Abstract
Objective
The value students give to communication skills (CS), acquiring them, or other related matters can influence the effectiveness of educational programs. In this study, we explored first and fourth year medical students’ attitudes toward CS and their learning, assessing the possible influence they have on programmed experiential training in a medical school.
Subjects and methods
Two hundred and twenty first and fourth year medical students completed the Communication Skills Attitudes Scale, analyzing the positive and negative, and affective and cognitive attitude subscales toward learning.
Results
Fourth year students trained in CS showed less positive attitudes toward CS than first year untrained students. Cognitive and affective attitudes displayed different patterns in both groups; while affective attitudes decreased in fourth year students, cognitive attitudes did not vary significantly between groups. Accumulated learning experiences seem to be more influential than sex.
Conclusion
The findings suggest that students’ attitudes toward CS could decline as a result of CS training. Nevertheless, students’ attitudes at the cognitive and fundamental level stay fairly unchanged. Learning CS with experiential methods seems to be challenging for students at a personal level; so, educators should personalize these methods as much as possible. However, further studies using longitudinal research designs should be performed for exploring students’ attitudes changes over time.
Keywords: medical education, communication skills, medical students, experiential learning, students’ attitudes
Introduction
Different reviews show that the most effective educational methods for improving communication skills (CS) in trainees are the “experientials”. These strategies teach through role playing, simulated interaction with patients, or supervised practical work. Students can then reflect on their own behavior and that of others.1–3 Generally, the educational orientation of this teaching is focused on the impact these programs have on the students’ psychomotor skills (what they do) and cognitive skills (what they know). However, they do not focus so much on the affective matters (what they feel and think), which can be described as the attitude the students have toward communication and the different teaching methods. Previous research suggests that variables such as the value students give to communication and its learning, together with associated aspects such as how it is assessed, students’ experience of different educational methods, and sociodemographic differences, can influence the effectiveness of the programs.4–8 The students’ attitudes toward CS influence, for example, on matters such as the amount of time they dedicate to learning the skills9 and how they will put them into practice when treating certain patients.10 Different studies have described how the students’ attitudes toward this area and the CS decline and further they progress with their medical studies.11–15 This decline has been described as a process in which the medical students start school with an idealistic and altruistic attitude and end up finishing as cynical and detached.16 This is not something new, so attitudes are strong behavioral indicators,17 that is, the way in which doctors communicate with their patients correlates with the importance they give to certain aspects of health care, such as patient-centred matters and the application of bio psychosocial viewpoints.18,19 Other studies show how the different factors such as age, gender, self-perception of CS, educational or ethnic background can be related to positive or negative attitudes toward communication and its learning.18,20 Another variable which seems to influence students’ attitudes toward communication is their own learning experience in this subject during their medical studies. While some authors have pointed out differences in attitude between didactic and experiential methodologies,20 preferring the latter, others21 believe the opposite and connect the increase in negative attitudes specifically to the experiences of emotional distress, which training through direct or video observation can cause to students. The same can be said of interaction with real or simulated patients (SPs) and the subsequent feedback on their performance, either individually or in small groups.22–24 The aim of this study was to explore the attitudes that first and fourth year medical students at our school have regarding the training and use of CS. We also analyzed and compared these attitudes in relation to different sociodemographic factors and after the fourth year group’s 2 years of training experience in communication, which featured both experiential and interactive characteristics.
Subjects and methods
All the first and fourth year medical students from the Francisco de Vitoria University were invited to participate in this study (120 and 110, respectively). Taking advantage of the seminars the students attended and their prior consent, the students completed anonymously the Communication Skills and Attitudes Scale (CSAS). The UFV-Health Sciences Faculty review board approved this study. All participants gave written informed consent to participate in the study.
Study design
This was a cross-sectional study.
