Abstract
Background:
This study aimed to compare the effects of preoperative administration of midazolam and dexmedetomidine on cognitive dysfunction prevention after cataract surgery.
Materials and Methods:
This research was a double-blind controlled clinical trial. In this study, 150 candidates for cataract surgery under general anesthesia, over 65 years, and similar to American Society of Anesthesiologists I and II characteristics were selected as the sample and randomly assigned to three groups. Participants of these three groups were treated with 0.1 mg/kg of midazolam, 1 μg/kg of dexmedetomidine, and the same volume of normal saline (control), respectively. Hemodynamic parameters and cognitive dysfunction score of the participants were measured using the Mini-Mental State Examination (MMSE) before the surgery, 24 h and 1 week after the surgery.
Results:
An evaluation of hemodynamic parameters before anesthesia up to 24 h after the surgery showed no significant difference between the midazolam, dexmedetomidine, and control groups in terms of systolic and diastolic blood pressure, heart rate, and blood oxygen saturation (P > 0.05). In addition, there was no statistically significant difference between the midazolam and dexmedetomidine groups in the MMSE score before the surgery and 24 h and 1 week after that (P > 0.05). However, there was a significant difference between these two groups and control (P < 0.05).
Conclusion:
There was no significant difference between midazolam and dexmedetomidine in reducing postoperative cognitive dysfunction (POCD). However, there is a significant difference between these two groups and control. Hence, either midazolam or dexmedetomidine can be prescribed to reduce POCD in cataract surgeries.
Keywords: Cataract, cognitive dysfunction, dexmedetomidine, midazolam
Introduction
Cognitive dysfunction is among the most prevalent, severe, and life-threatening postoperative complications.[1] However, it is rarely diagnosed and usually considered an accidental finding.[2] The exact cause of cognitive dysfunction has not been identified yet.[3] Postoperative cognitive dysfunction (POCD) refers to a disorder in mental processes that may affect only one of the cognitive areas, such as visual memory, verbal memory, attention, and concentration. Cognitive dysfunction should be differentiated from postoperative delirium, a transient and fluctuating disturbance of alertness occurring shortly after a surgery.[4]
This disorder can alter patients’ personality and memory and increase postoperative complications.[1,3] Changes in personality and social solidarity even last for a long time in some patients and they lose their ability to understand and skills. These changes altogether are known as POCD.[5,6,7] Since cataract surgery is a short procedure with light anesthesia that rarely causes water and electrolyte disorders, only hemodynamic and hypoxic disorders may trigger POCD in cataract surgeries.[8]
POCD is associated with increased mortality and disability, extended length of stay, and the need for long-term post-discharge care and rehabilitation facilities, increasing the pre- and post-operative costs.[9] POCD may occur acutely and continue until 3 months after the surgery. There are reports of both short-term and long-term effects and complications of POCD.[10]
Although many studies have been carried out on POCD around the world, a few studies have been conducted in Iran about the effects of intravenous administration of midazolam and dexmedetomidine after the induction of general anesthesia on the incidence of cognitive dysfunction in elderly candidates for cataract surgery.
The results of some studies indicate that the use of dexmedetomidine, a selective alpha-2 antagonist, reduces the incidence of POCD and the duration of mechanical ventilation, compared to other sedatives.[11,12] Some other studies have also reported the effectiveness of midazolam in reducing POCD.[13,14] Nevertheless, there has been no consensus about their effects so far. Considering the high prevalence of POCD and paucity of studies on prevention effects of dexmedetomidine in Iran, the present study aims to compare the effects of preoperative intravenous administration of midazolam and dexmedetomidine on the prevention of POCD among the elderly candidates for cataract surgery.
Materials and Methods
The present research was a randomized, double-blind controlled clinical trial that was conducted in Feiz Ophthalmology Hospital of Isfahan in 2017–2018. The statistical population consisted of the elderly candidates for cataract surgery under general anesthesia over 65 years with similar American Society of Anesthesiologists (ASA) I and II characteristics.
