Abstract
Background:
Muscle energy technique (MET) and strain–counterstrain (SCS) technique are found to be effective as a sole treatment of acute low back pain (LBP), but the combined effect of these two techniques has not been evaluated.
Objective:
The purpose of this randomized clinical trial was to evaluate the added effect of SCS to MET in acute LBP patients.
Methods:
In this trial, 50 patients were randomly allocated to MET or MET-SCS group to receive the assigned two treatment sessions for two consecutive days. Oswestry disability index (ODI) and Roland Morris disability questionnaire (RMDQ), visual analogue scale (VAS), lumbar range of motion (ROM) were recorded at baseline, after first and second session.
Results:
All the outcome measures showed statistically significant () improvement in both the groups after second session. Between the groups, analysis showed no statistically significant difference () after the first or second session.
Conclusions:
The improvement after second treatment sessions was noted in pain, ROM, and disability in both the groups, but immediate effect was seen only on pain intensity after first treatment session. When compared between the groups, no added effect of SCS to MET was found in reducing pain and disability and increasing lumbar ROM in acute LBP patients.
Keywords: Muscle energy technique, strain counterstrain technique, acute low back pain
Introduction
Low Back Pain (LBP) is defined as tiredness, discomfort, or pain in the low back region, with or without radiating symptoms to one or both lower extremities.1 LBP is an extremely common problem that most people experience at some point in their lives.2 The point prevalence of activity-limiting LBP lasting more than one day is %.3 LBP is the single largest contributor to musculoskeletal disability and causes substantial personal, community and financial burden globally.4-8
LBP is a multifactorial condition which can be associated with risk factors like gender, age, lifestyle, psychosocial profile, physical demands of the workplace, social support, pain perception, etc.9 It may start with an injury and can be exacerbated by factors like deconditioning, psychological issues, other chronic illnesses, genetics and even cultural factors.10 Only 15% of LBP has an identifiable cause while the rest of the 85% is non-specific LBP.11
Approaches use physiotherapy treatment to manage acute LBP by employing a variety of interventions such as exercise involving neuromuscular re-education, resistance training, therapeutic modalities and manual therapy12 to reduce the chances of developing chronic LBP.11 In the field of manual therapy, there are many techniques which include soft tissue mobilization, articulatory techniques, myofascial release techniques, muscle energy techniques (MET), functional techniques and strain–counterstrain technique (SCS) to address somatic dysfunctions associated with LBP.13
MET is a versatile technique traditionally used to address muscular strain, pain, localoedema and joint dysfunction and to improve range of motion (ROM), to relieve muscle tension and increase the strength of the muscle.14,15 It is a direct technique in that the patient, instead of the care provider, supplies the corrective force.16,17 SCS is a technique derived from positional release therapy (PRT) which uses a pain monitor (trigger points, TrP) to find the position of the pain when it is no longer felt at the monitoring point.13,18
MET is found to be effective in reducing lumbopelvic pain as a sole treatment19 and reducing disability in acute LBP when combined with neuromuscular re-education and resistance training.20 MET has also shown to lead to improvement in lumbar and cervical ROM in asymptomatic individuals.21,22 A recent systematic review done on MET concluded that MET is effective in the treatment of LBP, but needs to be compared with other manual therapy interventions.23 A case study on LBP showed that SCS is effective in reducing pain and disability.24 A randomized control trial showed the equal effectiveness of MET and SCS on pain reduction in acute LBP individuals.25 A study on SCS for the treatment of trapezius trigger points found that it can be effectively used to reduce pain and improve cervical ROM.26 SCS alone has no immediate effect in improving cervical ROM, but it was found to be effective when it was combined with other osteopathic techniques including myofascial release, MET, craniosacral treatment and high-velocity low amplitude mobilization.27 It was suggested that it could be combined with other osteopathic techniques like MET to determine its effectiveness in the treatment of conditions, including acute LBP.27
Acute LBP is documented as a substantial cause of disability. While clinicians have found an increased interest in MET for addressing acute LBP, SCS had no effectiveness as a single treatment intervention. We were interested in determining whether SCS along with MET had any added effect in reducing pain and disability and increasing ROM in acute LBP individuals.
The aim of this study is thus to determine the immediate effect of the MET, with and without the employment of the SCS technique, on pain, disability and ROM in patients with acute LBP.
Methodology
The study was approved by the Institutional Ethics Committee, Kasturba Medical College, Manipal Academy of Higher Education, Mangalore.
