Abstract
OBJECTIVE
This study examined associations of maternal glycemia during pregnancy with childhood glucose outcomes in the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) cohort.
RESEARCH DESIGN AND METHODS
HAPO was an observational international investigation that established associations of maternal glucose with adverse perinatal outcomes. The HAPO Follow-up Study included 4,832 children ages 10–14 years whose mothers had a 75-g oral glucose tolerance test (OGTT) at ∼28 weeks of gestation. Of these, 4,160 children were evaluated for glucose outcomes. Primary outcomes were child impaired glucose tolerance (IGT) and impaired fasting glucose (IFG). Additional outcomes were glucose-related measures using plasma glucose (PG), A1C, and C-peptide from the child OGTT.
RESULTS
Maternal fasting plasma glucose (FPG) was positively associated with child FPG and A1C; maternal 1-h and 2-h PG were positively associated with child fasting, 30 min, 1-h, and 2-h PG, and A1C. Maternal FPG, 1-h, and 2-h PG were inversely associated with insulin sensitivity, whereas 1-h and 2-h PG were inversely associated with disposition index. Maternal FPG, but not 1-h or 2-h PG, was associated with child IFG, and maternal 1-h and 2-h PG, but not FPG, were associated with child IGT. All associations were independent of maternal and child BMI. Across increasing categories of maternal glucose, frequencies of child IFG and IGT, and timed PG measures and A1C were higher, whereas insulin sensitivity and disposition index decreased.
CONCLUSIONS
Across the maternal glucose spectrum, exposure to higher levels in utero is significantly associated with childhood glucose and insulin resistance independent of maternal and childhood BMI and family history of diabetes.
Introduction
The incidence and prevalence of type 2 diabetes are increasing among children (1–6). The reasons for this are multifactorial, but animal and human studies have shown that intrauterine exposure to maternal preexisting diabetes or gestational diabetes mellitus (GDM) is associated with higher risk for altered offspring glucose metabolism (7–11). However, the relationship between maternal glucose levels across the spectrum of glucose values and childhood glucose metabolism is not known.
The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study recruited a multinational, racially and ethnically diverse cohort of women and showed that glucose levels below those diagnostic of diabetes were associated with adverse pregnancy outcomes (12). This led to new diagnostic criteria for GDM proposed by the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) (13). HAPO also demonstrated that the relationship between maternal glucose during pregnancy and newborn outcomes, including birth weight, sum of skinfolds, and cord C-peptide greater than the 90th percentile, was progressively higher across increasing categories of maternal glucose at 28 weeks of gestation. Whether similar relationships exist between maternal glucose levels during pregnancy across the continuum and childhood metabolic outcomes is unknown.
The HAPO Follow-up Study (FUS) offered a unique opportunity to examine this question in a cohort not confounded by treatment during pregnancy. We recently demonstrated an inverse association of GDM, using IADPSG criteria, with insulin sensitivity and the disposition index and positive association with impaired glucose tolerance (IGT) in HAPO FUS children at ages 10–14 years (11). The current study examined associations of in utero exposure to maternal glucose across the spectrum, including levels less than those diagnostic for GDM, with child glucose metabolism in the HAPO FUS cohort.
Research Design and Methods
HAPO was a population-based study in which women underwent a 75-g oral glucose tolerance test (OGTT) at ∼28 weeks of gestation (12). Fasting plasma glucose (FPG), 1-h, and 2-h plasma glucose (PG) were measured at a central laboratory (12). OGTT results remained blinded to caregivers and participants unless FPG >5.8 mmol/L and/or 2-h PG >11.1 mmol/L, either was <2.5 mmol/L, or random PG at 34–37 weeks of gestation was ≥8.9 mmol/L (12). Using these criteria, the results of 427 participants (1.8%) were unblinded based on FPG and/or 2-h PG. Blinded participants were untreated. Height, weight, and blood pressure were measured using standardized procedures. Demographic and lifestyle characteristics, including age, self-reported race and ethnicity, and smoking or alcohol use during pregnancy, were collected via questionnaire and parity via medical record abstraction.
Participants
HAPO FUS participants were recruited during 2013–2016 from 10 of 15 HAPO field centers based on recruitment feasibility. HAPO FUS eligibility criteria included caregivers and participants being blinded to HAPO OGTT results, gestational age at delivery ≥37 weeks, and no major neonatal malformations or fetal/neonatal death. This yielded 15,812 eligible mother-child pairs. The recruitment target was 7,000 pairs, based on the primary childhood outcome of overweight/obesity (14). Multiple attempts were made to contact all eligible participants through local Institutional Review Board (IRB)–approved means. Of the 15,812 eligible pairs, 6,490 could not be contacted and 4,488 declined participation (Supplementary Fig. 1). A total of 4,834 children completed all or part of the HAPO FUS visit. OGTT completion was not required for participation. One child was excluded due to inadequate fasting and a second for lack of cooperation. Of the remaining 4,832 children, data were analyzed from 4,160 who had an FPG and at least one other timed OGTT measurement or reported having diabetes on treatment and were not excluded for having type 1 diabetes by antibody testing (see below).
Each center’s IRB approved the protocol. All mothers provided written informed consent for their child, and children assented where required by the local IRB. There was an external Observational Study Monitoring Board.
Study Visit
Height was measured twice without shoes to the nearest 0.5 cm with a stadiometer and again if results differed by >1.0 cm. Weight was measured twice to the nearest 0.1 kg and again if results differed by >0.5 kg.
Participants underwent a 2-h OGTT with a glucose load of 1.75 g/kg body wt (maximum 75 g) after an 8-h overnight fast, with samples drawn for glucose and C-peptide at fasting, 30 min, 1 h, and 2 h, and fasting A1C. If the mother reported that the child had pharmacologically treated diabetes, only a nonfasting blood sample was collected. All samples were processed at the field center laboratory and stored at −80°C until shipment to the Central Laboratory.
Skinfolds (triceps, subscapular, suprailiac) were measured twice with calibrated calipers (Harpenden, London, U.K.) to the nearest 0.1 mm and again if results differed by >1.0 mm. Fat percentage was measured by air displacement plethysmography (BOD POD; COSMED, Rome, Italy). Tanner staging was performed by trained individuals using breast/areolar development and testicular volume (Prader orchidometer). Child’s age, first-degree family history of diabetes, and menstrual history for girls were collected from the mother via questionnaire.
Laboratory Measurements
Glucose was measured by hexokinase and A1C by standard methods in Northwestern Memorial Hospital’s Clinical Chemistry Laboratory on a Beckman Coulter SYNCHRON LX analyzer. Blinded duplicate samples were assayed several weeks apart. Coefficients of variation (CVs) were calculated within pairs for a random 10% subset; mean CV was 1.5% for fasting, 1-h, and 2-h PG, 1.3% for 30-min PG, and 3.1% for A1C. C-peptide was measured in Northwestern’s Comprehensive Metabolic Core using electrochemiluminescence immunoassay on a Roche cobas e 411 analyzer (15). Mean CVs were 2.8% for fasting, 2.9% for 30-min, 3.0% for 1-h, and 3.2% for 2-h C-peptide. Type 1 diabetes was evaluated with autoantibodies, as previously described (14), in children reported to have diabetes on treatment (n = 9) and in children with OGTT values indicative of diabetes (n = 5). Of these 14 children, 4 had positive antibody results and were excluded.
