ABSTRACT
The rate of human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) infections among health care workers that is caused by sharps injuries is higher in the Caribbean and Latin America than in other regions of the world. To respond to and reduce occupational exposures to bloodborne pathogens while also strengthening capacities in the Caribbean, needlestick injury prevention training programs for health care workers were implemented, beginning in 2011. The programs included lectures, workshops, policy reviews, evaluations of safety devices, and workplace assessment. During the training, baseline data from health care workers on their personal history of needlestick injuries and bloodborne pathogen exposure was collected. That baseline data showed that 40% of the participants had sustained sharps injuries during their professional career. In this capacity-building effort, 210 health care workers from five countries have been trained, six health care centers in the Caribbean have been evaluated. and occupational safety and health committees have been established in various countries to monitor and improve safety policies and practices.
Keywords: Needlestick injuries, accident prevention, health care surveys, health personnel, West Indies
RESUMEN
La tasa de infecciones por los virus de la inmunodeficiencia humana (VIH), de la hepatitis B (VHB) y de la hepatitis C (VHC) en los trabajadores de atención de salud debidas a heridas por materiales punzocortantes es mayor en América Latina y el Caribe que en otras regiones del mundo. Con objeto de responder a las exposiciones laborales a los agentes patógenos de transmisión sanguínea y reducirlas, además de reforzar las capacidades en el Caribe, se instituyeron programas de capacitación para la prevención de las heridas por pinchazos accidentales en los trabajadores de salud a partir del 2011. Los programas comprendían conferencias, talleres, revisión de las políticas, análisis de los dispositivos de seguridad y evaluación de los lugares de trabajo. Durante la capacitación, se recopilaron datos iniciales suministrados por los trabajadores de atención de salud sobre sus antecedentes personales de heridas por pinchazos accidentales y exposición a agentes patógenos de transmisión sanguínea. Esos datos iniciales indicaron que 40% de los participantes habían sufrido alguna herida por materiales punzocortantes a lo largo de su carrera profesional. En esta iniciativa de formación de capacidades, se han capacitado 210 trabajadores de atención de salud de cinco países, se han evaluado seis centros de atención de salud en el Caribe y se han establecido comités de seguridad y salud ocupacional en diversos países para vigilar y mejorar las normas y prácticas de seguridad.
Palabras clave: Lesiones por pinchazo de aguja, prevención de accidentes, encuestas de atención de la salud, personal de salud, Indias Occidentales
RESUMO
As taxas de infecção pelo vírus da imunodeficiência humana (HIV), vírus da hepatite B (HBV) e vírus da hepatite C (HCV) em profissionais da saúde decorrentes de acidentes com materiais perfurocortantes são mais elevadas no Caribe e na América Latina que em outras regiões do mundo. Para combater e reduzir a exposição ocupacional a patógenos de transmissão sanguínea, igualmente reforçando as competências no Caribe, programas de capacitação em prevenção de acidentes com agulhas para profissionais da saúde foram implementados a partir de 2011. Os programas consistiram de palestras, seminários, análises de políticas, avaliações de dispositivos de segurança e avaliação dos locais de trabalho. Durante a capacitação, foram coletados dados de base dos profissionais da saúde relativos ao histórico pessoal de acidentes com agulhas e exposição a patógenos de transmissão sanguínea. Estes dados indicaram que 40% dos participantes haviam sofrido acidentes com materiais perfurocortantes durante a atividade profissional. Como parte desta iniciativa de capacitação, foi dado treinamento a 210 profissionais da saúde de cinco países, foram avaliados seis centros de saúde no Caribe e instituídos comitês de saúde e segurança ocupacional em diversos países para monitorar e melhorar as políticas e práticas de segurança.
Palavras-chave: Ferimentos penetrantes produzidos por agulha, prevenção de acidentes, pesquisas sobre serviços de saúde, pessoal de saúde, Índias Ocidentais
Unsafe handling of sharps and other health care practices with the potential to introduce infectious agents among health care workers is prevalent in developing countries. Exposures occur under a wide variety of scenarios, as evidenced by various studies (1–4). The rate of human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) infections among health care workers that are caused by sharps injuries is higher in the Caribbean and Latin America than in other regions of the world (5). Of the 35 million health care workers worldwide, approximately 3 million of them experience percutaneous exposure to infectious agents annually. Approximately 90% of occupational exposures that cause severe illness and death occur in developing countries. An estimated 30% of HBV, 31% of HCV, and 5% of HIV infections are linked to sharps injuries. In 2002, 500 000 deaths were caused by unsafe injection practices worldwide (4).
