Watch a video presentation of this article
Answer questions and earn CME
Abbreviations
- ER
extended‐release
- IR
immediate‐release
- NSAID
nonsteroidal anti‐inflammatory drug
- SES
socioeconomic status
- SNRI
serotonin‐norepinephrine reuptake inhibitor
- SSRI
selective serotonin reuptake inhibitor
- t1/2
half‐life
- TCA
tricyclic antidepressant
Pain is a common, undertreated symptom in patients with cirrhosis and is associated with increased health care utilization (hospitalizations, clinic visits, and phone calls).1
Management of pain in this population is complex due to patient, clinician, pharmacological, and regulatory factors (Fig. 1). Bias, fear of litigation, and impaired metabolism/excretion often result in undertreatment of pain in this population. In an effort to facilitate safe pain control, this article will summarize the existing literature regarding impaired pharmacokinetics due to liver dysfunction and dosing recommendations for analgesic treatment in patients with cirrhosis.
Figure 1.
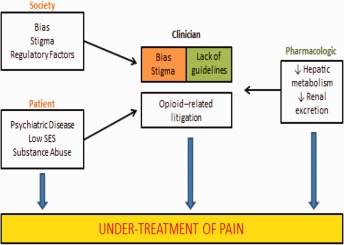
Factors that contribute to undertreatment of pain in patients with liver disease. Societal misconceptions, patient behaviors, as well as regulatory and litigious factors may consciously or unconsciously influence clinician perception of pain complaints. Moreover, impairment in drug metabolism and excretion in this medically complex population create uncertainty about how to safely and effectively use pain medications. Abbreviation: SES, socioeconomic status.
Unique Concerns in Patients With Cirrhosis
In patients with cirrhosis, liver dysfunction leads to alterations in drug pharmacokinetics and metabolism (Fig. 2), which can lead to an increased risk for hepatotoxicity and accumulation of toxic metabolites.2 Table 1 summarizes the unique management considerations in this population.
Figure 2.
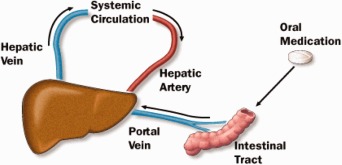
First‐pass metabolism of orally ingested medications. The drug enters the liver via the portal vein, becomes bioavailable after metabolism in the liver into active metabolites, and then enters systemic circulation via the hepatic vein. In patients with liver disease, impaired hepatic function, reduced hepatic blood flow, and portosystemic shunting reduce first‐pass metabolism, thereby increasing the proportion of drug that is bioavailable and increasing the risk for toxicity.
Table 1.
Important Considerations Regarding Analgesia Prescribing for Patients With Cirrhosis
| Impaired hepatic metabolism |
• Prescribe short‐acting (IR) analgesics whenever possible. • Start with low dosage and use extended dosing intervals (eg, every 6‐12 hour intervals). • Limit daily acetaminophen dose to 2000 mg. |
| Impaired renal excretiona |
• Dose is based on renal function. • Avoid morphine in patients with renal disease. |
| Risk for precipitating renal failure and gastrointestinal bleed | • Avoid NSAIDs in patients with cirrhosis. |
| Risk for precipitating hepatic encephalopathy |
• Monitor carefully and frequently for sedation. • If patient is not already receiving lactulose, a bowel regimen should be started and education on importance of avoiding constipation provided. |
| Potential for abuse | • When prescribing opioids, consider having patient sign a “pain agreement” (eg, obtaining opioids from only one provider, refills only during office visits or normal office hours) |
Up to 50% of patients with cirrhosis have concomitant renal disorders, resulting in impaired drug excretion and increased risk for toxicity.
Analgesics in Cirrhosis
Acetaminophen
There is a common misconception regarding the use of acetaminophen in patients with cirrhosis, resulting in recommendations that these patients should never take acetaminophen. It is true that when ingested in large amounts (doses greater than 10‐15 g) acetaminophen can cause severe hepatic necrosis and fulminant hepatic failure. Moreover, nearly half of all acetaminophen overdoses are unintentional, in part due to lack of knowledge that many over‐the‐counter and prescription medications contain acetaminophen.3 However, if taken in appropriate doses, acetaminophen is one of the safest analgesics for patients with cirrhosis.
Recommendations
Total daily dosage of acetaminophen should not exceed 2 g/day. Patients should be educated about over‐the‐counter and prescription medications that may also contain acetaminophen.
