Abstract
Background: Childhood obesity increases the risk of obesity and harmful comorbidities later in life. It is influenced by characteristics of a child's neighborhood, particularly among underserved groups. Our objective was to systematically review the evidence relating neighborhood environment and obesity risk among urban, low socioeconomic status (SES) Black and Hispanic children.
Methods: We included studies published from 1993 through early 2017 from PubMed, SCOPUS, Web of Science, and Sociological Abstracts databases investigating relationships between empirically measured neighborhood characteristics and obesity risk factors in the populations of interest. Databases were last searched on May 8, 2018. Initial analysis took place during 2014 and was completed during 2017. We extracted data on study population, design, and associations between neighborhood characteristics and obesity risk factors.
Results: We identified 2011 unique studies; 24 were included. Few studies demonstrated consistent patterns of association. Most neighborhood characteristics were not examined across multiple studies. BMI may be related to living in a lower-income neighborhood or convenience store access.
Conclusions: This review found that the body of evidence relating neighborhood exposures and obesity risk factors among urban, low SES Black (also commonly referred to in the literature as “non-Hispanic Black” or African American) and Hispanic children is limited. Given the high risk of obesity and cardiovascular disease among these populations throughout the life course, research on neighborhood determinants of obesity should specifically include these populations, ensuring adequate power and methodological rigor to detect differences.
Keywords: African American, childhood obesity, Hispanic, neighborhood, social determinants of health
Background
Childhood obesity affects one in six children in the United States. Low socioeconomic status (SES) and racial and ethnic minority children are disproportionately affected.1–3 Obesity in childhood is associated with lifelong obesity, which also increases the risk of cardiovascular disease (CVD) in adulthood.4 A simulation model based on current trends predicted that 57% of children today will be obese at age 35.5 Neighborhood environments are thought to influence childhood obesity risk in part through their potential effects on physical activity and diet. Therefore, the influence of neighborhood environment on obesity risk is a key area of ongoing research.6 While the literature regarding the types of environmental exposures examined is heterogeneous, most studies describe neighborhood environmental exposures in one or more of the following domains as potentially relevant to childhood obesity: neighborhood SES, food environment, physical activity environment, and social environment (e.g., crime).7
Neighborhood environments may also contribute to disparities in childhood obesity. For instance, low SES neighborhoods and neighborhoods with high concentrations of racial/ethnic minority residents tend to have higher concentrations of unhealthy foods and less access to affordable healthy foods; and individuals living in such neighborhoods are exposed to higher levels of crime and violence.8–16 Increased exposure to neighborhood crime and violence, in particular, has been linked to reduced energy expenditure and lower physical activity levels.8,14–16 Thus, the potential effects of adverse neighborhood conditions on obesity risk are further compounded among individuals living in low-income, predominantly racial/ethnic minority communities. Other potential mechanisms by which neighborhoods contribute to obesity disparities include chronic psychosocial stress and structural factors such as racial segregation, concentrated poverty, and discrimination that may potentiate material deprivation and stress.10,11,17,18
Prior research suggests that both access to larger food stores (e.g., grocery stores) and urban design characteristics (e.g., walkability) may influence obesity risk for Black and Hispanic adults. But, to our knowledge, no prior study has systematically reviewed the evidence for low SES Black and Hispanic children.13,19 Furthermore, many prior reviews aggregate results across child and adult populations to increase sample size and thus assume similarities in the associations between neighborhood environments and obesity risk across the life course, when in fact the relationships may differ.7,13,20–22 For instance, the scale at which neighborhood exposures may influence childhood obesity risk may be different compared with adults. In particular, for young children the characteristics of the immediate block where their home is located may have more bearing on outdoor play than neighborhood amenities located several blocks away. In contrast, for some children, planned extracurricular activities may occur largely outside the boundaries that define their neighborhood of residence.23 As such, the characteristics of a few blocks around the home could matter more than the overall characteristics of a larger area, such as a census tract.24
Living in a transit-oriented community may also have less bearing on children's physical activity than adults insofar as children in some settings may not use public transit to commute to school, while adults may use it more regularly for commuting. Additionally, parents may modify the extent to which they encourage their children to be active within their immediate neighborhood based on their perceptions of risk.25 They may also proactively seek resources outside their neighborhoods to provide their children access to alternative environments for physical activity or healthy eating, which may be different than the efforts that adults are willing to undertake for themselves. Focus group research by Showell et al. supports the notion that parents will compensate for neighborhood deficiencies and may go to great lengths to overcome neighborhood constraints to physical activity or healthy eating when their children's health is involved.
Despite the influence of neighborhood environments on childhood obesity risk, particularly among low-income and/or racial/ethnic minority children, research examining the evidence for environmental strategies to address childhood obesity among racial/ethnic minority children, particularly Black (also commonly referred to in the literature as “non-Hispanic Black” or African American) populations, is lacking.19 Given the increased lifetime risk of obesity for low SES and racial/ethnic minority children and associated increased risk of CVD and associated morbidity in adulthood,26 it is critical to examine the specific associations between neighborhood environmental exposures and obesity risk factors for these populations. Examining this association specifically among high-risk populations of children also serves to better inform and target prevention efforts or interventions at the subpopulations in greatest need, which is a necessary strategy for achieving health equity.
Study Purpose
The goal of this study was to systematically review the results of studies that investigated the association between neighborhood environment and obesity risk among urban, low SES Black and Hispanic children.
Methods
Eligibility Criteria
We identified studies that quantitatively analyzed an association between objectively-measured characteristics of residential neighborhoods of children aged 0–22 years (referred to as children) and BMI in a manner that conferred generalizability to Black or Hispanic children. Neighborhood definitions varied by study and included administrative boundaries such as census tracts, political boundaries such as counties, and buffers around the centroid of a zip code, an individual participant's address, or a community-defined neighborhood. Studies were deemed generalizable to Black or Hispanic children if they: (1) reported separate associations for Black and/or Hispanic children; (2) demonstrated no statistical differences in the association of neighborhood exposures and BMI between the overall population and the Black or Hispanic children in the cases where racial/ethnic minority subgroup analyses were performed; or (3) reported a study population ≥50% Black and/or Hispanic, which has been used in other studies seeking to identify relevant associations for a particular racial or ethnic group.19 Included studies were written in English, conducted in the United States or Canada, and included an urban population with low SES participants without known pre-existing medical conditions.
Literature Search Strategy
We searched PubMed, SCOPUS, Web of Science, and Sociological Abstracts databases to identify articles published between 1993 and early 2017. Prior reviews indicate that the majority of the literature emerged since 2000.7,13,20–22 The search strategy was developed and databases were chosen in consultation with a clinical librarian. Databases were last searched on May 8, 2018. Because we sought to be comprehensive in including early studies, our search timeframe dated back to 1993. Appendix Table A1 contains the complete strategy for PubMed. Earlier versions of the search strategy did not include all clinical outcomes that were ultimately selected for the final search strategy. The final search strategy yielded the most comprehensive set of relevant studies and included a full set of clinical and behavioral indicators of CVD risk applicable to populations of all ages. This included obesity, CVD and related conditions, eating behaviors, and physical activity behaviors. Search terms were originally developed as part of a larger review inclusive of both adults and children; therefore, some terms such as myocardial infarction and coronary artery disease were included.
This systematic review summarizes a subset of studies included in the overall search with a specific focus on obesity risk among low-income Black and Hispanic children and adolescents for whom age- and gender-specific BMI percentile and related measures (e.g., BMIz score) are appropriate. Our inclusion criteria allowed for studies with children and adolescents aged 0–22 years to be inclusive of older adolescents. However, once we reached the article abstraction phase, we evaluated all studies in our sample and determined that all studies either included children and adolescents between ages 2 and 18 years or high school students of an unspecified age range. We initially abstracted articles on physical activity behaviors as well; however, because of the small number of studies and variability in measurement, we restricted the final review to studies assessing the association of neighborhood characteristics with child BMI.
