Abstract
Schizophrenia is a mental disorder that is characterized by progressive cognitive impairment in areas of attention, working memory, and executive functioning. Although no clear etiology of schizophrenia has been discovered, many factors have been identified that contribute to the development of the disease, such as neurotransmitter alterations, decreased synaptic plasticity, and diminished hippocampal volume. Historically, antipsychotic medications have targeted biochemical alterations in the brains of patients with schizophrenia but have been ineffective in alleviating cognitive and hippocampal deficits. Other modalities, such as exercise therapy, have been proposed as adjuvant or primary therapy options. Exercise therapy has been shown to improve positive and negative symptoms, quality of life, cognition, and hippocampal plasticity, and to increase hippocampal volume in the brains of patients with schizophrenia. This article will briefly review the clinical signs, symptoms and proposed etiologies of schizophrenia, and describe the current understanding of exercise programs as an effective treatment in patients with the disease.
Keywords: exercise, schizophrenia, treatment, synaptic plasticity, neurodevelopment
Introduction
Schizophrenia is a mental disorder characterized by multiple psychiatric symptoms including hallucinations, delusions, disorganized speech, disorganized or catatonic behavior, and negative symptoms. Some patients experience cognitive symptoms, such as difficulty with attention, working memory, and executive functioning. Although an exact etiology of schizophrenia has not been discovered, many factors contribute to the development of the disease. Brain alterations such as neurotransmitter alterations and changes in hippocampal plasticity have been associated with schizophrenia. More recent evidence highlights the role of dysfunctional glutamatergic neurotransmission in the development of cognitive and negative symptoms. These biochemical alterations in the brains of patients with schizophrenia have historically been the targets of antipsychotic medications. In addition to the pharmacologic treatment of schizophrenia, other modalities, such as exercise therapy, have been proposed as adjuvant or primary therapy options. Numerous randomized controlled trials1 and meta-analyses2 have shown a positive effect of exercise in treating schizophrenia or schizophrenia-like illness. These improvements include decreased positive and negative symptoms, and improved quality of life. Research has shown that exercise leads to increased hippocampal plasticity in the brains of patients with schizophrenia and controls alike,3 suggesting that exercise can be used as part of a beneficial treatment plan for patients with schizophrenia. This article aims to briefly review the clinical signs, symptoms and proposed etiologies of schizophrenia, and describe the current understanding of exercise programs as an effective treatment in patients with the disease.
Background
Diagnostic Criteria
According to DSM-5, a formal clinical diagnosis of schizophrenia can be made in a patient when two or more of the following five symptoms are present for a period of at least one month (one of the two must be symptom 1, 2, or 3), and symptoms last for at least six months : (1) delusions, (2) hallucinations, (3) disorganized speech, (4) disorganized or catatonic behavior, and (5) negative symptoms (affect flattening, anhedonia, alogia, and avolition). Because schizophrenic symptoms may present in three phases—a prodromal, psychotic, and residual phase—the six month period may include prodromal and residual phases of the disease course, during which symptoms appear in an attenuated form.
The Phases of Schizophrenia and Associated Anatomic Changes
During the prodromal phase, a decline in functioning typically occurs. This phase precedes the first psychotic episode and is typically characterized by social isolation and irritability. Patients may also present with impaired bodily sensations, disrupted thought, disturbances in perception and motor activity, and impaired language. In one study, approximately half of the patients in a prodrome went on to develop schizophrenia and the mean transition time, after initial onset of prodrome, was 6.7 years for men and 4.3 years for women.4
A recent study reported that individuals in the prodromal phase evidenced structural changes in cingulate and temporal lobe volume, which progressed to further changes in the temporal lobe, cingulate, and parahippocampal gyrus during the first psychotic episode.5 This finding demonstrates that there are premorbid structural differences in the brains of individuals with a high likelihood of developing schizophrenia, and suggests there is progressive brain change during the course of the disease.