Nonsteroidal Anti‐inflammatory Drugs
Due to prostaglandin inhibition and increased bioavailability among patients with cirrhosis, nonsteroidal anti‐inflammatory drugs (NSAIDs) can precipitate acute renal failure and gastrointestinal bleeding. NSAIDs also increase risk for thrombocytopenia, which can further increase the risk for variceal and nonvariceal gastrointestinal bleeding. Finally, NSAIDs promote sodium retention, thereby worsening ascites and edema.
More recently, topical NSAIDs, such as diclofenac (Voltaren) gel, have been used to manage pain. Topical NSAIDs, which have primarily local penetration, have fewer systemic side effects. Presumably, minimal systemic absorption would suggest that topical NSAIDs would be safe to use in patients with cirrhosis, but further research is needed.
Recommendations
NSAIDs should be avoided in all patients with cirrhosis. Topical NSAIDs can be considered; however, further studies are needed to elucidate their safety profile in patients with cirrhosis.
Antidepressants, Anticonvulsants, and Anesthetics
Anticonvulsants
Calcium channel alpha‐2‐delta ligands are a class of anticonvulsants that are used to treat neuropathic pain. This class, which includes gabapentin and pregabalin, is not metabolized by the liver. Therefore, risks in patients with advanced liver disease are not greatly increased. However, there are case reports of pregabalin‐induced hepatoxicity.4 Gabapentin and pregabalin are renally excreted, so dosages need to be adjusted for renal failure.
Recommendations
Consider gabapentin as first line nonopioid therapy, particularly for patients with neuropathic pain. For gabapentin, start 300 mg daily and increase slowly over weeks. For pregabalin, start 50 mg bid for patients with normal renal function and increase slowly over weeks.
Topical Anesthetics
Lidocaine (Lidoderm) patches can be an effective treatment for localized pain in patients with cirrhosis. They have low systemic absorption; therefore, they do not need adjustment for liver dysfunction. Up to three patches can be used at one time. Patches may also be cut into smaller sizes for treatment of smaller areas.
Recommendations
Apply patch to affected area for up to 12 hours per day.
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs) are effective medications for pain of various etiologies. In patients with advanced liver disease, nortriptyline and desipramine are generally recommended over amitriptyline and imipramine because of decreased sedation effects.5
Recommendations
Nortriptyline 10 mg nightly is recommended. If necessary, consider titration over weeks to 25 mg nightly with careful monitoring for sedation.
Serotonin‐Norepinephrine Reuptake Inhibitors
Serotonin‐norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine and duloxetine have been increasingly used for pain management. Patients with cirrhosis demonstrate significantly increased half‐life (t 1/2) and reduced clearance of these medications; duloxetine is associated with drug‐induced liver injury (black box warning). Selective serotonin reuptake inhibitors (SSRIs) are not as effective as TCAs in management of neuropathic pain and can increase the risk for gastrointestinal bleeding from varices.6
Recommendations
Use gabapentin or TCAs for treatment of pain over SNRIs and SSRIs. Avoid duloxetine.
Opioids
The use of opioids in this population is controversial and complicated with unique concerns specific to patients with cirrhosis (Table 1). Based on a review of the literature and expert opinion, Table 2 summarizes the effect of advanced liver disease on the t 1/2 of each opioid and provides starting oral dosing recommendations for nonacute pain.7 In general, because of lengthened t 1/2 among patients with cirrhosis, immediate‐release (IR) formulations should be used, extended‐release (ER) formulations avoided, and extended dosing intervals (eg, every 6‐12 hours) should be prescribed.
Table 2.
Summary of Opioid Pharmacokinetics in Cirrhosis, Including Management Recommendations
| Drug | No Liver Disease (t 1/2 in hours) | Cirrhosis (t 1/2 in hours) | Recommended Starting Dosage in Advanced Liver Diseasea | Important Considerations | Reference |
|---|---|---|---|---|---|
| Tramadol IR | 5.1 | 13.3 | 50 mg q12h | Use with caution in patients taking SSRIs or TCAs. Avoid in patients with seizure history. | Park et al.14 |
| Hydrocodone IR | 3.8 | n/a | 5 mg q6h | Common form contains 325 mg acetaminophen per tablet. Limit is 6 tablets/day. | Saab et al.15 |
| Oxycodone IR | 3.4 | 13.9 | 5 mg q6h | Has variable onset and analgesic efficacy. | Murphy16 |
| Morphine IR | 3.3 | 5.5b | 5 mg q6h (elixir form)c | Avoid in renal failure. | Hasselström et al.9 |
| Hydromorphone IR | 2.5 | n/a | 1‐2 mg q6h | Consider first choice opioid in patients with renal failure. | Durnin et al.17 |
| Methadone | 19 | 35d | Not recommended unless used as part of addiction program. Avoid in severe liver disease. | Novick et al.12 | |
| Codeine | 2.9 | n/a | 15 mg q6h | Avoid use, if possible. | Rhee and Broadbent7 |
Abbreviations: n/a, not available.
