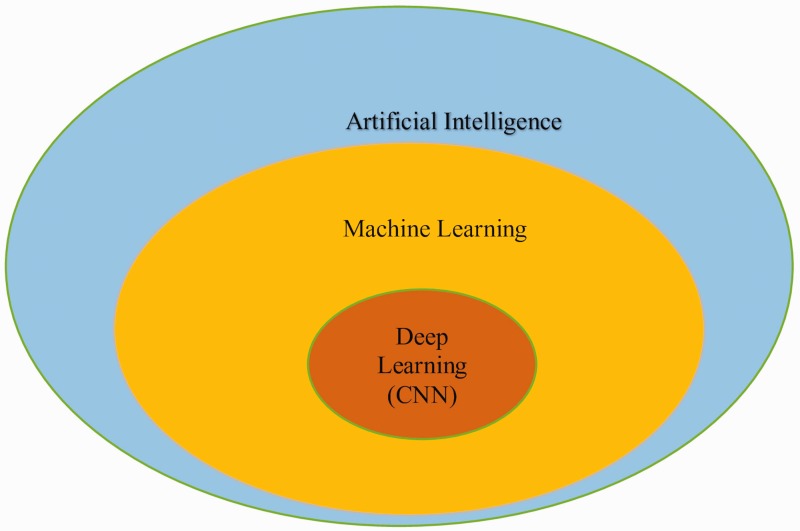
Artificial intelligence (AI) has been defined as computer systems able to perform tasks normally requiring human intelligence, e.g. visual perception, speech recognition, decision making, and language translating (1). Another simple way of describing AI is the ability of a computer program or a machine to think and learn. It is also a field of study which tries to make computers “smart.” They work on their own without being encoded with commands (2). In fact, AI is an umbrella term that comprises two components: machine learning (ML) and brain-inspired deep learning convolutional neural networks (CNN) (Fig. 1). Within the field of radiology, AI always refers to the more advanced components of deep learning/CNN (Fig. 1).
Fig. 1.
Artificial intelligence.
Description
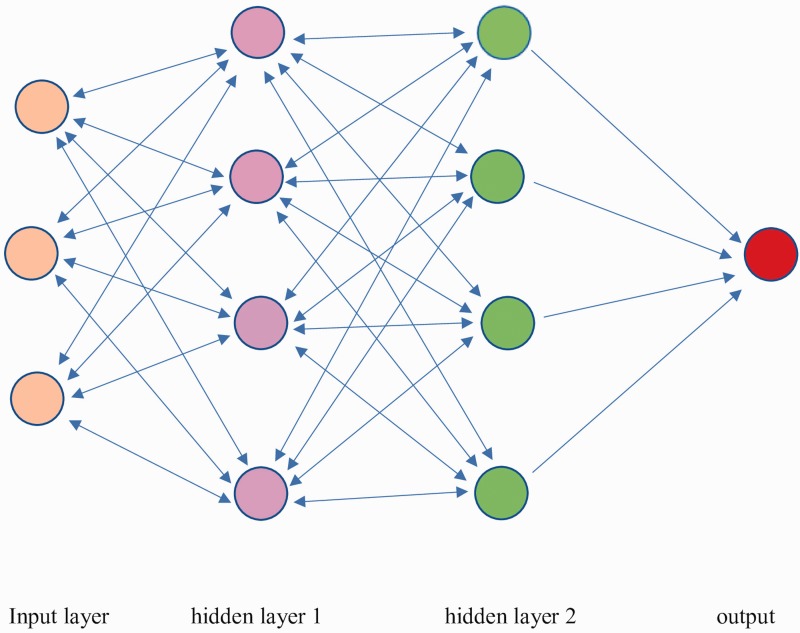
AI algorithms, particularly those used in deep learning, have already found a remarkable purpose in image recognition tasks. In particular, AI methods excel at automatically recognizing complex patterns in imaging data and providing a quantitative assessment of image characteristics (3). For their part, deep learning CNN networks work in the same way as an intelligent human brain and essentially mimic the function of human neural networks. They rely on input sections, in which data are entered, and at least one hidden layer (though often many layers) of neural rows. Each neuron-like unit interacts with the nearby units. The final layer of neural rows constitutes the output layer (Fig. 2). The most frequent programming languages used in AI are Python and R, and, as with the earlier inclusion of X-rays and ultrasound and magnetic resonance imaging (MRI) training in radiology curricula, it is conceivable that radiology curricula will include basic information about programming languages in the near future.