The inclusion criteria were age over 65 years, ASA score I or II, candidate for cataract surgery, patient‘s consent to participate in the study, no history of sensitivity to anesthetics, and no history of moderate to severe mental disorders, according to patient‘s medical records and history. In addition, the occurrence of severe hemodynamic disorder during the surgery leading to a change in anesthesia, extended surgery duration for >1 h, patient‘s refusal to complete the questionnaire after the surgery, and sensitivity to the examined anesthetics were determined as the exclusion criteria.
Considering a confidence level of 95%, a statistical power of 80%, the prevalence of cognitive dysfunction among patients undergoing the cataract surgery with general anesthesia (0.25), and the least significant difference between the two groups (0.2), the sample size was determined to be 46 in each experimental group. For further reliability, 50 patients from 150 total patients were assigned to each group randomly by random allocation software. The participants were selected using simple nonprobability and convenience sampling methods [Diagram 1].
Diagram 1.
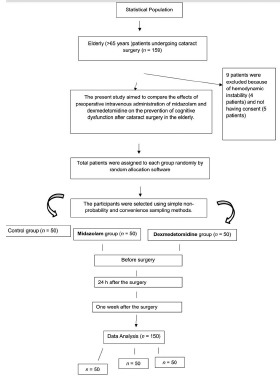
Research design
The participants were examined for cognitive dysfunction using the Mini-Mental State Examination (MMSE), a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive dysfunction. The maximum score obtainable on this test is equal to 30, and any score in the range 25–30, 20–25, and <20 indicates normal cognition, possible cognitive dysfunction, and definitive cognitive dysfunction, respectively. In this study, the MMSE was filled out before the surgery and 24 h and 1 week after the surgery.
After obtaining the Medical Ethics Committee of the University permission, 150 elderly patients over 65 who met the inclusion criteria were randomly assigned to three groups of 50, including midazolam, dexmedetomidine, and control. Anesthesia was induced to participants of all groups using 2 μg/kg of fentanyl, 5 mg/kg of sodium thiopental, and 0.6 mg/kg of atracurium. Then, participants of the three groups were treated with intravenous 0.1 mg/kg of midazolam, 1 μg/kg of dexmedetomidine, and the same volume of normal saline (control), respectively simultaneous with induction of general anesthesia. Then, tracheal intubation was performed for all participants and the anesthesia was maintained using a combination of oxygen and nitrous oxide and a minimum alveolar concentration isoflurane.
Hemodynamic parameters of patients (systolic and diastolic blood pressure, the mean arterial pressure, heart rate, respiratory rate, and SpO2) were measured and recorded before anesthesia, during anesthesia (0, 15, 30, 45, and 60 min after the induction of anesthesia), and at the arrival and discharge from the recovery ward. Hemodynamic parameters tried to be kept stable, and if there was a change in blood pressure of patients >30%, the patient was excluded from the study while receiving the necessary care.
To observe the principles of blinding, participants were unaware of the drug administered to them, drugs were prepared in similar syringes by an anesthesiologist who was not involved in the study and then were injected to participants by the researcher. In addition, one who completed the MMSE for participants was unaware of the anesthetic or sedation practice. The MMSE was filled out before the surgery and 24 h and 1 week after the surgery and the obtained scores were compared between the three groups.
Finally, the data were statistically analysed using one-way analysis of variance (mean age (year), mean weight (kg), duration of surgery), Chi-square test (gender, ASA) and a measurements repeated (MMSE score) the in SPSS-22 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
Results
In this study, 150 patients undergoing cataract surgery were examined in three groups of midazolam, dexmedetomidine, and control. Participants in the three groups were matched in terms of age, gender, weight, duration of surgery, and ASA (P > 0.05).
An evaluation of hemodynamic parameters before anesthesia up to 24 h after the surgery showed that there was no significant difference between the three groups of midazolam, dexmedetomidine, and control in terms of systolic and diastolic blood pressure, heart rate, and blood oxygen saturation (P > 0.05) [Table 1].
Table 1.