This study was a randomized clinical trial conducted at tertiary hospitals from June 2014 to March 2015. The sample size of 25 in each group was calculated using 95% confidence level and 80% power from the previous study.19
Inclusion criteria for patients were set based on a previous study of MET on acute LBP.20 These criteria were a symptom duration of weeks, age between 18 and 65 years, initial Oswestry disability index (ODI) score of 20–60% since a majority of patients with acute LBP have been found to have an initial ODI score within this range. Other inclusion criteria such as unilateral symptoms proximal to the knee and no bilateral symptoms were set based on treatment-based classification criteria28 since it provides an evidenced-based framework in the appropriate conservative management of individuals with LBP. The final inclusion criterion was confirmed lumbar dysfunction based on MET structured diagnostic protocol.17 Patients were excluded if they had a history of spinal surgery, spondylolisthesis, lumbar hypermobility, spinal structural deformity, piriformis and sacroiliac (SI) joint dysfunction.
Consultant-diagnosed cases of acute LBP referred for physiotherapy were approached and screened for inclusion and exclusion criteria. The purpose of the study was explained and informed consent was taken from willing patients, after which they were allocated to two groups based on the sequence generated by the computerized randomization method.
The outcome measure chosen for pain intensity was visual analogue scale (VAS) which was a 10 cm long horizontal line with no pain and the worst possible pain at the extremes of the line, ODI version 2.0 as advocated by the original author and the Roland Morris disability questionnaire (RMDQ) were used to measure disability, and lumbar ROM was measured with the BaselineTM Bubble Inclinometer as described by Norkin.29 The pre-treatment baseline data of pain, disability and lumbar ROM were collected by a blinded assessor, who was a physiotherapist but was not involved in the examination or treatment of the patient.
After completion of self-reported outcome measures and lumbar ROM assessment, the patients were examined by another physiotherapist, using a structured MET diagnostic protocol for lumbar spine dysfunction as described by Greenman.17 The diagnostic procedure followed the palpatory assessment of the paired transverse processes of the lumbar spine from caudal to cephalad. The examiner located the lumbar spinous processes and moved his thumbs laterally over the area of the transverse processes. An overall weighted kappa of 0.92 was found for the palpation of nominated lumbar spinal levels.20 The assessment was performed in neutral prone, forward-bent and sphinx positions. The patient was first assessed in neutral prone position, then sphinx position and last in forward bending with patient seated on a stool resting his feet on a floor. If one transverse process was fully posterior in the forward bent position and became symmetrical in the sphinx position, then the patient was diagnosed with extension dysfunction. If one transverse process was more prominent in the sphinx position but became symmetrical in the forward bent position, then the patient was diagnosed with flexion dysfunction. Side-bending dysfunction was diagnosed based on the side of the prominent transverse process. The same physiotherapist gave two treatment sessions for two consecutive days to all the patients. He was not blinded to the treatment groups.
A re-assessment of pain and lumbar ROM was made immediately after the first treatment session and again on the second day of the post-treatment session. ODI and RMDQ were reassessed only at the end of the second treatment session. In post-treatment, all the outcome measurements were taken by an independent assessor blinded to the group allocation.
MET group
Subjects randomized to the MET group received treatment as described by Seffinger13 and Greenman17 either in the erect sitting posture or lateral recumbent position. Large patients were treated in the erect sitting position so that gravity could be used as an assisting activating force while other patients were treated in the lateral recumbent position on the table on the side opposite to their side-bending dysfunction.17 During MET, patient’s trunk was drawn in to certain available lumbar ROM, depending upon the dysfunction, until the barrier was engaged. Dysfunctional barriers such as motion barrier is encountered before the physiologic barrier is reached and it shows distinctive qualities of restriction due to increased myotonus (neuromuscular barrier) which has a consistent elastic quality.
MET in sitting position
The patient was seated on the examination table with arms folded across the chest. The physiotherapist sat opposite the patient’s side-bending dysfunction. One hand of the physiotherapist monitored the vertebral segment being treated. While he placed the axilla of his other arm over the patient’s shoulder, brought his arm in front of the subject and placed the hand under the patient’s axilla. Then the physiotherapist extended or flexed the subject depending on the flexion or extension dysfunction, respectively, by palpating on the vertebral segment being treated with his hand until a barrier was engaged. Then the physiotherapist rotated and side bent the subject towards him until barrier was engaged.
Then the patient was asked to push his/her shoulder toward the ceiling using approximately 30% of his/her effort against the physiotherapist’s unyielding counterforce and to hold this position for 3 s to 5 s. The physiotherapist then re-engaged the barrier by further extending or flexing, rotating and side-bending the patient. The maneuver was repeated 3–5 times with a relaxation of 2 s to 3 s duration in between.
