Abstract
Objectives
Chronic otitis media with effusion (COME) in children can cause prolonged hearing loss, which is associated with an increased risk of learning delays and behavioural problems. Dispersal of bacterial pathogens from the nasal passages to the middle ear is implicated in COME. We sought to determine whether there is an association between nasal microbial composition and COME in children.
Methods
A case-control study of children aged 3 and 4 years was conducted. Cases undergoing placement of tympanostomy tubes for COME were compared to healthy controls. Nasal swabs were collected and a questionnaire was administered. The V1-3 region of the 16S rRNA gene was amplified, and sequenced on the Illumina MiSeq.
Results
73 children with COME had a lower Shannon diversity index than 105 healthy controls (1.62 [.80] versus 1.88 [.84], respectively; P = .046). The nasal microbiota of cases and controls differed in composition using Bray-Curtis dissimilarity (p = 0.002). Children with COME had a higher abundance of otopathogens and lower abundance of commensals including alpha haemolytic Streptococci and Lactococcus. Cluster analysis revealed 4 distinct nasal microbial profiles. Profiles that were Corynebacterium-dominated (aOR 4.18 [95%CI, 1.68–10.39], Streptococcus-dominated (aOR 3.12 [95%CI, 1.08–9.06], or Moraxella-dominated (aOR 4.70 [95%CI, 1.73–12.80] were associated with COME, compared to a more mixed microbial profile when controlling for age, ethnicity, and recent antibiotics use.
Conclusions
Children with COME have a less diverse nasal microbial composition with a higher abundance of pathogens, compared to healthy children who have a more mixed bacterial profile with a higher abundance of commensals. Further research is required to determine how nasal microbiota may relate to the pathogenesis or maintenance of COME, and whether modification of the nasal microbiota can prevent or treat children at risk of COME.
Introduction
Chronic otitis media with effusion (COME) is diagnosed when fluid gathers behind the tympanic membrane for three months or longer [1]. The hearing loss associated with COME may impact language acquisition, and increase the risk of learning delays and behavioural problems [2].
COME has historically been regarded as a sterile inflammatory condition, as pathogens were seldom cultured from effusion in the middle ear (ME). However, with the advent of culture-independent methods, otopathogens have been found in COME as often as in the closely-related condition acute otitis media (AOM) [3, 4]. This discrepancy in findings may be explained by bacteria that are less likely to be detected by culture because they are residing in a biofilm state [5]. The key otopathogens are non-typeable Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis, and to a lesser extent Staphylococcus aureus [3].
While pathogenic bacterial biofilms residing in the ME may be involved in the maintenance of chronic effusion [6], it is unknown whether the nasal microbiota are also involved. The composition of both commensals and potential pathogens in the nasal microbiota may affect the risk of pathogens spreading to the ME. Commensal bacteria provide resistance against pathogen overgrowth by competing for nutrients and epithelial cell binding sites, producing antimicrobials, disrupting bacterial biofilms, and inducing the host’s immune system [7, 8].
Low bacterial diversity in a niche is often a marker of disease [9] and is associated with AOM [10]. Higher abundances of Haemophilus, Moraxella, and Neisseria in the nose have also been found to be associated with AOM [11]. Conversely, lower abundances of Staphylococcus, Corynebacterium, Propionibacterium, Streptococcus (usually not S. pneumoniae) and Lactococcus have been found in children with AOM [10, 11].
There are no published data on associations between nasal microbiota compositions and COME using cluster analysis. Nasal microbiota compositions characterized by Moraxella, Streptococcus, or Haemophilus have been reported to be associated with upper respiratory infection (URI) [12] asthma [13], AOM [12], pneumonia, or bronchiolitis [14, 15]. Protective compositions may also be emerging, with those dominated by Staphylococcus, Sphingobium, Corynebacterium, or Dolosigranulum associated with reduced risk of AOM [12] and asthma [16].
We investigated whether nasal microbial composition is associated with COME. Commensal bacteria in the nasal passages may protect against otopathogen overgrowth, or ongoing otopathogen overgrowth in the nasal passages may maintain persistence of effusion in the ME. We hypothesized that COME would be associated with a less diverse nasal microbiome; higher relative abundance of the otopathogens H. influenzae, S. pneumoniae, and M. catarrhalis; and lower relative abundance of the commensals S. epidermidis, Corynebacterium, Propionibacterium, Dolosigranulum, Lactococcus, Lactobacillus, and the alpha haemolytic Streptococci (AHS) spp.
