Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- LMWH
low molecular weight heparin
- PVT
portal vein thrombosis
- VKA
vitamin K antagonist
Key Points
Patients with decompensated cirrhosis are relatively hypercoagulable and have higher prevalence of portal vein thrombosis (PVT).
The natural history of PVT in patients with decompensated cirrhosis is unclear.
Anticoagulation may provide additional benefits beyond PVT resolution.
Current evidence does not show increased adverse outcomes in patients with cirrhosis who are anticoagulated.
Anticoagulation is recommended in patients who are potential liver transplant candidates who have main portal vein trunk or progressive PVT.
PVT is a common problem in patients with cirrhosis.1 The prevalence rate (using any form of imaging) ranges from 0.6% to 40%, with a higher prevalence rate in patients with decompensated cirrhosis (8%‐25%) versus those with compensated cirrhosis (∼1%).1, 2, 3 In patients with compensated cirrhosis, the balance between procoagulant and anticoagulant factors is relatively stable, whereas in decompensated cirrhosis, the balance tips toward a procoagulant state.4 In patients with decompensated cirrhosis, synthesis of anticoagulant factors such as protein C and S are decreased, and procoagulants such as factor VIII, thrombin, tissue factor, and von Willebrand factor are increased, overall resulting in a prothrombotic state.5, 6, 7, 8
In compensated patients, the development of PVT is not predictive of decompensation9; however, in the decompensated patient, the effect of PVT on further decompensation is unclear. In patients with variceal hemorrhage, the presence of PVT is a significant independent predictor of 5‐day treatment failure, defined as rebleeding, uncontrolled bleeding, or death.10, 11 In addition, several studies show that patients with PVT who undergo hepatic transplantation have a higher morbidity and mortality post transplant. In a large cohort of patients from the Scientific Registry of Transplant Recipients from 2001 to 2007, pretransplant PVT did not affect wait‐list mortality but was associated with a 32% greater risk for death (HR, 1.32; confidence interval [CI], 1.1‐1.7; P = 0.02).12 Although PVT can be removed surgically at the time of transplant, mortality rates have a tendency to be higher post transplant, particularly if requiring nonphysiologic portal vein reconstruction.13 Other than posttransplant outcomes and intestinal ischemia with superior mesenteric vein thrombosis, no other clinical outcomes in cirrhosis have been clearly related to the development or presence of PVT.
Whether patients with PVT should be anticoagulated, and the duration of anticoagulation, has been controversial, especially because PVT appears to be a dynamic process. In a prospective study of 1243 patients with cirrhosis without PVT, 118 patients had PVT. Most of the PVTs were nonocclusive and resolved in 70% of cases. However, 12% progressed to occlusive thrombi with no clear predictors of thrombi progression.9 Despite this finding, it is important to note that this study was performed in patients with compensated cirrhosis who have a lower risk for thrombotic events. The course of PVT in patients with decompensated cirrhosis remains to be determined.
Anticoagulation in patients with PVT has shown that resolution of PVT is variable. Anticoagulants evaluated in these studies have included vitamin K antagonists (VKAs) or low molecular weight heparin (LMWH). A recent meta‐analysis including 12 studies of patients with cirrhosis with PVT who were treated with anticoagulation showed that 67% (95% CI, 55%‐78%) had some degree of PVT recanalization, and 42% (95% CI, 29%‐55%) of patients achieved complete PVT recanalization (Table 1).14
Table 1.
Studies Evaluating the Efficacy of Anticoagulation in Patients With Cirrhosis and PVT14, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27
| Study | Patients(n) | Anticoagulation Type | Duration of Anticoagulation (months) | No Recanalization (n) | Partial Recanalization (n) | Complete Recanalization (n) |
|---|---|---|---|---|---|---|
| Amitrano (2010)19 | 28 | LMWH | 6 | 5 | 14 | 9 |
| Delgado (2012)20 | 55 | LMWH (47), VKA (8) | 7 | 22 | 8 | 25 |
| Francoz (2005)21 | 19 | LMWH | 8.1 | 11 | 0 | 8 |
| Garcovich (2011)a | 15 | LMWH | 6 | 8 | N/A | N/A |
| Senzolo (2012) | 35 | LMWH | 6 | 12 | 9 | 12 |
| Cal (2013) | 5 | LMWH (2), VKA (3) | 3 | 1 | 0 | 4 |
| Chung (2014) | 14 | VKA | 3.7 | 3 | 5 | 6 |
| Risso (2014)22, b | 50 | N/A | N/A | 15 | N/A | N/A |
| Chen (2015)c | 30 | VKA | 7.6 | 7 | N/A | N/A |
| Wang (2016)24, d | 31 | VKA | 12 | 0 | N/A | N/A |
| Tonon (2016) | 42 | LMWH | 16 | 14 | 10 | 18 |
| Bento (2011)25 | 28 | LMWH, VKA | 6 | 10 | 5 | 13 |
| Naeshiro (2014) | 26 | LMWH | 0.5 | 6 | 16 | 4 |
| Werner (2013)27 | 28 | VKA | 12 | 5 | 12 | 11 |
Partial or total recanalization was seen in 7 patients, but differentiation between partial and total was not reported.