MET in lateral recumbent position
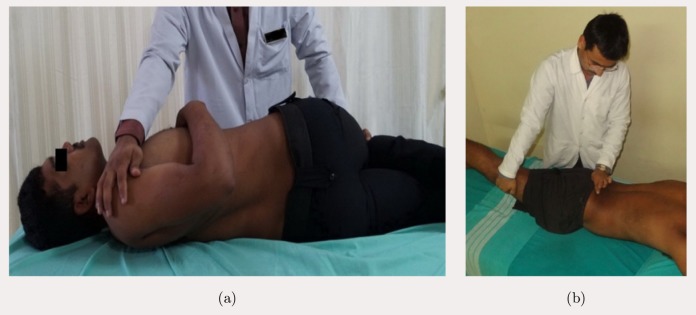
The patient was in the lateral recumbent position on the side opposite to his/her side-bending dysfunction while the physiotherapist stood facing the subject. The physiotherapist monitored the lumbar area with his one hand while with the other hand flexed the subject’s knees and hips until the barrier was engaged at the vertebral segment being treated. For flexion dysfunction, the physiotherapist induced an extension of the spine by pushing hips and knees posteriorly. The patient was then asked to straighten his/her bottom leg, and the foot of the leg positioned above was placed in the bottom leg’s popliteal space. The physiotherapist then palpated the dysfunctional vertebra and then the patient was pulled anteriorly and superiorly from the arm positioned below to introduce a rotation and side-bending of the lumbar spine until the barrier was engaged at the vertebral segment being treated. Then the physiotherapist’s other hand was placed over the upper shoulder of the patient and the patient was asked to push anteriorly with his/her shoulder using approximately 30% of their effort against the physiotherapist’s unyielding counterforce and to hold there for 3 s to 5 s. The physiotherapist then re-engaged the barrier by pulling the patient anteriorly and superiorly from the arm positioned below. The maneuver was repeated for 3–5 times with a relaxation of 2 s to 3 s duration in between (Fig. 1(a)).
Fig. 1.
(a) Muscle energy technique (MET) in lateral recumbent and (b) Strain-counterstrain (SCS) technique.
To treat the side-bending component, the physiotherapist flexed both of the patient’s hips and knees and lifted the ankles toward the ceiling until the barrier was reached. The patient then asked to push his/her ankles toward the floor using approximately 30% of their effort against the physiotherapist’s unyielding counterforce. The barrier was re-engaged by lifting the patient’s ankle further and the maneuver was repeated 3–5 times with a relaxation of 2 s to 3 s duration in between.
MET with SCS technique group
This group of patients was treated with MET as described above. In the SCS, specific distal tender points were localized over the posterior pelvis region of the lumbar spine, and then the position of ease was offered for the tender points till pain was reduced by approximately 70%. Clinically, this was determined by first asking patients to rate their initial tenderness to palpation at tender points at 100%. Then, in order to passively arrive at a position of ease, patients were asked to report if their tenderness was reduced at the same site by approximately 70%. Both perceived tissue tension and the patients’ reported tissue tenderness upon intermittent probing were used to guide the physiotherapist to the appropriate relieving position at tender points. This position was maintained passively for 90 s. The same maneuver was repeated three times with a rest interval of 30 s duration in between (Fig. 1(b)).
Data Analysis
SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. Sociodemographic and clinical characteristics of the participants were summarized with mean, standard deviation and percentages of descriptive statistics of frequency distributions. Data for the lost follow-up patients on the second day were analyzed using intention to treat analysis. value less than 0.05 was considered statistically significant.
A repeated measure ANOVA was used to assess within the group differences from baseline to post-first treatment session and post-second treatment session for VAS and lumbar ROM. Differences between the mean for the time period i.e., baseline to post-first treatment session and baseline to post-second treatment session were calculated using Bonferroni “” test. For within-group analysis of mean difference at baseline and post-second treatment session for ODI and RMDQ student, “” test was used. Independent sample -test was used to see the mean difference between the two groups for all the outcome measures at baseline, immediately post-first treatment session and then after the second treatment session.
Results
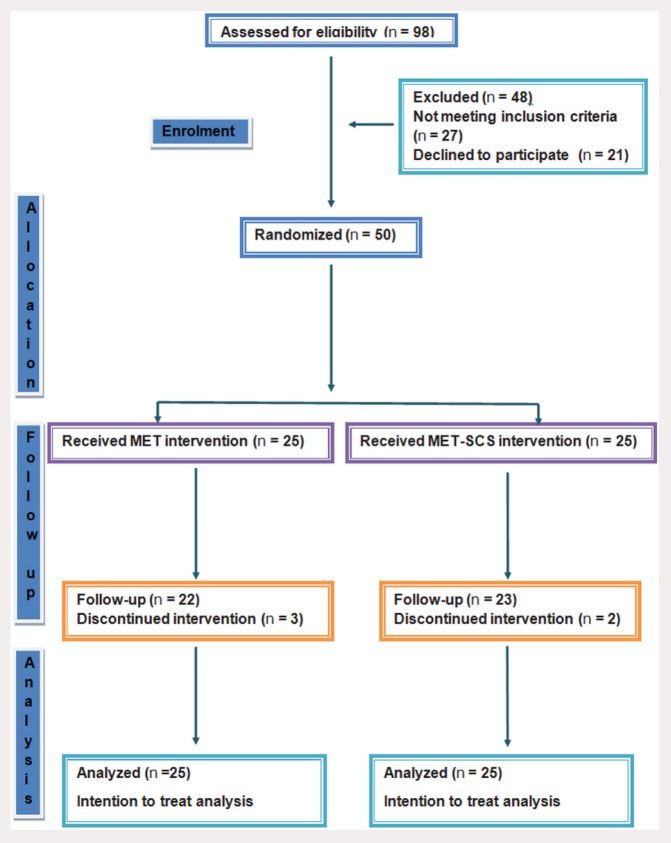
Figure 2 shows the progress of patients at each stage of the study. Gender distribution in both the group was statistically insignificant () with male in MET 18 (72%) and MET-SCS 17 (68%), while female in MET 7 (28%) and MET-SCS 8 (32%). The mean age of participants in MET ( years) and MET-SCS ( years) was statistically insignificant (). The symptom duration of both the MET ( days) and the MET-SCS ( days) group was also statistically insignificant ().