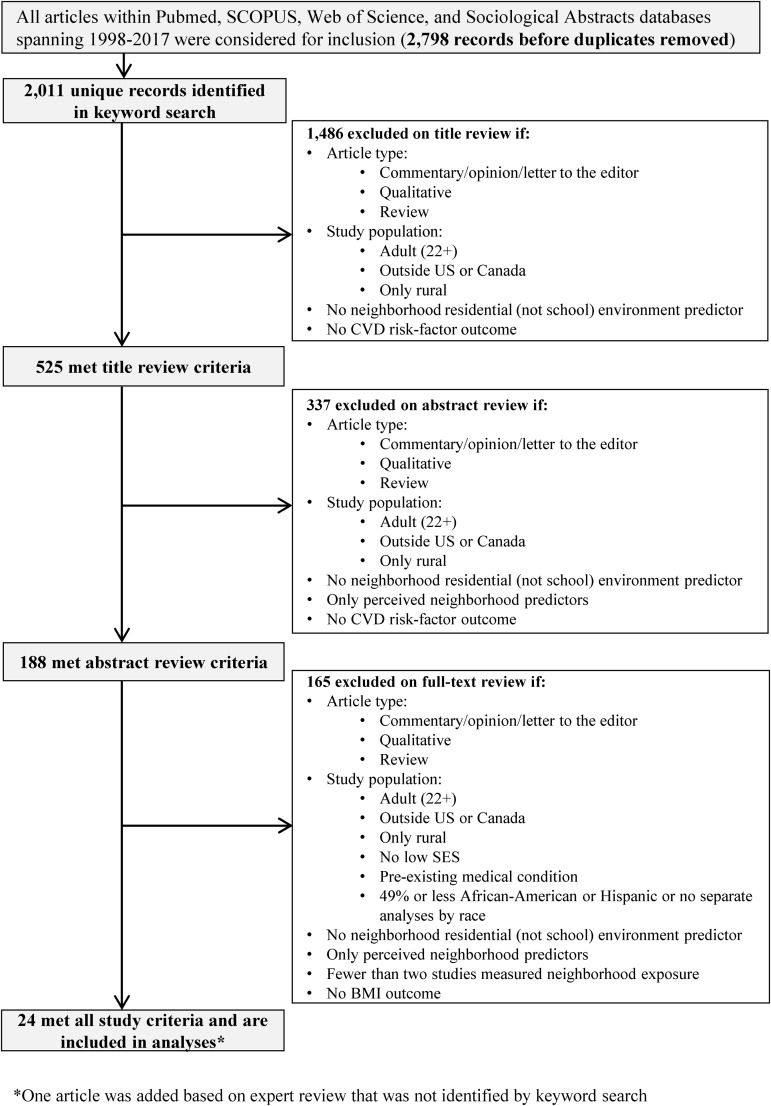
Of the 2011 unique records identified, 1486 were excluded at the title review stage because they were not original research, did not focus on children, or were not relevant to the exposures or outcomes under study. Of the 525 studies that met the criteria for inclusion at the title review stage, 337 were excluded because of the article type, study population, or exposures and outcomes reported in the abstract. An additional 165 were excluded at the full article review phase for similar reasons. Ultimately, we restricted this analysis to studies with outcomes of BMI or age-appropriate measures derived from BMI (e.g., BMI percentile, weight status categories based on BMI percentile, BMI z-score), as these were, by far, the most consistently reported outcomes and are consistent with the measures routinely used in pediatric clinical practice to assess obesity risk throughout the life course. There were 24 studies included in the final sample; one study was included in the final sample based on expert review, which was not identified by keyword search.
Article Screening and Full-Text Review
Initial search results were imported into RefWorks, and a subsequent search to update the database with articles published after 2013 was imported into Endnote.27,28 Duplicates were identified and removed in both reference management databases. Reviewers independently screened article titles and abstracts. Full texts of included titles/abstracts were retrieved, and these articles were screened for inclusion using the eligibility criteria described below. Discrepancies were resolved by discussion between reviewers and adjudicated by full-group consensus when needed.
Data Extraction and Management
Articles were reviewed by study author and team member (K.A.J.) and at least one other study team member. Two independent reviewers extracted data from each article, reviewed each field jointly, and adjudicated discrepancies. If agreement could not be reached through discussion and reviewing the source article, a third team member (either N.N.S. or R.L.J.T.) reviewed the article and adjudicated to achieve consensus. An electronic form designed using Qualtrics29 online survey software was used to extract data. To pilot the form and calibrate coding, all team members extracted data from four test articles using a draft form that was subsequently finalized.
Information regarding study population, study design, and measurements of associations between neighborhood characteristics and obesity risk were extracted from each article, including study population characteristics such as sample racial/ethnic and SES composition.
Neighborhood Exposure Measures
Four groups of neighborhood characteristics were examined: SES, food environment, physical activity environment, and crime. These groups of neighborhood exposures were selected because they represent the most common exposures found in prior reviews and/or are hypothesized to be particularly relevant for the population of interest. Only objectively-measured neighborhood exposures were included. Many of these exposure measures relied on the use of publicly-available data sources (e.g., US Census Data). Neighborhood exposures were considered to be objectively measured if they were derived from data that could be quantified and did not rely on subjective measures such as residents' perceptions. For example, we included neighborhood crime exposures that relied on reported crime counts or rates (e.g., crime data available from the Cincinnati police department30) but excluded studies where the neighborhood crime exposure was measured using residents' perceptions of crime or safety. For measures examining access to food retailers or physical activity resources, researchers also identified the methods used to operationalize access (i.e., whether the study examined access in terms of proximity, density, both, or another method).
Outcome Variables
The primary outcome for included studies was BMI. Associations were reported for the overall study population and for Black and Hispanic children, if these were reported separately.
Data Synthesis and Analysis
Initial analyses were completed in 2014 and updated during 2017. We created evidence tables containing information from the included studies. Each reported relationship between a neighborhood factor and outcome of interest in the authors' final, adjusted model was coded as follows: significant and direct (+), significant and inverse (−), not significant (0), mixed results (X), or other. As there was substantial variation in study design and context, significance levels were based on the original authors' definition of significance. Most studies used a p < 0.05 significance level; however, several studies used a p < 0.10 threshold.
BMI assessments were coded such that a significant inverse association indicated statistically significant decreasing BMI (generally considered a desirable outcome) as the neighborhood factor increased. For example, a study that reported a significant and inverse association between neighborhood income and BMI would show that, with increasing neighborhood income, BMI decreased. “Mixed results” was used to identify instances where there were multiple measures of a particular type of outcome, and the direction of the associations with a specific neighborhood factor was inconsistent. “Other” was used if the neighborhood factor was included in the final, adjusted model, but the significance and directionality were not reported. Neighborhood factors were always coded such that an increase represented an increase in the specific characteristic as described on the extraction form (Table 1).
Table 1.
Neighborhood Exposures by Category
| Neighborhood SES |
| Neighborhood income |
| Neighborhood education |
| Composite measure of neighborhood SES |
| Neighborhood food environment |
| Grocery store/supermarket access |
| Corner/convenience store access |
| Fast food access |
| Composite measure of the food environment |
| Neighborhood physical activity environment |
| Walkability |
| Recreation facility access |
| Park/playground access |
| Pedestrian safety measures |
| Traffic speed/volume |
| Vegetation |
| Neighborhood crimea |
Derived from objectively-measured crime statistics for a specific geographic area.
SES, socioeconomic status.
To characterize the evidence for each neighborhood factor and BMI, counts and measures of central tendency were calculated. We did not summarize relationships to obesity for neighborhood exposures examined in less than two studies. Researchers identified the articles with results most generalizable to Black and Hispanic children and conducted stratified analyses.