Methods
Study design and setting
As previously reported, a case-control study of children aged 3 and 4 years was conducted in Auckland, New Zealand, to compare children with COME to healthy children [17]. Briefly, recruitment and data collection were conducted between May 2012 and November 2013. Cases were referred for tympanostomy tube placement (TTP), and had a recent medical history of COME and/or signs of COME confirmed by an otorhinolaryngologist during surgery. Controls were selected at random from children enrolled in primary care practices that had referred children for TTP in the previous year. Controls had no medical history of TTP, no episodes of otitis media with effusion (OME) lasting longer than one month in the past year, and never had OME lasting longer than three months. Cases and controls were excluded if they had craniofacial abnormalities or immunodeficiency.
Ethics
The parent or legal guardian was informed about the study and provided written consent. The study was approved by the Northern X Regional Ethics Committee (reference NTX/11/EXP/027)
Specimen collection
A sterile paediatric FLOQ swab (Copan, California, USA) moistened with sterile saline was inserted into subjects’ anterior nares. The swab was rotated in each nostril three times and placed into a 2ml tube of sterile STGG medium (skim milk, oxoid tryptone soya broth, glucose, and glycerol). Samples were stored at -80°C.
DNA extraction, PCR, library preparation, sequencing, and bioinformatics
DNA was extracted from nasal samples and negative controls using the Qiagen Allprep kit (Qiagen, California, USA). We had 3 negative controls consisting of STGG broth and a swab exposed to the air, STGG broth only, and reagents only. The 16S ribosomal gene was PCR amplified using primers 27F and 534R to target the V1-3 region. Sequencing libraries were generated using the Nextera XT Index kit (Illumina Inc., San Diego. CA, USA) and amplicons sequenced on the Illumina MiSeq. USEARCH 64 (version 7) analysis pipeline was used. For operational taxonomic unit (OTU) assignment the UPARSE algorithm [18] was followed using a de novo picking approach with OTUs assignment clustered at 97% sequence similarity. Full details of the sample preparation, sequencing and nasal microbiota analysis are provided in Appendix A in S1 File.
Statistical analysis was carried out in R version 3.3.3 (www.r-project.org/) using the Phyloseq [19], vegan [20], DESeq2 [21], and cluster packages [22].
Downstream analysis
OTUs were filtered to remove contaminants (see Appendix A in S1 File). OTUs with a total read number less than .005% of total reads and samples containing less than 1000 reads were removed. Additional species-level identification was achieved by aligning representative sequences using the Basic Local Alignment Search Tool (BLAST). Due to the limitations of classification using the 16S rRNA gene, these species identifications are not definitive.
Subject characteristics
Statistical analysis was conducted using JMP 13, SAS Institute Inc., Cary, NC, 1989–2016. Categorical variables were analyzed using a chi-squared test and continuous variables were analyzed using a Student t-test. A P < .05 was considered statistically significant.
Diversity analysis
Alpha diversity was calculated with absolute numbers using the Shannon diversity index in the R vegan package. Beta diversity was assessed with the Bray-Curtis dissimilarity measure. Permutation multivariate analysis of variance (PERMANOVA) using distance matrices was used to assess differences and significance was tested using ADONIS.
Differential abundance
DESeq2 package from R was used for differential abundance analysis with Benjamini-Hochberg adjustment to control for multiple testing. We adjusted for age, ethnicity and antibiotic usage in the past month. A two-tailed P < .05 was considered statistically significant.
OTU presence
For OTUs that were differentially abundant, presence of any reads was compared between cases and controls in JMP 13 using a Chi-square test with Benjamini-Hochberg adjustment, and a two-tailed P < .05 test for statistical significance.
Cluster profiling
OTUs were collapsed at the genus level. To assess nasal microbiota profiles, we partitioned using a medoid clustering approach (PAM) and the Bray-Curtis dissimilarity metric. Number of clusters was selected using the gap statistic [23]. Using JMP 13, cluster was entered into a multivariable logistic regression model along with age, ethnicity, and antibiotics in the last month, which were identified as potential confounding variables. A two-tailed P < .05 test was considered statistically significant.
Results
Study population
Of 190 subjects who provided nasal samples, 12 were excluded due to having fewer than 1000 reads in total. The subjects whose samples were included did not differ from those whose samples were excluded, in terms of the subject characteristics listed in S1 Table.
As shown in Table 1, the mean age of the cases was younger than controls, there were more children of Asian ethnicity in the control group than in the case group, and the cases were younger than the controls when they were first given antibiotics. There was no difference between cases and controls for sex, season seen, method of delivery, being fully vaccinated, antibiotic exposure in the last month, attendance at daycare, or having older siblings.