During the active and progressive psychotic phases, the first onset of overt psychosis occurs. This period typically lasts for 5 to 10 years and is characterized by progressive deterioration as well as increased psychotic symptomatology. Suicide risk is highest in this phase of disease. Again, changes in the brain may be seen on MRI during the active phase including a decrease in gray matter volume and integrity, and progressive reduction in white matter and frontal cortex size.6
A study conducted by Klauser et al. assessed white matter structures in patients with schizophrenia and controls using Fractional Anisotropy (FA) and Mean Diffusivity MRI techniques.7 FA is an MRI technique that measures the directional diffusion of water. When diffusion of water is constrained so it occurs in one direction as it moves through a series of neuronal fibers, diffusion is anisotropic (high FA). When diffusion through neural fiber bundles is disrupted, the diffusion of water occurs in all directions (isotropic diffusion) and has low fractional anisotropy. Klauser et al found that there is a significant reduction in fractional anisotropy affecting more than 40% of cerebral white matter volume in patients with schizophrenia, and that mean diffusivity was significantly increased in these patients as well. This study showed that all cerebral lobes were affected and that cortico-cortical as well as cortico-subcortical white matter fiber bundles were disrupted, demonstrating widespread pathology affecting many brain regions in patients with schizophrenia and schizophrenia-like illness.
Several post mortem studies have shown other alterations in the brain structure of patients with schizophrenia. These changes include decreased density of dendritic spines in pyramidal neurons of the prefrontal cortex, a primary site for excitatory synaptic input,8 and evidence of altered neural connectivity or “circuitry” in the hippocampus of schizophrenic patients.9
The chronic residual stage of schizophrenia usually begins within five to ten years following the first psychotic break. This phase includes persistence of residual “breakthrough” symptoms and disability resulting from positive, cognitive and negative symptoms. During the residual phase there is decreased disease progression and slowed decompensation as compared to the active stage. During the residual phase, patients continue to abuse substances, including alcohol (87% of patients), cannabis (44%), and cocaine (36%).10
Evidence from recent MRI studies and the presence of structural changes in schizophrenia underlie the view that schizophrenia is a neurodegenerative disease. However, some researchers suggest that other factors such as antipsychotic medication use and substance abuse with marijuana, tobacco, and alcohol, contribute to the structural brain changes observed in the disease.11
Other Proposed Etiologies of Schizophrenia
Neurodevelopmental Model
The neurodevelopmental model of schizophrenia is a theory that suggests prenatal and perinatal insults and then later adolescent developmental processes, such as pruning, contribute to the pathophysiology of disease. The neurodevelopmental model posits that schizophrenic illness is the end result of abnormal neurodevelopment that started many years before the disease clinically manifests. Some pre- and perinatal factors that have been associated with risk for disease include prenatal infection, famine during pregnancy, placental pathology, and low birth weight.12 By altering brain development, these insults increase susceptibility to disease. Events that take place later in adolescence, such as synaptic pruning of pyramidal cell circuits in the prefrontal cortex, may unmask the earlier abnormal development, or abnormal pruning itself may trigger the onset of the disease.13
Genetics
An exact etiology of schizophrenia has not been isolated; however, genetic predisposition is thought to account for up to 80% of the risk of developing the disease. Gottesman et al. showed that identical twins have a 48% chance of both developing schizophrenia if one twin has the disease. Furthermore, fraternal twins have a 17% chance, children of parents with schizophrenia have a 13% chance, and siblings have a 9% chance of developing the disease.14 Multiple alleles have been identified that may contribute to the risk of developing schizophrenia, however these alleles are all shown to have a small to moderate risk of disease progression alone. Genome Wide Association Studies (GWAS) have shown that the risk genes may include ZNF804A, OPCML, RPGRIP1L, NRGN, and TCF4 alleles.15 Additionally, DNA copy number variants (CNV) have been strongly associated with schizophrenia, the most strongly supported CNVs include chromosomal deletions at 1q21, 2p53, 3q29, 15p11.2, 15q11.3, 17q12, 22q11.2 and Neurexin 1 (NRXN1), and chromosomal duplications at 7q36.3, 25q11–13, 16p11.2 and 16p13.1.12 Alterations in these genes may contribute to problems during brain development and later cognitive function. Yet, these genetic anomalies only account for a small amount of observed schizophrenia, with sporadic cases still predominating.