Associations between neighborhood factors and obesity risk were compared manually between studies of different quality, children of different ages, and different measurement modalities for outcome variables. A meta-analysis was not performed due to wide variability in exposure definitions and specific outcomes across studies. For those studies with adequate data reported in the articles reviewed, we graphically displayed effect sizes for the associations between BMI, obesity, or overweight across studies where both effect sizes and 95% confidence intervals were provided. Some effects were reported as regression coefficients (such as the association between standardized BMI and proximity to greenspace), while other studies reported effect sizes as odds ratios (such as the association between obesity and proximity to greenspace).
Study Quality (Risk-of-Bias Assessment)
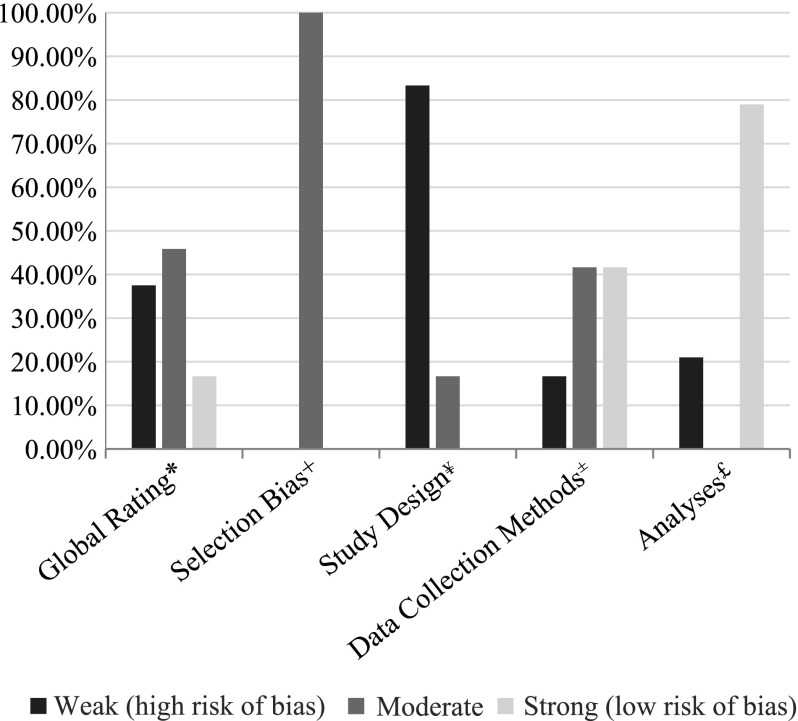
Study quality was coded as strong, moderate, or weak based on the risk of bias in the study design. We used a modified version of the Quality Assessment Tool from the Effective Public Health Practice Project (EPHPP).31 A previous study on evaluating natural experiments in obesity used the EPHPP tool; this study cited benefits of using this tool to evaluate quality of obesity studies, including simplicity and interpretability across study designs.32 Four components of study quality were assessed: selection bias, study design, data collection methods, and analyses.
Selection bias was assessed in reference to the likelihood that the study was representative of the target population of low SES Black and Hispanic children in the United States. Because our study inclusion criteria were to only include studies that had either majority Black or Hispanic children or separate analyses by race, we determined that each study was somewhat likely to be representative of the target population, and thus moderate quality for selection bias.
Study design was rated as moderate quality if it was longitudinal and weak quality if it was cross-sectional. The EPHPP quality measure only categorizes randomized controlled trials as strong quality for the study design category.
Data collection methods were rated in terms of validity and reliability of collection of outcome measures. If BMI was self-reported, it was considered not validated and not reliable. If BMI was measured by study staff or clinic staff, it was considered valid, and if the measurements were taken by people who were trained or taken multiple times, they were considered reliable. If outcome measurement was determined to be both valid and reliable, it was categorized as strong; if outcome measurement was either valid or reliable, it was categorized as moderate; if it was determined to be neither valid nor reliable, it was categorized as weak.
Analyses were considered strong quality if neighborhood-level clustering was accounted for. A global rating was made for each study based on these four criteria. Studies were considered strong if they had no weak ratings, moderate if they had one weak rating, and weak if they had two or more weak ratings.
Results
Search Results
A total of 24 articles were included (Fig. 1).30,33–55 We identified 2011 unique records, 23 of which were included in this review after title, abstract and article screening, and an additional article50 was identified based on expert review that did not come up using our database search strategy.
Figure 1.
PRISMA flow diagram.
Study Characteristics
Measurements of association were most commonly reported as odds ratios. Measures used to evaluate the proportion of low SES participants included parental educational attainment, household income, and eligibility for means-tested benefit programs (e.g., Medicaid).
The direction and significance of each reported relationship between neighborhood characteristics (Table 1) and obesity risk were considered. Study designs, methods of defining a child's neighborhood, and other characteristics of included studies are in Table 2. Study quality by category and global rating is shown in Figure 2. Most studies were either low or medium quality30,33–55; only four utilized a longitudinal design.51–54 The vast majority of studies used an administrative boundary or buffer around a child's residence for neighborhood measurement tactics.
Table 2.
Characteristics of Included Studies (n = 24)
| Study characteristic | n (%) |
|---|---|
| Study quality (risk of bias)a | |
| Weak quality | 9 (38) |
| Moderate quality | 10 (42) |
| Strong quality | 5 (21) |
| Neighborhood definition(s)b | |
| Administrative boundaryc | 19 (79) |
| Buffer around residence | 11 (46) |
| Otherd | 8 (33) |
| Political boundarye | 2 (8) |
| Age | |
| Early childhood (2–5 years) | 3 (13) |
| School age (5–14 years) | 8 (33) |
| Adolescents (12–21 years) | 6 (25) |
| All ages (∼2 to ∼18 years) | 5 (21) |
| Other | 2 (8) |
| Race/ethnicity | |
| Separate analysis for Black children | 3 (13) |
| Studies with ≥50% Black participants | 11 (46) |
| Separate analysis for Hispanic children | 2 (8) |
| Studies with ≥50% Hispanic participants | 6 (25) |
Study quality was determined by risk of bias; see Methods section.
Categories do not sum to 100% as many studies used multiple definitions.
Defined by the census, for example, census tract or zip code.
For example, buffer around centroid of zip code, or community-defined neighborhood.
Defined as political jurisdiction, for example, county, city, or voting district boundaries.
Figure 2.
Study quality bar graph. *Global rating: Studies were considered strong if they had no weak ratings, moderate if they had one weak rating, and weak if they had two or more weak ratings. +Selection bias: Selection bias was determined based on the extent to which the study population was deemed representative of the target population. Based on our racial inclusion criteria, the study team deemed all studies to be somewhat likely to be representative; this equated with a moderate quality with respect to selection bias. ¥Study Design: To be rated strong, a study had to involve a randomized controlled design; none of the included studies did. Moderate studies used a longitudinal design. Weak studies used a cross sectional design. ±Data Collection Methods: Strong studies used study or clinic staff to measure height and weight. Moderate studies used BMI measurements that were taken multiple times. Weak studies used self-reported BMI. £Analyses: We dichotomized this criterion into strong and weak to be more applicable for observational studies. Studies were rated as strong if they accounted for neighborhood-level clustering and weak if they did not account for neighborhood-level clustering.
Study Population Characteristics
Study populations differed across studies (Table 2). Eight studies (33%) examined relationships among school-aged children (ages 5–14), 6 (25%) among adolescents (ages 12–21), and 3 (13%) in younger children (ages 2–5). Eleven studies of Black children and six of Hispanic children either reported associations separately, or had ≥50% participants who were Black or Hispanic, respectively. These studies comprised the sample for the stratified analyses by race/ethnicity.30,35–37,39–43,45,47,48,51,53–55
Study Outcomes
Common BMI assessments included BMI percentile and BMI z-score. Other outcomes were infrequently reported and were excluded from subsequent analyses. Relationships are only reported between neighborhood factors and BMI for factors for which there were at least two studies examining their effect on BMI.