Table 1. Characteristics of 178 children with chronic otitis media with effusion and healthy controls.
| Variable | Cases n (%) n = 73 |
Controls n (%) n = 105 |
P value |
|---|---|---|---|
| Mean age in months [SD] | 47.5 [6.7] | 49.6 [6.8] | .05 |
| Sex | .68 | ||
| Female | 29 (39.7) | 45 (42.9) | |
| Male | 44 (60.3) | 60 (57.1) | |
| Ethnicity | .004 | ||
| European & Other | 45 (61.6) | 51 (48.6) | |
| Asian | 3 (4.1) | 20 (19.1) | |
| Maori | 14 (19.2) | 19 (18.1) | |
| Pacific Island | 11 (15.1) | 15 (14.3) | |
| Season of sampling | .72 | ||
| Summer (December-February) | 12 (16.4) | 14 (13.3) | |
| Autumn (March–May) | 11 (15.1) | 18 (17.1) | |
| Winter (June-August) | 23 (31.5) | 40 (38.1) | |
| Spring (September-November) | 27 (37.0) | 33 (31.4) | |
| Method of delivery at birth | .19 | ||
| Normal vaginal delivery | 41 (56.2) | 58 (55.2) | |
| C-section–elective | 6 (8.2) | 17 (16.2) | |
| C-section–emergency | 20 (27.4) | 18 (17.1) | |
| Assisted vaginal delivery (forceps or ventouse) | 6 (8.2) | 12 (11.4) | |
| Fully vaccinated | .11 | ||
| No | 5 (6.9) | 15 (14.4) | |
| Yes | 68 (93.2) | 89 (85.6) | |
| Mean age of first antibiotic (months) [SD] | 10.9 [8.4] | 18.8 [10.7] | < .001 |
| Antibiotics in last month | .10 | ||
| No | 55 (75.3) | 88 (87.1) | |
| Yes | 11 (15.1) | 6 (5.9) | |
| Unknown | 7 (9.6) | 7 (6.9) | |
| Mean daycare hours per week [SD] | 24.2 [11.4] | 21.2 [10.9] | .08 |
| Older siblings | .65 | ||
| No | 31 (42.5) | 41 (39.1) | |
| Yes | 42 (57.5) | 64 (61.0) |
Microbiota analysis
A total of 3,606,750 sequences were assembled from pair-end reads across all samples. After filtering and chimera removal, 3,428,213 sequences were assembled into 300 OTUs. The median number of sequences per sample was 21,255 in cases (range 1,011–80,297) and 9,562 in controls (range 1,100–82,013).
OTU9 was classified in Greengenes as Alloiococcus, however the representative sequence matched Dolosigranulum pigrum in BLAST. This is a known misclassification in the Greengenes database. The representative sequence for OTU1 matched Corynebacterium pseudodiptheriticum using BLAST. OTU1 made up 97% of all reads of genus Corynebacterium.
Core microbiome
The core nasal microbiome, defined as those OTUs present in over 80% of all samples, consisted of 16 taxa including Corynebacterium, Moraxella, Streptococcus, unknown Bacilli (Staphylococcus), Alloiococcus/Dolosigranulum pigrum, and Neisseria; see S2 Table.
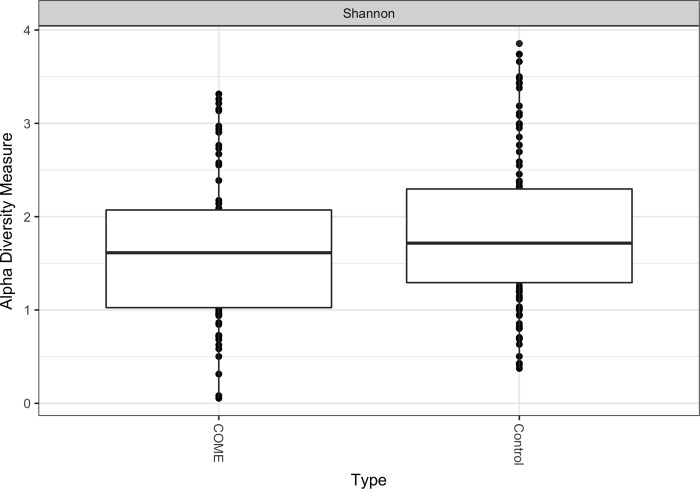
Diversity
Shannon diversity index was lower in children with COME than in healthy controls (mean = 1.62 [.80] versus mean = 1.88 [.84] respectively; P = .046); see Fig 1. Shannon diversity index was also measured using only subjects with the most frequently observed ethnicity (European) due to the strong inverse correlation between COME and Asian ethnicity. In this sensitivity analysis Shannon diversity was also lower in children with COME than in the healthy controls; see Appendix B in S1 File. We also found a significant difference in the microbial composition of children with COME and healthy controls (Bray-Curtis dissimilarity, unadjusted R2 = 0.02, P < .002); see S1 Fig.