Fig. 2.
CNNs operating sample.
Evolution
Radiology is a medical specialty that is naturally related to technology and is very much dependent on machines; thus, it has experienced nearly constant evolution, in comparison to other medical specialties. At the same time, as is well-known, the field of information technology (IT) has evolved tremendously during the new millennium. Some of the innovations we have already witnessed are the development of driverless cars, automated chatbots for online banking, AI-driven multimedia, robotic arms for surgical procedures, mobile phone applications, the iPhone’s Siri assistant, innovations within the Google Chrome browser, applications that can recognize materials, plants, and living creatures, learning robots, and AI-driven strategies for large business chains. Along these same lines, AI has been rapidly progressing as a highly innovative area of radiological science in recent years. Moreover, it is widely used in almost all financial sectors, including the health sector, and has become a very popular topic within the field of radiology, particularly among radiology societies and recent ground-breaking research.
Present and future directions
Without question, AI appears to have a bright future ahead as a potentially “game-changing” tool in healthcare.
However, this overwhelming technological development has not come without the introduction of an element of fear within the field of radiological science, fear that has caused anxiety within radiological societies worldwide as some radiology professionals’ question whether AI will replace the need for trained radiologists. In contrast, other respected radiology researchers have made several encouraging statements, particularly during the 2018 Radiology Society of North America (RSNA) Congress in the US. For example, the president of the RSNA, Dr. Vijay M Rao, called for leaders within the radiology field to combat fear related to AI by promoting its benefits in her statement how AI promotes and augments radiology. Dr. Rao described how some associate deans in her institution had mentioned to medical students that radiology jobs would be replaced by AI and advised them not to go into radiology, which was the cause of rising anxiety among junior medical trainees (4).
Within the field of radiology, AI, or more specifically CNN, has been restricted to the role of a research topic to this point in time. That is, there is no adjunct method of using AI in radiology practice in Western countries. However, there has been an increase in the number of applications for U.S. Food and Drug Administration (FDA) approval of AI-driven imaging equipment (5), by large, well-known AI technology vendors, and it would appear that AI-dependent medical imaging in day-to-day practice is not far in the future.
AI publications
The recent RSNA meeting included the presentation of several papers and talks on this topic. Moreover, the RSNA also announced the premier of a new journal called Radiology: Artificial Intelligence and has begun to receive submissions of AI-related scientific papers.
In addition, there has been an increase in the number of papers related to AI submitted to the RSNA’s official journal, Radiology, a journal with a particularly high impact factor. A recent review article provided the exact numbers of AI paper submissions year by year from 2015 onwards. As quoted in the journal, there were no publications on AI in Radiology in 2015, three in 2016, 17 in 2017, and about 10% of submissions were AI-related studies in 2018 (6).
For example, Yasaka et al. conducted a study using CNN to characterize five categories of liver lesions using dynamic computed tomography (CT) scan: category A = classic hepatocellular carcinomas (HCC); category B = malignant liver tumors other than classic and early HCC; category C = indeterminate masses or mass-like lesions, including early HCCs and dysplastic nodules and rare benign liver masses other than hemangiomas and cysts; category D = hemangiomas; and category E = cysts. Their results were very encouraging in that the median accuracy of differential diagnosis of liver masses for test data was 0.84. The median area under the receiver operating characteristic (ROC) curve for differentiating categories A and B from C–E was 0.92. Their results confirmed that deep learning with CNN showed high diagnostic performance in the differentiation of liver masses in dynamic post-contrast CT studies (7).
In another recent study, Rajpurkar et al. demonstrated how their CNN, called the CheXNext algorithm, had roughly the same detection results, with high AUC and CIs, as radiologist recognition and classification of chest pathologies. For example, the worst performance value of the algorithm was 0.704, versus radiologist achievement of 0.911 for emphysema. On the other hand, their algorithm performed better than radiologist detection of atelectasis (0.862 vs. 0.808, respectively), while radiologists performed better in terms of detecting cardiomegaly and hernia. The detection rates for other pathologies (e.g. consolidation, edema, effusion, mass, nodule, fibrosis, and others) were similar (8).