Calculations
The Matsuda index was calculated using C-peptide levels from the child OGTT to determine insulin sensitivity (16). The insulinogenic index, a measure of insulin secretion, was calculated using C-peptide levels and defined as ΔC-peptide (fasting – 30-min, nmol/L)/Δglucose (fasting – 30-min, mmol/L) (17). The disposition index, a measure of pancreatic β-cell function, was calculated as the product of Matsuda and insulinogenic indices and log transformed (18).
Outcomes and Predictors
Dichotomous outcomes in this analysis were child impaired fasting glucose (IFG) (FPG 5.6–6.9 mmol/L according to American Diabetes Association criteria [19]) or impaired glucose tolerance (IGT) (2-h PG 7.8–11.0 mmol/L). Cases of type 2 diabetes were too few for meaningful analysis (n = 10) (FPG ≥7.0 mmol/L and/or 2-h PG ≥11.1 mmol/L or self-reported diabetes on treatment at HAPO FUS visit). Additional outcomes were continuous measures using fasting, 30-min, 1-h, and 2-h PG and C-peptide levels and A1C from the child OGTT. An integrated measure of child glucose was obtained using the sum of individual glucose z scores, calculated by subtracting the mean glucose level, dividing by the SD for each time point, and summing these individual “z scores.” Insulin sensitivity and secretion were examined using Matsuda, insulinogenic, and disposition indices.
Primary predictors were maternal fasting, 1-h, and 2-h PG during the HAPO pregnancy OGTT, scaled by their SDs, and the sum of their z scores using means and SDs for timed glucose measurements from the HAPO Study. Child outcome frequencies and associations were also examined according to maternal glucose categories. Five categories for each glucose measure were defined according to original HAPO analyses and IADPSG GDM diagnostic thresholds. The fifth and highest category for each measure corresponded to IADPSG GDM diagnostic thresholds (FPG ≥5.1 mmol/L, 1-h PG ≥10.0 mmol/L, 2-h PG ≥8.5 mmol/L) (13). The lowest three categories for each measure were the same as those used for analyses of glucose during HAPO. The fourth category included values between the third and fifth categories. Maternal HAPO pregnancy OGTT glucose levels at fasting, 1-h, and 2-h were also grouped into classes based on their trajectory over the time points of the pregnancy OGTT, as described below. These classes were evaluated for association with child metabolic outcomes.
Statistical Analyses
HAPO FUS data were summarized using frequencies and counts for categorical variables and means and SDs for continuous variables. Histograms and box plots were examined to determine the shape of distributions and identify potential outliers. For dichotomous child IFG and IGT outcomes, multiple logistic regression was used to evaluate associations with maternal glucose predictors. For continuous child outcomes, multiple linear regression was used. Covariate adjustments were examined as follows: model 1: field center, child age, sex, and pubertal status (Tanner stage 1, 2/3, 4/5) with sex by Tanner stage interaction terms, and maternal variables at pregnancy OGTT (age, height, mean arterial pressure, parity [0, 1+], smoking [yes/no], drinking alcohol [yes/no], gestational age), child’s family history of diabetes in first-degree relatives; model 2: model 1 plus maternal BMI at pregnancy OGTT; model 3: model 1 plus child’s BMI z score; model 4: model 1 plus maternal BMI at pregnancy OGTT plus child’s BMI z score.
Child BMI z scores were calculated according to L (lambda), M (mu), and S (sigma) curves used by the International Obesity Task Force (20). Although the study was not powered to evaluate Tanner stage–specific associations, interaction terms between maternal glucose measures and Tanner stage were evaluated to explore potential variability in associations according to pubertal status. Exploratory association analyses were also performed within Tanner stage 1, 2/3, and 4/5 groups. Multiple imputation in the full data set that included measurements of sex steroid hormones in children was used to account for missing Tanner stage data. A “missing at random” assumption was used after confirming findings varied little under “missing not at random” (14). Logistic regression model fit was measured using C statistics and confirmed by Hosmer-Lemeshow goodness-of-fit tests. Linear regression model fit was assessed by scatterplots of residuals versus fitted values, histograms, and qqplots of residuals and DFBETA statistics. Adjusted R2 values were used to summarize variability explained in linear models. Quadratic terms and restricted cubic splines estimated with the rms R software package (21) were used to assess linearity assumptions. P values <0.05 were considered statistically significant. All analyses were conducted in R 3.4.1 software (22).
To evaluate shapes of maternal PG values over the course of the OGTT, the R package lcmm (23) was used to estimate trajectories of fasting, 1-h, and 2-h maternal PG and identify groups of mothers with similar OGTT trajectories according to latent class analysis (24). Random effects were specified for linear, quadratic, and cubic terms for time to explore the best-fitting shape, and the number of similar trajectory groups was allowed to range from two to six. Unadjusted models and separate models adjusted for field center, maternal age, drinking status, smoking status, family history of diabetes, gestational age, height, mean arterial pressure, parity, and BMI at pregnancy OGTT were evaluated. Optimal trajectory shape, number of groups, and model adjustment were selected by criteria generally used in latent class analyses, including model convergence, Bayesian information criterion, and at least 2% membership in each latent class with posterior probabilities greater than 0.7 (25,26).
Results
Participants
Characteristics of the 4,160 participating children during the HAPO FUS and their mothers during HAPO are reported in Supplementary Table 1. Mothers of children who did and did not participate (unable to contact or declined) in this study are compared in Supplementary Table 2 (weighted summaries). The mean age and frequency of GDM were 30.0 years and 14.9% and 29.1 years and 16.9% in mothers of children who did and did not participate, respectively. Mean BMI, FPG, 1-h, and 2-h PG during the HAPO OGTT and race/ethnicity were similar between groups.
Model Diagnostics
Hosmer-Lemeshow P values for logistic regression models ranged 0.53–0.96 for all outcomes, indicating reasonable model fit. C statistics for logistic regression models ranged 0.69–0.78, and R2 values ranged 0.05–0.39 for linear models. C statistics and R2 values changed little for each outcome for models 1–4, indicating that detected associations varied little across covariate adjustments. Colinearity was not a concern, with pairwise correlations ranging from 0 to 0.20 for model covariates. Residual plots indicated reasonable linearity. Confirming this, P values for quadratic terms and restricted cubic splines ranged 0.05–0.99, indicating no significant departure from linearity for all analyses. DFBETA statistics indicated no observations of undue influence.
Associations Between Continuous Maternal Glycemia and Continuous Child Glucose Outcomes
Initial analyses examined associations of continuous maternal fasting, 1-h, and 2-h PG and the sum of glucose z scores during the pregnancy OGTT with measures of child glucose metabolism (Table 1). Maternal FPG was positively associated with child FPG, 30-min PG, the sum of glucose z scores, and A1C. Adjusting for maternal BMI and/or child BMI z score (models 2–4) had minimal effect on these associations. Maternal FPG was not associated with 1-h or 2-h child PG. In contrast, maternal 1-h and 2-h PG during the pregnancy OGTT and maternal sum of glucose z scores were positively associated with all child glucose measures and A1C in all models (Table 1). Adjusting for maternal BMI at pregnancy OGTT and/or child BMI z score at follow-up did not attenuate these associations.
Table 1.