Opioid‐tolerant individuals will require careful uptitration of dosages. Dosages represent general guidelines and should be individualized.
t 1/2 by Child Pugh class: Class A = 3.4 h, Class B = 4.3 h, Class C = 4.5 h.
Morphine IR in 5‐mg increments is available only in elixir form. If tablet form is desired, the smallest dosage is 15 mg. Splitting tablets is not recommended.
t 1/2 by Child Pugh class: Class A = 11.3 h, Class B = 13.0 h, Class C = 35.5 h.
Tramadol
Tramadol can cause less sedation and respiratory depression, and has less potential for tolerance compared with other opioids8; however, it lowers seizure threshold and can precipitate serotonin syndrome when used with SSRIs or TCAs.
Recommendations
Start with 50 mg every 12 hours and use extended dosing intervals. Use with careful monitoring in patients taking SSRIs or TCAs. Avoid in patients with seizure history.
Hydrocodone
Hydrocodone is most commonly available in combination with acetaminophen. Therefore, education and careful attention to total daily acetaminophen dosage is necessary. Avoid ER formulations (hydrocodone ER [Zohydro ER, Hysingla ER, Vantrela ER]) in patients with cirrhosis.
Recommendations
Start with 5 mg every 6 hours and use extended dosing intervals.
Oxycodone
Oxycodone has increased oral bioavailability because of diminished first‐pass effect and prolonged t 1/2 due to significant protein binding, which increases the risk for toxicity. Avoid ER formulations (oxycodone ER [OxyContin, Xtampza ER]).
Recommendations
Start with 5 mg every 6 hours and use extended dosing intervals.
Morphine
Morphine is metabolized into two major metabolites: one with analgesic properties (morphine‐6‐glucuronide) and the other (morphine‐3‐glucuronide) with neurotoxic side effects such as confusion, seizures, and respiratory depression.9 In the setting of renal failure, the neurotoxic metabolites are poorly excreted. Avoid ER formulations (MS Contin).
Recommendations
Start with 5 mg every 6 hours (elixir form). Avoid in patients with renal failure.
Hydromorphone
Hydromorphone is five times more potent than morphine.10 Hydromorphone is metabolized solely by glucuronidation into an inactive metabolite; therefore, metabolism and t 1/2 are less affected by cirrhosis. Hydromorphone's t 1/2 appears largely unaffected by advanced liver disease and less affected by concomitant renal disease compared with other opioids.11 Avoid the ER formulation.
Recommendations
First‐choice opioid in patients with concomitant renal failure; start with 1 mg every 6 hours.
Methadone
Methadone is a synthetic opioid that is widely used as maintenance treatment for individuals with opioid or heroin dependency. In patients with mild‐to‐moderate chronic liver disease, t 1/2 is not affected. However, it is greatly prolonged in those with severe liver failure.12
Recommendations
No dose modification is needed in mild‐to‐moderate liver disease; use with caution in severe liver failure. In general, methadone for pain management should be reserved for use by experienced clinicians.
Codeine
Codeine is a weak opioid with limited conversion to active metabolite, reducing its analgesic potency.
Recommendations
Avoid codeine because of diminished analgesic properties.
Fentanyl
Fentanyl causes reduced histamine release compared with other opioids, resulting in fewer cases of hypotension.
Recommendations
Transdermal fentanyl patch is not recommended until after assessment of total daily opioid requirements with short‐acting opioids.
Meperidine
Meperidine's active metabolite, normeperidine, is toxic, resulting in delirium, tremors, and seizures.
Recommendations
Avoid meperidine.
Marijuana
Marijuana use has become increasingly prevalent among those with chronic pain, including those with liver disease. In particular, among some of the states that have legalized medical marijuana, hepatitis C infection is one of the qualifying medical conditions. Because marijuana use has become more accessible and may not be openly disclosed by some patients, clinicians should routinely ask about its use for pain relief. Various formulations of marijuana exist, including inhalation, oral (edible, oils), sublingual, and topical. Inhaled marijuana is not recommended given the risk for pulmonary infections and scarring. An oral formulation of marijuana, dronabinol (Marinol), is US Food and Drug Administration approved for anorexia, nausea, and appetite stimulation. Conflicting data exist about risk for hepatotoxicity and fibrosis progression due to marijuana.13 Further studies are needed to determine the effectiveness of dronabinol and nonprescription formulations of cannabis for pain management in patients with cirrhosis.