Associations between Neighborhood Factors and BMI
Table 3 reports the associations between neighborhood exposures and BMI. Studies that included ≥50% or a separate analysis of Black children (Appendix Table A2), and studies that included ≥50% or a separate analysis of Hispanic children (Appendix Table A3) are included in the Appendix. Findings were mixed overall and for specific age groups and racial/ethnic populations. Few neighborhood factors were examined by multiple studies, and fewer still revealed consistent associations. Frequently, studies reported multiple associations between a specific neighborhood characteristic and outcome—for instance, separately reporting relationships with BMI of fast food restaurant density and proximity. Some also provided associations by different subgroups (e.g., by sex), which were included separately. As such, studies where multiple associations were assessed may be categorized as “mixed results” if different findings (e.g., both null and direct relationships) between a specific neighborhood exposure and outcome were reported or “other” if authors' stated variable was included in adjusted estimates, but results were not reported.
Table 3.
Associations between Neighborhood Characteristics and BMI for the Overall Study Population of Included Studies
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 33,38,41,42,44–46,48,50–53 | 0 | 3 | 5 | 1 | 3 |
| Neighborhood education | 44,53 | 0 | 0 | 1 | 1 | 0 |
| Composite SES measure | 34,36,37,50,54 | 0 | 4 | 1 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | 35,39,41,48,52 | 0 | 3 | 0 | 2 | 0 |
| Corner/convenience store access | 33,35,39–41,46,48,52 | 3 | 4 | 0 | 1 | 0 |
| Fast food access | 30,33,39,41,46–49,52 | 0 | 5 | 2 | 1 | 1 |
| Composite food environment | 34,41,48,54,55 | 1 | 2 | 0 | 2 | 0 |
| Physical activity environment | ||||||
| Walkability | 33,38,42,51 | 0 | 2 | 1 | 1 | 0 |
| Park/playground access | 30,38,42,46,55 | 0 | 3 | 1 | 1 | 0 |
| Traffic speed/volume | 38,42 | 0 | 2 | 0 | 0 | 0 |
| Vegetation | 41,51 | 0 | 0 | 2 | 0 | 0 |
| Neighborhood crime | ||||||
| Crime | 30,42,43,49,54 | 1 | 3 | 0 | 1 | 0 |
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance were not reported.
Variations in study quality, measurement modalities, or participant ages did not appear to have consistent or significant effects on the direction or strength of associations detected between neighborhood characteristics and outcomes of interest. Appendix Tables A4–A6 display associations for BMI assessments by study quality.
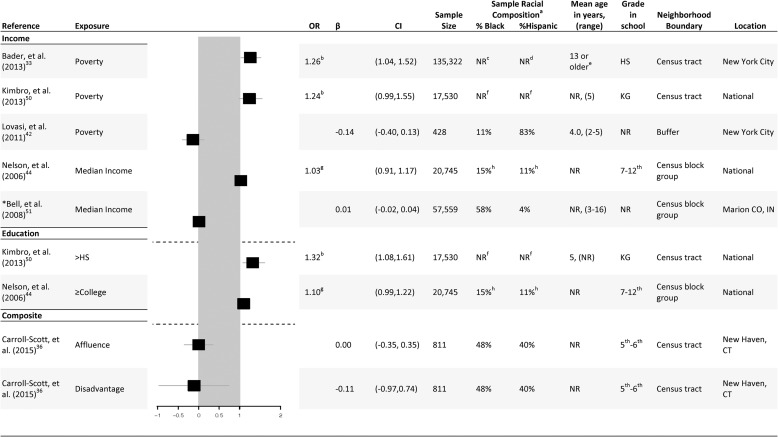
Neighborhood SES
Sixteen studies reported associations between neighborhood SES and BMI for overall study populations.33,34,36–38,41,42,44–46,48,50–54 Findings for studies with point estimates and confidence intervals are displayed in a forest plot (Fig. 3). These primarily investigated the relationship between neighborhood SES and BMI as measured by neighborhood income or a composite SES measure. Four studies36,37,50,54 found no association between a composite SES measure and BMI; one study34 found an inverse association between composite SES and BMI. Three studies found no association between a neighborhood income and BMI, and five studies found an inverse relationship between neighborhood income and BMI.
Figure 3.
Neighborhood socioeconomic status forest plot. *Longitudinal study design. aStudies met inclusion criteria if ≥50% of the study populations were Black or Hispanic, or if the study reported on subgroup analyses by race or evaluated the extent to which a particular neighborhood exposure was associated with child BMI among Black or Hispanic study subpopulations. bOdds ratio obese vs. normal weight. cThis study did not report racial composition for the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Black participants who were obese. dThis study did not report racial composition for the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Hispanic participants who were obese. eThe study did not report mean age or age range. The study sample consisted of high school students ≥13 years. fThis study did not report racial composition of the overall study population; it did adjust for race/ethnicity and was composed of a nationally representative sample. gRisk ratio of BMI ≥95% percentile (obese). hThis study adjusted for race/ethnicity in analyses. HS, high school; KG, kindergarten; NR, not reported; OR, odds ratio.
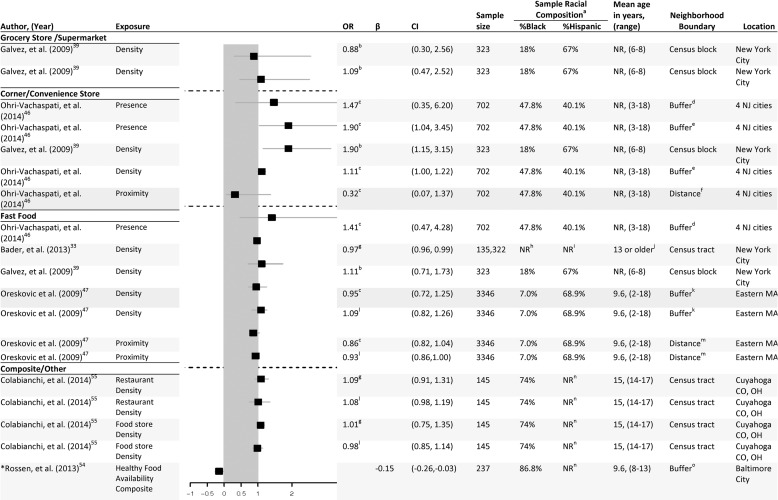
Neighborhood Food Environment
Overall, 14 studies30,33–35,39–41,46–49,52,54,55 reported associations between aspects of neighborhood food environment and BMI outcomes. Findings from these studies are displayed in a forest plot (Fig. 4). The most frequently assessed exposures were corner/convenience store (8 studies33,35,39–41,46,48,52) and fast food access (9 studies30,33,39,41,46–49,52). The most consistent evidence for a relationship between a characteristic of a child's neighborhood food environment and BMI was corner/convenience store access, particularly among Hispanic children. Three of eight studies39,41,48 found a direct relationship for overall study populations, suggesting that BMI may rise as access to corner/convenience stores increases. All three of these studies were low quality.39,41,48 Both studies examining this relationship specifically among Hispanic children (ages 8–1039 and 14–16,48 respectively) found a significant, direct association. There was no consistent relationship between fast food access and BMI in overall study populations or specifically among Black or Hispanic children of any age.
Figure 4.