Fig. 2.
Consort flow diagram.
Outcome measures at baseline (Table 1) between the groups were homogenous and not statistically significant.
Table 1.
Outcome measures at baseline.
| Variable | MET (Mean SD) | MET-SCS (Mean SD) | -value |
|---|---|---|---|
| VAS (cm) | 5.28 1.42 | 5.16 1.75 | 0.932 |
| Lumbar flexion (Degrees) | 36.08 12.60 | 30.48 12.30 | 0.148 |
| Lumbar extension (Degrees) | 14.16 6.79 | 13.68 7.70 | 0.536 |
| ODI (%) | 39.00 12.99 | 36.38 11.71 | 0.445 |
| RMDQ | 10.60 5.44 | 6.88 5.46 | 0.491 |
In both the groups, when analysis was done within the group, a statistically significant difference () was seen in VAS and lumbar ROM after the second day post-treatment (Table 2).
Table 2.
Differences of VAS and ROM within the group.
| Variable | Group | Pre-day 1 (Mean SD) | Post-day 1 (Mean SD) | Post-day 2 (Mean SD) | -value | |
|---|---|---|---|---|---|---|
| VAS (cm) | MET | 5.28 1.42 | 4.08 1.65 | 3.08 1.46 | 40.44 | * |
| MET-SCS | 5.16 1.75 | 4.04 1.67 | 3.20 1.84 | 37.44 | * | |
| Flexion (Degrees) | MET | 36.08 12.60 | 37.88 13.31 | 40.44 13.13 | 5.25 | * |
| MET-SCS | 30.48 12.30 | 36.08 14.30 | 35.08 13.34 | 12.58 | * | |
| Extension (Degrees) | MET | 14.16 6.79 | 13.92 9.02 | 18.12 7.56 | 9.37 | * |
| MET-SCS | 13.68 7.70 | 14.48 7.59 | 17.92 7.64 | 10.36 | * |
significant.
Time * group
VAS showed improvement in both the groups after the first day post-treatment. Lumbar extension ROM did not show improvement after the first day post-treatment in any group. But lumbar flexion ROM showed a statistically significant difference in the MET-SCS group, but not in the MET group after first day post-treatment. After second day post-treatment, both groups showed a statistically significant difference on ROM and VAS measures (Table 3).
Table 3.
Differences of VAS and ROM time group.
| Variable | Group | Factors | Mean difference | Std. error | -value | 95% confidence interval |
|---|---|---|---|---|---|---|
| Vas | MET | Pre-day 1 Post-day 1 | 1.20* | 0.25 | 0.001* | 0.55–1.84 |
| Pre-day 1 Post-day 2 | 2.20* | 0.28 | 0.001* | 1.48–2.92 | ||
| MET-SCS | Pre-day 1 Post-day 1 | 1.12* | 0.19 | 0.001* | 0.62–1.62 | |
| Pre-day 1 Post-day 2 | 1.96* | 0.28 | 0.001* | 1.24–2.68 | ||
| Lumbar flexion ROM | MET | Pre-day 1 Post-day 1 | 1.80 | 1.10 | 0.344 | 4.63–1.03 |
| Pre-day 1 Post-day 2 | 4.36* | 1.50 | 0.023* | 8.21–0.51 | ||
| MET-SCS | Pre-day 1 Post-day 1 | 5.600* | 1.14 | 0.001* | 8.54–2.65 | |
| Pre-day 1 Post-day 2 | 4.600* | 1.08 | 0.001* | 7.38–1.81 | ||
| Lumbar extension ROM | MET | Pre-day 1 Post-day 1 | 0.24 | 1.14 | 1.000 | 2.72–3.20 |
| Pre-day 1 Post-day 2 | 3.96* | 1.01 | 0.002* | 6.55–1.37 | ||
| MET-SCS | Pre-day 1 Post-day 1 | 0.80 | 0.86 | 1.000 | 3.01–1.41 | |
| Pre-day 1 Post-day 2 | 4.24* | 1.06 | 0.002* | 6.96–1.51 |
significant.