Neurotransmitter Changes
Another proposed etiology relates to altered dopamine expression in the brains of these patients. Specifically, excessive dopamine activity in the mesolimbic pathway has been associated with “positive” symptoms, whereas decreased dopamine activity in the prefrontal cortex has been associated with “negative” symptoms. The theory that dopamine disregulation may lead to schizophrenia has come to be known as the dopamine hypothesis.16
Evidence to support this model includes the efficacy of antipsychotic medications, which aim to block dopamine receptors in the brain and are effective at reducing the symptoms of schizophrenia. Typical antipsychotics, like haloperidol and fluphenazine, act by blocking dopamine D2 receptors. Atypical antipsychotics, such as risperidone and quietiapine, are mostly D2 antagonists, but also have effects on 5-HT2, dopamine, α-1 and H1-receptors. Because these therapies are often nonspecific for the targeted dopamine pathways, there are many side effects associated with these drugs. These include extrapyramidal side effects like tremor, rigidity, akathisia, and dystonia as a result of effects on the nigrostriatal dopamine pathway, and endocrine effects such as hyperprolactinemia and galactorrhea from effects on the tuberoinfundibular dopaminergic pathway. Non-dopamine pathways can be affected, leading to blockade of acetylcholine muscarinic receptors (dry mouth, constipation), α1 receptors (orthostatic hypotension), and histamine receptors (sedation).
Other neurotransmitter abnormalities that have been implicated in schizophrenia include elevated serotonin, elevated norepinephrine, decreased gamma-aminobutyric acid (GABA) concentration in the hippocampus, and decreased glutamate receptor expression.17
Exercise and Schizophrenia
Physical exercise may be beneficial for patients with schizophrenia, with the potential to improve cognition, clinical symptoms, and quality of life. Schizophrenia is associated with severe impairments in cognitive functioning, with deficits of 1-2 Standard Deviations below the general population. These cognitive impairments contribute significantly to the poor functional outcomes observed in patients with schizophrenia.18 Thus far, pharmacological approaches, including antipsychotics, have had limited efficacy in treating these cognitive deficits.19
The hippocampus plays an integral role in learning and memory, and is particularly vulnerable to impairment in schizophrenia. Patients with schizophrenia have been shown to have smaller hippocampal volume compared to the general population, likely secondary to neuronal atrophy.20 The hippocampus has a high degree of neuroplasticity, and is one of only two areas of the brain that has been shown to demonstrate adult neurogenesis, the other being the olfactory bulb.21 Abnormalities seen in the hippocampal neurons and olfactory neurons in schizophrenia further indicate an impairment in neural plasticity and adult neurogenesis in schizophrenia.22 These hippocampal abnormalities have been correlated with deficits in cognition memory, and executive functioning in schizophrenia.23 Patients with schizophrenia have also been found to have decreased serum levels of brain-derived neurotrophic factor (BDNF), a protein that supports survival, growth, and differentiation of neurons and synapses that enable learning, memory and cognition.24 Unfortunately, pharmacological treatment does not appear to increase hippocampal volume or neurogenesis25 or enhance cognition in these patients.19
In the general population, aerobic exercise has been shown to improve attention, processing speed, memory and executive functions,26 many of which are impaired in schizophrenia. Exercise has also been shown, in healthy individuals, to increase hippocampal volume and blood flow, stimulate neurogenesis, modulate synaptic plasticity, and increase growth factors such as BDNF that are involved in optimizing brain functioning.27,28 Specifically, BDNF has been shown to mediate the effects of exercise on synaptic plasticity through actions on axonal and dendritic remodeling, synaptogenesis, and synaptic efficacy. It has been found to be integrally involved in learning and memory. For example, in rat studies by Gomez et al, suppression of BDNF action during exercise blocked the exercise-mediated enhancement of synaptic plasticity and cognitive function.29
In summary, aerobic exercise has a promising role to play in combating the deficits in cognition, memory, hippocampal volume, and neural plasticity.
Structural Effects and Neuroplasticity
Pajonk et al.3 demonstrated in a randomized controlled trial that 3 months of aerobic exercise training in patients with schizophrenia (moderate-intensity cycling) increased hippocampal volume by 12% compared to no improvement (−1%) in the non-exercise group (P = 0.002). Furthermore, the changes in hippocampal volume in the exercise group correlated significantly with improvements in aerobic fitness, measured by the change in oxygen consumption. Improvement in test scores of short-term memory was also significantly correlated with change in hippocampal volume for the total group, indicating a clinical correlation between memory functioning, hippocampal volume and physical fitness. Patients in the aerobic exercise group had a 34% increase in short-term memory test scores, while the control group’s scores decreased by 17%. These findings suggest that the hippocampus in patients with schizophrenia retains a degree of plasticity in response to aerobic exercise, increasing in volume with associated improvements in memory and symptoms.