Partial or total recanalization was seen in 35 patients, but differentiation between partial and total was not reported.
Although 30 patients were treated, only 22 had follow‐up. Partial or total recanalization was seen in 15 patients, but differentiation between partial and total was not reported.
Partial or total recanalization was seen in 31 patients, but differentiation between partial or total was not reported.
In addition, recent evidence suggests that anticoagulation may have benefits beyond resolution of PVT. In a randomized open‐label trial of enoxaparin versus no enoxaparin in decompensated (Child B/C) patients with cirrhosis and without PVT at baseline, Villa et al.15 showed a lower incidence of PVT in patients within the enoxaparin group. Importantly, the study also showed both a significantly lower rate of further decompensation in the enoxaparin group (11.7% compared with 59.4% in the control group; P < 0.0001) and a significantly lower mortality rate with enoxaparin (24% compared with 36% in the control group; P = 0.020), independent of PVT. The study also shows that serum bacterial s16 DNA and levels of the proinflammatory cytokine interleukin‐6 were significantly lower in the enoxaparin group, suggesting that the observed beneficial effect of enoxaparin may have been because of a decrease in bacterial translocation or inflammation, factors that are known drivers of further decompensation.15
The possibility that enoxaparin may have effects beyond resolution of PVT has been further supported by experimental studies in rats with common bile duct ligation or carbon tetrachloride–induced cirrhosis and ascites. These studies demonstrated a significant decrease in portal pressure with enoxaparin (compared with saline‐treated animals). However, the mechanism of reduction in portal pressure was not due to a decrease in portal flow but a decrease in intrahepatic resistance, which was secondary to decreased hepatic stellate cell activation (aSMA protein), decreased microthrombi formation (fibrin protein) in the liver, and decreased liver fibrosis.16
Despite these data and consensus recommendations to start anticoagulation in patients on the transplant list who experience occlusive or progressive PVT,17 there is still hesitation due to concerns of bleeding complications. Current evidence does not show increased adverse outcomes in patients with cirrhosis who are receiving anticoagulation. A recent meta‐analysis evaluating the effects of anticoagulation in 257 patients with cirrhosis and PVT showed no difference in major or minor bleeding between the groups who received anticoagulation versus those who did not (rate of occurrence was 11% for both groups). Notably, four of the studies included in the analysis that evaluated variceal bleeding demonstrated a lower rate of variceal bleeding in patients who received anticoagulation (2% in patients who were anticoagulated versus 12% in patients who were not anticoagulated; odds ratio, 0.232; 95% CI, 0.06‐0.94; P = 0.04) (Table 2).18
Table 2.
