ABSTRACT
Objective
To analyze economic evaluations of interventions related to tuberculosis (TB) diagnostics/screening, treatment, and prevention in homeless people.
Methods
A systematic review was conducted. The eligibility criteria were original studies reporting economic evaluation results. The search was not restricted by language or year. A critical appraisal approach was used.
Results
A total of 142 studies were identified, including five research articles (three full economic evaluations and two partial) that were selected for the final review. Most of the studies were conducted in the United States, adopted a public health perspective, and analyzed active TB. Interventions related to diagnostics/screening (the use of interferon-gamma release assay (IGRA) and mobile screening units), treatment (incentives for continuing treatment, and housing programs), and prevention (with the Bacillus Calmette–Guérin (BCG) vaccine) were identified.
Conclusions
No high-quality data were found on cost-effectiveness of interventions on TB diagnostics/screening, treatment, or prevention in homeless people. However, active searching for cases via mobile screening, and financial incentives, could help increase treatment adherence, and the use of IGRA helps boost detection. TB in homeless people is neglected worldwide, especially in developing countries, where this disease tends to afflict more people made vulnerable by their precarious living conditions. Public funding mechanisms should be created to develop cross-sectoral actions targeting homeless people, as the complex dynamics of this group tend to hamper prevention and diagnosis of TB and the completion of TB treatment.
Keywords: Homeless persons, tuberculosis, cost-benefit analysis, review
RESUMEN
Objetivo
Analizar la evaluación económica de intervenciones relacionadas con el diagnóstico y tamizaje, el tratamiento y la prevención de la tuberculosis en las personas sin hogar.
Métodos
Se realizó una revisión sistemática en la cual se usó como criterio de selección estudios originales en los que se presentaran los resultados de una evaluación económica. No se restringió la búsqueda por idioma ni por año. Se usó el enfoque de la evaluación crítica.
Resultados
Se encontraron en total 142 estudios, entre los cuales había cinco artículos de investigación (tres evaluaciones económicas completas y dos parciales) que se seleccionaron para la revisión final. En la mayoría de los estudios, realizados en los Estados Unidos, se adoptó una perspectiva de salud pública y se analizó la tuberculosis activa. Se encontraron intervenciones relacionadas con el diagnóstico y tamizaje (el uso de la prueba de liberación de interferón gamma —IGRA, por su sigla en inglés— y los equipos móviles de tamizaje), el tratamiento (incentivos para continuar el tratamiento y programas de viviendas) y la prevención (el uso de la vacuna BCG).
Conclusiones
No se encontraron datos de calidad alta sobre la costo-efectividad de las intervenciones relacionadas con el diagnóstico o tamizaje, el tratamiento o la prevención de la tuberculosis en personas sin hogar. Sin embargo, la búsqueda activa de casos mediante el uso de equipos móviles para el tamizaje, así como los incentivos financieros, podrían ayudar a aumentar la adhesión al tratamiento; además, el uso de la prueba IGRA ayuda a lograr una mayor detección. La tuberculosis en las personas sin hogar se subestima en todo el mundo, especialmente en los países en desarrollo donde esta enfermedad tiende a afectar a más personas que pasan a ser vulnerables por la precariedad de sus condiciones de vida. Deben crearse mecanismos de financiamiento con fondos públicos para llevar adelante medidas intersectoriales dirigidas a las personas sin hogar, puesto que la compleja dinámica de este grupo tiende a obstaculizar tanto la prevención y el diagnóstico de la tuberculosis como la finalización del tratamiento antituberculoso.
Palabras clave: Personas sin hogar, tuberculosis, análisis costo-beneficio, revisión
RESUMO
Objetivo
Examinar as análises econômicas de intervenções relacionadas à prevenção, detecção precoce/diagnóstico e tratamento da tuberculose (TB) em pessoas sem-teto.
Métodos
Foi realizada uma revisão sistemática. Os critérios para inclusão foram estudo original contendo resultados de análise econômica. A busca não foi restrita por idioma ou ano. Foi usada uma abordagem de análise crítica.
Resultados
Foram identificados ao todo 142 estudos, dentre eles cinco artigos de pesquisa (três análises econômicas completas e duas parciais) que foram selecionados para a revisão final. A maioria dos estudos foi realizada nos Estados Unidos, partindo de uma perspectiva de saúde pública e com análise de TB ativa. Foram identificadas intervenções relacionadas à detecção precoce/diagnóstico (ensaio de liberação de interferon-gama [IGRA] e unidades móveis para prevenção), tratamento (incentivos para o tratamento continuado e programas de moradia) e prevenção (vacinação com o bacilo de Calmette-Guérin [BCG]).
Conclusões
Não foram encontrados dados de alta qualidade sobre o custo-efetividade das intervenções de detecção precoce/diagnóstico, tratamento ou prevenção de TB em pessoas sem-teto. Porém, a busca ativa de casos por meio da triagem em unidades móveis e incentivos financeiros poderiam ajudar a melhorar a adesão ao tratamento e o uso do IGRA intensifica a detecção de infecção. A TB em pessoas sem-teto é uma doença negligenciada em todo o mundo, principalmente nos países em desenvolvimento onde ela costuma afligir um número maior de pessoas por sua vulnerabilidade devido às condições de vida precárias. Mecanismos públicos de financiamento devem ser criados para desenvolver ações intersetoriais voltadas aos sem-teto, porque a dinâmica complexa deste grupo dificulta a prevenção, o diagnóstico e a conclusão do tratamento de TB.