Another analysis randomized chronic schizophrenia patients to either six months of aerobic exercise or “treatment as usual” and found that the exercise group had increased white matter integrity in a number of fiber tracts related to motor functioning, tracts that are also involved with attention, memory and executive functions.30 It has also been observed that exercise induces increased serum levels of BDNF as well as improved neurocognitive functioning in patients with schizophrenia after 12 weeks of an exercise program.31
Cognition
Cognitive impairment spanning multiple domains is a debilitating aspect of schizophrenia, for which an effective treatment has not been found. In a meta-analysis, Firth et al. showed that physical exercise was able to significantly improve global cognition in patients with schizophrenia compared to controls (g = 0.33, 95% CI=0.13–0.53, P = 0.001) in 10 studies with 385 total participants.32 Additionally, the researchers found that exercise programs that were supervised by physical activity professionals were significantly more effective than those that were not in improving global cognition (P < 0.001), likely due to increased exercise participation by subjects. Specifically, the researchers found that exercise was particularly beneficial in improving social cognition (g = 0.71), working memory (g = 0.39) and attention (g = 0.66). One hypothesis is that the improvement in cognition seen after aerobic exercise could be due to an increase in BDNF, leading to increased neurogenesis and cognitive performance. However, further research is needed to elucidate the potential mechanisms of how exercise improves cognitive functioning in schizophrenia.
In this analysis, exercise had the largest effect on improving social cognition, a finding that has vast potential benefits for patients with schizophrenia. In schizophrenia, improvement in social cognition has been linked to increased employment, independent living, and ability to function in society.33 Therefore, exercise has the potential to improve social cognitive deficits and psychosocial, functional, and socio-occupational outcomes for people with schizophrenia. These findings were further strengthened by a cross-sectional study that found aerobic fitness to be significantly correlated with performance in the cognitive domains of reasoning, problem solving, processing speed, social cognition and working memory, as well as with overall daily functioning in these patients.34
Clinical Symptoms
Positive symptoms of schizophrenia are effectively treated by antipsychotic medications, but negative symptoms have been more difficult to diminish. Moreover, negative symptoms in schizophrenia have been significantly associated with poorer functional outcomes.35 In a large-scale meta-analysis, Dauwan et al. found that physical exercise had an overall significant effect on improving the clinical symptoms of schizophrenia in a total of 1109 patients.36 Exercise was significantly superior to controls in improving total symptom severity (g = 0.32, P < 0.001), negative symptoms (g = 0.49, p < 0.001), and positive symptoms (g = 0.32, p < 0.01). Yoga, specifically, improved long-term memory. The results of these studies demonstrate that exercise can improve clinical symptoms, global functioning, quality of life, and depressive symptoms in schizophrenia. Specifically, the largest effect size was seen with improving negative symptoms, which has promising implications for future functional outcomes of these patients.
Exercise was able to reduce symptoms of schizophrenia in other studies as well. In a multicenter randomized clinical trial, Sheewe et al. compared the effect of exercise twice a week versus occupational therapy on the mental health of patients with schizophrenia.37 They found that exercise therapy significantly reduced symptoms of schizophrenia based on the Positive and Negative Syndrome Sale (P = 0.001) compared to occupational therapy. Symptoms of depression were also significantly decreased in the exercise group (P = 0.012).
Physical Health
Exercise can play a major role in mitigating health problems resulting from the pharmacologic treatment of schizophrenia. Specifically, antipsychotic (AP) medications often result in the side effects of obesity, diabetes and metabolic syndrome, which likely contributes to the shortened lifespan and 2-3-fold increased mortality rate seen in schizophrenia when compared to the general population.38 Weight gain can also contribute to impairment in these patients’ self-esteem as well as increased distress related to physical appearance and social interactions. Data from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia study demonstrated there was a 35.8% prevalence of metabolic syndrome among 1460 enrolled schizophrenic patients.10 Metabolic syndrome in these patients was strongly associated with poor self-rating of physical health (p < 0.001) and increased somatic preoccupation (p = 0.03). Exercise could be a beneficial adjunct to AP medications in order to mitigate the associated health risks, lower the increased mortality rates, and decrease the psychological stress associated with AP side effects, including metabolic syndrome (Table 1).