Adverse Outcomes Reported in Patients With Cirrhosis and PVT Who Were Treated With Anticoagulation18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
| Study | Anticoagulation Type | Patients (n) | Child‐Pugh Class A/B/C | Adverse Events Associated With Coagulation |
|---|---|---|---|---|
| Amitrano (2010)19 | LMWH | 28 | B/C | 1. Two patients with anemia secondary to portal hypertensive gastropathy requiring iron transfusion |
| Delgado (2012)20 | LMWH (47), VKA (8) | 55 | 25/21/9 |
1. One lower gastrointestinal bleeding 2. One obscure gastrointestinal bleeding 3. One oral bleeding after dental extraction 4. One vaginal bleeding 5. One surgical wound hemorrhage |
| Francoz (2005)21 | LMWH | 19 | 26/41/33% | 1. One postprocedural bleeding |
| Garcovich (2011) | LMWH | 15 | A/B | 1. None |
| Senzolo (2012) | LMWH | 35 | 11/16/8 |
1. One cerebral bleed 2. One epistaxis 3. One variceal bleed 4. One hematuria |
| Cal (2013) | LMWH (2), VKA (3) | 5 | 4/1/0 | 1. None |
| Chung (2014) | VKA | 14 | 6/8/0 | 1. None |
| Risso (2014)22, a | N/A | 50 | N/A | 17% minor bleeding |
| Chen (2015) | VKA | 30 | 6/17/5 |
1. Four with hematemesis 2. One with epistaxis 3. One with gingival bleeding |
| Wang (2016)24 | VKA | 31 | 12/17/2 |
1. Two gastrointestinal bleeding 2. One variceal bleed |
| Tonon (2016) | LMWH | 42 | N/A |
1. One hemoperitoneum after paracentesis 2. Five nonmajor bleeding events |
| Bento (2011)25 | LMWH, VKA | 28 | N/A | None |
| Naeshiro (2014) | LMWH | 26 | 13/8/5 | None |
| Werner (2013)27 | VKA | 28 | N/A | 1. One vaginal bleeding |
Details of minor bleeding were not described.
The current consensus recommends that anticoagulation be considered in potential liver transplant candidates with thrombosis of the main portal vein trunk or progressive PVT, to reduce posttransplant morbidity and mortality.17 If left untreated, patients with cirrhosis and PVT should undergo screening every 3 months to evaluate for progression of the PVT. Anticoagulation should be considered in those with progression of the PVT or extension into the SMV.17 A potential algorithm of patients in whom anticoagulation should be considered is shown in Fig. 1. However, given the benefits that go beyond resolution of PVT (Fig. 2), one could even consider extending these recommendations to patients with cirrhosis who do not meet these criteria. Further studies defining the specific subpopulation of patients who benefit from anticoagulation are eagerly awaited.
Figure 1.
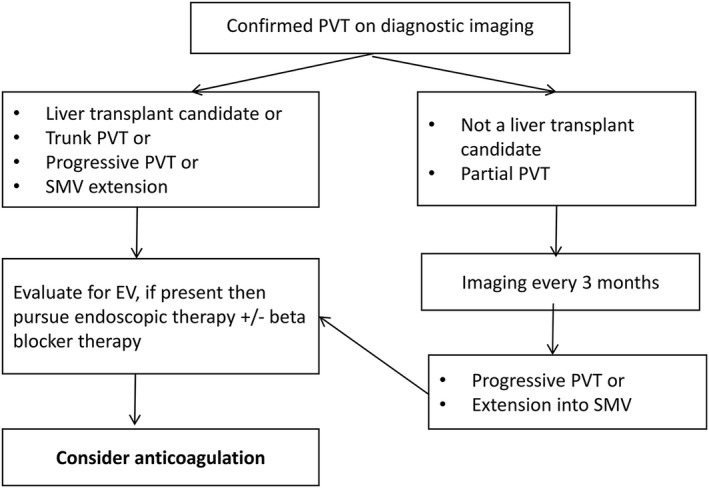
Potential algorithm for treatment of PVT in patients with cirrhosis.
Figure 2.
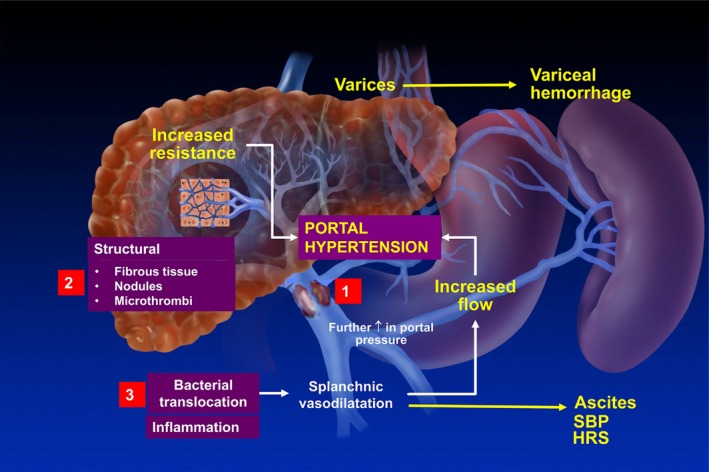
Pathophysiology of portal hypertension in the context of PVT and potential sites for a beneficial effect of anticoagulation. Portal hypertension in cirrhosis results from increased intrahepatic resistance and increased portal blood flow. Development of an occlusive thrombus in the main portal vein will lead to a further increase in portal pressure proximal to the site of obstruction and could potentially lead to a higher rate of variceal hemorrhage (but not to increased development of ascites). The sites at which anticoagulation could lead to better outcomes in cirrhosis are depicted in the figure: (1) Clot dissolution would decrease the proximal increase in portal vein pressure, (2) microthrombi arising from the main clot (or from the hypercoagulable state per se) could obstruct intrahepatic venules and cause an increase in sinusoidal pressure, and (3) bacterial translocation and consequent inflammation contribute to the splanchnic vasodilatation and increased portal flow that maintains the portal hypertensive state and leads to a stage of further decompensation. Abbreviations: HRS, hepatorenal syndrome; SBP, spontaneous bacterial peritonitis.