Fig 1. Shannon diversity index of the nasal microbiota of 73 children with chronic otitis media with effusion and 105 healthy controls.
Diversity calculated using absolute abundance. Controls have higher alpha diversity than cases (P < .046).
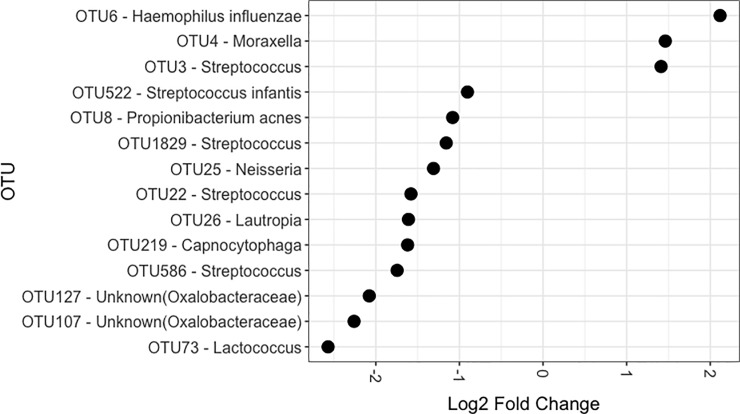
Differential abundance
OTUs that were more common in children with COME were OTU3 (Streptococcus), OTU4 (Moraxella), and OTU6 (H. influenzae) (Fig 2). Examining their representative sequences on BLAST, OTU3 matched S. pneumoniae (but also S. mitis at 99%), and OTU4 matched M. catarrhalis (but also M. caprae at 99%).
Fig 2. Differential abundance of the nasal microbiota.
Calculated using R package DESeq2. Log2 fold change from 105 healthy controls to 73 children with chronic otitis media with effusion, controlling for age, ethnicity and recent antibiotic usage.
All three OTUs that had greater abundance in the cases were also found to be present in a majority of the control samples (see S3 Table). OTU6 (H. influenzae) was found in 68% of the cases and 52% of the controls, OTU3 (Streptococcus) was found in 99% of the cases and 100% of the controls and OTU4 (Moraxella) was found in 92% of the cases and 85% of the controls. No significant differences were observed between detection of these OTUs in cases compared to controls.
Taxa more common in the healthy controls were three Streptococcus OTUs of uncertain species, Streptococcus infantis, Propionibacterium acnes, Lactococcus sp., Neisseria sp., Lautropa sp., Capnocytophaga sp., and two Oxalobacteraceae OTUs.
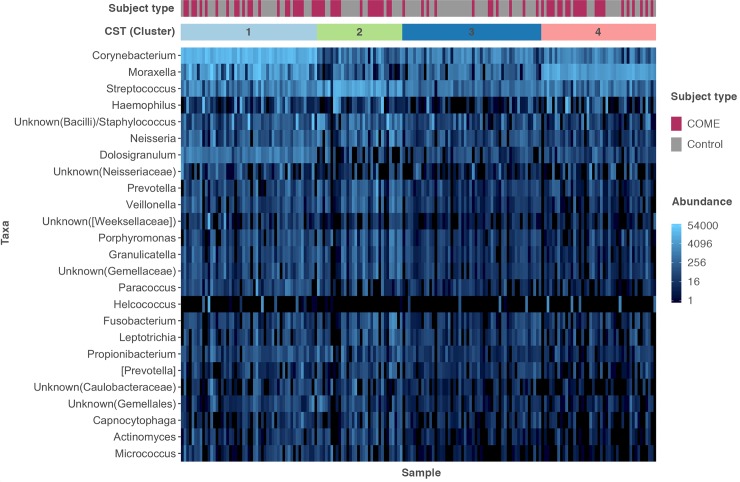
Cluster profiles
Nasal microbiota clustered into 4 distinct profiles consisting of a Corynebacterium-dominated cluster (40% of case subjects were in this cluster, and 27% of control subjects), Streptococcus-dominated cluster (cases: 19%, controls: 15%), Moraxella-dominated cluster (cases: 27%, controls: 19%), and a mixed profile cluster (cases: 14%, controls: 39%); see Fig 3. Cluster was not associated with age, ethnicity, or antibiotics in the last month in univariable analyses. In an unadjusted analysis, Corynebacterium-dominated (OR 4.25 [95%CI, 1.84–10.47]), Streptococcus-dominated (OR 3.59 [95%CI, 1.34–9.98]), and Moraxella-dominated (OR 4.10 [95%CI, 1.64–10.72]) profiles were associated with COME, compared to the more mixed microbial profile. When controlling for potential confounders (age, ethnicity, and antibiotics in the last month), the Corynebacterium-dominated (aOR 4.18 [95%CI, 1.68–10.39], Streptococcus-dominated (aOR 3.12 [95%CI, 1.08–9.06]), and Moraxella-dominated (aOR 4.70 [95%CI, 1.73–12.80]) profiles remained associated with COME compared to the mixed profile.