Palavras-chave: Pessoas em situação de rua, tuberculose, análise custo-benefício, revisão
Although significant progress has been made, tuberculosis (TB) remains a major public health problem, affecting 9.0 million people worldwide (1). Even in countries with low and declining case notification at the national level, TB is still a challenge in certain high-risk groups, including homeless people, drug and alcohol users, and migrants (2–4). A meta-analysis of 30 studies, covering a total of 20 554 individuals, identified homelessness as one of the most important risk factors for TB transmission, with an odds ratio of 2.87 (95% confidence interval (CI): 2.05–4.02) for TB among homeless people compared to those who were not homeless (5). Lack of access to medical care among homeless people is associated with late detection of disease progression, poor adherence to treatment, and the emergence of drug resistance (6, 7). These outcomes have a direct impact on health care costs, particularly hospitalization. Homeless persons are more likely to be hospitalized during treatment than people in stable housing, with an adjusted relative risk (RR) of 2.5 (95% CI: 1.5–4.3) (8). The average hospitalization cost for homeless patients has been estimated at US$ 9 834, versus US$ 7 967 for non-homeless patients (9).
The aim of this study was to analyze economic evaluations of interventions related to TB diagnostics/screening, treatment, and prevention among homeless people. Cost-effectiveness evidence can help policymakers make better decisions about resource allocation, improving outcomes and health care efficiency for this vulnerable population.
MATERIALS AND METHODS
Search strategy
A systematic literature search was conducted in Medline, Web of Science, Scopus, Science Direct, Centre for Reviews and Dissemination (CRD)/University of York (UK), and the Cochrane Library in June 2015, followed by an update on 31 August 2016, using the following strategy: (“homeless persons” [MeSH terms] OR “homeless youth” [MeSH terms]) AND (“tuberculosis” [MeSH terms] OR “tuberculosis, pulmonary” [MeSH terms]) AND (“costs and cost analysis” [MeSH terms] OR “economics” [MeSH terms] OR “cost-benefit analysis” [MeSH terms] OR “cost-effectiveness analysis” [MeSH terms] OR “cost-utility analysis” [MeSH terms]), in different combinations. Complementary manual reference searches, and a search for grey literature in the theses and dissertations databases of the Coordination for the Improvement of Higher Education Personnel (CAPES), International Society for Pharmacoeconomics and Outcomes Research (ISPOR), and Brazil's Virtual Health Library in Health Economics (Biblioteca Virtual de Saúde em Economia da Saúde, BVS ECOS), were also carried out. Zotero Standalone (George Mason University, Fairfax, VA, USA) was used to gather, organize, and analyze the retrieved records. The authors developed the review protocol in 2015.
Eligibility criteria
The eligibility criteria were 1) studies that analyzed homeless people; 2) studies that analyzed interventions targeting TB, including diagnostics/screening, treatment, and prevention; and 3) original studies reporting the results of economic evaluations where both costs and outcomes were measured. Exclusion criteria were 1) editorials, letters, and commentaries; 2) reviews; and 3) studies without comparators (i.e., single interventions). The literature search was not restricted by language or date of publication.
Study selection and data extraction
Two researchers (ENS and ACESP) independently reviewed the retrieved studies by analyzing the titles and abstracts. Disagreements were resolved by author consensus or by a third reviewer (FTSE). The author, type of TB, country, year when costs were measured, currency, type of economic evaluation, study perspective, target population, interventions, costs, outcomes, incremental cost-effectiveness ratio (ICER), study conclusion, and sensitivity analysis of each article included in the study were extracted. All costs were converted to U.S. dollars using the exchange rates at the time the study was published.
Quality assessment
The critical appraisal checklist developed by Drummond et al. (10), which consists of 10 questions for assessing the methodological validity of the evidence, was used for the quality assessment.
RESULTS
A total of 142 studies were found (141 in the literature search, and one in the manual searches of the reference lists); 29 duplicates were excluded. After screening the remaining 113 titles and abstracts, 98 studies that did not meet the selection criteria were excluded, leaving 15 studies for full-text assessment. A total of 10 studies were excluded in the full-text assessment (8, 9; 11–18), leaving five studies for analysis in the systematic review (19–23) (Figure 1). No grey literature was found.
FIGURE 1. Flowchart for search, selection, and inclusion of economic evaluations on interventions designed to tackle tuberculosis (TB) in homeless people.