This study was supported by the Yale Liver Center (National Institutes of Health grant P30 DK34989).
Potential conflict of interest: Nothing to report.
References
- 1. Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Iannaccone L, D'Andrea G, et al. Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology 2000;31:345‐348. [DOI] [PubMed] [Google Scholar]
- 2. Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, et al. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. JHepatol 2004;40:736‐741. [DOI] [PubMed] [Google Scholar]
- 3. Nonami T, Yokoyama I, Iwatsuki S, Starzl TE. The incidence of portal vein thrombosis at liver transplantation. Hepatology 1992;16:1195‐1198. [PMC free article] [PubMed] [Google Scholar]
- 4. Tripodi A, Primignani M, Lemma L, Chantarangkul V, Dell'Era A, Iannuzzi F, et al. Detection of the imbalance of procoagulant versus anticoagulant factors in cirrhosis by a simple laboratory method. Hepatology 2010;52:249‐255. [DOI] [PubMed] [Google Scholar]
- 5. Hugenholtz GC, Northup PG, Porte RJ, Lisman T. Is there a rationale for treatment of chronic liver disease with antithrombotic therapy? Blood Rev 2015;29:127‐136. [DOI] [PubMed] [Google Scholar]
- 6. Carnevale R, Raparelli V, Nocella C, Bartimoccia S, Novo M, Severino A, et al. Gut‐derived endotoxin stimulates factor VIII secretion from endothelial cells. Implications for hypercoagulability in cirrhosis. JHepatol 2017;67:950‐956. [DOI] [PubMed] [Google Scholar]
- 7. Basili S, Ferro D, Violi F. Endotoxaemia, hyperfibrinolysis, and bleeding in cirrhosis. Lancet 1999;353:1102. [DOI] [PubMed] [Google Scholar]
- 8. Kleinegris MC, Bos MH, Roest M, Henskens Y, Ten Cate‐Hoek A, Van Deursen C, et al. Cirrhosis patients have a coagulopathy that is associated with decreased clot formation capacity. JThromb Haemost 2014;12:1647‐1657. [DOI] [PubMed] [Google Scholar]
- 9. Nery F, Chevret S, Condat B, de Raucourt E, Boudaoud L, Rautou PE, et al. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: results of a longitudinal study. Hepatology 2015;61:660‐667. [DOI] [PubMed] [Google Scholar]
- 10. Amitrano L, Guardascione MA, Manguso F, Bennato R, Bove A, DeNucci C, et al. The effectiveness of current acute variceal bleed treatments in unselected cirrhotic patients: refining short‐term prognosis and risk factors. Am J Gastroenterol 2012;107:1872‐1878. [DOI] [PubMed] [Google Scholar]
- 11. Cerini F, Gonzalez JM, Torres F, Puente A, Casas M, Vinaixa C, et al. Impact of anticoagulation on upper‐gastrointestinal bleeding in cirrhosis. A retrospective multicenter study. Hepatology 2015;62:575‐583. [DOI] [PubMed] [Google Scholar]
- 12. Englesbe MJ, Schaubel DE, Cai S, Guidinger MK, Merion RM. Portal vein thrombosis and liver transplant survival benefit. Liver Transpl 2010;16:999‐1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hibi T, Nishida S, Levi DM, Selvaggi G, Tekin A, Fan J, et al. When and why portal vein thrombosis matters in liver transplantation: A critical audit of 174 cases. Ann Surg 2014;259:760‐766. [DOI] [PubMed] [Google Scholar]
- 14. Qi X, De Stefano V, Li H, Dai J, Guo X, Fan D. Anticoagulation for the treatment of portal vein thrombosis in liver cirrhosis: A systematic review and meta‐analysis of observational studies. Eur J Intern Med 2015;26:23‐29. [DOI] [PubMed] [Google Scholar]
- 15. Villa E, Camma C, Marietta M, Luongo M, Critelli R, Colopi S, et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology 2012;143:1253‐1260.e1‐4. [DOI] [PubMed] [Google Scholar]