Association of continuous maternal measures of glucose during pregnancy with child metabolic outcomes
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
|---|---|---|---|---|
| Continuous child metabolic outcomes | β (95% CI) P value, adjusted R2 | β (95% CI) P value, adjusted R2 | β (95% CI) P value, adjusted R2 | β (95% CI) P value, adjusted R2 |
| Maternal fasting glucose* | ||||
| Fasting glucose (mmol/L) | 0.044 (0.033–0.056) P < 0.001, R2 = 0.24 | 0.046 (0.034–0.058) P < 0.001, R2 = 0.24 | 0.042 (0.031–0.054) P < 0.001, R2 = 0.24 | 0.046 (0.034–0.058) P < 0.001, R2 = 0.24 |
| 30-min glucose (mmol/L) | 0.055 (0.012–0.10) P = 0.013, R2 = 0.12 | 0.063 (0.019–0.11) P = 0.006, R2 = 0.12 | 0.052 (0.0083–0.096) P = 0.019, R2 = 0.12 | 0.064 (0.018–0.11) P = 0.006, R2 = 0.12 |
| 1-h glucose (mmol/L) | 0.0022 (−0.054 to 0.059) P = 0.93, R2 = 0.07 | 0.0.011 (−0.048 to 0.068) P = 0.73, R2 = 0.07 | −0.0017 (−0.058 to 0.055) P = 0.96, R2 = 0.07 | 0.010 (−0.048 to 0.068) P = 0.73, R2 = 0.07 |
| 2-h glucose (mmol/L) | 0.032 (−0.0061 to 0.069) P = 0.10, R2 = 0.08 | 0.033 (−0.0061 to 0.073) P = 0.095, R2 = 0.08 | 0.019 (−0.018 to 0.057) P = 0.31, R2 = 0.09 | 0.032 (−0.0061 to 0.071) P = 0.10, R2 = 0.09 |
| Sum of glucose z scores | 0.19 (0.10–0.27) P < 0.001, R2 = 0.16 | 0.20 (0.11–0.29) P < 0.001, R2 = 0.16 | 0.16 (0.08–0.25) P < 0.001, R2 = 0.17 | 0.20 (0.11–0.29) P < 0.001, R2 = 0.17 |
| A1C (%) | 0.014 (0.005–0.024) P = 0.003, R2 = 0.10 | 0.013 (0.003–0.022) P = 0.009, R2 = 0.10 | 0.012 (0.002–0.021) P = 0.01, R2 = 0.11 | 0.013 (0.003–0.023) P = 0.01, R2 = 0.11 |
| Matsuda index | −62.2 (−84.5 to −39.3) P < 0.001, R2 = 0.23 | −45.3 (−68.7 to −21.8) P < 0.001, R2 = 0.23 | −37.1 (−57.3 to −16.9) P < 0.001, R2 = 0.38 | −43.6 (−64.4 to −22.9) P < 0.001, R2 = 0.38 |
| Insulinogenic index | 0.028 (0.0042–0.052), P = 0.022, R2 = 0.06 | 0.014 (−0.011 to 0.039) P = 0.27, R2 = 0.06 | 0.0018 (−0.0053 to 0.042) P = 0.13, R2 = 0.08 | 0.013 (−0.011 to 0.037) P = 0.29, R2 = 0.08 |
| Disposition index | 0.00 (−0.02 to 0.02) P = 0.76, R2 = 0.07 | −0.01 (−0.03 to 0.01) P = 0.55, R2 = 0.07 | 0.00 (−0.02 to 0.02) P = 0.93, R2 = 0.07 | −0.01 (−0.03 to 0.01) P = 0.56, R2 = 0.07 |
| Maternal 1-h glucose* | ||||
| Fasting glucose (mmol/L) | 0.025 (0.013–0.037) P < 0.001, R2 = 0.23 | 0.024 (0.013–0.036) P < 0.001, R2 = 0.23 | 0.023 (0.012–0.035) P < 0.001, R2 = 0.23 | 0.024 (0.013–0.036) P < 0.001, R2 = 0.23 |
| 30-min glucose (mmol/L) | 0.17 (0.13–0.21) P < 0.001, R2 = 0.13 | 0.18 (0.13–0.22) P < 0.001, R2 = 0.13 | 0.17 (0.13–0.21) P < 0.001, R2 = 0.13 | 0.18 (0.13–0.22) P < 0.001, R2 = 0.13 |
| 1-h glucose (mmol/L) | 0.20 (0.14–0.25) P < 0.001, R2 = 0.08 | 0.20 (0.15–0.26) P < 0.001, R2 = 0.08 | 0.19 (0.14–0.25) P < 0.001, R2 = 0.08 | 0.20 (0.15–0.26) P < 0.001, R2 = 0.08 |
| 2-h glucose (mmol/L) | 0.10 (0.063–0.14) P < 0.001, R2 = 0.08 | 0.10 (0.063–0.14) P < 0.001, R2 = 0.08 | 0.092 (0.055–0.13) P < 0.001, R2 = 0.10 | 0.098 (0.061–0.14) P < 0.001, R2 = 0.08 |
| Sum of glucose z scores | 0.40 (0.31–0.48) P < 0.001, R2 = 0.18 | 0.40 (0.32–0.49) P < 0.001, R2 = 0.18 | 0.38 (0.30–0.47) P < 0.001, R2 = 0.18 | 0.40 (0.31–0.49) P < 0.001, R2 = 0.18 |
| A1C (%) | 0.019 (0.010–0.028) P < 0.001, R2 = 0.11 | 0.018 (0.009–0.028) P < 0.001, R2 = 0.11 | 0.017 (0.008–0.027) P < 0.001, R2 = 0.12 | 0.018 (0.008–0.027) P < 0.001, R2 = 0.12 |
| Matsuda index | −75.3 (−97.6 to −52.9) P < 0.001, R2 = 0.23 | −67.1 (89.5 to −44.7) P < 0.001, R2 = 0.24 | −59.9 (−79.64 to −39.8) P < 0.001, R2 = 0.39 | −62.2 (−82.4 to −42.0) P < 0.001, R2 = 0.39 |
| Insulinogenic index | −0.034 (−0.58 to −0.01) P < 0.001, R2 = 0.05 | −0.042 (−0.066 to −0.018) P < 0.001, R2 = 0.06 | −0.041 (−0.065 to −0.018) P < 0.001, R2 = 0.08 | −0.045 (−0.068 to −0.021) P < 0.001, R2 = 0.06 |
| Disposition index | −0.07 (−0.10 to −0.06) P < 0.001, R2 = 0.08 | −0.08 (−0.10 to −0.06), P < 0.001, R2 = 0.08 | −0.07 (−0.09 to −0.05) P < 0.001, R2 = 0.08 | −0.08 (−0.10 to −0.06) P < 0.001, R2 = 0.08 |
| Maternal 2-h glucose* | ||||
| Fasting glucose (mmol/L) | 0.016 (0.0039–0.027) P = 0.008, R2 = 0.23 | 0.015 (0.0–39–0.027) P = 0.010, R2 = 0.23 | 0.014 (0.00028–0.026) P = 0.014, R2 = 0.23 | 0.014 (0.0033–0.026) P = 0.012, R2 = 0.23 |
| 30-min glucose (mmol/L) | 0.093 (0.051–0.14) P < 0.001, R2 = 0.12 | 0.096 (0.053–0.14) P < 0.001, R2 = 0.12 | 0.092 (0.050–0.13) P < 0.001, R2 = 0.12 | 0.095 (0.053–0.14) P < 0.001, R2 = 0.12 |
| 1-h glucose (mmol/L) | 0.14 (0.088–0.20) P < 0.001, R2 = 0.07 | 0.15 (0.092–0.20) P < 0.001, R2 = 0.07 | 0.14 (0.087–0.20) P < 0.001, R2 = 0.07 | 0.15 (0.091–0.20) P < 0.001, R2 = 0.07 |
| 2-h glucose (mmol/L) | 0.062 (0.024–0.10) P = 0.001, R2 = 0.08 | 0.062 (0.0.025–0.099) P = 0.001, R2 = 0.08 | 0.056 (0.0.019–0.092) P = 0.003, R2 = 0.10 | 0.059 (0.023–0.10) P = 0.002, R2 = 0.10 |