Future predicted directions
It is difficult to predict whether AI will ultimately surpass human performance or where use of AI in radiology is heading in the future. However, a recent survey of AI experts conducted by Grace et al. mentioned that, for some complex tasks, AI will outperform humans in many activities in the next decade, such as translating languages (by 2024), driving a truck (by 2027), and working as a surgeon (by 2053). The experts who had participated in the survey believed that there is a likelihood of a 50% chance of AI surpassing human skills in 45 years (9). In terms of whether AI is a friend or foe to radiologists, it is similarly difficult to predict whether AI will become so powerful that it surpasses human skill. Some see that day arriving soon and extreme predictions see entire disciplines, such as radiology and dermatology, disappearing as they are replaced by AI. The true outcome of the application of AI to medicine, however, is much less clear (10,11).
Nonetheless, the year 2017 marked a steep change for AI in healthcare. Demonstrable successes with deep learning in other industries have triggered remarkable clinical interest. However, AI requires a thorough and systematic evaluation before its integration into routine clinical care. Nonetheless, like other disruptive technologies, the potential benefits of AI in healthcare should not be underestimated (12).
Technological innovation is constantly evolving. At the same time, every single innovation brings with it the apprehension of humans, who have been historically skeptical about sweeping new changes to established knowledge. Of course, the introduction of AI (i.e. CNN, learning machines, and advanced robots) to day-to-day medical practice will be accompanied by handicaps, e.g. misdiagnosis, over-diagnosis, low accuracy, and low specificity issues. In one example, recently published in an article about cardiovascular disease prediction in the Journal of the American Heart Association (JAHA), a machine learning risk calculator outperformed the American College of Cardiology/American heart Association (ACC/AHA) risk calculator by recommending less drug therapy and missing fewer cardiovascular disease events. The findings demonstrated the potential of machine learning for improving cardiovascular risk prediction and assisting in medical decision-making (13).
Of course, current radiologists may believe that AI is a threat to the specialty and may well fear that they will lose jobs in the near future. Without doubt, there will be job shortages, particularly in private health services, at all levels, from receptionists to healthcare assistants to higher level managers and, finally, radiologists. One prominent IT company, IBM, eliminated several hundred jobs in recent years. The same could happen in radiology, but to a lesser degree, especially in Europe and, specifically, in the UK, where there is an increasing shortage of radiologists, including trainees. According to the Royal College of Radiologists, the percentage of unfilled consultant radiology posts has been increasing and recently hit 10.3% (14).
Another fear related to AI is that human beings will one day be beaten by a CNN, as happened during play of a very complex board game—more sophisticated than chess—called Go. The AlphaGo computer program beat the world Go master champion, Lee Sedol, an 18-time world champion, representing a significant milestone for AI (15). It can easily be postulated that this could happen in medicine and radiology in the near future, despite the fact that medicine is multifaceted, extremely complex, and requires a human touch in most instances.
AI strengths and weaknesses
Generally speaking, AI has its limitations. Like an advanced scientific calculator, it can surpass human beings only in limited areas. However, AI could be programmed to surpass humans in the case of more complex tasks. For example, Xiaoyi, an AI-powered robot in China, recently took the national medical licensing examination and passed, making it the first robot to have done so. Not only did the robot pass the exam, it actually earned a score of 456 points, which is 96 points above the required marks (16).
In a recent review article from Japan, the limitations that exist as it relates to using current AI capabilities in radiology were described. Yet, it remains unclear how AI works and how it arrives at its outcomes; these areas will likely remain, at least for a time, the “black box” of AI. The optimal structuring and hyperparameters of CNNs and the numbers of cases needed to train models differ from one task to another and remain an ongoing challenge. Furthermore, the use of AI would raise privacy concerns among patients, particularly those with rare diseases. As it currently stands, present-day CNN models are task-specific and must be further developed to handle more complex diagnostic studies (17).
AI has been introduced in almost all sectors of the economy, including healthcare. It shows promise as a groundbreaking innovation in the same way that Wilhelm Conrad Roentgen’s X-ray transformed radiology. Moreover, it appears inevitable that AI will ultimately be introduced not only to the diagnostic side of radiology but also will be applied to triaging radiological investigations. Of course, AI also requires quality assurance (QA) checks, clinical trials, and more robust data to enhance its benefits.