Disability outcome measures also showed a statistically significant difference () within the groups after the second day post-treatment in both the MET and the MET-SCS group.
When a between groups’ analysis was carried out for all the outcome measures, no statistically significant difference () was noted after the first day and the second day post-treatment (Table 4).
Table 4.
Analyses between MET and MET-SCS groups.
| Variable | MET | MET-SCS | -value | |
|---|---|---|---|---|
| VAS (cm) | Post-day 1 | 4.00, 3.00–5.00 | 4.00, 3.00–4.50 | 0.706 |
| Post-day 2 | 3.00, 2.00–4.00 | 3.00, 2.00–4.00 | 0.889 | |
| Flexion (Degrees) | Post-day 1 | 38.00, 31.00–47.50 | 33.00, 25.50–50.00 | 0.793 |
| Post-day 2 | 40.00, 30.50–50.00 | 40.00, 25.00–48.50 | 0.145 | |
| Extension (Degrees) | Post-day 1 | 13.00, 9.00–17.50 | 15.00, 10.00–18.50 | 0.681 |
| Post-day 2 | 16.00, 14.00–22.50 | 17.00, 12.50–24.50 | 0.992 | |
| ODI (%) | Post-day 2 | 26.00, 15.35–40.00 | 25.00, 19.00–34.44 | 0.907 |
| RMDQ | Post-day 2 | 7.00, 4.00–12.00 | 5.00, 4.00–8.00 | 0.370 |
Discussion
The purpose of the study was to compare the added effect of SCS to MET in treating acute LBP patients. The results showed a significant improvement in both groups in VAS, lumbar ROM, ODI and RMDQ at the end of the treatment. However, no significant difference was seen between the groups.
The hypothesis of this study was generated favoring the MET-SCS group. The result of this study refuted the hypothesis, as there was no statistically significant difference found between groups post-treatment, in respect to VAS, lumbar ROM, ODI and RMDQ.
Pain
At the end of the treatment, the pain scores improved significantly within both groups, but there was no significant difference noted between the groups.
In this study, the MET technique used was post-isometric relaxation stretch procedure for the patient’s group of muscles to lengthen a shortened or contracted muscle, and to mobilize restricted articulation into its proper position.13 The possible hypoalgesic effect can be explained by golgi tendon reflex inhibition, sympathoexcitation evoked by somatic efferents and localized activation of periaqueductal gray matter, which can be produced by muscle and joint proprioception activation.30 The other possible mechanism for the therapeutic effects of MET may involve a variety of biomechanical mechanisms such as the change in tissue fluids, altered proprioceptions, motor programming and control and neurophysiologic responses.31
A number of studies have been carried out in which MET has been used in combination with other modalities or compared with other forms of treatment, but these have given mixed results. These studies have been done in both acute and chronic LBP patients and hence, the results cannot be generalized to acute LBP.
One study has shown greater effectiveness of MET combined with neuromuscular re-education and strength training rather than neuromuscular re-education and strength training alone, in acute LBP patients.20 In another study, MET was compared with a sham technique in the management of lumbopelvic pain, and was found to be effective in reducing pain.19 Another clinical trial concluded that for improvement and reduction in pain, core stability exercises are superior to MET. But in this trial, the groups of LBP patients were heterogeneous and treatment-based classification criteria for manual therapy intervention and stabilization exercise were not followed. Further methodology was not clearly defined.32 MET with interferential therapy (IFT) was found to be better on VAS, ODI and spinal ROM than IFT alone in acute LBP.33 MET has been shown to have a superior effect than transcutaneous electrical nerve stimulation (TENS) in non-specific acute LBP patients.34 In chronic LBP patients, MET and SCS have produced similar effects after four weeks of intervention.35
In another study treating SI joint dysfunction, MET was found to be equally effective as SI joint manipulation,36 but more effective than TENS.37 When used in adjunct to conventional physiotherapy, MET has also been found to be effective in reducing pain in other joints like those of the shoulder,38,39 the knee,40 temporomandibular joint41 and the cervical spine.30,31,42
To the best of our knowledge, this is the first study which compared the added effect of SCS to MET. The results showed that adding SCS to MET did not have any beneficial immediate effect on VAS. In this study, we have followed the therapeutic approach advocated by MET authors, something that was not followed by many previously mentioned studies using MET for the treatment of acute LBP.37
When the SCS technique was used in the treatment of LBP, it showed immediate pain relief, but there was no short-term (24–72 h) effect on pain.24 Similar results were also shown in our study. Another study which combined SCS with exercise in acute LBP did not show any added effect.43 When SCS and MET were used in the treatment of acute LBP, both were found to be equally effective in reducing pain after eight days of intervention.25 SCS shows no better improvement than the sham protocol in the treatment of cervical tender points.44 However, SCS is proved to be more effective in the upper trapezius latent trigger points than ultrasound.45 Large effect size was noted in terms of active mouth opening and pressure pain threshold when SCS was used for masseter muscle trigger points.46
Range of motion
Lumbar flexion ROM showed significant difference immediately after the first treatment session in the MET-SCS group, but not for the lumbar extension ROM. After the second treatment session, both the MET and the MET-SCS group showed significant improvement for lumbar ROM. However, no difference between the groups was seen in the ROM at the end of the second treatment session.