Table 1. Effects of Exercise in Schizophrenia.
| Improve attention, processing speed, memory and executive functions. | Smith et al., 201126 |
| Increase hippocampal volume and blood flow. | Pajonk et al., 20103 Erickson et al., 201127 Van Praag, 200828 |
| Stimulate neurogenesis, modulate synaptic plasticity. | Erickson et al., 201127 Van Praag, 200828 |
| Increase growth factors such as BDNF that are involved in optimizing brain functioning. | Kim et al., 201431 |
| Short term memory improvement. | Pajonk et al., 20103 |
| Increase white matter integrity in tracts related to motor functioning, attention, memory and executive functions. | Svatkova et al., 201530 |
| Improve global cognition in areas of social cognition, working memory and attention. | Firth et al., 201632 |
| Improve cognitive domains of reasoning, problem solving, processing speed, social cognition, working memory, and daily functioning. | Kimhy et al., 201534 |
| Improve total symptom severity (g = 0.32, P < 0.001), negative symptoms (g = 0.49, p < 0.001), and positive symptoms (g = 0.32, p < 0.01). | Dauwan, Begemann, Heringa, Sommer, 201636 |
| Improve symptoms of depression. | Scheewe et al., 201337 Schuch et al., 201639 |
| Improvement in physical health; weight loss. |
Exercise as a Treatment in Depression
Exercise has been shown to be an effective treatment in mental illness other than schizophrenia. In a meta-analysis of randomized controlled trials involving exercise interventions in people with depression, Schuch et al. found that exercise had a large and significant effect on reducing depressive symptoms when compared to controls.39 There was a mean improvement of 6.46 points (p < 0.001) on the Beck depression inventory scale of depressive symptoms in the exercise group compared to the control group. The largest effects were seen with interventions in patients with major depressive disorder (MDD), that utilized aerobic exercise of moderate intensity, and that included supervised exercise treatments. Exercise was demonstrated to have significant antidepressant effect on patients with MDD, supporting the idea (or concept) that exercise could be an evidence-based treatment for depression.
The efficacy of exercise compared to antidepressant medication has also been investigated. Blumenthal et al. randomly assigned 156 people with depression to an exercise, medication, or exercise plus medication group.40 The exercise group involved walking or jogging on a treadmill at 70–85% of maximum heart rate for 30 minutes 3 times per week for 16 weeks. The medication group received sertraline, which was adjusted based on efficacy and side effects. The combination group received both interventions. Results demonstrated that while sertraline reduced depressive symptoms more quickly, there were no significant differences in depressive symptoms among treatment groups at 16 weeks (P = 0.39). There was also no significant difference in remission rates among groups (60.4% in the exercise group, 68.8% in the medication group, and 65.5% in the combination group, p = 0.67). These results indicate that exercise was as effective as medication for reducing symptoms of depression and inducing remission. Additionally, at 10-month follow-up, the exercise group had significantly lower rates of depression than those in the medication or combination groups (70% vs 48% vs 54%, p = 0.028) indicating a lasting antidepressant effect of exercise therapy. Additionally, continued regular exercise involvement after 10 months was a significant predictor of lower rates of depression (OR = 0.49, P < 0.01).
Major depression, like schizophrenia, is associated with reduced hippocampal volumes and decreased synaptic plasticity. Antidepressant medications have been shown to promote synaptogenesis, neurogenesis, and neuronal maturation in the hippocampus. One mechanism through which this is believed to occur is by increasing BDNF synthesis in the hippocampus.41 This is one theory behind the disconnect between the delayed onset of antidepressant effects of SSRIs (weeks) and the peak of serotonin levels within 6–8 hours. It is believed that these psychotropic medications are causing antidepressant effects by increasing BDNF levels and inducing neurogenesis, which can take weeks to take effect. Exercise has also been shown to increase BDNF levels and improve synaptic plasticity of the hippocampus, likely playing a role in the mechanism of the significant antidepressant effects of exercise.
Conclusion
Schizophrenia can be a devastating, life-long illness that leads to cognitive impairment, debilitating positive and negative symptoms, and a shortened lifespan (Figure 1). Psychopharmacological treatments are not entirely effective in alleviating the cognitive deficits, negative symptoms, and increased mortality. Exercise, as a nonpharmacological adjunctive treatment, increases hippocampal volume and BDNF levels leading to improvements in synaptic plasticity and neurogenesis, cognition, negative symptoms, and functional outcomes. Furthermore, aerobic exercise may reduce the physical health problems associated with schizophrenia and offset antipsychotic side effects, such as obesity, diabetes, and metabolic syndrome, resulting in improved mortality rates. Barriers to exercise treatment include patient adherence, particularly in patients with severe negative symptoms. Structured, observed aerobic exercise programs appear to be the most effective in achieving compliance.