The risk of infection among health care workers depends on various factors. One is an individual's personal characteristics, such as their knowledge and awareness of safety protocols and level of immunity to illness. Another factor is the biological properties of the pathogen, such as the type of pathogen and its contagiousness and infectiousness. A third factor is the frequency and severity of needlestick injury. Another factor is the lack of compliance with safety protocols and access to proper postexposure prophylaxis (6).
To reduce occupational exposures to bloodborne pathogens and build capacities in the Caribbean, a “train-the-trainer” program for health care workers was established. The effort was carried out by three organizations: 1) the Caribbean Program Coordination Office of the Pan American Health Organization/World Health Organization (PAHO/WHO); 2) the United States Centers for Disease Prevention and Control (CDC)/National Institute for Occupational Safety and Health (NIOSH); and 3) the St. George's University Department of Public Health and Preventive Medicine. The program was aimed at five countries in the Caribbean: Grenada (population, 106 825), Saint Lucia (184 999), Saint Vincent and the Grenadines (109 462), Suriname (542 975), and Trinidad and Tobago (1 360 088). This report describes the training and its outcomes.
MATERIALS AND METHODS
WHO developed a number of materials as part of its Protecting Healthcare Workers: Preventing Needlestick Injuries Toolkit (7). In partnership with CDC/NIOSH and PAHO, that program was adapted and modified for Caribbean countries in 2011. As a first step, PAHO, CDC/NIOSH, the Ministry of Health of Grenada, and St. George's University organized a 2.5-day train-the-trainer workshop aimed at establishing a network for occupational safety and health (OSH). The focus of the workshop was to assist Caribbean countries in decreasing occupational exposures to bloodborne pathogens and reducing needlestick accidents by enhancing workforce knowledge and establishing preventative practices in the health care industry. In addition, an emphasis was placed on creating a surveillance network to address prophylactic treatment for health workers who were exposed.
Following the workshop, a two-day train-the-trainer program was developed with the following five objectives:
provide OSH training, knowledge, and skill sets to prevent bloodborne infections
establish OSH committees for health care workers in individual institutions at each participating country in the Caribbean
implement workplace assessments, using PAHO tools
evaluate and assess occupational safety preparedness and procedures and develop recommendations for each country
collect and analyze baseline data on needlestick injury, and establish an occupational health surveillance network for needlestick injuries and bloodborne pathogen exposure
PAHO country representatives and ministry of health officers were invited to participate in this program. Each training activity was facilitated by the recently trained site trainer from the country and two trained instructors from the St. George's University. A two-day training program at each site included lectures, workshops, discussions, site assessment visits, and review of policy and guidelines. The training curriculum included the following topics: epidemiology of bloodborne infections; introduction to hierarchy of controls, including safe medical devices; prevention and control strategies; committee on occupational safety and health for health care workers; postexposure follow-up; and conducting a health care workplace assessment. Under the supervision of trainers, during the practical component, trainees visited various health care facilities to identify risks and hazards for needlestick injuries. Using the standardized assessment tools, an on-the-job assessment of health and safety practices was conducted.
The baseline data on needlestick injuries and bloodborne pathogen exposures from the target countries was collected and analyzed. In collaboration with ministry of health representatives, OSH committees were established in health facilities in each country. Available policies and regulations were assessed, evaluated, and compared with the PAHO guidelines. Results and recommendations were shared with each country's ministerial representatives in order to ensure safe practices and continued training of health care workers.
RESULTS
For the initial workshop in 2011, a total of 35 participants from nine Caribbean territories (Barbados, Belize, British Virgin Islands, Dominica, Grenada, Saint Lucia, Saint Vincent and the Grenadines, Suriname, and Trinidad and Tobago) attended and were trained as trainers. Following this workshop, 210 health care workers from five countries (Grenada, Saint Lucia, Saint Vincent and the Grenadines, Suriname, and Trinidad and Tobago) have been trained, and six health care centers in Caribbean countries have been evaluated. The participants have included health care workers, physicians, veterinarians, dentists, nurses, midwives, occupational health and/or infection control officers, ministry of health representatives, medical and nursing students, and home care workers. Table 1 and Table 2 summarize the data collected and the recommendations for each country, respectively.
TABLE 1. Baseline assessment (number and percentage) of needlestick injury among training workshop attendees in 2011 from five Caribbean countries.
| Characteristic | Grenada (N = 54) | Saint Lucia (N = 32) | Saint Vincent and the Grenadines (N = 41) | Suriname (N = 32) | Trinidad and Tobago (N = 51) |
|---|---|---|---|---|---|
| Attendees who had sustained an injury during their professional career | 6 (11.1%) | 12 (37.5%) | 34 (82.9%) | 20 (62.5%) | 13 (25.5%) |
| Attendees who reported the injury | 6 (11.1%) | 3 (9.38%) | 3 (7.3%) | 20 (62.5%) | 9 (17.6%) |
| Attendees who received treatment | 6 (11.1%) | 2 (6.3%) | 3 (7.3%) | 20 (62.5%) | 9 (17.6%) |
| Attendees aware of health and safety policy within their country at the time of the workshop | 6 (11.1%) | 30 (93.8%) | 14 (34.1%) | 26 (81.3%) | 3 (5.9%) |
Source: Table prepared by the authors based on the results of the study.