The reason for the immediate improvement could be the combined action of MET and SCS. It could be that MET produced reflex muscle relaxation and lengthened the shortened muscle of the back and improved joint function.30 Post-isometric relaxation could have activated the golgi tendon organ and inhibited the influence on the motor neuron pool.31 Improved ROM can also be attributed to a change in the viscoelastic property and change in stretch tolerance.47
According to the proprioceptive theory, altered neurophysiologic regulation can lead to aberrant activity of agonist and antagonist muscle spindles. In the SCS technique by passively shortening dysfunctional agonist muscle, its spindle activity can be reset and aberrant neuromuscular activity can be reduced. This may be caused by altered neurophysiologic regulation. It is also proposed to be effective because it improves local blood circulation influenced by the sympathetic nervous system. SCS may also affect muscle-ligament reflex by reducing the strain over the ligament which, in turn, reduces muscle excitability.48
MET was found to be effective in improving the overall trunk rotation ROM in asymptomatic volunteers.49 MET and positional release therapy both showed lumbar extension ROM improvement when given along with a moist heat pack in acute LBP individuals.43
Disability questionnaire
The two groups showed a significant difference in ODI and RMDQ scores. Reduced pain and improved ROM might be the reason for a reduction in disability. Both outcome measures have been found to be used widely for clinical trials to document LBP-associated disability. In this study, ODI was administered as a tool for inclusion criteria and also as an outcome measure to determine the effectiveness of the treatment. RMDQ is found to be used to monitor short-term effects of intervention in mild to moderate LBP. Patients who have a disability score of 20–60% on ODI are found to be more suited for MET intervention.19 A change in the ODI score in our study was found to be 5.84 points which falls in the range of minimum detectable change (MDC) of 4–10 points in the literature.28 The minimal clinically important difference (MCID) values for RMDQ depend on the initial score of the patients. The MCID values are calculated in five subgroups i.e., 0 to 8 (MCID 2), 5 to 12 (MCID 4), 9 to 16 (MCID 5), 13 to 20 (MCID 8) and 17 to 24 (MCID 8).50 In our study the MCID value could not be achieved (it was 2.92 as against the value of 4 required for a 5–12 initial score of RMDQ).50 This could probably be owing the number of treatment sessions being restricted to two. A greater number of treatment sessions may be required to achieve a clinically significant difference. Hence, future studies should be done over a longer period of time to get clinically significant results in the treatment of acute LBP.
Limitation
The SCS intervention procedures used in this study did not conform to the general treatment guidelines recommended by SCS technique proponents such as tender points located anteriorly in the abdominal and pelvic regions. The therapist had no control over the patients’ pain medications.
Conclusion
Examination of the results revealed no added effect of SCS to MET in acute LBP patients. Immediately following one treatment session, the effect of MET was determined for pain and disability, but not for lumbar ROM. While MET-SCS showed a reduction in pain and disability and an increase in lumbar flexion ROM immediately upon one treatment session, it did not display the same for lumbar extension ROM. Both MET and MET-SCS showed improvement in all the outcome measures after the second day, post-treatment. When a comparison was drawn between the groups, both the MET and MET-SCS groups were found to be equally benefitted in terms of a reduction of pain and disability. An increase in lumbar ROM was observed in acute LBP patients following the two treatment sessions.
Conflict of Interest
The authors have no conflict of interest relevant to this paper.
Funding/Support
Partial financial support was provided by Manipal Academy of Higher Education for the work discussed in this paper.
Author Contributions
All authors contributed to the study design. Data were collected by Vivek D Patel. Data analysis and interpretation, and writing of the manuscript were carried out by Vivek D Patel, Dr. Charu Eapen and Mr. Zulfeequer CP, with the revision of the manuscript by all the authors.