Figure 1.
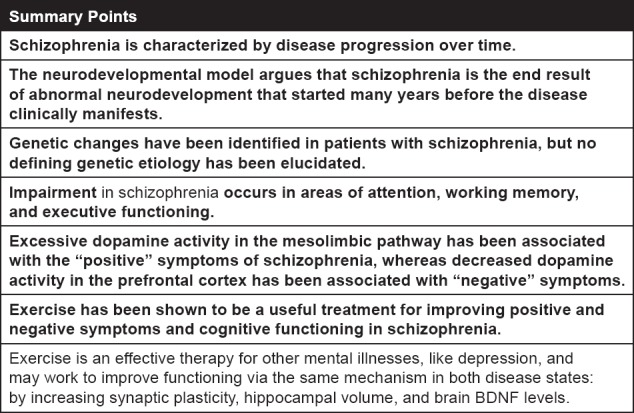
Summary Points: Changes in Schizophrenia and the Effects of Exercise
This review indicates significant benefits to including structured exercise programs in the treatment of schizophrenia. However, additional research is needed to better understand the most effective treatment approach, addressing variables such as exercise modality, frequency, and duration, as most studies have only looked at 3-month follow-ups. The efficacy of exercise routines introduced at different stages of disease progression—prodromal, psychotic, and residual—could be studied. For example, early intervention with a sustained aerobic exercise program in the prodromal phase may slow progression to the psychotic phase. The research presented here suggests exercise is a beneficial modality in the treatment of schizophrenia, and more research is needed to best understand optimal implementation of exercise regimens in patients with this chronic disorder.
Conflict of Interest
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. They have no conflicts of interest to report.
Acknowledgments
Daniel Kanofsky, MD MPH for teaching us about alternative treatment methods for patients with schizophrenia and inspiring the idea behind this review.
Footnotes
Author Contributions
Steven Girdler, MD- Responsible for literature review, interpretation, and drafting of the introduction, background, and etiology sections of the manuscript. Responsible for critical revision of the manuscript.
Jamie Confino, BS- Responsible for literature review, interpretation, and drafting of the exercise and schizophrenia section of the manuscript. Responsible for critical revision of the manuscript.
Mary Woesner, MD- Responsible for critical revision of the manuscript and key administrative support.
References
- 1.Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. The Cochrane Database of Systematic Reviews. 2010;(5) doi: 10.1002/14651858.CD004412.pub2. CD004412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. 2016 doi: 10.1017/S0033291714003110. [DOI] [PubMed] [Google Scholar]
- 3.Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I, Falkai P. Hippocampal plasticity in response to exercise in schizophrenia. Archives of General Psychiatry. 2010;67(2):133–43. doi: 10.1001/archgenpsychiatry.2009.193. [DOI] [PubMed] [Google Scholar]
- 4.Klosterkötter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Archives of General Psychiatry. 2001;55(2):158–64. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- 5.Pantelis C, Yücel M, Wood SJ, McGorry PD, Velakoulis D. Early and late neurodevelopmental disturbances in schizophrenia and their functional consequences. The Australian and New Zealand Journal of Psychiatry. 2003;37(4):399–406. doi: 10.1046/j.1440-1614.2003.01193.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12873323. [DOI] [PubMed] [Google Scholar]
- 6.Thompson PM, Vidal C, Giedd JN, Gochman P, Blumenthal J, Nicolson R, Rapoport JL. Mapping adolescent brain change reveals dynamic wave of accelerated gray matter loss in very early-onset schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(20):11650–5. doi: 10.1073/pnas.201243998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klauser P, Baker ST, Cropley VL, Bousman C, Fornito A, Cocchi L, Zalesky A. White Matter Disruptions in Schizophrenia Are Spatially Widespread and Topologically Converge on Brain Network Hubs. Schizophrenia Bulletin. 2016 doi: 10.1093/schbul/sbw100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glantz LA, Lewis DA. Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Archives of General Psychiatry. 2000;57(1):65–73. doi: 10.1001/archpsyc.57.1.65. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10632234. [DOI] [PubMed] [Google Scholar]
- 9.Harrison PJ. The hippocampus in schizophrenia: a review of the neuropathological evidence and its pathophysiological implications. Psychopharmacology. 2004;174(1):151–62. doi: 10.1007/s00213-003-1761-y. [DOI] [PubMed] [Google Scholar]
