ABSTRACT
Objective
To evaluate the Programa Mais Médicos (More Doctors Program; PMM) in Brazil by estimating the proportional increase in the number of doctors in participating municipalities and the program costs, stratified by cost component and funding source.
Methods
Official data from the 2013 edition of Demografia Médica no Brasil (Medical Demography in Brazil) was used to estimate the number of doctors prior to PMM. The number of doctors at the end of the fourth PMM recruiting cycle (July 2014) was obtained from the Ministry of Health. Cost components were identified and estimated based on PMM legislation and guidelines. The participating municipalities were chosen based on four criteria, all related to vulnerability.
Results
The PMM provided an additional 14 462 physicians to highly vulnerable, remote areas in 3 785 municipalities (68% of the total) and 34 Special Indigenous Sanitary Districts. There was a greater increase of physicians in the poorest regions (North and Northeast). The estimated annual cost of US$ 1.1 billion covered medical provision, continuing education, and supervision/mentoring. Funding was largely centralized at the federal level (92.6%).
Conclusion
The cost of PMM is considered relatively moderate in comparison to its potential benefits for population health. The greater increase of doctors for the poorest and most vulnerable met the target of correcting imbalances in health worker distribution. The PMM experience in Brazil can contribute to the debate on reducing physician shortages.
Keywords: Costs and cost analysis, delivery of health care, medically underserved areas, health economics, Brazil
RESUMEN
Objetivo
Evaluar el Programa “Mais Médicos” en el Brasil mediante el cálculo del aumento proporcional del número de médicos en los municipios participantes y los costos del programa, con estratificación por componente del costo y fuente de financiamiento.
Métodos
Se utilizaron datos oficiales de la edición del 2013 de Demografia médica no Brasil [demografía médica en el Brasil] para calcular el número de médicos antes del Programa “Mais Medicos”. El número de médicos al final del cuarto ciclo de reclutamiento del programa (julio del 2014) se obtuvo del Ministerio de Salud. Se determinaron y calcularon los componentes de costos sobre la base de la legislación y las directrices del programa. Se eligieron los municipios participantes según cuatro criterios, todos relacionados con la vulnerabilidad.
Resultados
Mediante el Programa “Mais Médicos” se destinaron 14 462 médicos más a zonas sumamente vulnerables y remotas en 3 785 municipios (68% del total) y 34 distritos sanitarios indígenas especiales. El aumento del número de médicos fue mayor en las zonas más pobres (al Norte y Nordeste). El costo anual estimado de US$ 1 100 millones incluyó la dotación de médicos, la educación continua y la supervisión y tutoría. El financiamiento estuvo principalmente centralizado en el nivel federal (92,6%).
Conclusiones
Se considera que el costo del Programa “Mais Médicos” es relativamente moderado en relación con los posibles beneficios para la salud de la población. Con el mayor aumento de la dotación de médicos en las poblaciones más pobres y vulnerables se cumplió el objetivo de corregir los desequilibrios en la distribución del personal de salud. La experiencia de este programa en el Brasil puede contribuir al debate sobre cómo paliar la escasez de médicos.
Palabras clave: Costos y análisis de costo, prestación de atención de salud, áreas sin atención médica, economía de la salud, Brasil
RESUMO
Objetivo
Avaliar o Programa Mais Médicos (PMM) no Brasil estimando o aumento proporcional do número de médicos nos municípios participantes e os custos do programa, estratificado pelo componente de custo e fonte de financiamento.
Métodos
Os dados oficiais da edição de Demografia médica no Brasil de 2013 foram usados para estimar o número de médicos anterior ao PMM. O número de médicos ao final do quarto ciclo de recrutamento do PMM (julho de 2014) foi fornecido pelo Ministério da Saúde. Os componentes de custo foram identificados e calculados de acordo com a legislação e as diretrizes do PMM. Os municípios participantes foram selecionados segundo quatro critérios relacionados à vulnerabilidade.
Resultados
O PMM proveu um adicional de 14.462 médicos para áreas remotas bastante vulneráveis em 3.785 municípios (68% do total) e 34 distritos sanitários especiais indígenas. Houve aumento maior do número de médicos nas regiões mais pobres (Norte e Nordeste). O custo anual estimado de US$ 1,1 bilhão cobriu provisões médicas, educação continuada e supervisão/mentoria. O financiamento foi em grande parte centralizado ao nível federal (92,6%).
Conclusão
Considera-se que o custo do PMM seja relativamente moderado em relação aos benefícios em potencial à saúde da população. O aumento maior no número de médicos para atender a população mais pobres e vulnerável alcançou a meta de corrigir a má distribuição de profissionais da saúde. A experiência do PMM no Brasil pode subsidiar o debate visando reduzir a escassez de médicos.