References
- 1. Jacobs P, Golmohammadi K. The Cost of Low-Back Pain: A Review of the Literature. Alberta: Health Services Utilization and Outcomes Commission of Alberta, 2003. [Google Scholar]
- 2. Anderson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354(9178):581–5. [DOI] [PubMed] [Google Scholar]
- 3. Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of LBP. Arthritis Rheumatol 2012;64(6):2028–37. [DOI] [PubMed] [Google Scholar]
- 4. Anderson GB. Epidemiology of LBP. Acta Orthop Scand Suppl 1998;28:28–31. [DOI] [PubMed] [Google Scholar]
- 5. Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing 2006;35:229–34. [DOI] [PubMed] [Google Scholar]
- 6. Rapoport J, Jacobs P, Bell NR, Klarenbach S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can 2004;25:13–21. [PubMed] [Google Scholar]
- 7. Deyo RA, Cherkin D, Conrad D, Volinn E. Cost, controversy, crisis: LBP and the health of the public. Annu Rev Public Health 1991;12: 141–56. [DOI] [PubMed] [Google Scholar]
- 8. Coste J, Delecoeuillerie G, Cohen de Lara A, et al. Clinical course and prognostic factors in acute LBP: An inception cohort study in primary care practice. BMJ 1994;308:577–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schneider S, Randoll D, Buchner M. Why do women have back pain more than men? A representative prevalence study in the federal republic of Germany. Clin J Pain 2006;22:738–47. [DOI] [PubMed] [Google Scholar]
- 10. Goertz M, Thorson D, Bonsell J, et al. Institute for Clinical Systems Improvement. Bloomington: Adult Acute and Subacute Low Back Pain, 2012. [Google Scholar]
- 11. Patel AT, Ogle AA. Diagnosis and management of acute LBP. Am Fam Physician 2000;61(6): 1779–86. [PubMed] [Google Scholar]
- 12. Hoehler FK, Tobis JS, Buerger AA. Spinal manipulation for LBP. JAMA 1981;245:1835–8. [PubMed] [Google Scholar]
- 13. Seffinger MA, Hruby RJ, Evidence-Based Manual Medicine — A Problem-Based Approach. Philadelphia, PA: Saunders Publishing, 2007. [Google Scholar]
- 14. Chaitow L. Muscle Energy Techniques. 3rd ed. Philadelphia, PA: Churchill Livingstone, 2006. [Google Scholar]
- 15. Varghese S. A study on the effectiveness of muscle energy techniques compared to manipulation therapy in chronic low back pain. Int J Latest Res Sci Technol 2012;1(2):D214–7. [Google Scholar]
- 16. Derosa CP, Porterfield JA. A physical therapy model for the treatment of LBP. Phys Ther 1992;72:261–9. [DOI] [PubMed] [Google Scholar]
- 17. Destefano LA. Greenman’s principles of manual therapy. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins, a Wolters Kluwer business, 2011:300–326. [Google Scholar]
- 18. Chaitow L, Wilson E, Morrissey D, Mcpartland J. Positional release techniques. 3rd ed. London: Elsevier health sciences, 2007. [Google Scholar]
- 19. Selkow NM, Grindstaff TL, Cross KM, Pugh K, Hertel J, Saliba S. Short-term effect of muscle energy technique on pain in individuals with non-specific lumbopelvic pain: A pilot study. J Man Manip Ther 2009;17(1):14–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wilson E, Payton O, Donegan-Shoaf L, Dec K. Muscle energy technique in patients with acute LBP: A pilot clinical trial. J Orthop Sports Phys Ther 2003;33:502–12. [DOI] [PubMed] [Google Scholar]
- 21. Schenk RJ, Adelman K, Rousselle J. The effects of muscle energy technique on cervical range of motion. J Man Manip Ther 1994;2:149–55. [Google Scholar]
- 22. Schenk RJ, Macdiarmid A, Rousselle J. The effects of muscle energy technique on lumbar range of motion. J Man Manip Ther 1997;5:179–83. [Google Scholar]
- 23. Joseph MD, Arthur JN. The effect of muscle energy technique on disability and pain scores in individuals with LBP. J Sport Rehabil 2012;21(2):194–8. [DOI] [PubMed] [Google Scholar]
- 24. Lewis C, Flynn TW. The use of strain–counterstrain in the treatment of patients with LBP. J Man Manip Ther 2001;2:92–8. [Google Scholar]
- 25. Naik PP, Heggannavar A, Khatri SM. Comparison of muscle energy technique and positional release therapy in acute low back pain–RCT. Indian J Physiother Occup Ther 2010;4(2):32–6. [Google Scholar]
- 26. Sheikh SA, Chorsiya V. Strain–counterstrain technique for immediate relief of trapezitis in sitting job professionals. Int J Sci Res 2013;2(6): 411–2. [Google Scholar]
- 27. Klein R, Bareis A, Schneider A, Linde K. SCS to treat restrictions of the mobility of the cervical spine in patients with neck pain — A sham-controlled randomized trial. Complement Ther Med 2013;21:1–7. [DOI] [PubMed] [Google Scholar]