- 10.Meyer JM, Nasrallah HA, McEvoy JP, Goff DC, Davis SM, Chakos M, Lieberman JA. The Clinical Antipsychotic Trials Of Intervention Effectiveness (CATIE) Schizophrenia Trial: clinical comparison of subgroups with and without the metabolic syndrome. Schizophrenia Research. 2005;80(1):9–18. doi: 10.1016/j.schres.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Zipursky RB, Reilly TJ, Murray RM. The myth of schizophrenia as a progressive brain disease. Schizophrenia Bulletin. 2013;39(6):1363–1372. doi: 10.1093/schbul/sbs135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rapoport JL, Giedd JN, Gogtay N. Neurodevelopmental model of schizophrenia: update 2012. Molecular Psychiatry. 2012;17(12):1228–38. doi: 10.1038/mp.2012.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WooTU. W. Neurobiology of Schizophrenia Onset. 2013:267–295. doi: 10.1007/7854_2013_243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGue M, Gottesman II. The genetic epidemiology of schizophrenia and the design of linkage studies. European Archives of Psychiatry and Clinical Neuroscience. 1991;240(3):174–81. doi: 10.1007/BF02190760. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1827604. [DOI] [PubMed] [Google Scholar]
- 15.Umeda-Yano S, Hashimoto R, Yamamori H, Weickert CS, Yasuda Y, Ohi K, Takeda M. Expression analysis of the genes identified in GWAS of the postmortem brain tissues from patients with schizophrenia. Neuroscience Letters. 2014;568:12–6. doi: 10.1016/j.neulet.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 16.Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: Version III—The final common pathway. Schizophrenia Bulletin. 2009 doi: 10.1093/schbul/sbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egan M. F., Hyde T. M. (n.d.). CHAPTER 12. SCHIZOPHRENIA 12.4 SCHIZOPHRENIA: NEUROBIOLOGY Role of Genes and Environment Structural and Functional Neuroimaging Neuropathology Neurochemistry Neural Circuits Neurobiological Models. [Google Scholar]
- 18.Hoff AL, Sakuma M, Wieneke M, Horon R, Kushner M, DeLisi LE. Longitudinal neuropsychological follow-up study of patients with first-episode schizophrenia. The American Journal of Psychiatry. 1999;156(9):1336–41. doi: 10.1176/ajp.156.9.1336. [DOI] [PubMed] [Google Scholar]
- 19.Harvey PD. Pharmacological cognitive enhancement in schizophrenia. Neuropsychology Review. 2009 doi: 10.1007/s11065-009-9103-4. [DOI] [PubMed] [Google Scholar]
- 20.Steen RG, Mull C, McClure R, Hamer RM, Lieberman JA. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. British Journal of Psychiatry. 2006;188:510–518. doi: 10.1192/bjp.188.6.510. doi: 188/6/510 [pii]\r10.1192/bjp.188.6.510. [DOI] [PubMed] [Google Scholar]
- 21.Ernst A, Frisén J. Adult Neurogenesis in Humans-Common and Unique Traits in Mammals. PLoS Biology. 2015;13(1):e1002045. doi: 10.1371/journal.pbio.1002045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reif A, Fritzen S, Finger M, Strobel A, Lauer M, Schmitt A, Lesch KP. Neural stem cell proliferation is decreased in schizophrenia, but not in depression. Mol Psychiatry. 2006;11(5):514–522. doi: 10.1038/sj.mp.4001791. doi: 4001791 [pii]\r10.1038/sj.mp.4001791. [DOI] [PubMed] [Google Scholar]
- 23.Gur RE, Turetsky BI, Cowell PE, Finkelman C, Maany V, Grossman RI, Gur RC. Temporolimbic volume reductions in schizophrenia. Archives of General Psychiatry. 2000;57(8):769–75. doi: 10.1001/archpsyc.57.8.769. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10920465. [DOI] [PubMed] [Google Scholar]
- 24.Green MJ, Matheson SL, Shepherd A, Weickert CS, Carr VJ. Brain-derived neurotrophic factor levels in schizophrenia: a systematic review with meta-analysis. Molecular Psychiatry. 2011;16(9):960–972. doi: 10.1038/mp.2010.88. [DOI] [PubMed] [Google Scholar]
- 25.Wood SJ, Velakoulis D, Smith DJ, Bond D, Stuart GW, McGorry PD, Pantelis C. A longitudinal study of hippocampal volume in first episode psychosis and chronic schizophrenia. Schizophrenia Research. 2001;52(1–2):37–46. doi: 10.1016/S0920-9964(01)00175-X. [DOI] [PubMed] [Google Scholar]