Palavras-chave: Custos e análise de custo, assistência à saúde, área carente de assistência médica, economia da saúde, Brasil
There is an estimated shortage of 4 million health workers worldwide (1), a gap that affects both developed and developing countries (2 – 5). Imbalances in health worker distribution are greater in rural and remote areas and the rural-urban fringe (6). Overcoming the problem of health worker shortages requires a wide range of actions and involvement of numerous stakeholders, within and beyond the health sector (7). A systematic review of strategies that aim to attract and retain health workers in rural and remote areas found that most focused on educational programs and few on programs that use financial incentives and personal and professional support (8).
In order to address physician shortages in remote, highly vulnerable areas, the Government of Brazil implemented the Programa Mais Médicos (PMM; More Doctors Program) in 2013 through Law 12 871 (9). PMM consists of three strategic actions: (i) professional qualification by increasing medical school enrollment and implementing new curricular guidelines to improve training in primary, urgent, and emergency care; (ii) investment in health care infrastructure and improving Basic Health Care Units; and (iii) supplying doctors to vulnerable municipalities (10). Alternative strategies implemented before the PMM include the Program for the Enhancement of Primary Care; however, its scope and coverage were far lower (11). Under the PMM, by July 2014, a total of 14 462 physicians had been allocated to 3 785 Brazilian municipalities. To the best of our knowledge, this is the world's largest public intervention aimed at increasing the number of primary care physicians in vulnerable and rural areas in a developing country. It reached approximately 50 million people during its first year. Other countries have implemented similar programs. With the exception of Venezuela, whose 14-year Misión Barrio Adentro (Into the Neighborhood Mission) initiative involved 15 420 doctors, the number of professionals recruited in other countries has been far lower than in Brazil. For example, in Australia, 549 doctors were recruited for primary care in 2015; and in Angola, 1 893 Cuban doctors in 2014 (12).
To ensure comprehensive health care, the Ministry of Health of Brazil established the following PMM priority criteria for eligible municipalities: (i) more than 20% of the population living in extreme poverty; (ii) being one of the 100 municipalities with more than 80 000 inhabitants, low levels of public investment in health per capita, and high social vulnerability; (iii) shelter an Indigenous Health District an Indigenous Health District; and (iv) having areas among the 40% of census tracts with the highest percentage of the population living in extreme poverty, among others.
This article contributes to the debate on strategies to attract and retain doctors in remote and vulnerable areas by analyzing the implementation of the PMM in Brazil, and included two dimensions that are poorly documented in the literature. The first was measuring the increased number of doctors in municipalities participating in the PMM in order to determine whether the program was contributing to reducing regional imbalances in the distribution of health care professionals. The second involved estimating the cost of PMM, stratified by cost component and funding source, to calculate the average cost per doctor allocated. Based on these objectives, this study sought to determine the cost of implementing policies aimed at providing primary care physicians, with a view to ensuring comprehensive care.
MATERIALS AND METHODS
Study setting
Brazil is divided into three levels of autonomous governments: municipalities/counties at the local level; states at the intermediate subnational level; and the Union, representing the national government. All of these levels of government fund the Sistema Único de Saúde (the Unified Health System; SUS), Brazil's public health system. Created by the Federal Constitution of 1988, the SUS ensures the right of all Brazilians to health care. Governed by the principles of decentralization and social participation, the SUS is a single-payer system that provides universal, egalitarian, and comprehensive health care aimed at meeting the health needs of the entire population (13). In this respect, the primary community-based intervention is the Family Health Program, more recently renamed the Family Health Strategy (FHS), which delivers a set of individual and collective health actions, including health promotion and protection, disease prevention, diagnosis, treatment, rehabilitation, harm reduction, and health maintenance (14). FHS teams are composed of at least one physician, one nurse, one nursing assistant, and four – six full-time community health agents (15). Ministry of Health data show that 55.4% (113 181 649 individuals) of Brazilians had primary care coverage in 2016 at 40 044 basic health units (16).
The distribution of doctors in Brazil has consistently shown inequalities in a number of aspects. The first is among geographic regions, with the North and Northeast having a lower density compared to other more developed parts of the country (South, Southeast, and Central-West). Second, the private sector (out-of-pocket and health insurance) comprises 43.5% of the doctors in Brazil, but covers only 25% of the population. Third, the family and community medicine specialty accounts for only 1.21% of all specialists in the country, reflecting the lack of interest in primary care (17).
When the PMM was founded in 2013, the Ministry of Health attempted to recruit doctors who were already registered with a Brazilian medical council. Since the number of candidates was far fewer than the number of positions offered, the criteria were broadened to include Brazilian and foreign doctors with a diploma obtained abroad (not validated in Brazil) (18). The cooperation agreement signed with the Pan American Health Organization/World Health Organization (PAHO/WHO) was crucial in providing around 12 000 doctors from the Ministry of Public Health of Cuba.