Neighborhood food environment forest plot. *Longitudinal study design. aStudies met inclusion criteria if ≥50% of the study populations were Black or Hispanic, or if the study reported on subgroup analyses by race or evaluated the extent to which a particular neighborhood exposure was associated with child BMI among Black or Hispanic study subpopulations. bOR child's BMI percentile being in the top tertile. cOR overweight or obese vs. normal weight. d0.5 mile radius buffer around child's residence. 0.25 mile radius buffer around child's residence. fDistance to nearest convenience store from child's home was measured in roadway network miles. gOR obese vs. normal weight. hThis study did not report racial composition of the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Black participants who were obese. iThis study did not report racial composition of the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Hispanic participants who were obese. jThe study did not report mean age or age range. The study sample consisted of high school students ≥13 years. k400 m buffer zone around child's residence. lOverweight vs. normal weight. mDistance to the nearest fast food restaurant was measured via street networks from child's residence. nRacial composition of the sample was not reported for all participants; only the percentage of Black was reported. o100 m buffer of path between child's home and school.
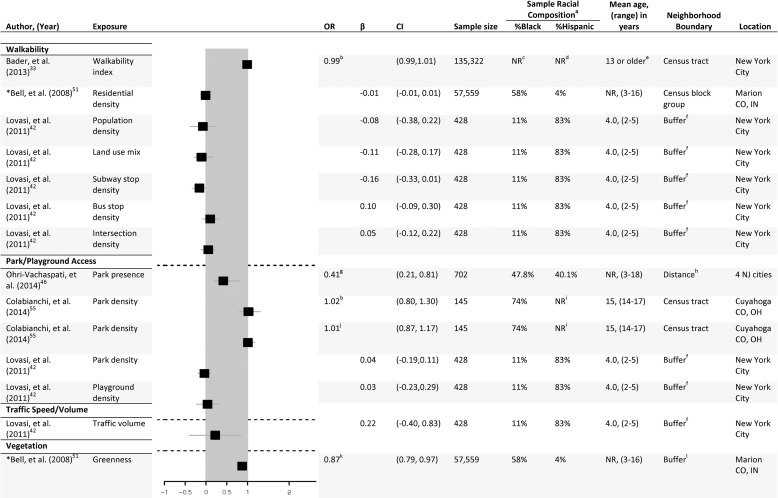
Neighborhood Physical Activity Environment
Eight studies30,33,38,41,42,46,51,55 measured associations between characteristics of physical activity environment, mainly park/playground access, and BMI within overall study populations. Findings of these studies are displayed in a forest plot in Figure 5.
Figure 5.
Neighborhood physical activity environment forest plot. *Longitudinal study design. aStudies met inclusion criteria if ≥50% of the study populations were Black or Hispanic, or if the study reported on subgroup analyses by race or evaluated the extent to which a particular neighborhood exposure was associated with child BMI among Black or Hispanic study subpopulations. bObese vs. normal weight. cThis study did not report racial composition of the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Black participants who were obese. dThis study did not report racial composition of the overall study population; it adjusted for race/ethnicity. The study reported on the proportion of Hispanic participants who were obese. eThe study did not report mean age or age range. The study sample consisted of high school students ≥13 years. fBuffer drawn as a 0.5 km buffer around a line between the child's home and school. gOR overweight or obese vs. normal weight. hPark presence within half a mile radius of child's home. iRacial composition of the sample was not reported for all participants; only the percentage of Black was reported. jOverweight vs. normal weight. kOR of increasing BMI-z over time. l1 km straight line circular buffer surrounding child's residence.
Two studies41,51 reported relationships between neighborhood vegetation (measured using Normalized Difference Vegetation Index, a measure of greenness derived from satellite pictures) and BMI. Both these studies reported an inverse relationship between vegetation and BMI overall and for Black children. One study was high quality51 and one was low quality.41
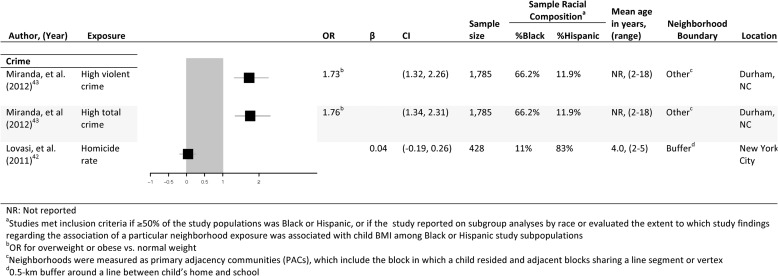
Neighborhood Crime
Five studies30,42,43,49,54 reported associations between neighborhood crime and BMI. These studies reporting on the association between crime only and BMI found no consistent relationships. Findings from these studies are displayed in a forest plot in Figure 6. Three of these studies found no association between crime and BMI30,42,54; one43 had mixed results; and one had a significant, positive relationship.
Figure 6.
Neighborhood crime forest plot. aStudies met inclusion criteria if ≥50% of the study populations were Black or Hispanic, or if the study reported on subgroup analyses by race or evaluated the extent to which a particular neighborhood exposure was associated with child BMI among Black or Hispanic study subpopulations. bOR for overweight or obese vs. normal weight. cNeighborhoods were measured as PACs, which include the block in which a child resided and adjacent blocks sharing a line segment or vertex. d0.5 km buffer around a line between child's home and school. NR, not reported; PAC, primary adjacency community.
Conclusion and Discussion
Our systematic review found that the body of research specifically examining the relationship between neighborhood environments and obesity risk among low-income African American and Hispanic children of any age is limited. Of the studies that exist with findings applicable to these populations, the strongest evidence suggests that urban, low SES Black and Hispanic children living in poorer neighborhoods and those with increased access to corner/convenience stores had higher BMIs, while those living in neighborhoods with more vegetation had lower BMIs. There is not enough evidence regarding neighborhood social environment, particularly neighborhood crime, to suggest an association with increased BMI. Grocery store access, one of the most common proxies in the literature for a healthful food environment,8 was not related to BMI for the focal populations.
Perhaps the most striking finding of this review is the dearth of research specifically examining the association between neighborhood environments and obesity risk for urban, low SES Black and Hispanic children of all ages. Less than 2% of the 2011 studies identified in our literature search provided relevant findings for urban, low SES Black or Hispanic children. Only 11 of these studies had either a majority Black study population or conducted separate analyses for Black children, and only 6 had either a majority of Hispanic children or conducted separate analyses for Hispanic children. Of the studies that reached the article review phase (n = 188), only 24 met all study criteria (13%). This is a very small evidence base, particularly given that these populations are known to be at increased risk of obesity throughout the life course, and may also experience differences in neighborhood context that further potentiate this risk compared with other socioeconomic and racial/ethnic groups of children within the United States.
Other limitations of this evidence base relate to the fact that these studies span multiple age groups for whom the mechanisms by which neighborhood environments impact obesity risk may be different. For example, toddlers and young children (ages 2–5 years) are likely to interact with neighborhood environments, particularly with respect to physical activity and its impacts on obesity, with their surroundings very differently than adolescents or school-aged children for whom fast food or healthy food access may be more strongly associated with obesity risk. Thus, the size of the relevant evidence base generalizable to low-income Black and Hispanic children in urban areas is quite low compared with the burden of disease among this population.
Similarly, this review points out the lack of a consistent approach to understanding environmental determinants of obesity risk among these high-risk populations and emphasizes the importance in future research of ensuring that the sample size of Black and Hispanic children in such studies is adequate to detect effects, whether in studies tailored to look at relationships only in these populations or in nationally representative studies where subgroup analyses to assess relationships for these specific groups are examined.
Thus, despite widespread interest in implementing policies to support healthy weight among these high-risk children, there is a need to invest in additional research to inform such policies.7
Limitations
There are several potential sources of bias in this review, as well as in the underlying studies. The majority of studies reviewed used cross-sectional analyses that cannot assess temporality, and many did not properly statistically control for the clustering of children in neighborhoods, which can bias results and inflate effect sizes.8 The interpretation of study results may be limited because most studies relied on school- and clinic-based sampling frames, which may result in a sample of children whose health outcomes or exposures are not fully representative of a given neighborhood.