TABLE 2. Country-specific and general recommendations on needlestick injury in five Caribbean countries.
| Country-specific/General | Recommendations |
|---|---|
| Grenada | • Locate disposal bins on walls at eye level |
| • Review protocols at the hospital level | |
| Saint Lucia | • Establish policies, protocols, and procedures |
| • Implement safe needle disposal and use protective needles | |
| Saint Vincent and the Grenadines | • Establish policies, protocols, and procedures |
| Suriname | • Standardize safety protocols |
| • Repair uneven floors and eliminate storage in passageways | |
| Trinidad and Tobago | • Make protective equipment available |
| General | • Facilitate cooperation among authorities from the Caribbean countries |
| • Add workshops to cover the remaining health care workers | |
| • Address the practice of recapping of needles | |
| • Make occupational safety and health policies available | |
| • Enforce safety guidelines | |
| • Reorganize and maintain physical work environment for best safety and ergonomic practices | |
| • Enforce policies and procedures to ensure safe handling of hazardous material and infection control/isolation | |
| • Establish psychosocial services |
Source: Table prepared by the authors based on the results of the study.
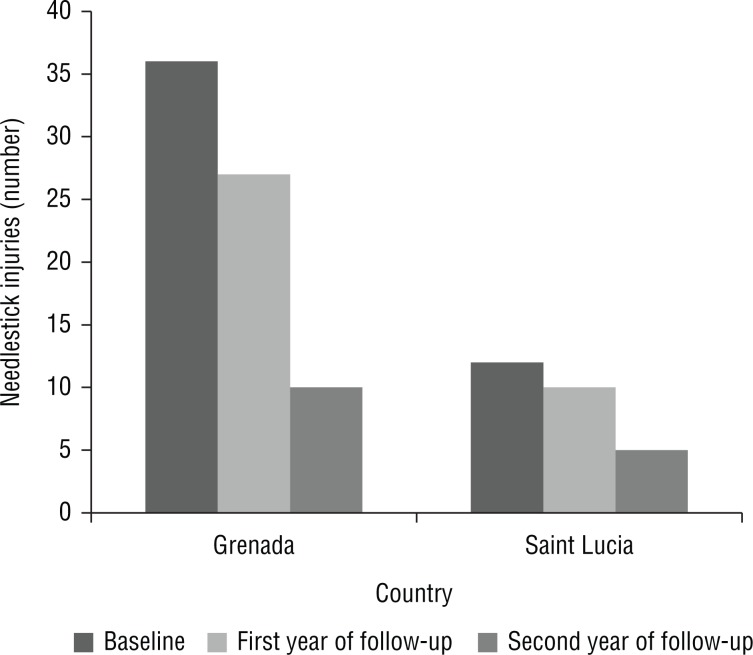
The needlestick injury reporting for Grenada and Saint Lucia was followed up for two years after the training program in 2011 (Figure 1). (Only two countries out of the five were available for this follow-up, as the remaining countries did not share their data.) The baseline data for 2011 from the respective ministry of health showed 36 injuries for Grenada and 12 for Saint Lucia. In 2013, the respective figures were 10 for Grenada (a 72.2% decrease) and 5 for Saint Lucia (a 58.3% decrease).
FIGURE 1. Number of needlestick injuries in the baseline year of training (2011) and the two following years in Grenada and Saint Lucia.
Source: Figure prepared by the authors based on the results of their study.
DISCUSSION
Sharps injuries are the most common cause of occupational exposure to bloodborne pathogens Among our participants, 40% of them had sustained a sharps injury during their professional career.
A study from Trinidad and Tobago found that needlesticks caused 78.6% of the inoculation injuries (8). In Jamaica, about 1.5% of the adult population is HIV-positive and 1% of blood donors are HIV-positive. The risk of contracting HBV from a needlestick injury is between 6% and 30% for a health care worker who has not been not vaccinated against HBV (6). Lack of dexterity in handling needles due to wearing multiple pairs of gloves—which constricts hand motion—is also reported as a contributing factor for inexperienced nurses and medical students (9). In addition, there is an underestimation of the severity of this problem, given that many health care workers do not report their needlestick injuries (6). Our observations confirmed that a surveillance system needs to be in place for proper evaluation and monitoring of needlestick injuries.