Regarding the characteristics of the 3 785 municipalities selected for PMM participation, 35.2% were classified as having 20% or more residents living in extreme poverty; 2.5% as G-100 (among the 100 municipalities with a population living in extreme poverty, low levels of per capita government revenue, and high social vulnerability); 9.9% as large metropolitan areas; and 0.7% were the capitals of their municipalities. The remaining municipalities did not fit into any of these categories (19).
Study design
This paper analyzes the implementation of the PMM to provide doctors in highly vulnerable remote areas and the costs incurred by the Government of Brazil over a 1-year period (2014). Information on the number of physicians and their respective work locations was obtained from the Ministry of Health for the fourth recruitment cycle (July 2014), totaling 14 462 doctors distributed among 3 785 Brazilian municipalities and Indigenous Health Districts. Since there was no publicly available information on the actual amounts spent by the Government of Brazil, cost components were identified and estimated based on legislation and PMM guidelines. In this respect, estimates include funds spent by the Ministry of Health and the Ministry of Education, as well as the Brazilian municipalities that were assigned physicians in 2014.
Supplying doctors to rural and remote locations
To determine the increase in physician density in Brazilian municipalities participating in the PMM, the proportional differences between the following were calculated: (i) the number of doctors per 1 000 inhabitants in the 5 570 municipalities prior to the program's implementation (baseline), according to the Medical Demography in Brazil (17); and (ii) the number of doctors per 1 000 inhabitants in these municipalities at the end of the program's fourth recruitment cycle (July 2014), adding the baseline figures to those obtained from official Ministry of Health records.
The Medical Demography in Brazil study (17) lacked any data on physician numbers in 28% of Brazilian municipalities, particularly those with small populations. To extrapolate for this missing data, the researchers imputed the regional medians (North, Northeast, Central-West, Southeast, and South) for five municipality categories (< 5 000 inhabitants; 5 001 – 10 000 inhabitants; 10 001 – 20 000 inhabitants; 20 001 – 50 000 inhabitants; > 50 000 inhabitants). Medians were used to prevent extreme values from biasing the data. The trend line was plotted and the result showed that the imputed data scarcely altered the distribution of values for the states. Since the Medical Demography was published, five new municipalities have been created. For the analysis, these new municipalities were assigned the same ratio of doctors per 1 000 inhabitants as their original.
Cost of the Programa Mais Médicos
An extensive set of rulings govern the PMM, including ordinances (established by the Ministries of Health and Education), decree-laws (set out by the Presidency of the Republic), and laws (approved by the National Congress). Of these, eight cost components relating to the PMM were identified (Table 1), as well as the methodology used to estimate their respective annual costs, based on 2014 prices (20). Minimum and maximum amounts were calculated for components subject to cost variations. Amounts were converted into United States dollars (US$) from Brazilian Reais (R$) using an exchange rate of US$ 1 = R$ 2.35, the average rate for 2014.
TABLE 1. Description of the cost components of the Programa Mais Médicos (More Doctors Program), Brazil, 2014.
| Cost component | Description | Total cost calculation formula | Variation | Funding source |
|---|---|---|---|---|
| Doctor's monthly earnings | US$ 4 473 tax free | The number of doctors (14 462) was multiplied by annual remuneration (US$ 53 683) | Not applicable | Ministry of Health |
| Relocation costs | Financial support to help doctors settle in the municipality, varying between US$ 4 255 and US$ 12 765 depending on the location the physician is allocated to | Municipalities were stratified into the categories established by the Ministry of Health | Not applicable | Ministries of Health and Education |
| Air and ground transport | Payment of airfares and ground transport costs from the country of origin to the doctor's allocated municipality, with additional payment for up to two financial dependents. | Average airfares of five airlines, excluding the highest amounts; for ground transport, we used the maximum fare coefficient applied to mileage. We assumed the inclusion of one financial dependent. | Lower limit: physician with no financial dependents Upper limit: two financial dependents. |
Ministry of Health |
| Living costs | Living cost assistance varies between US$ 213 and US$ 1 064 | Data from the 2008-2009 Household Expenditure Survey were used | Lower limit: US$ 213 Upper limit: US$ 1 064 |
Participating municipalities |
| Food costs | Food cost assistance varies between US$ 158 and US$ 213 | Data from the 2008-2009 Household Expenditure Survey were used | Lower limit: US$ 158 Upper limit: US$ 213 |
Participating municipalities |
| Monthly earnings for supervision | Tax-free monthly earnings of US$ 1 702 for permanent and continuous supervision of the participating physician | Annual earnings (US$ 20 426) were multiplied by the total number of supervisors (1 522 supervisors). | Lower limit: one supervisor for every 10 doctors (1 446) Upper limit: Six doctors per supervisor (2 410) | Ministry of Health |
| Monthly earnings for academic mentoring | Tax-free monthly earnings of US$ 2 128 as a mentor for the participating physician and to help plan supervision activities | Annual earnings (US$ 25 532) were multiplied by the total number of mentors (120) | Lower limit: one mentor for every 144 doctors (100) Upper limit: one mentor for every 100 doctors (144) |
Ministry of Health |
| Specialization course | Costs related to taking a specialization course, mandatory for all participating physicians | Contracts and agreements signed totaled US$ 43 319 149 | Not applicable | Ministries of Health and Education |
Note: The exchange rate used was US$ 1 = R$ 2.35 (Central Bank of Brazil, 2014).