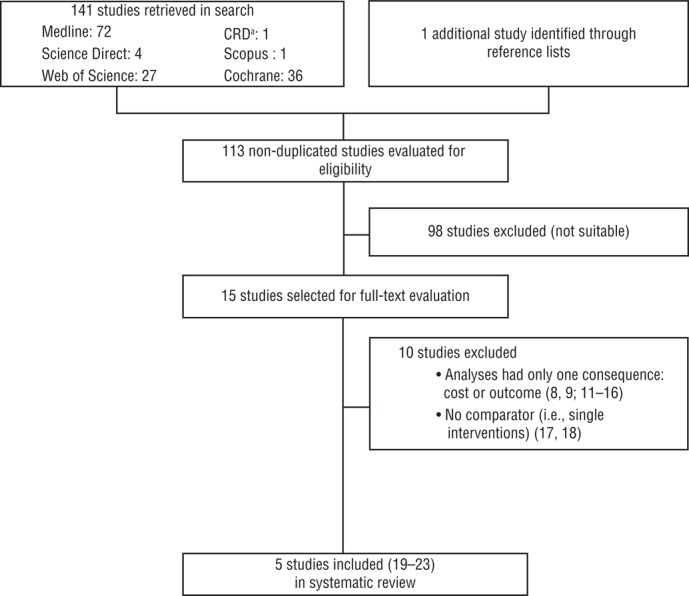
a CRD: Centre for Reviews and Dissemination, University of York (UK).
Source: Compiled by the authors based on the search/selection process for the systematic review.
Three of the five studies included in the review were full economic evaluations (19–21) and two were partial evaluations (22, 23). Most of the five studies were conducted in the United States (20–23), adopted a public health perspective (19–21), and analyzed active TB (19, 21, 23). The earliest study dated back to 1993 (21) and the two most recent were from 2011 (19, 20). All five studies analyzed homeless people with TB, but two of them (19, 20) encompassed a broader target population and covered other social risk factors (Table 1).
TABLE 1. Characteristics of economic evaluations on interventions designed to tackle tuberculosis (TB) in homeless people.
| Study | Type of TB | Country | Year (cost) | Currency | Type of study | Study perspective | Target population |
|---|---|---|---|---|---|---|---|
| Jit et al. (19) | Active | UK | 2010 | British pound | Cost-utility | Health system | Population > 16 years old associated with social risk factors |
| Linas et al. (20) | Latent | USA | 2011 | US$ | Cost-utility | Public health | Homeless and other risk groups |
| Nettleman (21) | Active | USA | Not provided | US$ | Cost-effectiveness | Public health | Homeless people > 35 years old |
| Tulsky et al. (22) | Latent | USA | 1997 | US$ | Cost-consequence | Not provided | Homeless and marginally housed adults |
| LoBue et al. (23) | Active | USA | 1995–1997 | US$ | Cost-consequence | Not provided | Homeless adults at risk of infection |
Source: Compiled by the authors based on the results of the systematic review.
In the critical appraisal, which was based on the checklist from Drummond et al. (10), two studies (19, 20) fulfilled the 10 criteria for high-quality evidence. Lack of 1) information on the measurement and valuation of costs/outcomes, 2) discounting, 3) incremental analyses, and 4) sensitivity analyses were the main issues that impaired the methodological quality of the three other studies included in the review (Table 2).
TABLE 2. Quality assessmenta of economic evaluations on interventions designed to tackle tuberculosis (TB) in homeless people.
| Variable | Jit et al. (19) | Linas et al. (20) | Nettleman (21) | Tulsky et al. (22) | LoBue et al. (23) |
|---|---|---|---|---|---|
| Well-defined question | Yes | Yes | Yes | Yes | Yes |
| Adequate alternatives description | Yes | Yes | Yes | Yes | Yes |
| Evidence of effectiveness | Yes | Yes | No | Yes | No |
| Relevant cost / outcomes | Yes | Yes | No | Yes | Yes |
| Cost/outcomes measured accurately | Yes | Yes | No | No | No |
| Valuation cost / outcomes credible | Yes | Yes | No | No | No |
| Discounting | Yes | Yes | No | Not applicable | No |
| Incremental analysis appropriately reported | Yes | Yes | Yes | No | No |
| Sensitivity analysis reported | Yes | Yes | Yes | No | No |
| Adequate discussion | Yes | Yes | No | No | No |
| Total | 10 | 10 | 4 | 4 | 3 |
Source: Compiled by the authors based on the results of the systematic review.
Based on the Drummond et al. (10) critical appraisal checklist.
The main findings of the five studies were divided into three categories: 1) diagnostics/screening, 2) treatment, and 3) prevention. For diagnostics/screening, evidence was found on mobile screening and on the Mantoux tuberculin skin test (TST) versus the interferon-gamma release assay (IGRA). For treatment, the studies included information on incentives such as supervised housing programs (versus hospitalization) and cash payments (versus noncash incentives). Information for the third category—prevention—was found in a study on the Bacillus Calmette–Guérin (BCG) vaccine.