| Sum of glucose z scores | 0.25 (0.16–0.34) P < 0.001, R2 = 0.17 | 0.25 (0.16–0.34) P < 0.001, R2 = 0.17 | 0.24 (0.15–0.33) P < 0.001, R2 = 0.17 | 0.25 (0.16–0.33) P < 0.001, R2 = 0.17 |
| A1C (%) | 0.011 (0.002–0.021) P = 0.02, R2 = 0.10 | 0.010 (0.0009–0.020) P = 0.03, R2 = 0.10 | 0.010 (0.0004–0.019) P = 0.04, R2 = 0.11 | 0.010 (0.0005–0.019) P = 0.04, R2 = 0.11 |
| Matsuda index | −52.4 (−74.7 to −30.0) P < 0.001, R2 = 0.23 | −46.4 (−68.2 to −24.0) P < 0.001, R2 = 0.23 | −40.4 (−60.0 to −20.2) P < 0.001, R2 = 0.38 | −41.5 (−61.6 to −21.8) P < 0.001, R2 = 0.38 |
| Insulinogenic index | −0.018 (−0.042 to 0.0048) P = 0.12, R2 = 0.05 | −0.024 (−0.048 to −0.0059) P = 0.046, R2 = 0.06 | −0.024 (−0.048 to −0.0012) P = 0.040, R2 = 0.08 | −0.026 (−0.049 to −0.0030) P = 0.026, R2 = 0.08 |
| Disposition index | −0.05 (−0.07 to −0.03) P < 0.001, R2 = 0.07 | −0.05 (−0.07 to −0.03) P < 0.001, R2 = 0.07 | −0.07 (−0.07 to −0.03) P < 0.001, R2 = 0.07 | −0.05 (−0.07 to −0.03) P < 0.001, R2 = 0.08 |
| Maternal sum of glucose z scores | ||||
| Fasting glucose (mmol/L) | 0.016 (0.011–0.021) P < 0.001, R2 = 0.23 | 0.013 (0.011–0.021) P < 0.001, R2 = 0.23 | 0.015 (0.010–0.019) P < 0.001, R2 = 0.24 | 0.015 (0.011–0.021) P < 0.001, R2 = 0.24 |
| 30-min glucose (mmol/L) | 0.059 (0.041–0.078) P < 0.001, R2 = 0.12 | 0.063 (0.044–0.082) P < 0.001, R2 = 0.12 | 0.058 (0.040–0.077) P < 0.001, R2 = 0.12 | 0.063 (0.044–0.082) P < 0.001, R2 = 0.13 |
| 1-h glucose (mmol/L) | 0.064 (0.040–0.088) P < 0.001, R2 = 0.07 | 0.069 (0.044–0.093) P < 0.001, R2 = 0.07 | 0.062 (0.039–0.086) P < 0.001, R2 = 0.07 | 0.068 (0.044–0.092) P < 0.001, R2 = 0.07 |
| 2-h glucose (mmol/L) | 0.036 (0.020–0.052) P < 0.001, R2 = 0.08 | 0.037 (0.021–0.053) P < 0.001, R2 = 0.08 | 0.031 (0.015–0.047) P < 0.001, R2 = 0.10 | 0.036 (0.020–0.052) P < 0.001, R2 = 0.10 |
| Sum of glucose z scores | 0.15 (0.12–0.19) P < 0.001, R2 = 0.17 | 0.16 (0.12–0.20) P < 0.001, R2 = 0.17 | 0.15 (0.11–0.18) P < 0.001, R2 = 0.18 | 0.16 (0.12–0.20) P < 0.001, R2 = 0.18 |
| A1C (%) | 0.008 (0.004–0.012) P < 0.001, R2 = 0.11 | 0.008 (0.004–0.012) P < 0.001, R2 = 0.11 | 0.007 (0.003–0.012) P < 0.001, R2 = 0.12 | 0.008 (0.004–0.012) P < 0.001, R2 = 0.12 |
| Matsuda index | −34.9 (−44.7 to −25.6) P < 0.001, R2 = 0.23 | −30.0 (−39.3 to −20.2) P < 0.001, R2 = 0.24 | −25.6 (−33.8 to −16.9) P < 0.001, R2 = 0.38 | −27.8 (−36.5 to −19.1) P < 0.001, R2 = 0.38 |
| Insulinogenic index | −0.0048 (−0.015 to 0.0053) P = 0.34, R2 = 0.05 | −0.010 (−0.021 to 0.00) P = 0.047, R2 = 0.052 | −0.089 (−0.019 to 0.0012) P = 0.081, R2 = 0.08 | −0.011 (−0.021 to 0.0012) P = 0.031, R2 = 0.08 |
| Disposition index |
−0.02 (−0.03 to −0.2) P < 0.001, R2 = 0.08 |
−0.03 (−0.03 to −0.02) P < 0.001, R2 = 0.08 |
−0.02 (−0.03 to −0.01) P < 0.001, R2 = 0.08 |
−0.03 (−0.03 to 0.02) P < 0.001, R2 = 0.08 |
| Dichotomous child metabolic outcomes |
OR (95% CI) P value, C statistic |
OR (95% CI) P value, C statistic |
OR (95% CI) P value, C statistic |
OR (95% CI) P value, C statistic |
| Maternal fasting glucose** | ||||
| IFG | 1.22 (1.07–1.39) P = 0.003, C = 0.78 | 1.23 (1.07–1.40) P = 0.003, C = 0.78 | 1.21 (1.06–1.38) P = 0.004, C = 0.78 | 1.22 (1.07–1.40) P = 0.003, C = 0.78 |
| IGT | 1.10 (0.96–1.27) P = 0.19, C = 0.69 | 1.12 (0.97–1.30) P = 0.13, C = 0.69 | 1.08 (0.94–1.25) P = 0.28, C = 0.70 | 1.12 (0.97–1.30) P = 0.13, C = 0.70 |
| Maternal 1-h glucose** | ||||
| IFG | 1.12 (0.98–1.27) P = 0.084, C = 0.78 | 1.12 (0.98–1.27) P = 0.089, C = 0.78 | 1.11 (0.98–1.27) P = 0.10, C = 0.78 | 1.12 (0.98–1.27) P = 0.097, C = 0.78 |
| IGT | 1.40 (1.22–1.61) P < 0.001, C = 0.70 | 1.42 (1.23–1.63) P < 0.001, C = 0.70 | 1.39 (1.21–1.60) P < 0.001, C = 0.71 | 1.42 (1.23–1.63) P < 0.001, C = 0.71 |
| Maternal 2-h glucose** | ||||
| IFG | 1.08 (0.95–1.23) P = 0.24, C = 0.78 | 1.08 (0.95–1.23) P = 0.25, C = 0.78 | 1.07 (0.94–1.22) P = 0.28, C = 0.78 | 1.08 (0.94–1.22) P = 0.27, C = 0.78 |
| IGT | 1.17 (1.02–1.34) P = 0.025, C = 0.69 | 1.17 (1.02–1.34) P = 0.021, C = 0.69 | 1.16 (1.01–1.33) P = 0.034, C = 0.70 | 1.17 (1.02–1.34 P = 0.023, C = 0.70 |
| Maternal sum of glucose z scores | ||||
| IFG | 1.07 (1.01–1.13) P = 0.013, C = 0.78 | 1.07 (1.01–1.13) P = 0.013, C = 0.78 | 1.07 (1.01–1.14) P = 0.018, C = 0.78 | 1.07 (1.01–1.13) P = 0.015, C = 0.78 |
| IGT | 1.11 (1.05–1.18) P < 0.001, C = 0.70 | 1.12 (1.06–1.19) P < 0.001, C = 0.70 | 1.10 (1.04–1.17) P < 0.001, C = 0.70 | 1.12 (1.05–1.19) P < 0.001, C = 0.71 |
Model 1: Adjusted for field center + child age, sex, pubertal status (Tanner stage 1, 2/3, 4/5, sex × Tanner stage interaction) + maternal variables at pregnancy OGTT (age, height, mean arterial pressure, parity [0, 1+], smoking [yes/no], drinking [yes/no], gestational age), child’s family history of diabetes in first-degree relatives. Model 2: model 1 + maternal BMI at pregnancy OGTT. Model 3: model 1 + child’s BMI z score. Model 4: model 1 + maternal BMI at pregnancy OGTT + child’s BMI z score.