There have been many promising AI research results since 2015 in radiology-related journals. Worldwide, radiology societies have begun to understand the significance of AI and its implementation and to adjust themselves to the prospect of using AI in day-to-day practice within the next decade or so. Close collaboration between technology experts and data scientists in radiology departments is needed to address QA issues and conduct relevant scientific studies. AI offers a promising future for healthcare, despite its risks and potential QA issues, and tremendous changes are sure to occur in terms of how radiological services are delivered in the future. The introduction of AI could allow radiologists to take on more complex tasks, along with a more intensive role in terms of job satisfaction and patient care.
In conclusion, AI, which is waiting for endorsements from the health regulator governmental bodies worldwide, seems to be a promising adjunctive tool for diagnosis and triaging, looks a reliable, hard-working friend rather than a foe to radiology despite some anxiety about for its implementation to the radiology practice and should be included in radiology training curricula in the near future.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Oxford Living Dictionaries. Artificial intelligence description in English. Available at: https://en.oxforddictionaries.com/definition/artificial_intelligence (accessed 23 December 2018).
- 2.Artificial intelligence. Available at: https://simple.wikipedia.org/wiki/Artificial_intelligence (accessed 23 December 2018).
- 3.Hosny A, Parmar C, Quackenbush J, et al. Artificial intelligence in radiology. Nat Rev Cancer 2018; 18:500–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rau VM. RSNA president calls for radiology leaders to explain AI. Available at: http://ai-med.io/rsna-president-calls-for-radiology-leaders-to-explain-ai/ (accessed 24 December 2018).
- 5.AI and the FDA. Available at: https://medium.com/datadriveninvestor/demystifying-the-current-upward-trend-in-fda-approvals-of-medical-devices-using-artificial-cb9cc18d175 (accessed 26 December 2018).
- 6.Bluemke DA. Are you working with AI or being replaced by AI? Radiology 2018; 287:365–366. [DOI] [PubMed] [Google Scholar]
- 7.Yasaka K, Akai H, Abe O, et al. Deep learning with convolutional neural network for differentiation of liver masses at dynamic contrast enhanced CT: A preliminary study. Radiology 2018; 286:887–896. [DOI] [PubMed] [Google Scholar]
- 8.Rajpurkar P, Irvin J, Ball RL, et al. Deep learning for chest radiograph diagnosis: a retrospective comparison of CheXNeXt to practicing radiologists. PLoS Med 2018; 15:e1002686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grace K, Salvatier J, Dafoe A, et al. When will AI exceed human performance? Evidence from AI experts. Available at: https://arxiv.org/pdf/1705.08807.pdf (accessed 25 December 2018).
- 10.Darcy AM, Louie AK, Roberts LW. Machine learning and the profession of medicine. JAMA 2016; 315:551–552. [DOI] [PubMed] [Google Scholar]
- 11.Coiera E. The fate of medicine in the time of AI. Lancet 2018; 392:2331–2332. [DOI] [PubMed] [Google Scholar]
- 12.Artificial intelligence in healthcare: within touching distance. Lancet 2017;390:2739. [DOI] [PubMed]
- 13.Kakadiaris IA, Vrigkas M, Yen AA, et al. Machine learning outperforms ACC/AHA CVD risk calculator in MESA. J Am Heart Assoc 2018; 7:e009476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Royal College of Radiologists (RCR) Census Report 2017. Available at: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr185_cr_census_2017.pdf (accessed 26 December 2018).
- 15.Google’s AlphaGo AI wins three – match series against the world’s best Go player. Available at: https://techcrunch.com/2017/05/24/alphago-beats-planets-best-human-go-player-ke-jie/?guccounter=1 (accessed 26 December 2018).
- 16.Galeon D. For the first time, a robot passed a medical licensing exam. Available at: https://futurism.com/first-time-robot-passed-medical-licensing-exam (accessed 26 December 2018).
- 17.Yasaka K, Akai H, Kunimatsu A, et al. Deep learning with convolutional neural network in radiology. Jpn J Radiol 2018; 36:257–272. [DOI] [PubMed] [Google Scholar]