The rapid assessment of the various facilities in the Caribbean, using standardized tools, also revealed a lack of effective prophylactic protocols. Measures are needed to prevent infections from health care workers’ occupational exposure to bloodborne pathogens. These steps should include personal practices such as immunization, immediate disposal of used sharps into a nonreusable sharps container, use of safety devices such as protective needles and personal protective equipment, and elimination of unnecessary use of needles and sharps. Other procedures should include such administrative practices as implementing universal precautions, training workers to protect themselves from risks, and promoting prevention of transmission. However, a majority of these health systems do not have sufficient resources or are severely cash-strapped, so they cannot fully implement the necessary protocols.
Health care workers in the Dominican Republic who received two or more training sessions were less likely to experience a needlestick injury (10). Training on sharps-handling techniques increased compliance with some precautionary measures. In addition, combining training with an intervention and use of safety devices may further decrease the number of needlestick injuries (9). After our program training, the two years of follow-up in Grenada and Saint Lucia showed that the reported injuries decreased substantially, indicating the positive impact of the workshop for those two nations.
Conclusions
This work was unique in its global approach to increasing occupational safety and health in the Caribbean. However, a major limitation of the study was that the follow-up was conducted in only two countries. Another limitation is that due to the small sample size for the study, we did not run any statistical analyses. The baseline data demonstrate needlestick injuries are a significant burden in the Caribbean. The lack of knowledge and awareness of needlestick injuries contributes greatly to underreporting and the lack of policies and procedures. Combining training, use of safety equipment, and policy implementation could substantially reduce the burden of needlestick injuries.
Acknowledgments
The authors thank all the individuals from the five Caribbean countries for their participation in the workshop, along with the ministries of health of the five nations for their support, as well as the Pan American Health Organization/World Health Organization and the U.S. Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. The authors would also like to thank Mrs. M. Bartholmae for her help with the literature search.
Footnotes
Suggested citation Akpinar-Elci M, Bidaisee S, Durgampudi P, Radix R, Rodriquez-Guzman J, Nguyen MT, et al. Needlestick injury prevention training among health care workers in the Caribbean. Rev Panam Salud Publica. 2018;42:e93. https://doi.org/10.26633/RPSP.2018.93
REFERENCES
- 1.He L, Lu Z, Huang J, Zhou Y, Huang J, Bi Y, et al. An integrated intervention for increasing clinical nurses’ knowledge of HIV/AIDS-related occupational safety. Int J Environ Res Public Health. 2016 Nov 07;13(11):1094–1094. doi: 10.3390/ijerph13111094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Memon AG, Naeem Z, Zaman A, Zahid F. Occupational health related concerns among surgeons. Int J Health Sci (Qassim) 2016 Apr;10(2):279–291. [PMC free article] [PubMed] [Google Scholar]
- 3.Rice BD, Tomkins SE, Ncube FM. Sharp truth: health care workers remain at risk of bloodborne infection. Occup Med (Lond) 2015 Apr;65(3):210–214. doi: 10.1093/occmed/kqu206. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . The world health report 2002: reducing risks, promoting healthy life. Geneva: WHO; 2002. [Accessed on 3 July 2015]. Available from: http://www.who.int/whr/2002/en/ [Google Scholar]
- 5.Pan American Health Organization . Regional goals for human resources for health 2007–2015. (Working Document CSP27) Washington, D.C.: PAHO; 2007. [Accessed on 13 July 2015]. Available from: http://iris.paho.org/xm-lui/handle/123456789/4157. [Google Scholar]
- 6.Foster TM, Lee MG, McGaw CD, Frankson MA. Prevalence of needlestick injuries and other high risk exposures among healthcare workers in Jamaica. West Indian Med J. 2010 Mar;59(2):153–158. [PubMed] [Google Scholar]
- 7.World Health Organization Protecting Healthcare Workers: Preventing Needlestick Injuries Toolkit. [Accessed on 3 July 2015]. Available from: http://www.who.int/occupational_health/activities/pnitoolkit/en/index5.html.
- 8.Chadee DD, Edwards JR, Sharma K, Shivnath B. Inoculation injuries in hospitals in Trinidad and Tobago. West Indian Med J. 1999 Dec;48(4):227–230. [PubMed] [Google Scholar]
- 9.Higginson R, Parry A. Needlestick injuries and safety syringes: a review of the literature. Br J Nurs. 2013 May 25;22(8) doi: 10.12968/bjon.2013.22.Sup5.S4. [DOI] [PubMed] [Google Scholar]
- 10.Moro PL, Moore A, Balcacer P, Montero A, Diaz D, Gómez V, et al. Epidemiology of needlesticks and other sharps injuries and injection safety practices in the Dominican Republic. Am J Infect Control. 2007 Oct;35(8):552–559. doi: 10.1016/j.ajic.2007.06.001. [DOI] [PubMed] [Google Scholar]