*β-Values for child continuous outcomes are reported for maternal fasting, 1-h, and 2-h glucose values higher by 1 SD.
**ORs are reported for maternal fasting, 1-h, and 2-h glucose values higher by 1 SD.
Regarding child insulin resistance, continuous maternal FPG, 1-h and 2-h PG, and the sum of glucose z scores were inversely associated with child Matsuda index (i.e., associated with greater insulin resistance) (Table 1). Adjusting for maternal BMI or child BMI z score in models 2–4 attenuated associations with the Matsuda index, but all associations remained significant. Regarding child insulin secretion, maternal FPG was not associated with the insulinogenic index after adjusting for maternal BMI and/or child BMI z score (models 2–4). However, maternal 1-h PG was inversely associated with the child insulinogenic index in all models, and maternal 2-h PG was inversely associated with the insulinogenic index after adjusting for child BMI z score alone or together with maternal BMI (models 3 and 4). Maternal sum of glucose z scores was inversely associated with child insulinogenic index only after adjusting for maternal BMI alone or together with child BMI z score (models 2 and 4). Regarding child β-cell function, maternal FPG was not significantly associated with disposition index, but maternal 1-h and 2-h glucose and the sum of OGTT z scores were inversely associated with the child disposition index in all four models. Although interaction terms between maternal glucose levels and Tanner stage were not statistically significant, exploratory analyses within the Tanner stage suggested some associations may be strongest after onset of puberty (Supplementary Table 3).
Associations Between Continuous Maternal Glycemia and Dichotomous Child Glucose Outcomes
Associations of continuous maternal FPG, 1-h, and 2-h PG and the sum of glucose z scores from the maternal OGTT with child IFG and IGT were examined next (Table 1). Maternal FPG and maternal sum of glucose z scores during pregnancy were associated with child IFG. Neither maternal 1-h nor 2-h PG was associated with child IFG. In contrast, maternal FPG was not associated with child IGT, but maternal 1-h and 2-h PG and the sum of glucose z scores were associated with IGT. Adjustment for maternal BMI and/or child BMI z score did not attenuate observed associations. Interaction terms between maternal glucose levels and Tanner stage were not statistically significant, but exploratory analyses within Tanner stage again suggested associations may be strongest for IGT after onset of puberty (Supplementary Table 4).
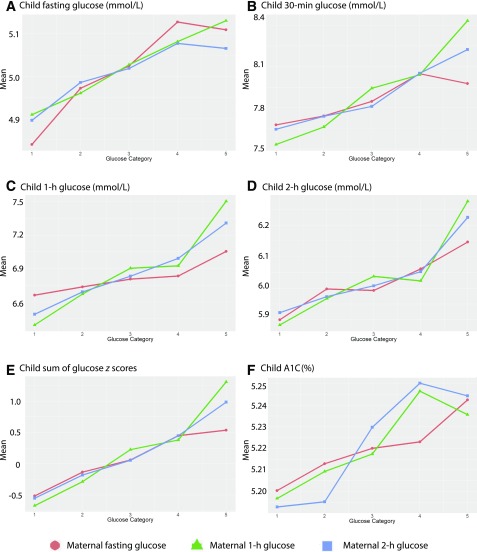
Associations Between Categorical Maternal Glycemia and Child Glucose Outcomes
Subsequent analyses examined individual child glucose and A1C levels during the HAPO FUS OGTT across categories of maternal FPG, 1-h, and 2-h PG during pregnancy. The highest maternal glucose category at each time point represents the threshold for GDM diagnosis using IADPSG criteria. Means of child fasting, 30-min, 1-h, and 2-h PG, A1C, and the sum of glucose z scores were generally higher across increasing categories of maternal fasting, 1-h, and 2-h PG during pregnancy. Differences in group means adjusted for model 1–4 covariates confirmed linear trends (Fig. 1 and Supplementary Table 5).
Figure 1.
Child glucose levels across categories of maternal glucose levels. Mean levels of child fasting (A), 30-min (B), 1-h (C), and 2-h (D) glucose levels, sum of glucose z scores (E) and A1C (F) across categories of fasting, 1-h, and 2-h PG are shown. Glucose categories are defined as follows: fasting PG level—category 1, <4.2 mmol/L; category 2, 4.2–4.4 mmol/L; category 3, 4.5–4.7 mmol/L; category 4, 4.8–5.0 mmol/L; and category 5, ≥5.1 mmol/L; 1-h PG level—category 1, ≤5.8 mmol/L; category 2, 5.9–7.3 mmol/L; category 3, 7.4–8.6 mmol/L; category 4, 8.7–9.9 mmol/L; and category 5, ≥10.0 mmol/L; and 2-h PG level—category 1, ≤5.0 mmol/L; category 2, 5.1–6.0 mmol/L; category 3, 6.1–6.9 mmol/L; category 4, 7.0–8.4 mmol/L; and category 5, ≥8.5 mmol/L.
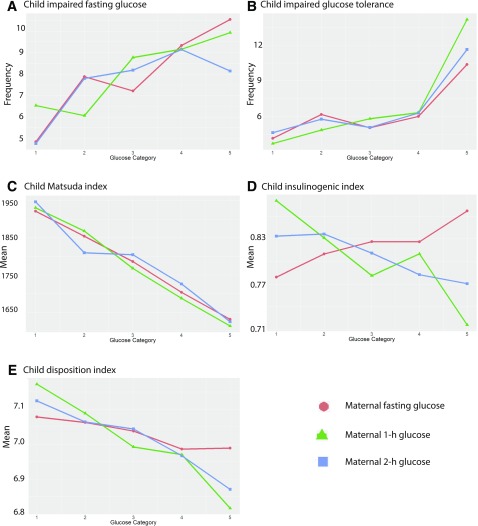
Child insulin sensitivity and disposition index decreased across categories of maternal fasting, 1-h, and 2-h PG during the pregnancy OGTT (Fig. 2). Adjusted mean differences in models 1–4 confirmed linear trends between maternal glucose predictors and these child outcomes (Supplementary Table 6). There was no clear pattern for child insulinogenic index across maternal glucose categories.