Diagnostics/screening
Diagnostic/screening interventions were analyzed in the two studies with the highest-quality evidence, based on the Drummond et al. (10) critical appraisal checklist: Jit et al. (19) and Linas et al. (20) (Table 3). The study by Jit et al. focused on an active strategy for detecting TB cases using a mobile screening unit and further engagement via the Find and Treat program (“F ind and Treat service”) in London (19). Implementing the Find and Treat service (mobile screening plus referral to the program) was 5.5 times more costly in terms of direct health care costs than interventions without this service (US$ 2.21 million versus US$ 400 000 respectively). Two major outcomes of using the service were 1) a substantial reduction in loss of follow-up (2.1% versus 17.2% respectively) and 2) improved completion of treatment (67.1% versus 56.8% respectively) (Table 3). The incremental cost-utility ratio (ICUR) was US$ 8 320/quality-adjusted life year (QALY) (ranging from US$ 5 330 to US$ 33 800 per QALY in the sensitivity analysis). The authors of the study concluded that the Find and Treat service was good value for the money given its cost-effectiveness threshold of US$ 26 000–US$ 39 000/QALYs in the United Kingdom. The study by Linas et al. compared screening strategies using TST or IGRA for vulnerable populations in the United States, including homeless people (20). They identified a large variation in the incremental direct health care costs of the IGRA and TST tests, which ranged from a US$ 10.00 savings to a US$ 20.00 cost per person, depending on the risk group (only aggregate costs were reported; no incremental costs were included). Based on the evidence of sensitivity and specificity for both tests, the authors estimated undiscounted life expectancy gains of 0.00–0.01 life months for IGRA screening compared with TST. Meanwhile, IGRA proved better than TST when it came to the number needed to screen to prevent one case of active TB (411 versus 436 respectively) (Table 3). The ICER of IGRA related to TST was US$ 194 300/QALY (ranging from US$ 140 600 to US$ 363 600 per QALY in the sensitivity analysis) (Table 4).
TABLE 3. Costs and outcomes in economic evaluations on interventions designed to tackle tuberculosis (TB) in homeless people.
| Study | Intervention | Cost | Outcome |
|---|---|---|---|
| Jit et al. (19)a | Diagnosis 1. Having no Find and Treat service 2. Having only one part of the service (the mobile screening unit or the case management component) 3. Having both parts of the Find and Treat service |
Direct health care costs: salaries; training and development; travel and subsistence; administration; maintenance; cleaning; insurance; fuel; office management; radiography equipment maintenance; tests; overhead; and TB treatment; including multidrug-resistant patients Total cost: with Find and Treat (US$ 2.21 million); without Find and Treat (US$ 400 000) |
QALYb: patients with no treatment (0.68); after two months of treatment (0.81) Loss to follow-up: Find and Treat service (2.1%); no Find and Treat service (17.2%) Completed treatment: Find and Treat service (67.1%); no Find and Treat service (56.8%) |
| Linas et al. (20) | Diagnosis (screening) 1. No screening 2. Using TSTc to screen 3. Using IGRAd to screen |
Direct health care costs: TST and IGRA screening; diagnostic; physician and nurse visits; drugs; hospitalization; DOTe; contact tracing Compared with TST screening, IGRA resulted in incremental costs ranging from a savings of US$ 10 to a cost of US$ 20. |
Sensitivity: TST (89%); IGRA (83%) Specificity: TST (92%–98%); IGRA (99%) Number needed to screen to prevent one case of active TB: TST (436); IGRA (411) Life expectancy: compared with TST screening, IGRA resulted in undiscounted life expectancy gains of 0.00–0.01 life months. QALY: cured (1.0); nonfatal isoniazid hepatitis (0.85); active TB (0.8) |
| Nettleman (21) | Prevention 1. No vaccination 2. BCGf vaccination |
Direct health care costs: vaccine and side effects; diagnostic tests; hospitalizations; outpatient visits; drug therapy, including TB-resistant; cost of testing and treating close contacts Cost per case of active TB: US$ 7 526 |
Efficacy of BCG vaccination in preventing TB: 8%–100% At an efficacy of 50%, approximately one life would be saved, 12 life years would be gained, and 23 cases of active TB would be prevented for every 1 000 persons entering the vaccination program. |
| Tulsky et al. (22) | Treatment (incentive for adhering to treatment) 1. Cash incentive (US$ 5 payment); noncash incentive (fast food or grocery coupons, phone cards, or bus tokens, with a face value of US$ 5) |
Direct health care costs: incentives (US$ 5), staff time, cost of rent, office supplies, phone lines, and personalized letter Total cost of incentive-enhanced DOPTg was US$ 460.98 per participant in the cash incentive group and US$ 494.45 in the noncash incentive group. |
Completion of preventive therapy: cash incentive group (89%); noncash incentive group (81%), with P = 0.23 Median and mean follow-up hours were 0.5 and 2.0 in the cash incentive group compared to 1.7 and 4.5 in the noncash incentive group. |
| LoBue et al. (23) | Treatment (housing program) 1. Housing for homeless people 2. Hospitalization |
Direct health care costs: health staff, treatment, drug, DOT, hospitalization Cost per day: housing program (US$ 55.90); hospital (US$ 651) Projected total cost saving of housing program: US$ 27 034.54 per patient |
Completion of therapy: 84.6% to 100% |
Source: Compiled by the authors based on the results of the systematic review.
British pounds were converted to US$ using an exchange rate of £ 1 = US$ 1.30.
QALY: quality-adjusted life years.