Fig 3. Cluster/Community structure type (CST) of the nasal microbiota of 73 children with chronic otitis media with effusion and 105 healthy controls.
Profiles were partitioned using a medoid clustering approach (PAM) and the Bray-Curtis dissimilarity metric, based on absolute abundance. Four cluster profiles are indicated: Corynebacterium-dominated profile with prominent Moraxella and Streptococcus (1), Streptococcus-dominated profile (2), mixed profile (3), and Moraxella-dominated profile (4). A heatmap of the 25 most abundant genera is displayed adjacent.
Discussion
Our findings that the nasal microbiota of children with COME had lower diversity, higher relative abundance of otopathogens, and a lower relative abundance of commensal bacteria–compared with healthy controls–indicates that the nasal microbiota may be important in initiating or maintaining COME.
Nasal and nasopharyngeal diversity have not previously been examined in OME or COME. Two studies have found low diversity to be associated with AOM [10, 24], two have found no association [11, 12], and one found that children with AOM had higher diversity [25]. The association observed between COME and low nasal diversity may reflect well-balanced microbiota exhibiting a higher resilience to infection, however the causal direction of such relationships has not been fully established [9]. It could equally signify that a bacterial infection that led to COME has also caused an overgrowth of pathogenic bacteria in the nose, which would result in lower alpha diversity by reducing the evenness of bacterial abundance.
A high load of pathogenic bacteria in the nasal passages may increase the risk of movement of those bacteria up the ET to the ME. S. pneumoniae, non-typeable H. influenzae and M. catarrhalis are the three main bacterial pathogens that have been identified in relation to COME [26], and are commonly detected in the ME effusion of children with COME [3]. Specific strains of these otopathogens are shared between the nasopharynx and the ME in individuals [27]. In some animal models, injection of bacteria into the nose results in ME carriage of those bacteria. [28] Polymicrobial infection further increases the risk of spread to the ME, as shown by nasal challenges using co-infection with multiple bacteria or respiratory viruses [29, 30].
We found that children with COME had higher nasal levels of H. influenzae, a Streptococcus OTU matching S. pneumoniae (and S. mitis), and a Moraxella OTU resembling M. catarrhalis (and M. caprae). Haemophilus has been found to be differentially abundant in children with recurrent AOM [25]. This correlation may reflect overgrowth of these pathogens initiating or maintaining COME by spreading to the ME. Although these three OTUs had higher differential abundance in the cases than the controls, they were all present in more than half of the controls. These OTUs may therefore be endogenous pathobionts, common microorganisms of children’s noses that may be disrupted and become infectious due to stimuli such URI [9]. URI often precedes OM, and can disrupt the airway microbiota. Viruses may promote adherence and virulence of otopathogens [31] by disrupting the airway epithelial barrier [32], decreasing mucociliary clearance [33], inducing the host to supply nutrients to pathogenic bacteria [34], and provoking biofilms to release virulent dispersed bacteria [35].
We also found that certain commensal bacteria were more common in controls. These included several AHS spp., a Lactococcus sp., and Propionibacterium acnes. AHS have been reported to help prevent otopathogen infection and OM [36]. Nasal Lactococcus also has higher relative abundance in healthy children than in children with AOM [11]. Propionibacteria appear to be protective against S. pneumoniae colonization, URI, and OM, and nasal levels are inversely associated with levels of S. pneumoniae and S. aureus [11, 37, 38].
We report the first cluster analysis of nasal bacterial profile in any OM-related condition. Our observation that a mixed nasal profile was inversely associated with COME compared with profiles dominated by Corynebacterium, Streptococcus, or Moraxella has not previously been reported in relation to OM. This finding may indicate that a more mixed profile is protective against infection. Adult profiles tend to be more mixed, more stable, and more resistant to infection that those of children [39].
The association between COME and a profile dominated by Corynebacterium was unexpected, as this genus has previously been inversely associated with otitis media [25]. Nearly all reads of Corynebacterium belonged to an OTU classified in BLAST as Corynebacterium pseudodiptheriticum. This species is an opportunistic pathogen [40, 41]. However, it was not differentially abundant in our cases. The association may therefore be due to a higher abundance of Streptococcus and Moraxella in the Corynebacterium-dominated cluster than in the mixed cluster, rather than a direct association with Corynebacterium pseudodiptheriticum itself.