The mean and standard deviation of age, weight, and duration of surgery in the three experimental groups
| Variable | Midazolam | Dexmedetomidine | Placebo | P |
|---|---|---|---|---|
| Mean age (year) | 63.6±8.29 | 66.5±1.6 | 64.02±7.25 | 0.14 |
| Mean weight (kg) | 70.2±14.89 | 69.66±7.94 | 68.58±10.61 | 0.76 |
| Duration of surgery (min) | 20±9 | 18±7 | 20±9 | 0.27 |
| Gender (%) | ||||
| Male | 25 (50) | 25 (50) | 19 (38) | 0.38 |
| Female | 25 (50) | 25 (50) | 31 (62) | |
| ASA (%) | ||||
| I | 40 (80) | 40 (80) | 43 (86) | 0.67 |
| II | 10 (20) | 10 (20) | 7 (14) | |
ASA: American Society of Anesthesiologists
Table 2 presents the frequency distribution of cognitive dysfunction in the three groups of midazolam, dexmedetomidine, and control. Based on the results, 3 (6%), 5 (10%), and 2 (4%) participants exhibited cognitive dysfunction in the three groups, respectively, but there was no statistically significant difference between them (P = 0.47). At 24 h after the surgery, 7 (14%), 6 (12%), and 12 (24%) participants in the above-mentioned groups developed cognitive dysfunction, respectively, and the difference between the two groups (dexmedetomidine and midazolam) with control was statistically significant (P < 0.05). However, there was no significant difference between midazolam and dexmedetomidine group (P > 0.05). One week after the surgery, 4 (8%), 6 (12%), and 10 (20%) patients were diagnosed with cognitive dysfunction in midazolam, dexmedetomidine, and control groups, respectively. These figures indicate a significant difference between the two groups (dexmedetomidine and midazolam) with control. However, there was no significant difference between midazolam and dexmedetomidine group (P > 0.05).
Table 2.
The frequency distribution of cognitive dysfunction and the Mini-Mental State Examination score in the three experimental groups
| Variable | Time | Midazolam | Dexmedetomidine | Control | P |
|---|---|---|---|---|---|
| Frequency (percentage) of cognitive dysfunction | Before surgery | 3 (6) | 5 (10) | 2 (4) | 0.47 |
| 24 h after the surgery | 7 (14) | 6 (12) | 12 (24) | 0.031 | |
| 1 week after the surgery | 4 (8) | 6 (12) | 10 (20) | 0.042 | |
| MMSE score (%) | |||||
| Before surgery | <20 | 3 (6) | 6 (12) | 2 (4) | 0.002 |
| 20-25 | 6 (12) | 8 (16) | 4 (8) | ||
| 26-30 | 41 (82) | 36 (72) | 44 (88) | ||
| 24 h after the surgery | <20 | 7 (14) | 6 (12) | 12 (24) | 0.001 |
| 20-25 | 4 (8) | 4 (8) | 8 (16) | ||
| 26-30 | (78) 39 | 40 (80) | 30 (60) | ||
| 1 week after the surgery | <20 | 4 (8) | 6 (12) | 10 (20) | 0.000 |
| 20-25 | 10 (20) | 8 (16) | 8 (16) | ||
| 26-30 | 36 (72) | 36 (72) | 32 (64) | ||
MMSE: Mini-Mental State Examination
Discussion
POCD is a relatively common complication of surgeries. Although different methods have been proposed to reduce the incidence and severity of POCD, no desirable and ideal method has been proposed to control it. Recently, dexmedetomidine has been prescribed for intensive care unit patients as an alternative to gamma-aminobutyric acid GABA-based anesthetics. The present study aimed to compare the effects of preoperative intravenous administration of midazolam and dexmedetomidine on reducing cataract POCD in the elderly candidates for cataract surgery.
Based on the study findings, there was no significant difference between the two groups of midazolam, dexmedetomidine in terms of POCD. However, there was significant difference between the two groups with control in terms of POCD. The severity of cognitive dysfunction before the surgery and 24 h and 1 week after the surgery also indicated a significant difference between the three groups, but midazolam and dexmedetomidine were not significantly different in the reduction of cognitive dysfunction.