Communication Skills and Attitudes Scale
The CSAS was developed to explore the attitudes of medical students toward learning of CS.25 This scale has been used for research in several medical schools.26–29 The items evaluate the students’ perceptions of the way CS are taught, the importance of good CS to pass exams and be a good doctor, and the use of CS to show respect to patients. The positive and negative items are ordered randomly. Using the original version in English, together with a Catalan version, which was validated for a similar cultural context to ours,30 we used a back translation method and a pilot study with ten students to create a Spanish version of the CSAS. The initial psychometric analysis by Rees et al25 identified two subscales or factors, each with 13 items and representing positive and negative attitudes toward CS learning. In this previous study with 490 students, both subscales showed a satisfactory reliability and internal consistency. In a subsequent study performed on 1,833 students in the four Norwegian faculties of medicine, Anvik et al28 identified three factors in the CSAS different from those previously described: factor 1, labeled as “Learning”, suggests that this factor will mainly measure students’ feelings about how CS are taught, and it would mainly be reflected in the affective aspects of the attitudes; factor 2, known as “Importance”, would encompass the attitudes of students toward CS, mainly reflecting basic cognitive attitudes and values; and finally, factor 3, labeled as “Respect”, because all the items establish that CS are useful to the student when it comes to respecting patients. The analysis of our data considers both the Rees and Anvik factors: Positive, Negative, Affective, Cognitive, and Respect Attitudes. Age, gender, whether students’ fathers were doctors, the mark they received in final CS structured clinical exam (fourth), the mark obtained in the university entrance exams (first), and how they regarded their own CS (on 1–5 Likert scale) were the other variables included.
Structure and teaching activities in communication training at UFV University
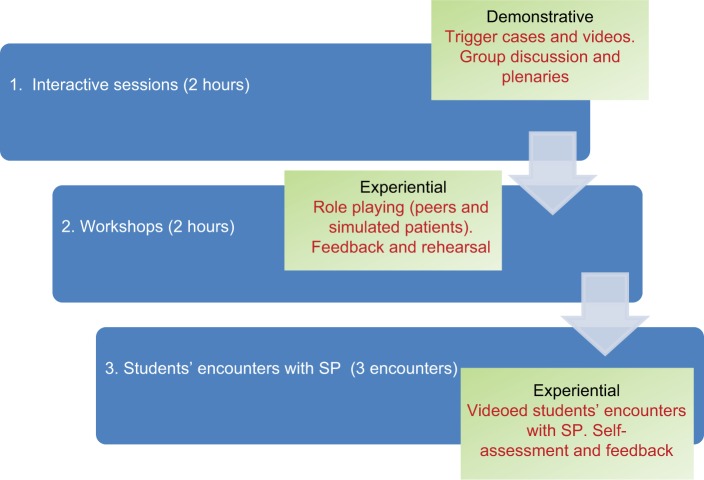
Patient–physician communication training is a requisite training for third and fourth year medical students at the UFV Faculty of Medicine. For 6 weeks each year, students work in-depth with patients in consultations in hospital and primary care. In the third year, they receive basic training focused on CS for performing “person-centered interviews”. The fourth year is devoted to more specific and advanced CS. The overall training program has four modules. The objective of the first module is to train students in the use of CS to obtain relevant clinical information and to establish a suitable doctor–patient relationship. The objectives of the second module focus on providing information and sharing in the decision-making process. The aims of third module deal with emotions in consultation and giving bad news. The final module introduces students to communicative strategies to influence patients’ behavior, mainly by motivational means. The first two modules are imparted during the third year and the final two in the fourth year.31 All the course modules involve the following activities:
Demonstrative and small group work sessions and three sessions addressing the specific interview topics and CS. Students work in small groups on situations depicted in videos and clinical cases. These sessions involve individual reflection and plenaries with a discussion and presentation of evidence and analysis of the strategies proposed.
Workshops with SPs: Some students interview an SP, while the rest observe and evaluate the interaction in terms of objectives achieved and skills used. After each encounter, the student receives feedback from peers, SP, and the teaching staff (faculty).
Group practice and reports: Additional groups of four students are organized to interview, observe, and provide feedback to each other. In these encounters, the students perform role-play situations. Points of interest are collected in a notebook for each student with information about the development of their skills and the experience in general.
Interviews with SP: All students hold two or three videotaped encounters with SPs in every module. This is performed in the simulation center equipped with a built-in video recording system that allows videos to be viewed online for assessment. After each interview, all students complete a quantitative self-assessment form (1 Deficient, 5 Excellent) of their interview skills and have the chance to make a few comments. Subsequently, each student receives individualized feedback from the teaching staff using the same qualitative–quantitative methodology.