Recommendations
There is insufficient evidence for or against marijuana use at this time.
Conclusion
Patients with cirrhosis often experience pain. Yet pain remains one of the most undertreated symptoms in this patient population. A variety of medications are available to help address pain; however, several factors have to be taken into consideration prior to starting any pain regimen in patients with cirrhosis. Factors to consider include potential for overuse/abuse, severity of hepatic and renal impairment, and presence of hepatic encephalopathy. Chronic pain can be well managed in patients with cirrhosis; however, choice of analgesic and dosing regimen should be highly individualized and side effects carefully monitored.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Rogal SS, Winger D, Bielefeldt K, Rollman BL, Szigethy E. Healthcare utilization in chronic liver disease: the importance of pain and prescription opioid use. Liver Int 2013;33:1497‐1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chandok N, Watt KDS. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc 2010;85:451‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al.; Acute Liver Failure Study Group . Acetaminophen‐induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 2005;42:1364‐1372. [DOI] [PubMed] [Google Scholar]
- 4. Doğan S, Ozberk S, Yurci A. Pregabalin‐induced hepatotoxicity. Eur J Gastroenterol Hepatol 2011;23:628. [DOI] [PubMed] [Google Scholar]
- 5. Bosilkovska M, Walder B, Besson M, Daali Y, Desmeules J. Analgesics in patients with hepatic impairment: pharmacology and clinical implications. Drugs 2012;72:1645‐1669. [DOI] [PubMed] [Google Scholar]
- 6. Andrade C, Sandarsh S, Chethan KB, Nagesh KS. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry 2010;71:1565‐1575. [DOI] [PubMed] [Google Scholar]
- 7. Rhee C, Broadbent AM. Palliation and liver failure: palliative medications dosage guidelines. J Palliat Med 2007;10:677‐685. [DOI] [PubMed] [Google Scholar]
- 8. Kotb HI, Fouad IA, Fares KM, Mostafa MG, Abd El‐Rahman AM. Pharmacokinetics of oral tramadol in patients with liver cancer. J Opioid Manag 2008;4:99‐104. [DOI] [PubMed] [Google Scholar]
- 9. Hasselström K, Eriksson S, Persson A, Rane A, Svensson JO, Säwe J. The metabolism and bioavailability of morphine in patients with severe liver cirrhosis. Br J Clin Pharmacol 1990;29:289‐297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pasero C, Portenoy RK, McCaffery M. Opioid analgesics In: McCaffery M, Pasero C, eds. Pain: A Clinical Manual. New York, NY: Mosby; 1999:161‐199. [Google Scholar]
- 11. Durnin C, Hind ID, Ghani SP, Yates DB, Molz KH. Pharmacokinetics of oral immediate‐release hydromorphone (Dilaudid IR) in subjects with moderate hepatic impairment. Proc West Pharmacol Soc 2001;44:83‐84. [PubMed] [Google Scholar]
- 12. Novick DM, Kreck MJ, Fanizza AM, Yancovitz SR, Gelb AM, Stenger RJ. Methadone disposition in patients with chronic liver disease. Clin Pharmacol Ther 1981;30:353‐362. [DOI] [PubMed] [Google Scholar]
- 13. Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol 2008;6:69‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park SH, Wackernah RC, Stimmel GL. Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract 2014;27:71‐78. [DOI] [PubMed] [Google Scholar]
- 15. Saab S, Konyn PG, Viramontes MR, Jimenez MA, Grotts JF, Hamidzadah W, et al. Limited knowledge of acetaminophen in patients with liver disease. J Clin Transl Hepatol 2016;4:281‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Murphy EJ. Acute pain management pharmacology for the patient with concurrent renal or hepatic disease. Anaesth Intensive Care 2005;33:311‐322. [DOI] [PubMed] [Google Scholar]
- 17. Durnin C, Hind ID, Wickens MM, Yates DB, Molz KH. Pharmacokinetics of oral immediate‐release hydromorphone (Dilaudid IR) in subjects with renal impairment. Proc West Pharmacol Soc 2001;44:81‐82. [PubMed] [Google Scholar]