Randomized controlled trials of probiotics have demonstrated that bacterial interference can be successful in reducing nasal colonization with otopathogens to treat URIs and OM in children [42], although not all trials show a protective effect for every condition [43]. Such studies support the plausibility of certain microbial compositions, such as the mixed bacterial profile that we observed, helping to protect against disease.
The study has potential limitations. Cases and controls differed by ethnicity, however similar results were found in a sensitivity analysis that examined all major findings in the largest single ethnicity, and when including ethnicity in a multivariable analysis. Limitations of 16S rRNA gene sequencing are that it is unable to distinguish between live and dead microbial DNA, and is poorly suited to distinguishing between many bacteria below the genus level, including genera that include both respiratory pathogens and commensals. We did identify the key otopathogen H. influenzae using 16S rRNA sequencing, however future research using whole genome sequencing would enable more precise differentiation between pathogen and commensal species and strains. We did not include analysis of the virome which may have provided additional clarification. Finally, this case-control study could not investigate the causal direction of the association between COME and nasal bacterial composition, therefore we recommend future longitudinal studies.
Conclusion
The spread of pathogenic bacteria from the nasal passages to the ME may be involved in the pathogenesis of COME. Children with COME had a different nasal microbial profile to healthy controls, with lower diversity, higher abundance of pathogens, and lower abundance of commensals. Pathogens were equally likely to be present in the noses of healthy controls as in children with COME, and may therefore be endogenous pathobionts. Higher abundance of these pathobionts may increase the risk of COME, or help to maintain effusion once established. More research is required to determine the order of events leading to COME. If a more diverse and mixed nasal bacterial composition dominated by commensals proves to be protective against the spread of bacteria to the ME, this may present new opportunities to prevent or treat COME by influencing the microbiota of the nasal passages.
Supporting information
Appendix A. Detailed Methods and Appendix B. Detailed Results.
(DOC)
(DOCX)
(DOCX)
(DOCX)
(TIFF)
Acknowledgments
We would like to thank Ann Paddy, DHSc, who administered the questionnaires and performed part of the physical examinations for the children involved in the study. Dr. Rinki Murphy reviewed the manuscript and provided statistical advice. We would like to acknowledge the staff at Waitakere and North Shore Hospital, Bede Saldanha and Denise Burdett for going above and beyond reception support, and especially ear nurse specialist Barbara Middleton. Finally, a thank you to the families and their general practitioners whose help and support made the study possible.
Data Availability
The dataset is available in the SRA repository https://www.ncbi.nlm.nih.gov/bioproject/PRJNA414455/.
Funding Statement
This work was supported by: REW -The Oticon Foundation (Grant no. 3701863) http://www.oticon.org.nz/; REW -CRC Starship Foundation (Grant No. 18071300) https://www.starship.org.nz/; REW -Brian Johns Fellowship Trust (Grant no. 4711); EAM -Deafness Research Foundation (Grant no. 2013/08) https://www.nfd.org.nz/. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gates GA, Klein JO, Lim DJ, Mogi G, Ogra PL, Pararella MM, et al. Recent advances in otitis media. 1. Definitions, terminology, and classification of otitis media. The Annals of Otology, Rhinology & Laryngology Supplement 2002;188:8. [DOI] [PubMed] [Google Scholar]
- 2.Bennett KE, Haggard MP, Silva PA, Stewart IA. Behaviour and developmental effects of otitis media with effusion into the teens. Arch Dis Child 2001;85:91–5. 10.1136/adc.85.2.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngo CC, Massa HM, Thornton RB, Cripps AW. Predominant bacteria detected from the middle ear fluid of children experiencing otitis media: a systematic review. PLoS One 2016;11:e0150949 10.1371/journal.pone.0150949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stol K, Verhaegh SJ, Graamans K, Engel JA, Sturm PD, Melchers WJ, et al. Microbial profiling does not differentiate between childhood recurrent acute otitis media and chronic otitis media with effusion. Int J Pediatr Otorhinolaryngol 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall-Stoodley L, Hu FZ, Gieseke A, Nistico L, Nguyen D, Hayes J, et al. Direct detection of bacterial biofilms on the middle-ear mucosa of children with chronic otitis media. JAMA 2006;296:202–11. 10.1001/jama.296.2.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coates H, Thornton R, Langlands J, Filion P, Keil AD, Vijayasekaran S, et al. The role of chronic infection in children with otitis media with effusion: Evidence for intracellular persistence of bacteria. Otolaryngology—Head and Neck Surgery 2008;138:778–81. 10.1016/j.otohns.2007.02.009 [DOI] [PubMed] [Google Scholar]