Figure 1 shows the general teaching program for all modules.
Figure 1.
General teaching communication skills program characteristics for all modules.
Abbreviation: SP, simulated patient.
Data analyses
The data were analyzed with the 10Æ0 version of SPSS. First, an analysis of the exploratory data was performed to establish the distribution of the continuous variables. The student means were compared using Student’s t-test and the Pearson correlation coefficients. Finally, to assess possible associations between different variables and the CSAS global and affective dimensions score, a multivariate analysis was performed (linear regression).
Ethics approval and informed consent
The UFV Health Sciences Faculty Review Board approved this study, which was carried out in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Results
A total of 220 students answered the questionnaire (first year: 114 and fourth year: 106; 95.6%). The average age of the first and fourth year students was 18.7 and 23.4 years, respectively. Most of the students, both in the first and fourth year, were female (76 [74.5%]); 30 (38%) had a mother or father who was a doctor and 74 (73%) had completed their sixth-form studies (baccalaureate) at private schools (mostly religious schools). The self-assessment of CS was 10 points better in fourth-year students than in first-year ones (66% compared to 56%).
The students’ self-assessment of their own CS had a positive correlation with a general positive attitude (0.211, P=0.004) and in the affective (0.260, P=0.00) and respect (0.152, P=0.03) areas and a negative correlation with a negative attitude (0.260, P=0.001). The mark obtained in the practical CS exam only had a negative correlation with a negative attitude (−0.212, P=0.03). No other significant correlations were found.
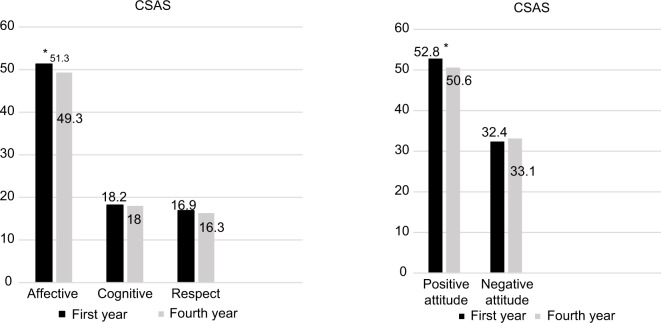
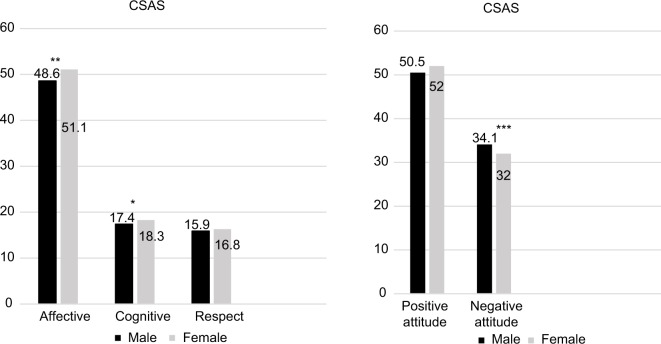
Figures 2 and 3 show the results of the CSAS in the global attitude and in its three dimensions (affective, cognitive, and respect) of first and fourth year students of both sexes. In both multivariate linear regression models that took the global positive attitude score in the CSAS and the positive score of the affective domain as a dependent variable, significant positive associations were found with the self-perception of CS in the students (β=2.363, P=0.003 and β=2.663, P=0.000) and negative associations were found with the upper course (fourth year) (value β=−0.771, P=0.025 and β=−0.602; P=0.04), but no associations were found with sex.
Figure 2.
Scores of first and fourth year medical students in the different subscales of the CSAS.
Note: *P=0.02.
Abbreviation: CSAS, Communication Skills and Attitudes Scale
Figure 3.
Scores of male and female medical students in the different subscales of the CSAS.
Notes: *P=0.042; **P=0.018; ***P=0.016.