Source: Prepared by the authors from the study data, including data taken from regulations for the Programa Mais Médicos. Data on the number of supervisors and mentors were taken from the report by the Court of Auditors, 8 May 2014, available from: http://portal3.tcu.gov.br/portal/page/portal/TCU/imprensa/noticias/noticias_arquivos/005.391-2014-8%20Mais%20M%C3%A9dicos.pdf
RESULTS
By July 2014, a total of 14 462 physicians had been assigned to highly vulnerable or remote areas, covering 3 785 municipalities (67.9% of Brazilian municipalities) and 34 Indigenous Health Districts. It is estimated that around 50 million people are being served by PMM doctors, in compliance with the Ministry of Health's recommendation that each health care team serve 3 450 inhabitants.
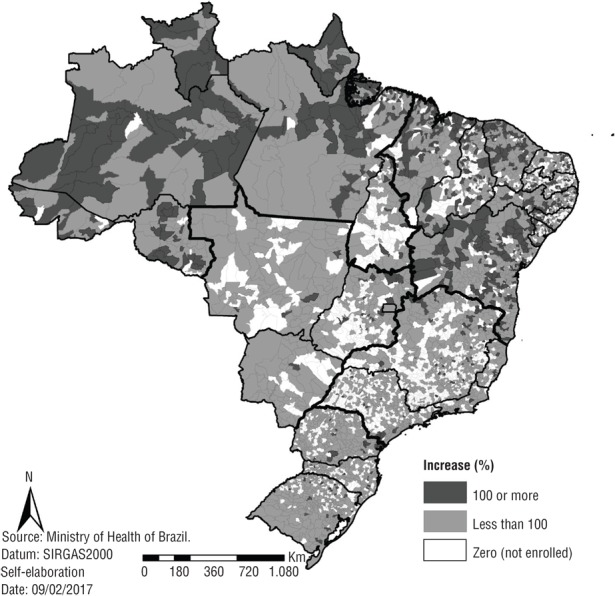
In participating municipalities, the average national increase in physician density per 1 000 inhabitants was 0.76 (standard deviation [SD] = 0.91), that is, there was a 76% increase in the availability of physicians in these areas. In regional terms, the North and Northeast benefitted the most from the increased number of doctors under the PMM, representing an average rise of 1.23 (SD = 1.36) and 1.10 (SD = 1.05), respectively, compared to the Central-West (average increase = 0.51; SD = 0.57), Southeast (average increase = 0.45; SD = 0.57) and South (average increase = 0.47; SD = 0.47). Figure 1 illustrates these regional differences, as well as non-participating municipalities.
FIGURE 1. Increase in doctors density after implementation of the Programa Mais Médicos (More Doctors Program), Brazil, 2014.
The total cost for 1 year of the PMM was estimated at US$ 1.1 billion, based on 2014 figures (Table 2). Doctor's earnings accounted for 70.5% of program costs, totaling US$ 776.4 million; the second highest expenditure was relocation assistance, accounting for just over 10% of the total (US$ 111 million). Air and ground transport represented the third highest cost, at slightly more than 5% of the total (US$ 56 million). This was largely due to the nationality of PMM doctors, most of whom were foreign; only 2 294 were Brazilians (nearly 15.9%). Cubans were the predominant nationality, accounting for 79.1% of physicians; 47 other nationalities participated minimally in the programs (5.02%).
TABLE 2. Estimated costs of the Programa Mais Médicos (More Doctors Program), Brazil, 2014.
| Cost component | Estimated cost (US$) |
|---|---|
| Doctors salaries | 776 370 131 |
| Relocation | 111 000 000 |
| Air and ground transportation | 56 022 656 |
| Living expenses | 51 193 482 |
| Food | 29 909 396 |
| Monthly earnings for supervision | 31 087 660 |
| Monthly earnings for academic mentoring | 3 063 830 |
| Specialty courses | 43 319 149 |
| TOTAL | 1 101 966 303 |
Note: The exchange rate used was US$ 1 = R$ 2.35 (Central Bank of Brazil, 2014).