TST: [Mantoux] tuberculin skin test.
IGRA: interferon-gamma release assay.
DOT: Directly Observed Therapy.
BCG: Bacillus Calmette–Guérin vaccine.
DOPT: Directly Observed Prevention Therapy.
TABLE 4. Analysis and interpretation of results from economic evaluations on interventions designed to tackle tuberculosis (TB) in homeless people.
| Study | ICERa | Study conclusion | Sensitivity analysis |
|---|---|---|---|
| Jit et al. (19)b | ICER of Find and Treat service compared to no Find and Treat service was US$ 8 320/QALYc | Mobile screening unit and case management seem cost-effective | In the most unfavorable scenario, the ICURd would range from US$ 5 330/QALY to US$ 33 800/QALY |
| Linas et al. (20) | ICER: 1) TSTe compared with no screening: US$ 95 000 / QALY 2) IGRAf compared with TST: US$ 194 300/QALY |
Case detection was better by IGRA than by TST but improved case detection resulted in little life expectancy gain because the risk of reactivation TB was small and the rate of isoniazid therapy completion was low. | ICER of IGRA compared with TST ranged from US$ 140 600 to US$ 363 600 per QALY |
| Nettleman (21) | A vaccine with 40% efficacy would result in net savings if provided for persons in homeless shelters. At an efficacy of 50%, capital outlay would be US$ 621 per TB case prevented and US$ 9 100 per life saved. |
If the BCGg vaccine had moderate efficacy, the vaccination of homeless people would be cost-effective. | The vaccination would become dominant if: 1) TB incidence in homeless people was 25 times that of the general population; 2) the probability of cases of active infection being found by tracing contacts with active TB was higher than 0.18. |
| Tulsky et al. (22) | Not provided | Incentives are a valuable way of helping people overcome barriers to completing a course of DOPT.h Cash and noncash incentives were equally effective. | Not performed |
| LoBue et al. (23) | Not provided | Data suggest that implementation of a housing program in conjunction with the use of DOTi is effective for improving TB therapy in homeless people. | Not performed |
Source: Compiled by the authors based on the results of the systematic review.
ICER: incremental cost-effectiveness ratio.
British pounds were converted to US$ using an exchange rate of £ 1 = US$ 1.30.
QALY: quality-adjusted life year.
ICUR: incremental cost-utility ratio.
TST: [Mantoux] tuberculin skin test.
IGRA: interferon-gamma release assay.
BCG: Bacillus Calmette–Guérin vaccine.
DOPT: Directly Observed Prevention Therapy.
DOT: Directly Observed Therapy.
Treatment
Two studies investigated treatment strategies—one focusing on incentives for adherence to treatment (22) and the other analyzing a housing program for homeless only (23) (Table 3). The study by Tulsky et al. (22) identified the potential benefits of using incentives to improve the completion of preventive therapy for homeless people. They compared two approaches: 1) cash payment (US$ 5.00) and 2) noncash incentives (fast food or grocery coupons, bus tokens, or phone cards with a face value of US$ 5.00). The noncash costs were slightly higher than the cash incentive (US$ 494.45 versus US$ 460.98 respectively), but no statistically significant difference was found between them in terms of completion of the prevention therapy (Directly Observed Prevention Therapy or DOPT). The authors of the study did not calculate the ICER or the sensitivity analysis (Table 4). The study by LoBue et al. (23) compared two alternative TB treatments for infectious homeless patients in San Diego, California: 1) a supervised housing program and 2) hospitalization until patients were no longer infectious (23). Based on 20 patient records, more than 80% of the patients completed an adequate course of TB treatment, reaching 100% at one site (Bissell House, a detached cottage in a local residential complex, where they were isolated from the community). The direct costs were almost 10 times higher in the hospitalization scenario than in the housing program (US$ 651.00 versus US$ 55.90 respectively), corresponding to a projected cost savings of US$ 27 034.54 per patient if the housing program were adopted instead of hospitalization. The main limitations of this study were related to the small number of patients and the absence of some methodological steps, such as calculation of the incremental ratio between costs and outcomes, and sensitivity analysis.
Prevention
The fifth study by Nettleman (21) analyzed prevention (the efficacy of the BCG vaccine in preventing active TB in homeless people over 35 years old). The author considered a broad range of assumed levels of efficacy of the BCG vaccination (8%–100%) and found that if it were 50% effective approximately 23 cases of active TB would be prevented for every 1 000 persons entering the vaccine program, resulting in a cost of US$ 621.00 per case of TB prevented. The main problem with this study was the absence of high-quality evidence, according to the checklist criteria from Drummond et al. (10), on the efficacy of BCG vaccination in preventing active cases of TB.
DISCUSSION
This systematic review included five economic assessments of TB interventions among the homeless that covered: 1) diagnosis/screening (19, 20) (IGRA and mobile screening); 2) treatment (22, 23) (incentives for adherence to treatment and housing programs); and 3) prevention (21) (the BCG vaccine). No robust evidence was found on the cost-effectiveness of the five interventions analyzed because: 1) so few studies of these types of interventions have been carried out, with only one study found for prevention); 2) the relevant studies have only been carried out in developed countries (the United States and the United Kingdom); and 3) the methodology used in three of the five studies that met the inclusion criteria was not of high quality (21–23).