Additionally, this review demonstrates the variability of neighborhood definitions in this body of research. This variability in measurement of neighborhood exposures using administrative data sources highlights the need for theory-driven research and further efforts within the scientific community to develop, disseminate, and implement a set of recommendations regarding best practices for measuring neighborhood environments for health disparities and childhood obesity research. A recent systematic review of natural experiments and obesity may provide concrete guidance to this field regarding measurement of environmental factors, and it also outlines key methodological considerations for future research examining the association between environmental factors and obesity whether through natural experiments or observational studies.32
Our decision to use a select approach to determine study quality brings about certain limitations as well. We chose to use this approach as it is a standardized, organized method of study quality assessment. However, this approach did not allow for a consideration of individual- and neighborhood-level confounders. These confounders could introduce a risk of bias in our studies that is not captured in our study quality categorization.
Given that the true causally-relevant geographic area is unknown, future research should use strategies to reduce the effects of uncertain geographic context problem on inference.56 Some of the studies included did make attempts to do this, though these findings were not a focus of the review. Future reviews specifically focused on relevant geography for environmental effects among low-income Black and Hispanic children are also needed. Studies included in this review operationalized neighborhood boundaries in multiple ways. For example, one study compared the association between several neighborhood factors and obesity using three different neighborhood boundaries: self-defined, 0.75 mile buffer around participants' home addresses, and census tracts.55 Other studies used zip code48 or other municipal boundaries.47
Similarly, this review did not examine neighborhood segregation or neighborhood racial/ethnic composition as it relates to obesity risk. There is a growing body of childhood obesity research in this area, and it warrants attention in future reviews. Also, the results of this review may overstate the evidence for statistically significant relationships between neighborhood exposures and obesity risk because studies reporting null results are less likely to be published (publication bias). Yet, the challenges of measuring neighborhood exposures with precision would tend to bias the results of such analyses toward the null, assuming that measurement error is nondifferential. Thus, any significant findings may be suggestive of an even stronger “true” association between neighborhood exposures and obesity risk. Given the variability in the research summarized in this review, we did not conduct a formal meta-analysis or funnel plot analysis to assess publication bias, which should be part of future meta-analyses in this area.
Some included studies reported pooled results for children across SES strata and for children of different urbanicity; so the results of these studies may be less generalizable to the low SES Black and Hispanic children who are the focus of this review. This may be particularly problematic for SES, as race and SES are strongly correlated in the United States and Canada. In the case of a study stratified by urbanicity, we presented results for children from an urban area and excluded studies focusing only on rural populations from the review.35 However, most studies in this review focused on urban populations or aggregated across different urbanicities; so future research should explore whether and how relationships between neighborhood environments and obesity vary in rural, suburban, and urban contexts for low SES Black and Hispanic children. Similarly, relevant studies were excluded if adiposity measures other than BMI-derived measures were used, which may result in missing important information about neighborhood environments and growth patterns among children relevant to childhood obesity risk.
To our knowledge, this is the first study to systematically review the evidence linking neighborhood characteristics to BMI among urban, low SES Black and Hispanic children. While there are limitations to this review, it fills a critical gap in the literature and highlights the need for additional, rigorous research assessing the association between neighborhood characteristics and CVD risk factors for high-risk children from early childhood through adolescents. This includes a need for more longitudinal studies and those that assess possible effects of exposure at critical times in a child's development, such as in early childhood when lifelong taste preferences, dietary habits, and physical activity patterns are being formed.57
Acknowledgments
The authors would like to thank the biostatistician Jamie Perin, PhD, for her assistance with analyses to produce forest plots for this review. We would like to thank Susan You and Caroline Pribble for their assistance with article revisions. We also wish to thank JHU Clinical Informationist Katie Lobner for her guidance in developing the search protocol, and Tracy Yang for her work on title and abstract review phase. Support for this study and to Dr. Johnson was provided by the Center for a Livable Future—Lerner Fellowship and the Johns Hopkins Bloomberg School of Public Health Sommer Scholarship. Drs. Showell and Thornton also received support from the Johns Hopkins Center to Eliminate Cardiovascular Health Disparities funded by the National Heart, Lung, and Blood Institute (grant ID P50HL0105187). Dr. Thornton was also supported by the National Heart, Lung, and Blood Institute (grant ID K23HL121250-01A1). Dr. Showell was also supported by the Johns Hopkins Institute for Clinical and Translational Research (grant ID KL2 TR001077).
Appendix
Appendix Table A1.
Complete Literature Search Strategy and Search Terms for PubMed
| PubMed |
| (“Urban Health”[Mesh] OR “City Planning”[Mesh] OR “Environment Design”[Mesh] OR “Urban Renewal”[Mesh] OR “Cities”[Mesh] OR “urban”[tiab] OR “inner city”) |
| AND |
| (“transit” OR “mixed use” OR “pedestrian” OR “environment design” OR “environmental design” OR “built environment” OR “walkability” OR “walkable” OR “green space” OR “park”[tiab] OR “parks”[tiab] OR “community garden” OR “community gardens” OR “food environment” OR “food security” OR “food desert” OR “fast food” OR “restaurant density” OR “Healthy Food Availability Index”[all] OR “HFAI” OR “nutrition environment measures survey”[all] OR “NEMS” OR “nutrition environment”[all] OR “alcohol outlets” OR “alcohol sales” OR “alcohol availability” OR “taverns” OR “tavern” OR “vehicle ownership” OR “car ownership” OR “automobile ownership”[all] OR “social environment” OR “social context” OR “neighborhood”) |
| AND |
| (“Cardiovascular Diseases”[Mesh] OR “Hyperlipidemias”[Mesh] OR “Diabetes Mellitus, Type 2”[Mesh] OR “Obesity”[Mesh] OR “Exercise”[Mesh] OR “cardiovascular disease” OR “cardiovascular diseases” OR “hyperlipidemias” OR “hyperlipidemia” OR “diabetes mellitus” OR “obesity” OR “obese” OR “exercise” OR “physical activity” OR “fruit” OR “vegetable” OR “vegetables” OR “Healthy eating index” OR “dietary outcome” OR “dietary outcomes” OR “diet” OR “BMI” OR “weight” OR “overweight” OR “prediabetes” OR “Coronary Artery Disease”[Mesh] OR “Myocardial Infarction”[Mesh] OR “coronary artery disease” OR “myocardial infarction” OR “Life Style”[Mesh] OR “Sedentary Lifestyle”[Mesh] OR “Diet”[Mesh] OR “life style” OR “lifestyle” OR “lifestyles” OR “life styles” OR “Hypertension”[Mesh] OR “hypertension” OR “high blood pressure”) |
| AND |
| (“Child”[mh] OR “Infant”[mh] OR “Infant, Newborn”[mh] OR “Adolescent”[mh] OR “Child, Preschool”[mh] OR “child”[tiab] OR “infant”[all] OR “adolescent”[all] OR “children”[all] OR “infants”[all] OR “adolescents”[all] OR “pediatric patient”[all] OR “pediatric patients”[all] OR “adolescence”[all] OR “youth”[all] OR “youths”[all] OR “juvenile”[all] OR “childhood”[all] OR “teenager”[all] OR “teenagers”[all] OR “teen”[all] OR “teens”[all] OR “preschool child”[all] OR “neonate”[all] OR “newborn”[all] OR “baby”[all] OR “pediatric”[tiab] OR “pediatrics”[tiab] OR “paediatric”[tiab] OR “paediatrics”[tiab]) |
| AND |
| (“US”[tw] OR “United States”[tw] OR “America”[tw] OR “american”[tw] OR “U.S.”[tw] OR “U. S.”[tw] OR “USA”[tw] OR “U.S.A.”[tw] OR “U. S. A.”[tw] OR “Canada”[mh] OR “Canada”[tw] OR “Canadian”[tw]) |
Updated search February 23, 2017, limited to 2014–2017/English, 397 results.