In a study conducted by Ke et al. on patients under chemotherapy, the results demonstrated that although dexmedetomidine was not significantly effective in the reduction of cognitive dysfunction, the incidence of cognitive dysfunction in patients treated with dexmedetomidine was significantly lower than that of the control.[15] This difference can be attributed to the type of patients and the sample. In another clinical trial carried out by Bekker et al. The effectiveness of dexmedetomidine was compared with propofol and midazolam and the results showed that the alertness of patients who received dexmedetomidine was higher than patients treated with propofol or midazolam.[16]
Arpaci and Bozkırlı compared the effects of remifentanil plus dexmedetomidine and remifentanil plus midazolam on the reduction of cognitive dysfunction in patients under cystoscopy and reported that there was no significant difference between the two groups in the incidence of cognitive dysfunction.[17]
According to a study conducted by Alipour et al. dexmedetomidine seems to be a healthy and cost-effective alternative to midazolam, propofol, and fentanyl because of its excellent sedative effects without suppressing respiration and creating active metabolites, anti-sympathetic properties, no need to discontinue it when weaning the patient from mechanical ventilation and maintaining the hemodynamic status of the patient in an acceptable range.[18]
Talakoub et al. compared the effects of intravenous administration of diazepam and midazolam, as anesthesia prodrugs, on preoperative SpO2 and the results showed that both drugs reduced SpO2, but the effects of midazolam were greater, as t-test indicated a significant difference between the two groups during the first 5 min after the prodrug administration.[19]
Although the same positive results were obtained in the present study regarding the maintenance of the mean heart rate and reduction of SpO2 in patients treated with dexmedetomidine, the results were not significantly different from those obtained from participants in the midazolam group.
Based on the review of some previous findings, it seems that there are still doubts about the effects of midazolam and dexmedetomidine on reducing POCD and more studies are needed to be conducted in this regard.
Conclusion
The study findings indicated that there was no significant difference between midazolam and dexmedetomidine in the reducing POCD. However, there is a significant difference between these two groups and control. Hence, midazolam and dexmedetomidine can be prescribed by physicians to reduce POCD in candidates for cataract surgery. However, further studies in this area are recommended to be conducted in the future.
This article was approved in Isfahan University of medical sciences research department with the number of 396679.
Financial support and sponsorship
Isfahan University of Medical sciences, Research Department.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was financially supported by Isfahan University of Medical sciences, Faculty of Medicine, Anesthesiology Department, Isfahan University of Medical sciences, Faculty of Medicine, Ophthalmology Department Isfahan University of Medical Sciences, Research Department.
References
- 1.Engelhard K, Werner C. Postoperative cognitive dysfunction. Anaesthesist. 2005;54:588–94. doi: 10.1007/s00101-005-0829-y. [DOI] [PubMed] [Google Scholar]
- 2.Norkienė I, Samalavičius R, Misiūrienė I, Paulauskienė K, Budrys V, Ivaškevičius J. Incidence and risk factors for early postoperative cognitive decline after coronary artery bypass grafting. Medicina (Kaunas) 2010;46:460–4. [PubMed] [Google Scholar]
- 3.Steinmetz J, Jespersgaard C, Dalhoff K, Hedley P, Abildstrøm H, Christiansen M, et al. Cytochrome P450 polymorphism and postoperative cognitive dysfunction. Minerva Anestesiol. 2012;78:303–9. [PubMed] [Google Scholar]