One factor neglected in the five studies was investigation of contacts of homeless persons with TB. This is probably due to the high numbers of individuals who share or transit through homeless spaces, hampering identification, localization, and follow-up of contacts for transmission control (24, 25). High-income countries have identified this as a priority issue for controlling the disease (26).
Interventions for homeless people with TB in developed countries
Only two countries have undertaken economic evaluations of interventions targeting TB in homeless people: the United States and the United Kingdom. There are an estimated 650 000 homeless people in the United States and about 380 000 in the United Kingdom. The two countries' homeless populations combined account for about 1% of the total global homeless population (27).
Of the five studies included in this systematic review, two were carried out in the 2010s (19, 20); the others are from previous decades (21–23). The increasing focus on TB in homeless people is due to the high incidence of the disease in this population group. In the United States, TB is 10 times more prevalent in homeless people than in the general population (7), while in the United Kingdom the disease is 29 times more prevalent among homeless people than in the general public (28). According to Zenner et al., many countries have cut their investments in TB control programs because of the low prevalence of the disease in the population at large, but this has only heightened the problem of TB among vulnerable population groups, including homeless people (16).
Interventions for homeless people with TB in developing countries
No studies with economic assessments of efforts to tackle TB in homeless people in developing countries were found. Generally speaking, programs in such countries tend to focus on the whole population, with an eye to meeting the Millennium Development Goals (MDGs) and, more recently, the Sustainable Development Goals (SDGs). Homeless people are not mentioned explicitly in either the MDG or SDG program (29).
As available data about TB in homeless are scarce, the authors of this review were not able to determine a reliable profile of epidemiological and demographic characteristics for this population in developing countries. In the city of São Paulo (Brazil), TB incidence for 2015 was 51.1/100 000 people in the general population and 4 389/100 000 people in the homeless population (30). Nonadherence to treatment was 2.83 times higher in the homeless population than in the general population (40.5% versus 14.3% respectively) in São Paulo (31).
Although there are no economic evaluations of interventions for homeless people in Brazil, the country has had specific programs for this population group since 2011, conducted by the Consultório na Rua (“Street Consultancy”) teams, part of the primary health care service (32). These programs are basically mobile health units staffed by health workers who go out on the streets to meet, build rapport with, and provide guidance for homeless people (33, 34). As they go about their work, these professionals ask the people about their life history, education, official documents, and health and welfare needs (35). This strategy has been seen as promising for improving the health of this vulnerable population group. It would therefore be worthwhile to analyze these programs' costs and health outcomes in order to determine their cost-effectiveness.
Research and policy implications
Policies designed to address TB in homeless people should prioritize cross-sectoral measures involving social services, the health system, and income generation and educational opportunities. Implementing these three types of initiatives together tends to yield better results, for the same amount of resources, than implementing them separately. The ultimate goal is to not only cure the disease but also help people overcome their vulnerable status.
Strengths and limitations
This systematic review was carried out according to high-quality methodological standards, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, but it had some limitations. The first was related to the broad research question, which covered diagnostics/screening, treatment, and prevention of TB in the homeless. A broad research question was used because the authors only expected to find a few studies on each of the three types of TB interventions, given that both TB and homeless people are a neglected topic in the literature. As stated in PRISMA (36), broad questions might increase the applicability of the results and facilitate detection of bias, exploratory analyses, and sensitivity analyses. Second, the number of identified studies was insufficient for conducting a meta-analysis; only one study was found for each health technology. Third, the strength of recommendations to health practice depends on the quality of included articles (37). As mentioned above, the studies available in the literature on interventions targeting TB in homeless people are limited and mostly of low quality. However, these results enabled the authors to map gaps in this field and suggest future exploratory analysis that could help support additional policy and research. Finally, the five studies had some gaps in terms of scope, including 1) their lack of estimated costs and health outcomes of cases of contagion via contact with homeless people and 2) their lack of methodologies that include equity in the economic evaluations, especially for vulnerable population groups.
The authors of this review recommend that future studies on TB in homeless people take these issues into account. Given that interrupting further transmission between contacts tends to improve the cost-effectiveness of interventions, studies that identify and measure cases of contagion among contacts of homeless people would be useful. Including some type of health equity measure to adjust for differences in resource distribution when conducting evaluation among highly vulnerable population groups would help enable more equitable distribution of health care services.
Conclusions
While no high-quality evidence was found on the cost-effectiveness of interventions designed to diagnose/screen for, treat, or prevent TB in homeless people, the results of this review indicate that 1) active searching for cases via mobile screening and financial incentives could help increase the chances of TB treatment completion and 2) IGRA could help boost the detection of cases of TB. The results also show that TB in homeless people is neglected worldwide, especially in developing countries, where this disease tends to afflict more people made vulnerable by their precarious living conditions. Funding mechanisms should be created to develop cross-sectoral actions targeting homeless people, as the complexity of the dynamics of this population group tends to hamper the prevention and diagnosis of the disease and the completion of treatment.