Appendix Table A2.
Associations between Neighborhood Characteristics and BMI for Black Youth
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 41,48,51,53 | 0 | 2 | 1 | 1 | 0 |
| Neighborhood education | 53 | 0 | 0 | 1 | 0 | 0 |
| Composite SES measure | 36,54 | 0 | 2 | 0 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | 41,48 | 0 | 1 | 0 | 1 | 0 |
| Corner/convenience store access | 35,41,49 | 1 | 2 | 0 | 0 | 0 |
| Fast food access | 30,41,48 | 0 | 2 | 0 | 1 | 0 |
| Composite food environment | 41,48,54,55 | 0 | 1 | 0 | 2 | 1 |
| Physical activity environment | ||||||
| Walkability | 51 | 0 | 0 | 1 | 0 | 0 |
| Park/playground access | 30, 55 | 0 | 1 | 0 | 1 | 0 |
| Traffic speed/volume | — | |||||
| Vegetation | 41,51 | 0 | 0 | 2 | 0 | 0 |
| Crime | ||||||
| Crime | 30,43,54 | 0 | 2 | 0 | 1 | 0 |
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance were not reported.
SES, socioeconomic status.
Appendix Table A3.
Associations between Neighborhood Characteristics and BMI for Hispanic Youth
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 42,45,48 | 0 | 1 | 1 | 1 | 0 |
| Neighborhood education | — | |||||
| Composite SES measure | 37 | 0 | 1 | 0 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | 39,48 | 0 | 1 | 0 | 1 | 0 |
| Corner/convenience store access | 39,48 | 2 | 0 | 0 | 0 | 0 |
| Fast food access | 39,47,48 | 0 | 1 | 0 | 1 | 1 |
| Composite food environment | 48 | 0 | 0 | 0 | 0 | 1 |
| Physical activity environment | ||||||
| Walkability | 42 | 0 | 1 | 0 | 0 | 0 |
| Park/playground access | 42 | 0 | 1 | 0 | 0 | 0 |
| Traffic speed/volume | 42 | 0 | 1 | 0 | 0 | 0 |
| Vegetation | — | 0 | 0 | 0 | 0 | 0 |
| Neighborhood crime | ||||||
| Crime | 42 | 0 | 1 | 0 | 0 | 0 |
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance was not reported.
Appendix Table A4.
Associations between Neighborhood Characteristics and BMI Among Strong-Quality Studies
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 51–53 | 0 | 1 | 2 | 0 | 0 |
| Neighborhood education | 53 | 0 | 0 | 1 | 0 | 0 |
| Composite SES measure | 54 | 0 | 1 | 0 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | 52 | 0 | 1 | 0 | 0 | 0 |
| Corner/convenience store access | 52 | 0 | 1 | 0 | 0 | 0 |
| Fast food access | 52 | 0 | 1 | 0 | 0 | 0 |
| Composite food environment | 54 | 0 | 0 | 0 | 1 | 0 |
| Physical activity environment | ||||||
| Walkability | 51 | 0 | 0 | 1 | 0 | 0 |
| Park/playground access | — | 0 | 0 | 0 | 0 | 0 |
| Traffic speed/volume | — | 0 | 0 | 0 | 0 | 0 |
| Vegetation | 51 | 0 | 0 | 1 | 0 | 0 |
| Neighborhood crime | ||||||
| Crime | 54 | 0 | 1 | 0 | 0 | 0 |
Studies were considered strong quality if they had no weak ratings for selection bias, study design, data collection methods, or analyses.
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance were not reported.
Appendix Table A5.
Associations between Neighborhood Characteristics and BMI among Moderate-Quality Studies
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 33,42,45,50 | 0 | 1 | 3 | 0 | 0 |
| Neighborhood education | — | 0 | 0 | 0 | 0 | 0 |
| Composite SES measure | 34,36,50 | 0 | 2 | 1 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | — | 0 | 0 | 0 | 0 | 0 |
| Corner/convenience store access | 33 | 0 | 1 | 0 | 0 | 0 |
| Fast food access | 30,33,47,49 | 0 | 1 | 2 | 1 | 0 |
| Composite food environment | 34,55 | 1 | 1 | 0 | 0 | 0 |
| Physical activity environment | ||||||
| Walkability | 33,42 | 0 | 2 | 0 | 0 | 0 |
| Park/playground access | 30,42,55 | 0 | 2 | 0 | 1 | 0 |
| Traffic speed/volume | 42 | 0 | 1 | 0 | 0 | 0 |
| Vegetation | – | 0 | 0 | 0 | 0 | 0 |
| Neighborhood crime | ||||||
| Crime | 30,42,43,49 | 1 | 2 | 0 | 1 | 0 |
Studies were considered moderate quality if they had one weak rating on selection bias, study design, data collection methods, and analyses.
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance were not reported.
Appendix Table A6.
Associations between Neighborhood Characteristics and BMI among Weak-Quality Studies
| BMI study counts | ||||||
|---|---|---|---|---|---|---|
| Neighborhood exposure | Refs. | + | 0 | − | Mixed | Other |
| Neighborhood SES | ||||||
| Neighborhood income | 38,41,44,46,48 | 0 | 1 | 0 | 1 | 3 |
| Neighborhood education | 44 | 0 | 0 | 0 | 1 | 0 |
| Composite SES measure | 37 | 0 | 1 | 0 | 0 | 0 |
| Food environment | ||||||
| Grocery store/supermarket access | 35,39,41,48 | 0 | 2 | 0 | 2 | 0 |
| Corner/convenience store access | 35,39–41,46,48 | 3 | 2 | 0 | 1 | 0 |
| Fast food access | 39,41,46,48 | 0 | 3 | 0 | 0 | 1 |
| Composite food environment | 41,48 | 0 | 1 | 0 | 1 | 0 |
| Physical activity environment | ||||||
| Walkability | 38 | 0 | 0 | 0 | 1 | 0 |
| Park/playground access | 38,46 | 0 | 1 | 1 | 0 | 0 |
| Traffic speed/volume | 38 | 0 | 1 | 0 | 0 | 0 |
| Vegetation | 41 | 0 | 0 | 1 | 0 | 0 |
| Neighborhood crime | ||||||
| Crime | — | 0 | 0 | 0 | 0 | 0 |
Studies were considered weak quality if they had two or more weak ratings on selection bias, study design, data collection methods, and analyses.