- 7.Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nature Reviews Genetics 2012;13:260 10.1038/nrg3182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brook I. The role of bacterial interference in otitis, sinusitis and tonsillitis. Otolaryngology—Head and Neck Surgery 2005;133:139–46. 10.1016/j.otohns.2005.03.012 [DOI] [PubMed] [Google Scholar]
- 9.Man WH, de Steenhuijsen Piters WAA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nature Reviews Microbiology 2017;15:259–70. 10.1038/nrmicro.2017.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hilty M, Qi W, Brugger SD, Frei L, Agyeman P, Frey PM, et al. Nasopharyngeal microbiota in infants with acute otitis media. J Infect Dis 2012;205:1048–55. 10.1093/infdis/jis024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laufer AS, Metlay JP, Gent JF, Fennie KP, Kong Y, Pettigrew MM. Microbial communities of the upper respiratory tract and otitis media in children. mBio 2011;2:e00245–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chonmaitree T, Jennings K, Golovko G, Khanipov K, Pimenova M, Patel JA, et al. Nasopharyngeal microbiota in infants and changes during viral upper respiratory tract infection and acute otitis media. PLoS One 2017;12:e0180630 10.1371/journal.pone.0180630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Depner M, Ege MJ, Cox MJ, Dwyer S, Walker AW, Birzele LT, et al. Bacterial microbiota of the upper respiratory tract and childhood asthma. J Allergy Clin Immunol 2017;139:826–34. 10.1016/j.jaci.2016.05.050 [DOI] [PubMed] [Google Scholar]
- 14.Vissing NH, Chawes BL, Bisgaard H. Increased risk of pneumonia and bronchiolitis after bacterial colonization of the airways as neonates. Am J Respir Crit Care Med 2013;188:1246–52. 10.1164/rccm.201302-0215OC [DOI] [PubMed] [Google Scholar]
- 15.Hasegawa K, Mansbach JM, Ajami NJ, Espinola JA, Henke DM, Petrosino JF, et al. Association of nasopharyngeal microbiota profiles with bronchiolitis severity in infants hospitalised for bronchiolitis. Eur Respir J 2016:ERJ-00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teo SM, Mok D, Pham K, Kusel M, Serralha M, Troy N, et al. The infant nasopharyngeal microbiome impacts severity of lower respiratory infection and risk of asthma development. Cell host & microbe 2015;17:704–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker RE, Bartley J, Flint D, Thompson JM, Mitchell EA. Determinants of chronic otitis media with effusion in preschool children: a case-control study. BMC Pediatr 2017;17:4 10.1186/s12887-016-0767-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edgar RC. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nature methods 2013;10:996–8. 10.1038/nmeth.2604 [DOI] [PubMed] [Google Scholar]
- 19.McMurdie PJ, Holmes S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS One 2013;8:e61217 10.1371/journal.pone.0061217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oksanen J, Blanchet FG, Kindt R, Legendre P, Minchin PR, O’hara RB, et al. Package ‘vegan’. Community ecology package, version 2013;2. [Google Scholar]
- 21.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 2014;15:550 10.1186/s13059-014-0550-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maechler M, Rousseeuw P, Struyf A, Hubert M, Hornik K. cluster: Cluster Analysis Basics and Extensions. R package version 2.0.6. 2017. 2017. [Google Scholar]
- 23.Tibshirani R, Walther G, Hastie T. Estimating the number of clusters in a data set via the gap statistic. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 2001;63:411–23. [Google Scholar]
- 24.Pettigrew MM, Laufer AS, Gent JF, Kong Y, Fennie KP, Metlay JP. Upper respiratory tract microbial communities, acute otitis media pathogens and antibiotic use in healthy and sick children. Appl Environ Microbiol 2012;78:6262–70. 10.1128/AEM.01051-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lappan R, Imbrogno K, Sikazwe C, Anderson D, Mok D, Coates H, et al. A microbiome case-control study of recurrent acute otitis media identified potentially protective bacterial genera. BMC Microbiol 2018;18:13 10.1186/s12866-018-1154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Post JC, Preston RA, Aul JJ, Larkins-Pettigrew M, Rydquist-White J, Anderson KW, et al. Molecular analysis of bacterial pathogens in otitis media with effusion. JAMA 1995;273:1598–604. [PubMed] [Google Scholar]