Source: Prepared by the authors from the study data.
Taking into account the upper and lower limits of variable cost components, stipulated in PMM legal guidelines, estimated total costs would range between US$ 1.01 billion – US$ 1.28 billion. The average annual cost per physician was estimated at US$ 76 200 (ranging from US$ 69 960 – US$ 89 140), while estimated monthly expenditures were US$ 6 350 per doctor (US$ 5 830 – US$ 7 420). In terms of funding, federal resources (the Ministries of Health and Education) financed 92.6% of the program's total costs, while participating municipalities contributed with 7.4%. The total cost of the PMM corresponded to 0.04% of Brazil's Gross Domestic Product in 2014, and 1.1% of its total public health expenditure.
DISCUSSION
There was a greater increase in the number of doctors in the country's poor and vulnerable regions (North and Northeast), thereby meeting the target of correcting imbalances. These results are consistent with those of Nogueira and colleagues (21), who observed greater allocation of doctors to municipalities with lower Human Development Indices and less than 20 000 residents in the Northeast. However, these authors suggest there is room for improving the MPP by assigning more doctors to the semiarid regions (21).
A cross-sectional study conducted with a probability sample in two Northeastern cities in 2011 estimated that 16.2% of public health system users did not seek treatment, even when they needed it. The main reason given by interviewees (58.5%) was a lack of doctors (22).
The total cost for 2014 was estimated at US$ 1.1 billion, accounting for approximately US$ 6 000 a month per doctor. According to a survey by a market trends research group (Estação de Pesquisa de Sinais de Mercado; 23), more than 50% of physicians earned over 10 minimum monthly wages in 2010, corresponding to earnings of over R$ 7 880 (US$ 3 353), based on amounts for January 2015. However, this figure only represents remuneration for their primary duties; in addition, there is no information on workload, which was likely less than 40 hours a week. This same study found salaries exceeding R$ 10 000 (US$ 4 255) in 21% of the 739 municipalities that responded to the survey. It is important to note that these estimates are an average amount for Brazil and are heavily influenced by urban areas. Although salaries are higher in poor areas, physicians refuse to commit exclusively to one location and fail to comply with the stipulated working hours since they work under different contracts in several municipalities (24). Some municipalities offer monthly salaries of R$ 30 000 (US$ 12 766) or more. As such, it is difficult to make a comparative analysis between PMM and non-PMM salaries, due to the aforementioned characteristics of the medical workforce. Moreover, the cost of PMM per doctor could decrease across time if the Government of Brazil reduces the number of foreign recruits, thereby lowering the costs of international flights, specialization courses, supervision, and mentoring.
We believe that the PMM salaries are a good value for the money since many people from remote and highly vulnerable areas currently have access to primary health care. There is little evidence on the effectiveness of the PMM, since the program was implemented less than 3 years ago. However, numerous studies have highlighted positive patient perception in terms of satisfaction and the responsiveness of services provided by PMM doctors (25 – 31). One aspect heavily criticized by the Brazilian medical councils was the language barrier, arguing that many foreign doctors would not be proficient in Portuguese. Studies have questioned this argument, since 57% of patients reported no communication problem with foreign doctors and 32% cited few communication problems (25). Furthermore, a number of studies have demonstrated the high quality of care provided by PMM doctors, particularly Cubans, who spend more time on anamnesis and practice humanized clinical conduct, which better meets the health needs of the community (25, 26).
The model adopted in the first phase of the PMM was based on centralized federal funding (92.6% of the total funds). The decentralization of health care funding aims to facilitate the recruitment and retention of health workers in rural areas, in that it allows greater flexibility in hiring, defining contract periods, and establishing performance-based pay, in addition to exempting these contracts from the nationally established salary cap (32). Since the enactment of the 1988 Federal Constitution, Brazil has expanded the decentralization of health services and initiatives to subnational entities, giving states and municipalities greater autonomy (12). This is also reflected in the country's public health funding; in 2000, the Federal Government was responsible for 59.8% of the total public health expenditure, declining to 44.7% by 2011 (33). Nevertheless, decentralization has not overcome the physician shortage in vulnerable, remote areas. In January 2013, the National Mayor's Front (34) spearheaded a national movement to demand effective action from the Government of Brazil in supplying physicians, including the possibility of hiring foreign professionals. This led to the Federal Government's central role in funding the PMM.