Abbreviation: CSAS, Communication Skills and Attitudes Scale
Discussion
Fourth year medical students trained in CS showed lower attitudinal levels toward CS training than those of untrained first year students. Along with this slight but significant decrease in positive attitudes, trends of a more negative attitude toward CS learning in these trained students were also observed. As with our study, others have also shown a decline in the attitudes among medical students.11,13,14,20,32 In a more recent study performed by two cohorts of medical students differentiated only by having received CS training or not, which used the CSAS, the attitudes toward the teaching of CS during internship and the attitudes focused on the patient worsened in students trained in CS.29
Analyzing these results with the CSAS subscales proposed by Anvik et al, our findings are also concordant with those obtained by these authors21 as they indicate that the decline in attitudes among medical students mainly involves a decline in their affective attitude. This would be reflected in their feelings and experiences on the way in which these CS have been taught in the faculty and not so much on the importance that the students give to CS in their studies and clinical practice. According to the studies, experiential training is pivotal for success in teaching and learning CS.1–3 However, our study and those by Bombeke29 and, in particular, by Anvik21 move toward the hypothesis that this type of teaching may be producing significant changes in the attitudes of students toward the type of teaching received and not so much on the importance they give to these CS. After analyzing these results, we carried out a qualitative study for clarifying our own students’ points of view and experiences regarding the training they received during previous years in CS.31 This study revealed various associated topics. Although most students considered that communication topics were useful and practical, they confessed to having problems performing in small groups, interviewing an SP in front of peers, mainly due to difficulties in putting theory into practice and also the potential feelings of embarrassment. The summative assessment of these CS also brought about a wide range of negative feelings, with it being identified as the main source of stress. It seems that this way of learning CS often makes students feel uncomfortable and anxious (Ruiz Moral et al, unpublished data, 2018)24 and helps them to develop negative affective attitudes. In this same study, our students pointed out that receiving detailed and constructive feedback for learning new skills, performed in a careful and thoughtful way, was a very gratifying and productive experience. However, although this may mitigate the stress experienced,24,33 it does not seem sufficient to make the feeling of discomfort and embarrassment disappear. Nor does it address the distress of doing the first interviews, the obligatory nature of this learning, or performing a summative assessment34 based on the interviews with SPs. Finally, compared with males, females seem to have positive attitudes toward CS; however, in our study, the training program made these differences between sexes disappear. This highlights the possible influence of factors not only related to the implementation problems of experiential methodologies pointed out, but also to others (workload or study, work stress, contact with real scenarios with patients, etc).
Limitations
Because this is a cross-sectional and not a longitudinal or experimental study, the comparisons between year classes should be treated with caution, something which applies to most of the earlier studies as well. Possible confusing factors concerning generalization of these study findings are the number of students within a single university and the fact that the fourth year students group was the first cohort trained on the new communication course. There are also obvious elements of uncertainty as regards the validity of the CSAS and the use of statistical procedures. The CSAS was not designed for the purpose of differentiating between cognitive and affective attitudes. Nevertheless, the fact that other authors applied it to a large sample of students with very congruent results to ours21 supports the validity of distinguishing both subscales for analysis. We have also pointed out the existence of other variables not contemplated in this study that can influence this decrease in positive and affective attitudes and that may be related to the assumption by students of new responsibilities, or be similar to those related to the decrease in students’ empathy highlighted by other authors.13,35–37