Mixed results = multiple types of associations between neighborhood exposure and outcome reported. Other = neighborhood factor was included in the final, adjusted model, but the direction of association and significance were not reported.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016;315:2292–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nobari TZ, Whaley SE, Prelip ML, et al. Trends in socioeconomic disparities in obesity prevalence among low-income children aged 2–4 years in Los Angeles County, 2003–2014. Child Obes 2018;14:248–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. US Preventive Services Task Force. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA 2017;317:2417–2426 [DOI] [PubMed] [Google Scholar]
- 5. Ward ZJ, Long MW, Resch SC, et al. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med 2017;377:2145–2153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. The National Academies Press: Washington, DC, 2012 [PubMed] [Google Scholar]
- 7. Feng J, Glass TA, Curriero FC, et al. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 2010;16:175–190 [DOI] [PubMed] [Google Scholar]
- 8. Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics 2000;105:E83–E83 [DOI] [PubMed] [Google Scholar]
- 9. Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 2006;117:417. [DOI] [PubMed] [Google Scholar]
- 10. Kumanyika SK. Environmental influences on childhood obesity: Ethnic and cultural influences in context. Physiol Behav 2008;94:61–70 [DOI] [PubMed] [Google Scholar]
- 11. Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports 2001;116:404–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Franco M, Diez Roux AV, Glass TA, et al. Neighborhood characteristics and availability of healthy foods in Baltimore. Am J Prev Med 2008;35:561–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 14. Kuo J, Voorhees CC, Haythornthwaite JA, Young DR. Associations between family support, family intimacy, and neighborhood violence and physical activity in urban adolescent girls. Am J Public Health 2007;97:101–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Romero AJ, Robinson TN, Kraemer HC, et al. Are perceived neighborhood hazards a barrier to physical activity in children? Arch Pediatr Adolesc Med 2001;155:1143–1148 [DOI] [PubMed] [Google Scholar]
- 16. Ferrão MM, Gama A, Marques VR, et al. Association between parental perceptions of residential neighbourhood environments and childhood obesity in Porto, Portugal. Eur J Public Health 2013;23:1027–1031 [DOI] [PubMed] [Google Scholar]
- 17. Zenk SN, Schulz AJ, Israel BA, et al. Food shopping behaviors and exposure to discrimination. Public Health Nutr 2014;17:1167–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: A new view of “comfort food.” Proc Natl Acad Sci U S A 2003;100:11696–11701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kumanyika SK, Swank M, Stachecki J, Brennan LK. Examining the evidence for policy and environmental strategies to prevent childhood obesity in black communities: New directions and next steps. Obes Rev 2014;15:177–203 [DOI] [PubMed] [Google Scholar]
- 20. Ferdinand AO, Sen B, Rahurkar S, et al. The relationship between built environments and physical activity: A systematic review. Am J Public Health 2012;102:7–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda. Obes Rev 2011;12:217–230 [DOI] [PubMed] [Google Scholar]
- 22. Papas MA, Alberg AJ, Ewing R, et al. The built environment and obesity. Epidemiol Rev 2007;29:129–143 [DOI] [PubMed] [Google Scholar]
- 23. Schaefer-McDaniel N. Children Talk about Their New York City Neighborhoods—The Role of Subjective and Objective Neighborhood Evaluations in Understanding Child Health. VDM Verlag Dr. Mueller e.k.: Saarbrüken, Germany [Google Scholar]
- 24. Giles-Corti B, Kelty SF, Zubrick SR, Villanueva KP. Encouraging walking for transport and physical activity in children and adolescents. Sports Med 2009;39:995–1009 [DOI] [PubMed] [Google Scholar]
- 25. Showell NN, Cole KW, Johnson K, et al. Neighborhood and parental influences on diet and physical activity behaviors in young low-income pediatric patients. Clin Pediatr 2017;56:1235–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Go AS, Mozaffarian D, Roger VL, et al. Heart Disease and Stroke Statistics—2014 Update: A Report from the American Heart Association. Circulation 2014;129:e28–e292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Endnote X8. Clarivate Analytics, 2016 [Google Scholar]
- 28. RefWorks. ProQuest, LLC: Bethesda, MD, 2013. Available at www.refworks.com Last accessed January15, 2014. [Google Scholar]
- 29. Qualtrics. Qualtrics: Provo, Utah, 2015 [Google Scholar]
- 30. Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: Relationships to overweight in low-income preschool children. Prev Med 2004;38:57–63 [DOI] [PubMed] [Google Scholar]
- 31. Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies, 1998. Available at https://merst.ca/ephpp Last accessed May25, 2018.
- 32. Bennett WL, Cheskin LJ, Wilson RF, et al. Methods for Evaluating Natural Experiments in Obesity: Systematic Evidence Review. Agency for Healthcare Research and Quality (US): Rockville, MD, 2017 [PubMed] [Google Scholar]
- 33. Bader MDM, Schwartz-Soicher O, Jack D, et al. More neighborhood retail associated with lower obesity among New York City public high school students. Health Place 2013;23:104–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Burns JJ, Goff S, Karamian G, et al. The relationship between local food sources and open space to body mass index in urban children. Public Health Rep 2011;126:890–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carroll C, Andreyeva T. Access to SNAP-authorized food stores and nutrition outcomes of SNAP-participating adolescents. J Hunger Environ Nutr 2013;8:445–457 [Google Scholar]
- 36. Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Associations of neighborhood and school socioeconomic and social contexts with body mass index among urban preadolescent students. Am J Public Health 2015;105:2496–2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cohen DA, Finch BK, Bower A, Sastry N. Collective efficacy and obesity: The potential influence of social factors on health. Soc Sci Med 2006;62:769–778 [DOI] [PubMed] [Google Scholar]
- 38. Duncan DT, Castro MC, Gortmaker SL, et al. Racial differences in the built environment—Body mass index relationship? A geospatial analysis of adolescents in urban neighborhoods. Int J Health Geogr 2012;11:11–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Galvez MP, Hong L, Choi E, et al. Childhood obesity and neighborhood food store availability in an inner city community. Acad Pediatr 2009;9:339–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jilcott SB, Wade S, McGuirt JT, et al. The association between the food environment and weight status among eastern North Carolina youth. Public Health Nutr 2011;14:1610–1617 [DOI] [PubMed] [Google Scholar]
- 41. Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: Differences by population density. Am J Health Promot 2007;21:317–325 [DOI] [PubMed] [Google Scholar]
- 42. Lovasi GS, Jacobson JS, Quinn JW, et al. Is the environment near home and school associated with physical activity and adiposity of urban preschool children? J Urban Health 2011;88:1143–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Miranda ML, Edwards SE, Anthopolos R, et al. The built environment and childhood obesity in Durham, North Carolina. Clin Pediatr 2012;51:750–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nelson MC, Gordon-Larsen P, Song Y, Popkin BM. Built and social environments. Associations with adolescent overweight and activity. Am J Prev Med 2006;31:109–117 [DOI] [PubMed] [Google Scholar]
- 45. Nobari TZ, Wang M-C, Chaparro MP, et al. Immigrant enclaves and obesity in preschool-aged children in Los Angeles County. Soc Sci Med 2013;92:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ohri-Vachaspati P, Lloyd K, DeLia D, et al. A closer examination of the relationship between children's weight status and the food and physical activity environment. Prev Med 2013;57:162–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Oreskovic NM, Kuhlthau KA, Romm D, Perrin JM. Built environment and weight disparities among children in high- and low-income towns. Acad Pediatr 2009;9:315–321 [DOI] [PubMed] [Google Scholar]
- 48. Powell LM, Auld MC, Chaloupka FJ, et al. Associations between access to food stores and adolescent body mass index. Am J Prev Med 2007;33 (4 Suppl):S301–S307 [DOI] [PubMed] [Google Scholar]
- 49. Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Soc Sci Med (1982) 2013;95:106–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kimbro RT, Denney JT. Neighborhood context and racial/ethnic differences in young children's obesity: Structural barriers to interventions. Soc Sci Med 2013;95:97–105 [DOI] [PubMed] [Google Scholar]
- 51. Bell JF, Wilson JS, Liu GC. Neighborhood greenness and 2-year changes in body mass index of children and youth. Am J Prev Med 2008;35:547–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lee H. The role of local food availability in explaining obesity risk among young school-aged children. Soc Sci Med 2012;74:1193–1203 [DOI] [PubMed] [Google Scholar]
- 53. McTigue KM, Cohen ED, Moore CG, et al. Urban neighborhood features and longitudinal weight development in girls. Am J Prev Med 2015;49:902–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rossen LM, Curriero FC, Cooley-Strickland M, Pollack KM. Food availability en route to school and anthropometric change in urban children. J Urban Health 2013;90:653–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Colabianchi N, Coulton C, Hibbert JD, et al. Adolescent self-defined neighborhoods and activity spaces: Spatial overlap and relations to physical activity and obesity. Health Place 2014;27:22–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kwan MP. The uncertain geographic context problem. Ann Assoc Am Geogr 2012;102:958–968 [Google Scholar]
- 57. Dattilo AM, Birch L, Krebs NF, et al. Need for early interventions in the prevention of pediatric overweight: A review and upcoming directions. J Obes 2012;2012:1–18 [DOI] [PMC free article] [PubMed] [Google Scholar]