In regard to long-term sustainability, the provision of doctors via the PMM was established as a temporary policy, valid for 3 years (renewable for an equal period), according to Law 12 871 of 22 October 2013 (9). Provisional Measure 723, issued on 29 April, 2016, extends the temporary visa period for foreign exchange medical doctors; however, it has yet to be converted into law.
With respect to the program's significant focus on attracting foreign doctors, two important points should be underscored. First, PMM regulations stipulate that only foreign doctors from countries where physician density is higher than that of Brazil are eligible (1.8 doctors/1 000 inhabitants; 9). Moreover, the number of foreign physicians cannot exceed 10% of the total number of Brazilian doctors. Second, there is an effort by the Government to increase the training opportunities available to new doctors with a view to improving primary health care in the SUS priority areas. According to official data, 5 300 new undergraduate medical school places were created in 2015, with a goal of an additional 11 400 places by the end of 2017; furthermore, 12 400 medical residency positions will be created by 2018 (35). In this respect, it is expected that foreign participation in Brazil's workforce will be temporary, as stated in the law, in contrast to what occurred in Australia (36, 37); in the United States of America and the United Kingdom, foreign medical graduates account for 25% and 28% of the medical workforce, respectively (38). In addition, more Brazilian doctors are applying to the PMM, rising from 5.1% in July 2013 (the first cycle) (39); to 28.91% at the end of 2015, not including Brazilians trained abroad (18). The data show that the need for foreign doctors will gradually decrease, resulting in greater sustainability for the PMM.
Limitations. A limitation of this study was the lack of an official baseline for the number of physicians prior to PMM in each municipality. The data used came from the 2011 Medical Demography in Brazil study, and the 2-year gap between it and PMM implementation was not considered (17).
Conclusions
This study is, to the best of our knowledge, the first to identify and estimate the cost components of a program aim to attract and retain doctors in rural and remote areas that are socioeconomically vulnerable. Under the PMM, the poorest areas of Brazil (North and Northeast) benefitted the most from the increased number of doctors. The annual cost of the PMM (US$ 1.1 billion in 2014 and monthly salaries of about US$ 6 000 a month per doctor) is considered relatively moderate compared to its potential benefits in terms of population health. We believe that the Brazilian experience with the Programa Mais Médicos can contribute greatly to the topic, as well as identify successes and challenges regarding physician shortage and imbalances in health worker distribution. Further studies on the cost-effectiveness of this program are recommended.
Funding Statement
Financial support for the study was provided by the National Council for Scientific and Technological Development (CNPq) - Chamada MCTI/CNPq/CT-Saúde/MS/SCTIE/Decit Nº 41/2013. The funding was not specific to the study described in this article. The funder had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit this article for publication. All researchers´ decision have been entirely independent from funders.
Footnotes
Suggested citation Silva EN, Ramos MC, Santos W, Rasella D, Oliveira A, Santos LMP. Cost of providing doctors in remote and vulnerable areas: Programa Mais Médicos in Brazil. Rev Panam Salud Publica. 2018;42:e11. https://doi.org/10.26633/RPSP.2018.11
Funding. Financial support for the study was provided by the National Council for Scientific and Technological Development (CNPq) - Chamada MCTI/CNPq/CT-Saúde/MS/SCTIE/Decit Nº 41/2013. The funding was not specific to the study described in this article. The funder had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit this article for publication. All researchers´ decision have been entirely independent from funders.
Disclaimer. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH and/or PAHO.
REFERENCES
- 1.World Health Organization . The world health report: 2006. Working together for health. Geneva: WHO; 2006. [Google Scholar]
- 2.Dussault G, Franceschini MC. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4(1):12–12. doi: 10.1186/1478-4491-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rao M, Rao KD, Kumar AS, Chatterjee M, Sundararaman T. Human resources for health in India. Lancet. 2011;377(9765):587–598. doi: 10.1016/S0140-6736(10)61888-0. [DOI] [PubMed] [Google Scholar]
- 4.Peña S, Ramirez J, Becerra C, Carabantes J, Arteaga O. The Chilean Rural Practitioner Programme: a multidimensional strategy to attract and retain doctors in rural areas. Bull World Health Organ. 2010;88(5):371–378. doi: 10.2471/BLT.09.072769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Straumea K, Shawb DM. Effective physician retention strategies in Norway's northernmost county. Bull World Health Organ. 2010;88(5):390–394. doi: 10.2471/BLT.09.072686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dal Poz MR. The crisis of health workforce. Cad Saude Publica. 2013;29(10):1924–1926. doi: 10.1590/0102-311xpe011013. [DOI] [PubMed] [Google Scholar]
- 7.Shamian J, Murphy GT, Rose AE, Jeffs L. Human resources for health: a new narrative. Lancet. 2015;386(9988):25–26. doi: 10.1016/S0140-6736(15)61195-3. [DOI] [PubMed] [Google Scholar]
- 8.Dolea C, Stormont L, Braichet J-M. Evaluated strategies to increase attraction and retention of health workers in remote and rural areas. Bull World Health Organ. 2010;88(5):379–385. doi: 10.2471/BLT.09.070607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Government of Brazil [Accessed 24 October 2016];Diário Oficial da União. 2013 Institui o Programa Mais Médicos, altera as Leis no 8.745, de 9 de dezembro de 1993, e no 6.932, de 7 de julho de 1981, e dá outras providências. Lei 12.871 de 22 de outubro de 2013. Available from: http://www.planalto.gov.br/ccivil_03/_Ato2011-2014/2013/Lei/L12871.htm.