- 26.Smith PJ, Blumenthal JA, Hoffman BM, Strauman TA, Welsh-bohmer K, Jeffrey N, Sherwood A. Aerobic exercise and neurocognitive performance: a meta- analytic review of randomized controlled trials. Psychosomatic Medicine. 2011;72(3):239–252. doi: 10.1097/PSY.0b013e3181d14633.Aerobic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, Kramer A. F. Exercise training increases size of hippocampus and improves memory. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(7):3017–22. doi: 10.1073/pnas.1015950108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Praag H. Neurogenesis and exercise: Past and future directions. NeuroMolecular Medicine. 2008 doi: 10.1007/s12017-008-8028-z. [DOI] [PubMed] [Google Scholar]
- 29.Gomez-Pinilla F, Vaynman S, Ying Z. Brain-derived neurotrophic factor functions as a metabotrophin to mediate the effects of exercise on cognition. European Journal of Neuroscience. 2008;28(11):2278–2287. doi: 10.1111/j.1460-9568.2008.06524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Svatkova A, Mandl RCW, Scheewe TW, Cahn W, Kahn RS, Hulshoff Pol HE. Physical Exercise Keeps the Brain Connected: Biking Increases White Matter Integrity in Patients with Schizophrenia and Healthy Controls. Schizophrenia Bulletin. 2015;41(4):869–878. doi: 10.1093/schbul/sbv033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim H, Song B, So B, Lee O, Song W, Kim Y. Increase of circulating BDNF levels and its relation to improvement of physical fitness following 12 weeks of combined exercise in chronic patients with schizophrenia: A pilot study. Psychiatry Research. 2014;220(3):792–796. doi: 10.1016/j.psychres.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 32.Firth J, Stubbs B, Rosenbaum S, Vancampfort D, Malchow B, Schuch F, Yung AR. Aerobic Exercise Improves Cognitive Functioning in People With Schizophrenia: A Systematic Review and Meta-Analysis. Schizophrenia Bulletin. 2016 doi: 10.1093/SCHBUL/SBW115. sbw115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fett AKJ, Viechtbauer W, Dominguez MG, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: A meta-analysis. Neuroscience & Biobehavioral Reviews. 2011;35(3):573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 34.Kimhy D, Vakhrusheva J, Bartels MN, Armstrong HF, Ballon JS, Khan S, Sloan RP. The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: A single-blind, randomized clinical trial. Schizophrenia Bulletin. 2015;41(4):859–868. doi: 10.1093/schbul/sbv022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin CH, Huang CL, Chang YC, Chen PW, Lin CY, Tsai GE, Lane HY. Clinical symptoms, mainly negative symptoms, mediate the influence of neurocognition and social cognition on functional outcome of schizophrenia. Schizophrenia Research. 2013;146(1–3):231–237. doi: 10.1016/j.schres.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Dauwan M, Begemann MJH, Heringa SM, Sommer IE. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: A systematic review and meta-analysis. Schizophrenia Bulletin. 2016;42(3):588–599. doi: 10.1093/schbul/sbv164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scheewe TW, Backx FJG, Takken T, Jörg F, van Strater ACP, Kroes AG, Cahn W. Exercise therapy improves mental and physical health in schizophrenia: a randomised controlled trial. Acta Psychiatrica Scandinavica. 2013;127(6):464–473. doi: 10.1111/acps.12029. [DOI] [PubMed] [Google Scholar]
- 38.Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Current Opinion in Psychiatry. 2012;25:83–88. doi: 10.1097/YCO.0b013e32835035ca. [DOI] [PubMed] [Google Scholar]
- 39.Schuch FB, Deslandes AC, Stubbs B, Gosmann NP, Silva CTB. da, Fleck M. P. de A. Neurobiological effects of exercise on major depressive disorder: A systematic review. Neuroscience and Biobehavioral Reviews. 2016 doi: 10.1016/j.neubiorev.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 40.Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, Sherwood A. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic Medicine. 2007;691(7):587–96. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Castren E, Vaikar V, Rantamaki T. Role of neurotrophic factors in depression. Current Opinion in Pharmacology. 2007;7(1):18–21. doi: 10.1016/j.coph.2006.08.009. [DOI] [PubMed] [Google Scholar]