- 16. Cerini F, Vilaseca M, Lafoz E, Garcia‐Irigoyen O, Garcia‐Caldero H, Tripathi DM, et al. Enoxaparin reduces hepatic vascular resistance and portal pressure in cirrhotic rats. JHepatol 2016;64:834‐842. [DOI] [PubMed] [Google Scholar]
- 17. Trebicka J, De Gottardi A, Dell'Era A, Leebeek F, Sarin S, Seijo S, et al. Session 6: Consensus statements – vascular diseases of the liver in cirrhotic and noncirrhotic portal hypertension In: de Franchis R, ed. Portal Hypertension VI: Proceedings of the Sixth Baveno Consensus Workshop: Stratifying Risk and Individualizing Care. Cham, Switzerland: Springer International Publishing; 2016:421‐426. [Google Scholar]
- 18. Loffredo L, Pastori D, Farcomeni A, Violi F. Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: A systematic review and meta‐analysis. Gastroenterology 2017;153:480‐487.e1. [DOI] [PubMed] [Google Scholar]
- 19. Amitrano L, Guardascione MA, Menchise A, Martino R, Scaglione M, Giovine S, et al. Safety and efficacy of anticoagulation therapy with low molecular weight heparin for portal vein thrombosis in patients with liver cirrhosis. JClin Gastroenterol 2010;44:448‐451. [DOI] [PubMed] [Google Scholar]
- 20. Delgado MG, Seijo S, Yepes I, Achecar L, Catalina MV, Garcia‐Criado A, et al. Efficacy and safety of anticoagulation on patients with cirrhosis and portal vein thrombosis. Clin Gastroenterol Hepatol 2012;10:776‐783. [DOI] [PubMed] [Google Scholar]
- 21. Francoz C, Belghiti J, Vilgrain V, Sommacale D, Paradis V, Condat B, et al. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut 2005;54:691‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Risso A, Stradella D, Martini S, Rizzetto M, Salizzoni M. Liver transplantation in cirrhotic patients with portal vein thrombosis: A single centre experience. Dig Liver Dis 2014;46:e40. [Google Scholar]
- 23. Chen H, Liu L, Qi X, He C, Wu F, Fan D, et al. Efficacy and safety of anticoagulation in more advanced portal vein thrombosis in patients with liver cirrhosis. Eur J Gastroenterol Hepatol 2016;28:82‐89. [DOI] [PubMed] [Google Scholar]
- 24. Wang Z, Jiang MS, Zhang HL, Weng NN, Luo XF, Li X, et al. Is post‐TIPS anticoagulation therapy necessary in patients with cirrhosis and portal vein thrombosis? A randomized controlled trial. Radiology 2016;279:943‐951. [DOI] [PubMed] [Google Scholar]
- 25. Bento L, Huerta AR, Pascual C, Rus GP, Catalina V, Yepes I, et al. Antithrombotic therapy in non‐neoplastic chronic portal venous thrombosis in cirrhosis: recanalization and liver function evaluation. Blood 2011;118:1440‐1440. [Google Scholar]
- 26. Naeshiro N, Aikata H, Hyogo H, Kan H, Fujino H, Kobayashi T, et al. Efficacy and safety of the anticoagulant drug, danaparoid sodium, in the treatment of portal vein thrombosis in patients with liver cirrhosis. Hepatol Res 2015;45:656‐662. [DOI] [PubMed] [Google Scholar]
- 27. Werner KT, Sando S, Carey EJ, Vargas HE, Byrne TJ, Douglas DD, et al. Portal vein thrombosis in patients with end stage liver disease awaiting liver transplantation: outcome of anticoagulation. Dig Dis Sci 2013;58:1776‐1780. [DOI] [PubMed] [Google Scholar]
- 28. Qi X, Su C, Ren W, Yang M, Jia J, Dai J, et al. Association between portal vein thrombosis and risk of bleeding in liver cirrhosis: A systematic review of the literature. Clin Res Hepatol Gastroenterol 2015;39:683‐691. [DOI] [PubMed] [Google Scholar]