- 10.Santos LMP, Costa AM, Girardi SN. Mais Medicos Program: an effective action to reduce health inequities in Brazil. Cienc Saude Coletiva. 2015;20(11):3547–3552. doi: 10.1590/1413-812320152011.07252015. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira FP de, Vanni T, Pinto HA, Santos JTR dos, Figueiredo AM de, Araújo SQ de, et al. “Mais Médicos”: a Brazilian program in an international perspective. Interface-Comun Saúde Educ. 2015;19(54):623–634. [Google Scholar]
- 12.da Silva Carvalho VK, Pintas Marques C, da Silva EN. A contribuição do Programa Mais Médicos: análise a partir das recomendações da OMS para provimento de médicos. Rev Ciênc Saúde Coletiva. 2016;21(9):2773–2784. doi: 10.1590/1413-81232015219.17362016. [DOI] [PubMed] [Google Scholar]
- 13.Marten R, McIntyre D, Travassos C, Shishkin S, Longde W, Reddy S, et al. An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS) Lancet. 2014;384(9960):2164–2171. doi: 10.1016/S0140-6736(14)60075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Government of Brazil Diário Oficial da União. 2011. [Accessed 24 October 2016]. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes e normas para a organização da Atenção Básica, para a Estratégia Saúde da Família (ESF) e o Programa de Agentes Comunitários de Saúde (PACS). Portaria GM no. 2488, 21 outubro 2011. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt2488_21_10_2011.html.
- 15.Macinko J, Harris MJ. Brazil's family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–2181. doi: 10.1056/NEJMp1501140. [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Health of Brazil Sala de Apoio à Gestão Estratégica. Redes e Programas: Saúde Mais Perto de Você – Atenção Básica. [Accessed 24 October 2016]. Available from: http://sage.saude.gov.br/
- 17.Conselho Regional de Medicina do Estado de São Paulo . In: Demografia médica no Brasil. Scheffer M, editor. Vol. 2. São Paulo: CREMESP; 2013. [Google Scholar]
- 18.Ministry of Health of Brazil . Programa Mais Médicos-dois anos: mais saúde para os brasileiros. Brasília: Ministério da Saúde; 2015. [Google Scholar]
- 19.Oliveira JPA, Sanchez MN, Santos LMP. The Mais Médicos (More Doctors) Program: the placement of physicians in priority municipalities in Brazil from 2013 to 2014. Ciênc Saúde Coletiva. 2016;21(9):2719–2727. doi: 10.1590/1413-81232015219.17702016. [DOI] [PubMed] [Google Scholar]
- 20.Government of Brazil Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares (POF) 2008-2009. [Accessed 24 October 2016]. Available from: http://biblioteca.ibge.gov.br/visualizacao/livros/liv45419.pdf.
- 21.Nogueira PTA, Bezerra AFB, Leite AFB, Carvalho IM de S, Gonçalves RF, Brito-Silva KS de. Characteristics of the distribution of doctors in the Mais Médicos (More Doctors) Program in the states of Brazil's Northeast. Ciênc Saúde Coletiva. 2016;21(9):2889–2898. doi: 10.1590/1413-81232015219.17022016. [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, De Paepe P, da Silva MRF, Unger JP, et al. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med. 2014;106:204–213. doi: 10.1016/j.socscimed.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 23.Estação de Pesquisa de Sinais de Mercado . Estudo de levantamento de aspectos demográficos, de formação e de mercado de trabalho das profissões de saúde nível superior no Brasil entre 1991 e 2010. Belo Horizonte: NESCON/UFMG; 2014. pp. 79–80. [Google Scholar]
- 24.Maciel RH, Santos JBF dos, Sales TB, Alves MA de A, Luna AP, Feitosa LB. Multiple job contracts of physicians in Ceará, Northeastern Brazil. Rev Saude Publica. 2010;44(5):950–956. doi: 10.1590/s0034-89102010005000030. [DOI] [PubMed] [Google Scholar]
- 25.Government of Brazil Tribunal de Contas da União. TCU TC No.o 005.391/2014-8. 2014. [Accessed 24 October 2016]. Available from: http://portal3.tcu.gov.br/portal/page/portal/TCU/imprensa/noticias/noticias_arquivos/005.391-2014-8%20Mais%20M%C3%A9dicos.pdf.