- 4.Wang W, Wang Y, Wu H, Lei L, Xu S, Shen X, et al. Postoperative cognitive dysfunction: Current developments in mechanism and prevention. Med Sci Monit. 2014;20:1908–12. doi: 10.12659/MSM.892485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morimoto Y, Yoshimura M, Utada K, Setoyama K, Matsumoto M, Sakabe T. Prediction of postoperative delirium after abdominal surgery in the elderly. J Anesth. 2009;23:51–6. doi: 10.1007/s00540-008-0688-1. [DOI] [PubMed] [Google Scholar]
- 6.Juliebø V, Bjøro K, Krogseth M, Skovlund E, Ranhoff AH, Wyller TB, et al. Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J Am Geriatr Soc. 2009;57:1354–61. doi: 10.1111/j.1532-5415.2009.02377.x. [DOI] [PubMed] [Google Scholar]
- 7.Olin K, Eriksdotter-Jönhagen M, Jansson A, Herrington MK, Kristiansson M, Permert J, et al. Postoperative delirium in elderly patients after major abdominal surgery. Br J Surg. 2005;92:1559–64. doi: 10.1002/bjs.5053. [DOI] [PubMed] [Google Scholar]
- 8.Hall TA, McGwin G, Jr, Owsley C. Effect of cataract surgery on cognitive function in older adults. J Am Geriatr Soc. 2005;53:2140–4. doi: 10.1111/j.1532-5415.2005.00499.x. [DOI] [PubMed] [Google Scholar]
- 9.Ishii K, Kabata T, Oshika T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. 2008;146:404–9. doi: 10.1016/j.ajo.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Pan LF, Wang DX, Li J. Effects of different methods of anesthesia and analgesia on early postoperative cognitive dysfunction after non-cardiac surgery in the elderly. Beijing Da Xue Xue Bao Yi Xue Ban. 2006;38:510–4. [PubMed] [Google Scholar]
- 11.Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after noncardiac surgery: A systematic review. Anesthesiology. 2007;106:572–90. doi: 10.1097/00000542-200703000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Naghibi K, Nazemroaya B, Sargaran A. A comparison of the effect of intravenous dexamethasone and lidocaine on prevention of postoperative cognitive disorders in cataract surgery in elderly patients. J Isfahan Med Sch. 2018;36:666–72. [Google Scholar]
- 13.Bekker A, Haile M, Kline R, Didehvar S, Babu R, Martiniuk F, et al. The effect of intraoperative infusion of dexmedetomidine on the quality of recovery after major spinal surgery. J Neurosurg Anesthesiol. 2013;25:16–24. doi: 10.1097/ANA.0b013e31826318af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naghibi K, Shafa A, Hirmanpour A, Sabaghi B. The impact of general anesthesia vs. local anesthesia with intravenous sedation on the incidence of postoperative cognitive dysfunction after cataract surgery in elderly patients. J Isfahan Med Sch. 2016;34:134–42. [Google Scholar]
- 15.Ke JJ, Zhang ZZ, Feng XB. The effect of various dose of dexmedetomidine on the prevention of postoperative cognitive dysfunction in aged patients with intraperitoneal hyperthermic perfusion chemotherapy. Chin J Anesthesiol. 2013;33:1192–4. [Google Scholar]
- 16.Naghibi K, Dodangeh M, Hashemi ST, Moradi-Farsani D. Evaluation and comparison of the effects of propofol, dexamethasone, and ondonestrone in the prevention of complications during and after cataract surgery. J Isfahan Med Sch. 2018;36:372–8. [Google Scholar]
- 17.Arpaci AH, Bozkırlı F. Comparison of sedation effectiveness of remifentanil-dexmedetomidine and remifentanil-midazolam combinations and their effects on postoperative cognitive functions in cystoscopies: A randomized clinical trial. J Res Med Sci. 2013;18:107–14. [PMC free article] [PubMed] [Google Scholar]
- 18.Alipour M, Tabari M, Azad AM. Comparative study evaluating efficacy of sufentanil versus midazolam in preventing myoclonic movements following etomidate. J Anaesthesiol Clin Pharmacol. 2016;32:29–32. doi: 10.4103/0970-9185.173382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talakoub R, Rezvani M, Alikhani A, Golparvar M, Jabalameli M, Amini Z, et al. The effect of intravenous midazolam on duration of spinal anesthesia. Shiraz E Med J. 2015;16:e21586. [Google Scholar]