- 28. Burns SA, Foresman E, Kraycsir SJ, Egan W, Glynn P, Mintken PE, Cleland JA. A treatment-based classification approach to examination and intervention of lumbar disorders. Sports Health 2011;3(4):362–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 4th ed. Philadelphia, PA: F. A. Davis Company, 2009. [Google Scholar]
- 30. Yadav H. Goyal M. Efficacy of muscle energy technique and deep neck flexors training in mechanical neck pain — a randomized clinical trial. Int J Ther Rehabil Res 2015;4(1):52–66. [Google Scholar]
- 31. Mahajan R, Kataria C, Bansal K. Comparative effectiveness of muscle energy technique and static stretching for treatment of subacute mechanical neck pain. Int J Health Rehabil Sci 2012;1(1): 16–21. [Google Scholar]
- 32. Narain A, Singh J, Bhowmik S. To compare the effect of core stability exercises and muscle energy techniques on low back pain patients. IOSR J Sports Phys Educ 2013;1(2):9–15. [Google Scholar]
- 33. Patil PN, Basavaraj C, Metgud S, Khatri S. Effectiveness of muscle energy technique on quadrates lumborum in acute low back pain — randomized controlled trial. Indian J Physiother Occup Ther 2010;4(1):54–8. [Google Scholar]
- 34. Franke H, Fryer G, Ostelo RWJG, Kamper SJ. Muscle energy technique for non-specific low-back pain. The Cochrane Database Syst Rev 2015;27(2):CD009852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ellythy MA. Efficacy of muscle energy technique versus strain counter strain on low back dysfunction. Bull Fac Phys Ther 2012;17(2):29–35. [Google Scholar]
- 36. Sharma D, Sen S. Effects of muscle energy technique on pain and disability in patients with SI joint dysfunction. Int J Physiother Res 2014; 2(1):305–11. [Google Scholar]
- 37. Mullai D, Sareen A, Arora T. Comparative analysis of muscle energy technique and conventional physiotherapy in treatment of sacroiliac joint dysfunction. Indian J Physiother Occup Ther 2011; 5(4):127–30. [Google Scholar]
- 38. Moore SD, Laudner KG, McLoda TA, Shaffer MA. The immediate effects of muscle energy technique on posterior shoulder tightness: A randomized controlled trial. J Orthop Sports Phys Ther 2011; 6(4):400–7. [DOI] [PubMed] [Google Scholar]
- 39. Narayan A, Jagga V. Efficacy of muscle energy technique on functional ability of shoulder in adhesive capsulitis. J Exerc Sci Physiother 2014; 10(2):72–6. [Google Scholar]
- 40. Smith M, Fryer G. A comparison of two muscle energy techniques for increasing flexibility of the hamstring muscle group. J Bodyw Mov Ther 2008;12(4):312–7. [DOI] [PubMed] [Google Scholar]
- 41. Rajadurai V. The effect of muscle energy technique on temporo mandibular joint dysfunction: A randomized clinical trial. Asian J Sci Res 2011;4:71–7. [Google Scholar]
- 42. Nambi GS, Sharma R, Inbasekaran D, Vaghesiya A, Bhatt U. Difference in effect between ischemic compression and muscle energy technique on upper trepezius myofascial trigger points: Comparative study. Int J Health Allied Sci 2013;2:17–22. [Google Scholar]
- 43. Lewis C, Souvlis T, Sterling M. Strain-counterstrain therapy combined with exercise is not more effective than exercise alone on pain and disability in people with acute LBP: A randomised trial. J Physiother 2011;57:91–8. [DOI] [PubMed] [Google Scholar]
- 44. Brose SW, Jennings DC, Kwok J, et al. Sham manual medicine protocol for cervical strain–counterstrain research. PM & R 2013;5(5):400–7. [DOI] [PubMed] [Google Scholar]
- 45. Okhovatian F, Mehdikhani R, Naimi SS. Comparison between the immediate effect of manual pressure release and strain–counterstrain techniques on latent trigger point of upper trapezius muscle. Clin Chiropr 2012;15(2):55–61. [Google Scholar]
- 46. Ibáñez-García J, Alburquerque-Sendín F, Rodríguez-Blanco C, et al. Changes in masseter muscle trigger points following strain–counterstrain or neuro-muscular technique. J Bodyw Mov Ther 2009;13(1):2–10. [DOI] [PubMed] [Google Scholar]
- 47. Küçükşen S, Yilmaz H, Sallı A, Uğurlu H. Muscle energy technique versus corticosteroid injection for management of chronic lateral epicondylitis: Randomized controlled trial with 1-year follow-up. Arch Phys Med Rehabil 2013;94(11):2068–74. [DOI] [PubMed] [Google Scholar]
- 48. Wong CK, Straincounter strain: Current concepts and clinical evidence. Man Ther 2012; 17(1):2–8. [DOI] [PubMed] [Google Scholar]
- 49. Lenehan KL, Fryer G, McLaughlin P. The effect of muscle energy technique on gross trunk range of motion. J Osteopath Med 2003;6(1):13–8. [Google Scholar]
- 50. Vela LI, Haladay DE, Denegar C. Clinical assessment of low-back-pain treatment outcomes in athletes. J Sport Rehabil 2011;20(1):74–88. [DOI] [PubMed] [Google Scholar]