Footnotes
Suggested citation Silva EN, Pereira ACES, Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Rev Panam Salud Publica. 2018;42:e40. https://doi.org/10.26633/RPSP.2018.40
Disclaimer. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH or the Pan American Health Organization (PAHO).
REFERENCES
- 1.World Health Organization . Global tuberculosis report 2014. Geneva: WHO; 2014. Available from: http://apps.who.int/medicinedocs/en/d/Js21634en/ [Google Scholar]
- 2.de Vries G, Aldridge RW, Cayla JA, Haas WH, Sandgren A, van Hest NA, et al. Epidemiology of tuberculosis in big cities of the European Union and European Economic Area countries. Euro Surveill. 2014;19(9) doi: 10.2807/1560-7917.es2014.19.9.20726. pii: 20726. [DOI] [PubMed] [Google Scholar]
- 3.de Vries G, van Hest NA, Baars HW, Sebek MM, Richardus JH. Factors associated with the high tuberculosis case rate in an urban area. Int J Tuberc Lung Dis. 2010;14(7):859–865. [PubMed] [Google Scholar]
- 4.Marx FM, Fiebig L, Hauer B, Brodhun B, Glaser-Paschke G, Magdorf K, et al. Higher rate of tuberculosis in second generation migrants compared to native residents in a metropolitan setting in Western Europe. PLoS One. 2015;10(6):e0119693. doi: 10.1371/journal.pone.0119693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nava-Aguilera E, Andersson N, Harris E, Mitchell S, Hamel C, Shea B, et al. Risk factors associated with recent transmission of tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2009;13(1):17–26. [PubMed] [Google Scholar]
- 6.Goetsch U, Bellinger OK, Buettel KL, Gottschalk R. Tuberculosis among drug users and homeless persons: impact of voluntary X-ray investigation on active case finding. Infection. 2012;40(4):389–395. doi: 10.1007/s15010-011-0238-x. [DOI] [PubMed] [Google Scholar]
- 7.Bamrah S, Yelk Woodruff RS, Powell K, Ghosh S, Kammerer JS, Haddad MB. Tuberculosis among the homeless, United States, 1994–2010. Int J Tuberc Lung Dis. 2013;17(11):1414–1419. doi: 10.5588/ijtld.13.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor Z, Marks SM, Ríos Burrows NM, Weis SE, Stricof RL, Miller B. Causes and costs of hospitalization of tuberculosis patients in the United States. Int J Tuberc Lung Dis. 2000;4(10):931–939. [PMC free article] [PubMed] [Google Scholar]
- 9.Marks SM, Taylor Z, Burrows NR, Qayad MG, Miller B. Hospitalization of homeless persons with tuberculosis in the United States. Am J Public Health. 2000;90(3):435–438. doi: 10.2105/ajph.90.3.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005. [Google Scholar]
- 11.Stevens A, Bickler G, Jarrett L, Bateman N. The public health management of tuberculosis among the single homeless: is mass miniature x ray screening effective? J Epidemiol Community Health. 1992;46(2):141–143. doi: 10.1136/jech.46.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bothamley GH, Rowan JP, Griffiths CJ, Beeks M, McDonald M, Beasley E, et al. Screening for tuberculosis: the port of arrival scheme compared with screening in general practice and the homeless. Thorax. 2002;57(1):45–49. doi: 10.1136/thorax.57.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman R, Kato-Maeda M, Hauge KA, Horan KL, Oren E, Narita M, et al. Use of rapid genomic deletion typing to monitor a tuberculosis outbreak within an urban homeless population. J Clin Microbiol. 2005;43(11):5550–5554. doi: 10.1128/JCM.43.11.5550-5554.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bocchino M, Greco S, Rosati Y, Mattioli G, Marruchella A, De Mori P, et al. Cost determinants of tuberculosis management in a low-prevalence country. Int J Tuberc Lung Dis. 2006;10(2):146–152. [PubMed] [Google Scholar]
- 15.Rubado DJ, Choi D, Becker T, Winthrop K, Schafer S. Determining the cost of tuberculosis case management in a low-incidence state. Int J Tuberc Lung Dis. 2008;12(3):301–307. [PubMed] [Google Scholar]
- 16.Zenner D, Southern J, van Hest R, DeVries G, Stagg HR, Antoine D, et al. Active case finding for tuberculosis among high-risk groups in low-incidence countries. Int J Tuberc Lung Dis. 2013;17(5):573–582. doi: 10.5588/ijtld.12.0920. [DOI] [PubMed] [Google Scholar]
- 17.Kimerling ME, Shakes CF, Carlisle R, Lok KH, Benjamin WH, Dunlap NE. Spot sputum screening: evaluation of an intervention in two homeless shelters. Int J Tuberc Lung Dis. 1999;3(7):613–619. [PubMed] [Google Scholar]