Figure 2.
Child glucose outcomes across categories of maternal glucose levels. The frequency of childhood IFG (A) and IGT (B) and means of the Matsuda index (C), insulinogenic index (D), and disposition index (E) across categories of fasting, 1-h, and 2-h PG is shown. Glucose categories are defined as follows: fasting PG level—category 1, <4.2 mmol/L; category 2, 4.2–4.4 mmol/L; category 3, 4.5–4.7 mmol/L; category 4, 4.8–5.0 mmol/L; and category 5, 5.1 mmol/L or more; 1-h PG level—category 1, 5.8 mmol/L or less; category 2, 5.9–7.3 mmol/L; category 3, 7.4–8.6 mmol/L; category 4, 8.7–9.9 mmol/L; and category 5, ≥10.0 mmol/L; and 2-h PG level—category 1, ≤5.0 mmol/L; category 2, 5.1–6.0 mmol/L; category 3, 6.1–6.9 mmol/L; category 4, 7.0–8.4 mmol/L; and category 5, ≥8.5 mmol/L.
The frequency of child IFG increased, in general, across maternal glucose categories with a doubling in frequency across the lowest and highest categories of maternal FPG (4.9% vs. 10.5%) (Fig. 2 and Supplementary Table 7). All categories of maternal FPG were significantly associated with child IFG in the fully adjusted model (model 4). Maternal 1-h PG levels were not associated with child IFG. For maternal 2-h PG, the middle three categories were significantly different from the lowest reference category with similar odds ratios (ORs). The highest category of maternal 2-h PG was not significantly different from the reference category.
The frequency of child IGT was higher across increasing categories of maternal glucose, consistent with the linear associations confirmed in logistic regression models (Fig. 2). The highest categories of maternal FPG and 2-h PG demonstrated significant differences relative to the lowest reference categories. For maternal 1-h PG, the three highest categories of maternal 1-h PG were significantly different from the lowest reference category (Supplementary Table 7).
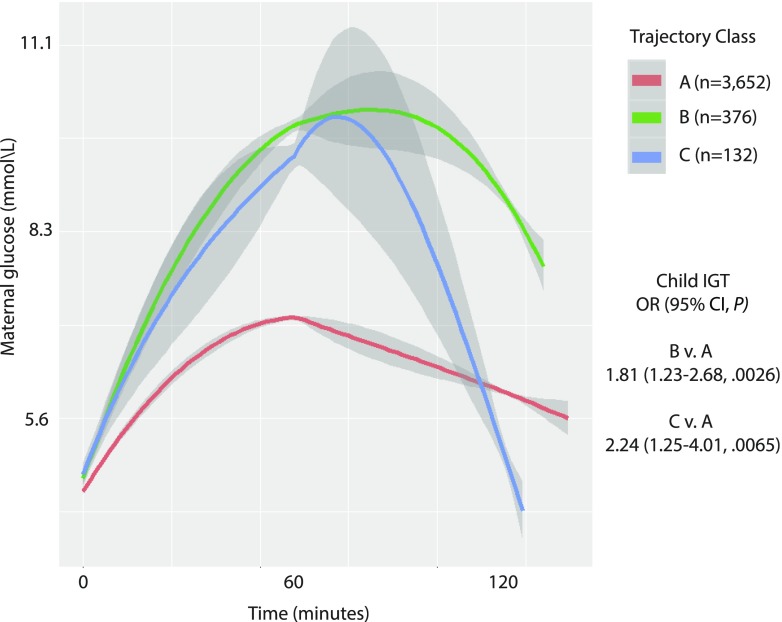
Maternal OGTT Glucose Trajectories and Childhood Glucose Outcomes
Trajectory analyses were performed to identify associations of overall maternal glucose response patterns during the HAPO OGTT with child outcomes. Analyses indicated best fit of quadratic trajectories adjusted for maternal BMI at OGTT with three estimated latent classes (Fig. 3). The largest class, class A, included 87.8% (3,652 of 4,160) of HAPO maternal OGTTs and reflects normal glucose tolerance. A second class, class B, included 9.0% (376 of 4,160) of HAPO OGTTs with high 1-h and 2-h PG values. Class C included 3.2% (132 of 4,160) of HAPO OGTTs with high 1-h PG and marked decline at 2-h. Estimated glucose response classes demonstrated associations with child IGT with ORs (95% CI) of 1.81 (1.23–2.68, P = 0.0026) for class B versus A and 2.24 (1.25–4.01, P = 0.0065) for class C versus A, after adjustment for model 4 covariates. Although the CIs for classes B and C relative to class A overlapped, OR estimates indicated a possible trend of higher risk of IGT for children with maternal pregnancy OGTT trajectories in class C. Trajectory classes were not associated with child IFG.
Figure 3.
Estimated latent class trajectories of maternal glucose levels from the HAPO OGTT during pregnancy. Best fit trajectories included a quadratic term and adjustment for maternal BMI during pregnancy and estimated three latent classes: class A (87.8% [3,652 of 4,160]), class B (9.0% [376 of 4,160]), and class C (3.2% [132 of 4,160]). OR (95% CIs) for IGT, in addition to maternal pregnancy BMI already included in trajectory estimates, included adjustments for all other model 4 covariates.
Conclusions
We recently demonstrated association of GDM based on IADPSG criteria with child glucose levels, insulin sensitivity, disposition index, and frequency of IGT (11). The current study demonstrates that the relationship between maternal glucose levels during pregnancy and child glucose levels and related outcomes was generally linear across the spectrum of glucose levels, including levels below those diagnostic of GDM. This included a positive relationship of maternal FPG and the sum of glucose z scores during the pregnancy OGTT with child FPG and IFG and of maternal 1-h and 2-h PG, A1C, and the sum of glucose z scores with child IGT and glucose levels during the child OGTT. Maternal 1-h and 2-h PG and the sum of glucose z scores also exhibited a continuous inverse relationship with child insulin sensitivity and disposition index. This is similar to the continuous relationship between maternal glucose levels during pregnancy and newborn outcomes demonstrated in HAPO (12) and to a related analysis in the HAPO FUS cohort demonstrating higher frequencies of childhood obesity and measures of adiposity across increasing categories of maternal fasting, 1-h, and 2-h PG during the HAPO pregnancy (27). A positive association of maternal third trimester postchallenge glucose levels in Pima Indians with offspring fasting and 2-h glucose levels at ages 10–14 years and type 2 diabetes as young adults has also been reported (10). Together, these results could have important implications for target maternal glucose levels during pregnancy in the setting of GDM or other metabolic disturbances.