- 26.Comes Y, Trindade J de S, Shimizu HE, Hamann EM, Bargioni F, Ramirez L, et al. Evaluation of user satisfaction and service responsiveness in municipalities enrolled in the Mais Médicos (More Doctors) Program. Ciênc Saúde Coletiva. 2016;21(9):2749–2759. doi: 10.1590/1413-81232015219.16202016. [DOI] [PubMed] [Google Scholar]
- 27.Comes Y, Trindade J de S, Pessoa VM, Barreto IC de HC, Shimizu HE, Dewes D, et al. The implementation of the Mais Médicos (More Doctors) Program and comprehensiveness of care in the Family Health Strategy. Ciênc Saúde Coletiva. 2016;21(9):2729–2738. doi: 10.1590/1413-81232015219.15472016. [DOI] [PubMed] [Google Scholar]
- 28.dos Santos MAM, de Souza EG, Cardoso JC. Avaliação da qualidade da estratégia saúde da família e do programa mais médicos na área rural de Porto Velho, Rondônia. Gest E Soc. 2016;10(26):1327–1346. [Google Scholar]
- 29.Giovanella L, Mendonça MHM de, Fausto MCR, Almeida PF de, Bousquat A, Lima JG, et al. Emergency supply of doctors by the Mais Médicos (More Doctors) Program and the quality of the structure of primary health care facilities. Ciênc Saúde Coletiva. 2016;21(9):2697–2708. doi: 10.1590/1413-81232015219.16052016. [DOI] [PubMed] [Google Scholar]
- 30.Girardi SN, Stralen AC de S van, Cella JN, Wan Der Maas L, Carvalho CL, Faria E de O. Impact of the Mais Médicos (More Doctors) Program in reducing physician shortage in Brazilian Primary Healthcare. Ciênc Saúde Coletiva. 2016;21(9):2675–2684. doi: 10.1590/1413-81232015219.16032016. [DOI] [PubMed] [Google Scholar]
- 31.Santos LMP, Oliveira A, Trindade JS, Barreto IC, Palmeira PA, Comes Y, et al. Implementation research: towards universal health coverage with more doctors in Brazil. Bull World Health Organ. 2017;95(2):103–103. doi: 10.2471/BLT.16.178236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haji M, Durairaj V, Zurn P, Stormont L, Mapunda M. Emerging opportunities for recruiting and retaining rural health workforce through decentralized health financing systems. Bull World Health Organ. 2010;88(5):397–399. doi: 10.2471/BLT.09.072827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Piola SF, Barreto de Paiva A, Batista de Sá E, Servo LMS. Financiamento público da saúde: uma história à procura de rumo. Brasília: Instituto de Pesquisa Econômica Aplicada; 2013. [Google Scholar]
- 34.Carvalho MS, Sousa MF. Como o Brasil tem enfrentado o tema provimento de médicos? Interface (Botucatu) 2013;7(47):913–926. [Google Scholar]
- 35.Cyrino EG, Pinto HA, Oliveira FP de, Figueiredo AM de. The Project “Mais Médicos” and training in and for the Brazilian Health System (SUS): why change it? Esc Anna Nery. 2015;19(1):5–6. [Google Scholar]
- 36.Scott M, Whelan A, Dewdney J, Zwi A. “Brain drain” or ethical recruitment? Solving health workforce shortages with professionals from developing countries. Med J Aust. 2004;180(4):174–176. doi: 10.5694/j.1326-5377.2004.tb05862.x. [DOI] [PubMed] [Google Scholar]
- 37.Han G-S, Humphreys JS. Overseas-trained doctors in Australia: community integration and their intention to stay in a rural community. Aust J Rural Health. 2005;13(4):236–241. doi: 10.1111/j.1440-1584.2005.00708.x. [DOI] [PubMed] [Google Scholar]
- 38.Mullan F. The metrics of the physician brain drain. N Engl J Med. 2005;353(17):1810–1818. doi: 10.1056/NEJMsa050004. [DOI] [PubMed] [Google Scholar]
- 39.Pereira LL, Santos LMP, Santos W, Oliveira A, Rattner D. Mais Médicos program: provision of medical doctors in rural, remote and socially vulnerable areas of Brazil, 2013–2014. Rural Remote Health. 2016;16(1):3616–3616. [PubMed] [Google Scholar]