- 27.Tonnaer EL, Rijkers GT, Meis JF, Klaassen CH, Bogaert D, Hermans PW, et al. Genetic relatedness between pneumococcal populations originating from the nasopharynx, adenoid, and tympanic cavity of children with otitis media. J Clin Microbiol 2005;43:3140–4. 10.1128/JCM.43.7.3140-3144.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wren JT, Blevins LK, Pang B, King LB, Perez AC, Murrah KA, et al. Influenza a virus alters pneumococcal nasal colonization and middle ear infection independently of phase variation. Infect Immun 2014;82:4802–12. 10.1128/IAI.01856-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnamurthy A, McGrath J, Cripps AW, Kyd JM. The incidence of Streptococcus pneumoniae otitis media is affected by the polymicrobial environment particularly Moraxella catarrhalis in a mouse nasal colonisation model. Microbes and Infection 2009;11:545–53. 10.1016/j.micinf.2009.03.001 [DOI] [PubMed] [Google Scholar]
- 30.Short KR, Diavatopoulos DA, Thornton R, Pedersen J, Strugnell RA, Wise AK, et al. Influenza virus induces bacterial and nonbacterial otitis media. The Journal of infectious diseases 2011;204:1857–65. 10.1093/infdis/jir618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Q, Wischmeyer J, Gonzalez E, Pichichero ME. Nasopharyngeal polymicrobial colonization during health, viral upper respiratory infection and upper respiratory bacterial infection. J Infect 2017;75:26–34. 10.1016/j.jinf.2017.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sajjan U, Wang Q, Zhao Y, Gruenert DC, Hershenson MB. Rhinovirus disrupts the barrier function of polarized airway epithelial cells. Am J Respir Crit Care Med 2008;178:1271–81. 10.1164/rccm.200801-136OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pittet LA, Hall-Stoodley L, Rutkowski MR, Harmsen AG. Influenza virus infection decreases tracheal mucociliary velocity and clearance of Streptococcus pneumoniae. Am J Respir Cell Mol Biol 2010;42:450–60. 10.1165/rcmb.2007-0417OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siegel SJ, Roche AM, Weiser JN. Influenza promotes pneumococcal growth during coinfection by providing host sialylated substrates as a nutrient source. Cell host & microbe 2014;16:55–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marks LR, Davidson BA, Knight PR, Hakansson AP. Interkingdom signaling induces Streptococcus pneumoniae biofilm dispersion and transition from asymptomatic colonization to disease. mBio 2013;4:e00438–13. 10.1128/mBio.00438-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brook I, Yocum P. Bacterial interference in the adenoids of otitis media-prone children. Pediatr Infect Dis J 1999;18:835–7. [DOI] [PubMed] [Google Scholar]
- 37.Lemon KP, Klepac-Ceraj V, Schiffer HK, Brodie EL, Lynch SV, Kolter R. Comparative analyses of the bacterial microbiota of the human nostril and oropharynx. mBio 2010;1:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lina G, Boutite F, Tristan A, Bes M, Etienne J, Vandenesch F. Bacterial competition for human nasal cavity colonization: role of staphylococcal agr alleles. Appl Environ Microbiol 2003;69:18–23. 10.1128/AEM.69.1.18-23.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stearns JC, Davidson CJ, McKeon S, Whelan FJ, Fontes ME, Schryvers AB. Culture and molecular-based profiles show shifts in bacterial communities of the upper respiratory tract that occur with age. ISME J 2015;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Camello TCF, Souza MC, Martins CAS, Damasco PV, Marques EA, Pimenta FP, et al. Corynebacterium pseudodiphtheriticum isolated from relevant clinical sites of infection: a human pathogen overlooked in emerging countries. Lett Appl Microbiol 2009;48:458–64. 10.1111/j.1472-765X.2009.02553.x [DOI] [PubMed] [Google Scholar]
- 41.Yang K, Kruse RL, Lin WV, Musher DM. Corynebacteria as a cause of pulmonary infection: a case series and literature review. Pneumonia 2018;10:10 10.1186/s41479-018-0054-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hao Q, Lu Z, Dong BR, Huang CQ, Wu T. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev 2011;9. [DOI] [PubMed] [Google Scholar]
- 43.Hatakka K, Blomgren K, Pohjavuori S, Kaijalainen T, Poussa T, Leinonen M, et al. Treatment of acute otitis media with probiotics in otitis-prone children—A double-blind, placebo-controlled randomised study. Clin Nutr 2007;26:314–21. 10.1016/j.clnu.2007.01.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A. Detailed Methods and Appendix B. Detailed Results.
(DOC)
(DOCX)
(DOCX)
(DOCX)
(TIFF)
Data Availability Statement
The dataset is available in the SRA repository https://www.ncbi.nlm.nih.gov/bioproject/PRJNA414455/.