Child adiposity, which is partly dependent on maternal adiposity (28,29), affects insulin sensitivity and glucose metabolism (30). However, adjustment for maternal BMI and/or child BMI z score did not attenuate associations of maternal glucose levels with child glucose outcomes, except for insulin sensitivity, although this association also remained significant after adjustment. These findings stand in contrast to marked attenuation of the association of GDM with child adiposity outcomes, including obesity, after adjusting for maternal BMI in the HAPO FUS cohort (14). Associations of maternal glucose with child glucose outcomes were also independent of the child’s family history of diabetes, although the associations of maternal FPG with child FPG and IFG and maternal 1-h and 2-h PG with child IGT suggest that shared genetics not captured by family history may have contributed to the associations. Beyond the contributions of shared genetics and postnatal environmental factors, the data are also consistent with a potential contribution of fetal programming.
The association of maternal glucose levels with child glucose outcomes was most evident for insulin sensitivity and disposition index compared with insulin secretion. The inverse association with child insulin sensitivity is consistent with previous studies demonstrating an association of maternal diabetes with child insulin resistance (31,32). The inverse association of maternal glucose levels with the child disposition index represents inadequate β-cell compensation for the insulin resistance in children exposed to higher levels of glucose in utero. In children, insulin resistance is an early finding in those with abnormal glucose metabolism (33), whereas children and adults with a low disposition index are most likely to progress to type 2 diabetes (19,34–38). Thus, children exposed in utero to higher levels of glucose may be at higher risk for progression to type 2 diabetes over time.
Using trajectory analyses to examine associations of glucose response patterns during the pregnancy OGTT with offspring outcomes was novel. A recent analysis of glucose levels during an OGTT in nonpregnant adults identified groups with trajectory classes similar to the three classes identified here (39). Individuals with curves similar to class C had lower first-phase insulin secretion and insulin sensitivity but greater insulin secretion overall. Individuals with a curve similar to class B were most insulin resistant and had impaired insulin secretion. A second study of nonpregnant adults showed that those with a curve similar to class C had a higher risk of future type 2 diabetes compared with those with a curve similar to class A (40), whereas those with a curve similar to class B had an even higher risk of type 2 diabetes as well as future cardiovascular disease. These data are consistent with the higher risk for IGT in offspring of women in classes B and C observed in the current study. The long-term type 2 diabetes risk associated with a pattern similar to class C and risk for child IGT with high 1-h PG observed in the current study demonstrate the importance of the maternal 1-h glucose level separate from other values and provide a rationale for its inclusion during the pregnancy OGTT.
This study has several strengths. First, HAPO was a blinded observational study in which both caregivers and mothers were not aware of maternal glucose levels, and thus, child outcomes were not confounded by treatment of maternal hyperglycemia. Second, HAPO included mothers with glucose values during pregnancy across the spectrum of maternal glycemia lower than those diagnostic of diabetes. Third, the HAPO and HAPO FUS cohorts included participants from multiple races and ethnicities around the world, making the results broadly applicable.
There are some limitations. First, the proportion of participants who met IADPSG GDM criteria and participated in the HAPO FUS (weighted estimate 14.9%) is lower than in all eligible participants (16.2%). Second, we were unable to completely diagnose IGT in all participants because of some missing 2-h PG measurements. Participants missing a 2-h PG value who had a normal FPG were defined as normal; thus, the number of individuals with IGT may have been underestimated. Third, participants with fasting and/or 2-h OGTT PG values during the HAPO pregnancy that were above predefined thresholds were unblinded during HAPO and excluded from the HAPO FUS. This subgroup (1.8% of the HAPO cohort) would likely include children at highest risk of altered glucose metabolism. Fourth, paternal BMI data were not available, and paternal diabetes data were limited to family history. Finally, the study was not powered to examine Tanner stage–specific associations.
In summary, the current study demonstrates that maternal glucose levels during pregnancy across the spectrum are associated with higher glucose levels and insulin resistance during childhood independent of maternal and child BMI and family history of diabetes and that this relationship is continuous. Although the underlying causes for the increasing prevalence of type 2 diabetes in children are complex, these findings suggest that maternal glycemia may also contribute.
Supplementary Material
Article Information
Acknowledgments. The HAPO FUS investigators are grateful for all mothers and children who participated in HAPO and HAPO FUS.
Funding. The HAPO FUS is funded by grant 1U01-DK-094830 from the National Institute of Diabetes, Digestive, and Kidney Diseases and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The HAPO Study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants R01-HD-34242 and R01-HD-34243). HAPO FUS data were collected and managed using REDCap electronic data capture tools hosted at Northwestern University Feinberg School of Medicine. REDCap is supported at Feinberg School of Medicine by the Northwestern University Clinical and Translational Science Institute. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences (grant UL1-TR-001422).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. D.M.S. researched the literature; designed the study; acquired, analyzed, and interpreted the data; and wrote the manuscript and figures. A.K. analyzed the data. L.P.L., W.L.L., and B.E.M. conceived and designed the study, researched the literature, assisted with data collection, interpreted the data, and wrote the manuscript. J.H. researched the literature, acquired the data, and wrote the manuscript. J.M.L., Y.L., W.J.B., P.C., R.C.M., D.M., and W.H.T. acquired data and participated in writing the manuscript. P.M.C. conceived and designed the study, acquired and interpreted the data, and wrote the manuscript. B.L. designed the study, interpreted the data, and wrote the manuscript. A.R.D. designed the study, acquired and interpreted the data, and wrote the manuscript. D.M.S. and B.E.M. are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-2021/-/DC1.
A complete list of the HAPO Follow-up Study Cooperative Research Group can be found in the Supplementary Data online.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This article is part of a special article collection available at http://care.diabetesjournals.org/gdm-new-evidence.