Conclusion
The findings suggest the hypothesis that students’ attitudes toward CS could decline as a result of CS training. Nevertheless, students’ attitudes on a cognitive and fundamental level remain mostly unchanged. The accumulated learning experiences during this learning process seem to be more influential in attitudes than sex. Learning CS with experiential methods seems to be challenging for students at a personal level, and this should be kept in mind by educators when designing them, emphasizing personalization as much as possible. However, further longitudinal studies are needed to confirm these results.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Berkhof M, van Rijssen HJ, Schellart AJ, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: an overview of systematic reviews. Patient Educ Couns. 2011;84(2):152–162. doi: 10.1016/j.pec.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Henry SG, Holmboe ES, Frankel RM. Evidence-based competencies for improving communication skills in graduate medical education: a review with suggestions for implementation. Med Teach. 2013;35(5):395–403. doi: 10.3109/0142159X.2013.769677. [DOI] [PubMed] [Google Scholar]
- 3.Smith S, Hanson JL, Tewksbury LR, et al. Teaching patient communication skills to medical students: a review of randomized controlled trials. Eval Health Prof. 2007;30(1):3–21. doi: 10.1177/0163278706297333. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman DM, Laidlaw TA, Macleod H. Communication skills in medical school exposure, confidence, and performance. Acad Med. 2000;75(10 Suppl):S90–92. doi: 10.1097/00001888-200010001-00029. [DOI] [PubMed] [Google Scholar]
- 5.Langille DB, Kaufman DM, Laidlaw TA, Sargeant J, Macleod H. Faculty attitudes towards medical communication and their perceptions of students’ communication skills training at Dalhousie university. Med Educ. 2001;35(6):548–554. doi: 10.1046/j.1365-2923.2001.00921.x. [DOI] [PubMed] [Google Scholar]
- 6.Howley LD, Wilson WG. Direct observation of students during clerkship rotations: a multiyear descriptive study. Acad Med. 2004;79(3):276–280. doi: 10.1097/00001888-200403000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Humphris GM, Kaney S. Assessing the development of communication skills in undergraduate medical students. Med Educ. 2001;35(3):225–231. doi: 10.1046/j.1365-2923.2001.00869.x. [DOI] [PubMed] [Google Scholar]
- 8.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 9.Dornan T, David T. Adult learning and continuing education. Diabet Med. 2000;17(1):78–86. doi: 10.1046/j.1464-5491.2000.00216-3.x. [DOI] [PubMed] [Google Scholar]
- 10.Newble DI. Editorial II: assessment of clinical competence. Br J Anaesth. 2000;84(4):432–433. doi: 10.1093/oxfordjournals.bja.a013464. [DOI] [PubMed] [Google Scholar]
- 11.Pfeiffer C, Madray H, Ardolino A, Willms J. The rise and fall of students’ skill in obtaining a medical history. Med. Educ. 1998;32(3):283–288. doi: 10.1046/j.1365-2923.1998.00222.x. [DOI] [PubMed] [Google Scholar]
- 12.Rosenthal F, Ogden F. Changes in medical education: the beliefs of medical students. Med. Educ. 1998;32(2):127–132. doi: 10.1046/j.1365-2923.1998.00163.x. [DOI] [PubMed] [Google Scholar]
- 13.Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934–941. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 14.Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: a cohort study. Med Educ. 2004;38(5):522–534. doi: 10.1046/j.1365-2929.2004.01820.x. [DOI] [PubMed] [Google Scholar]
- 15.Tsimtsiou Z, Kerasidou O, Efstathiou N, Papaharitou S, Hatzimouratidis K, Hatzichristou D. Medical students’ attitudes toward patient-centred care: a longitudinal survey. Med Educ. 2007;41(2):146–153. doi: 10.1111/j.1365-2929.2006.02668.x. [DOI] [PubMed] [Google Scholar]
- 16.Spencer J. Decline in empathy in medical education: how can we stop the rot? Med Educ. 2004;38(9):916–918. doi: 10.1111/j.1365-2929.2004.01965.x. [DOI] [PubMed] [Google Scholar]
- 17.Petty RE, Wegener DT, Fabrigar LR. Attitudes and attitude change. Annu Rev Psychol. 1997;48:609–647. doi: 10.1146/annurev.psych.48.1.609. [DOI] [PubMed] [Google Scholar]
- 18.Levinson W, Roter D. Physicians’ psychosocial beliefs correlate with their patient communication skills. J Gen Intern Med. 1995;10(7):375–379. doi: 10.1007/BF02599834. [DOI] [PubMed] [Google Scholar]