- 18.Dewan PK, Grinsdale J, Liska S, Wong E, Fallstad R, Kawamura LM. Feasibility, acceptability, and cost of tuberculosis testing by whole-blood interferon-gamma assay. BMC Infect Dis. 2006;6:47–47. doi: 10.1186/1471-2334-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jit M, Stagg HR, Aldridge RW, White PJ, Abubakar I. Find and Treat Evaluation Team. Dedicated outreach service for hard to reach patients with tuberculosis in London: observational study and economic evaluation. BMJ. 2011;343 doi: 10.1136/bmj.d5376. d5376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linas BP, Wong AY, Freedberg KA, Horsburgh CR., Jr. Priorities for screening and treatment of latent tuberculosis infection in the United States. Am J Respir Crit Care Med. 2011;184(5):590–601. doi: 10.1164/rccm.201101-0181OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nettleman MD. Use of BCG vaccine in shelters for the homeless. A decision analysis. Chest. 1993;103(4):1087–1090. doi: 10.1378/chest.103.4.1087. [DOI] [PubMed] [Google Scholar]
- 22.Tulsky JP, Hahn JA, Long HL, Chambers DB, Robertson MJ, Chesney MA, et al. Can the poor adhere? Incentives for adherence to TB prevention in homeless adults. Int J Tuberc Lung Dis. 2004;8(1):83–91. [PubMed] [Google Scholar]
- 23.LoBue PA, Cass R, Lobo D, Moser K, Catanzaro A. Development of housing programs to aid in the treatment of tuberculosis in homeless individuals: a pilot study. Chest. 1999;115(1):218–223. doi: 10.1378/chest.115.1.218. [DOI] [PubMed] [Google Scholar]
- 24.Yun LW, Reves RR, Reichler MR, Bur S, Thompson V, Mangura B, et al. Outcomes of contact investigation among homeless persons with infectious tuberculosis. Int J Tuberc Lung Dis. 2003;7(12 Suppl 3):S405–S411. [PubMed] [Google Scholar]
- 25.Lofy KH, McElroy PD, Lake L, Cowan LS, Diem LA, Goldberg SV, et al. Outbreak of tuberculosis in a homeless population involving multiple sites of transmission. Int J Tuberc Lung Dis. 2006;10(6):683–689. [PubMed] [Google Scholar]
- 26.Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2013;41(1):140–156. doi: 10.1183/09031936.00070812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–870. doi: 10.1016/S1473-3099(12)70177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Story A, Murad S, Roberts W, Verheyen M, Hayward AC. London Tuberculosis Nurses Network. Tuberculosis in London: the importance of homelessness, problem drug use and prison. Thorax. 2007;62(8):667–671. doi: 10.1136/thx.2006.065409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United Nations . Global sustainable development report. New York: UN; 2015. Available from: https://sustainabledevelopment.un.org/globalsdreport/2015. [Google Scholar]
- 30.Município de São Paulo (BR) Boletim TB 2011. São Paulo: MSP; 2011. [Accessed on 10 July 2016.]. Available from: http://www.prefeitura.sp.gov.br/cidade/secretarias/upload/chamadas/boletim_tuberculose2011_1335464303.pdf. [Google Scholar]
- 31.Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia (BR) Síntese de evidências para políticas de saúde: adesão ao tratamento de tuberculose pela população em situação de rua. Brasília: MS; 2016. Available from: http://bvsms.saude.gov.br/bvs/publicacoes/sintese_evidencias_politicas_adesao_tuberculose.pdf. [Google Scholar]
- 32.Hallais JAS, Barros NF. Consultório na Rua: visibilidades, invisibilidades e hipervisibilidade. Cad Saude Publica. 2015;31(7):1497–1504. doi: 10.1590/0102-311X00143114. [DOI] [PubMed] [Google Scholar]
- 33.Silva FP, Frazao IS, Linhares FMP. Práticas de saúde das equipes dos Consultórios de Rua. Cad Saude Publica. 2014;30(4):805–814. doi: 10.1590/0102-311X00100513. [DOI] [PubMed] [Google Scholar]
- 34.Bernardes IA, Antunes FM, Silva JOC, Oliveira ME, Campos SR. Anais do Congresso Internacional de Humanidades & Humanização em Saúde [Blucher Medical Proceedings. 2. Vol. 1. São Paulo: Blucher; 2014. Consultório na Rua: uma nova forma de cuidado em saúde. [DOI] [Google Scholar]
- 35.Santos CS, Franco ACF, Albuquerque ECC, Pereira MSS, Barros MN. Uma análise sobre o atendimento à população em situação de rua no município de Belém/PA: problematizações acerca do serviço de acolhimento institucional; Paper presented at VII Jornada Internacional de Políticas Públicas; São Luis, Brazil. 2015; São Luis: JOINPP; 2015. Available from: http://www.joinpp.ufma.br/jornadas/joinpp2015/pdfs/eixo4/uma-analise-sobre-o-atendimento-a-populacao-em-situacao-de-rua-no-municipio-de-belem.pdf. [Google Scholar]
- 36.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700–b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia (BR) Diretrizes metodológicas: Sistema GRADE – manual de graduação da qualidade da evidência e força de recomendação para tomada de decisão em saúde. Brasília: MS; 2014. Available from: http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_metodologicas_sistema_grade.pdf. [Google Scholar]