Contributor Information
Collaborators: HAPO Follow-Up Study Cooperative Research Group, Chaicharn Deerochanawong, Thadchanan Tanaphonpoonsuk, Sukeeta Binratkaew Uraiwan Chotigeat, Wanee Manyam, Martinette Forde, Andre Greenidge, Kathleen Neblett, Paula Michele Lashley, Desiree Walcott, Katie Corry, Loraine Francis, Jo-anne Irwin, Anne Langan, David R. McCance, Maureen Mousavi, Ian Young, Jennifer Gutierrez, Jennifer Jimenez, Jean M. Lawrence, David A. Sacks, Harpreet S. Takhar, Elizabeth Tanton, Wendy J. Brickman, Jennifer Howard, Jami L. Josefson, Lauren Miller, Jacqui Bjaloncik, Patrick M. Catalano, Ajuah Davis, Michaela Koontz, Larraine Presley, Shoi Smith, Amanda Tyhulski, Albert Martin Li, Ronald C. Ma, Risa Ozaki, Wing Hung Tam, Michelle Wong, Cindy Siu Man Yuen, Peter E. Clayton, Aysha Khan, Avni Vyas, Michael Maresh, Hadasse Benzaquen, Naama Glickman, Alona Hamou, Orna Hermon, Orit Horesh, Yael Keren, Yael Lebenthal, Shlomit Shalitin, Kristina Cordeiro, Jill Hamilton, Hahn Y. Nguyen, Shawna Steele, Fei Chen, Alan R. Dyer, Wenyu Huang, Alan Kuang, Maria Jimenez, Lynn P. Lowe, William L. Lowe, Jr, Boyd E. Metzger, Michael Nodzenski, Anna Reisetter, Denise Scholtens, Octavious Talbot, Paul Yim, David Dunger, Alicia Thomas, Mary Horlick, Barbara Linder, Aynur Unalp-Arida, and Gilman Grave
References
- 1.Hannon TS, Arslanian SA. The changing face of diabetes in youth: lessons learned from studies of type 2 diabetes. Ann N Y Acad Sci 2015;1353:113–137 [DOI] [PubMed] [Google Scholar]
- 2.Nadeau KJ, Anderson BJ, Berg EG, et al. Youth-onset type 2 diabetes consensus report: current status, challenges, and priorities. Diabetes Care 2016;39:1635–1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Viner R, White B, Christie D. Type 2 diabetes in adolescents: a severe phenotype posing major clinical challenges and public health burden. Lancet 2017;389:2252–2260 [DOI] [PubMed] [Google Scholar]
- 4.Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayer-Davis EJ, Lawrence JM, Dabelea D, et al.; SEARCH for Diabetes in Youth Study . Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med 2017;376:1419–1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–2642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metzger BE. Long-term outcomes in mothers diagnosed with gestational diabetes mellitus and their offspring. Clin Obstet Gynecol 2007;50:972–979 [DOI] [PubMed] [Google Scholar]
- 8.Pettitt DJ, Aleck KA, Baird HR, Carraher MJ, Bennett PH, Knowler WC. Congenital susceptibility to NIDDM. Role of intrauterine environment. Diabetes 1988;37:622–628 [DOI] [PubMed] [Google Scholar]
- 9.Silverman BL, Rizzo TA, Cho NH, Metzger BE; The Northwestern University Diabetes in Pregnancy Center . Long-term effects of the intrauterine environment. Diabetes Care 1998;21(Suppl. 2):B142–B149 [PubMed] [Google Scholar]
- 10.Franks PW, Looker HC, Kobes S, et al. Gestational glucose tolerance and risk of type 2 diabetes in young Pima Indian offspring. Diabetes 2006;55:460–465 [DOI] [PubMed] [Google Scholar]
- 11.Lowe WL Jr, Scholtens DM, Kuang A, et al. ; HAPO Follow-up Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS): maternal gestational diabetes mellitus and childhood glucose metabolism. Diabetes Care 2019;42:372–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metzger BE, Lowe LP, Dyer AR, et al.; HAPO Study Cooperative Research Group . Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:1991–2002 [DOI] [PubMed] [Google Scholar]
- 13.Metzger BE, Gabbe SG, Persson B, et al.; International Association of Diabetes and Pregnancy Study Groups Consensus Panel . International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowe WL Jr, Scholtens DM, Lowe LP, et al.; HAPO Follow-Up Study Cooperative Research Group . Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA 2018;320:1005–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manley SE, Stratton IM, Clark PM, Luzio SD. Comparison of 11 human insulin assays: implications for clinical investigation and research. Clin Chem 2007;53:922–932 [DOI] [PubMed] [Google Scholar]
- 16.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999;22:1462–1470 [DOI] [PubMed] [Google Scholar]
- 17.Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med 1994;11:286–292 [DOI] [PubMed] [Google Scholar]
- 18.Weiss R, Cali AM, Dziura J, Burgert TS, Tamborlane WV, Caprio S. Degree of obesity and glucose allostasis are major effectors of glucose tolerance dynamics in obese youth. Diabetes Care 2007;30:1845–1850 [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes—2017. Diabetes Care 2017;40(Suppl. 1):S11–S2427979889 [Google Scholar]
- 20.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012;7:284–294 [DOI] [PubMed] [Google Scholar]
- 21.Harrell FE Jr. rms: regression modeling strategies R package version 51-2 [Internet], 2018. Available at https://cran.r-project.org/web/packages/rms/index.html. Accessed 15 June 2018
- 22.R Core Team A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing, 2016 [Google Scholar]
- 23.Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. J Stat Softw 2017;78:1–56 [Google Scholar]
- 24.Muthén B. Latent variable mixture modeling. In New Developments and Techniques in Structural Equation Modeling. Marcoulides GA, Schumacker RE, Eds. Mahwah, NJ, Lawrence Erlbaum, 2001, p. 1–33 [Google Scholar]
- 25.Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling 2007;14:535–569 [Google Scholar]
- 26.Yang CC. Evaluating latent class analysis models in qualitative phenotype identification. Comput Stat Data Anal 2006;50:1090–1104 [Google Scholar]
- 27.Lowe WL Jr, Lowe LP, Kuang A, et al. ; HAPO Follow-up Study Cooperative Research Group. Maternal glucose levels during pregnancy and childhood adiposity in the Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study. Diabetologia. 15 January 2019. [Epub ahead of print]. DOI: 10.1007/s00125-018-4809-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Philipps LH, Santhakumaran S, Gale C, et al. The diabetic pregnancy and offspring BMI in childhood: a systematic review and meta-analysis. Diabetologia 2011;54:1957–1966 [DOI] [PubMed] [Google Scholar]
- 29.Zhao P, Liu E, Qiao Y, et al.; ISCOLE Research Group . Maternal gestational diabetes and childhood obesity at age 9-11: results of a multinational study. Diabetologia 2016;59:2339–2348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss R, Kaufman FR. Metabolic complications of childhood obesity: identifying and mitigating the risk. Diabetes Care 2008;31(Suppl. 2):S310–S316 [DOI] [PubMed] [Google Scholar]
- 31.Bush NC, Chandler-Laney PC, Rouse DJ, Granger WM, Oster RA, Gower BA. Higher maternal gestational glucose concentration is associated with lower offspring insulin sensitivity and altered beta-cell function. J Clin Endocrinol Metab 2011;96:E803–E809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lacroix M, Kina E, Hivert MF. Maternal/fetal determinants of insulin resistance in women during pregnancy and in offspring over life. Curr Diab Rep 2013;13:238–244 [DOI] [PubMed] [Google Scholar]
- 33.Chen ME, Chandramouli AG, Considine RV, Hannon TS, Mather KJ. Comparison of β-cell function between overweight/obese adults and adolescents across the spectrum of glycemia. Diabetes Care 2018;41:318–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abdul-Ghani MA, Williams K, DeFronzo RA, Stern M. What is the best predictor of future type 2 diabetes? Diabetes Care 2007;30:1544–1548 [DOI] [PubMed] [Google Scholar]
- 35.Holder T, Giannini C, Santoro N, et al. A low disposition index in adolescent offspring of mothers with gestational diabetes: a risk marker for the development of impaired glucose tolerance in youth. Diabetologia 2014;57:2413–2420 [DOI] [PubMed] [Google Scholar]
- 36.Lorenzo C, Wagenknecht LE, Rewers MJ, et al. Disposition index, glucose effectiveness, and conversion to type 2 diabetes: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 2010;33:2098–2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cali AM, Man CD, Cobelli C, et al. Primary defects in beta-cell function further exacerbated by worsening of insulin resistance mark the development of impaired glucose tolerance in obese adolescents. Diabetes Care 2009;32:456–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Utzschneider KM, Prigeon RL, Faulenbach MV, et al. Oral disposition index predicts the development of future diabetes above and beyond fasting and 2-h glucose levels. Diabetes Care 2009;32:335–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hulman A, Witte DR, Vistisen D, et al. Pathophysiological characteristics underlying different glucose response curves: a latent class trajectory analysis from the prospective EGIR-RISC study. Diabetes Care 2018;41:1740–1748 [DOI] [PubMed] [Google Scholar]
- 40.Hulman A, Vistisen D, Glümer C, Bergman M, Witte DR, Færch K. Glucose patterns during an oral glucose tolerance test and associations with future diabetes, cardiovascular disease and all-cause mortality rate. Diabetologia 2018;61:101–107 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.