- 19.Haidet P, Dains JE, Paterniti DA, Chang T, Tseng E, Rogers JC. Medical students’ attitudes toward patient-centered care and standardized patients’ perceptions of humanism: a link between attitudes and outcomes. Acad Med. 2001;76(10 Suppl):S42–S44. doi: 10.1097/00001888-200110001-00015. [DOI] [PubMed] [Google Scholar]
- 20.Rees C, Sheard C. The relationship between medical students’ attitudes towards communication skills learning and their demographic and education-related characteristics. Med Educ. 2002;36(11):1017–1027. doi: 10.1046/j.1365-2923.2002.01333.x. [DOI] [PubMed] [Google Scholar]
- 21.Anvik T, Grimstad H, Baerheim A, et al. Medical students’ cognitive and affective attitudes towards learning and using communication skills – a nationwide cross-sectional study. Med Teach. 2008;30(3):272–279. doi: 10.1080/01421590701784356. [DOI] [PubMed] [Google Scholar]
- 22.Beckman HB, Frankel RM. The use of videotape in internal medicine training. J Gen Intern Med. 1994;9(9):517–521. doi: 10.1007/BF02599224. [DOI] [PubMed] [Google Scholar]
- 23.Hargie O, Dickson D, Boohan M, Hughes K. A survey of communication skills training in UK schools of medicine: present practices and prospective proposals. Med Educ. 1998;32(1):25–34. doi: 10.1046/j.1365-2923.1998.00154.x. [DOI] [PubMed] [Google Scholar]
- 24.Nilsen S, Baerheim A. Feedback on video recorded consultations in medical teaching: why students loathe and love it – a focus-group based qualitative study. BMC Med Educ. 2005;5(1):28. doi: 10.1186/1472-6920-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rees C, Sheard C, Davies S. The development of a scale to measure medical students’ attitudes towards communication skills learning: the Communication Skills Attitude Scale (CSAS) Med Educ. 2002;36(2):141–147. doi: 10.1046/j.1365-2923.2002.01072.x. [DOI] [PubMed] [Google Scholar]
- 26.Rees C, Sheard C. Evaluating first-year medical students’ attitudes to learning communication skills before and after a communication skills course. Med Teach. 2003;25(3):302–307. doi: 10.1080/0142159031000100409. [DOI] [PubMed] [Google Scholar]
- 27.Cleland J, Foster K, Moffat M. Undergraduate students’ attitudes to communication skills learning differ depending on year of study and gender. Med Teach. 2005;27(3):246–251. doi: 10.1080/01421590400029541. [DOI] [PubMed] [Google Scholar]
- 28.Anvik T, Gude T, Grimstad H, et al. Assessing medical students’ attitudes towards learning communication skills – which components of attitudes do we measure? BMC Med Educ. 2007;7:4. doi: 10.1186/1472-6920-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bombeke K, van Roosbroeck S, De Winter B, et al. Medical students trained in communication skills show a decline in patient-centred attitudes: an observational study comparing two cohorts during clinical clerkships. Patient Educ Couns. 2011;84(3):310–318. doi: 10.1016/j.pec.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Molinuevo B, Torrubia R. Validation of the Catalan version of the Communication Skills Attitude Scale (CSAS) in a cohort of south European medical and nursing students. Educ Health (Abingdon) 2011;24(1):499–505. [PubMed] [Google Scholar]
- 31.Ruiz moral R, Caballero Martínez F, Garcia de Leonardo C, Monge D, Cañas F, Castaño P. Teaching and learning clinical communication skills in Francisco de Vitoria medical school (Madrid) Educ Med. 2017;18(4):289–297. [Google Scholar]
- 32.Haidet P, Dains JE, Paterniti DA, et al. Medical student attitudes toward the doctor–patient relationship. Med Educ. 2002;36(6):568–574. doi: 10.1046/j.1365-2923.2002.01233.x. [DOI] [PubMed] [Google Scholar]
- 33.Moulaert V, Verwijnen MG, Rikers R, Scherpbier AJ. The effects of deliberate practice in undergraduate medical education. Med Educ. 2004;38(10):1044–1052. doi: 10.1111/j.1365-2929.2004.01954.x. [DOI] [PubMed] [Google Scholar]
- 34.Boehler ML, Rogers DA, Schwind CJ, et al. An investigation of medical student reactions to feedback: a randomised controlled trial. Med Educ. 2006;40(8):746–749. doi: 10.1111/j.1365-2929.2006.02503.x. [DOI] [PubMed] [Google Scholar]
- 35.Rees C, Sheard C, McPherson A. Communication skills assessment: the perceptions of medical students at the University of Nottingham. Med Educ. 2002;36(9):868–878. doi: 10.1046/j.1365-2923.2002.01300.x. [DOI] [PubMed] [Google Scholar]
- 36.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 37.Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]