Abstract
Background:
Press-fit humeral fixation for reverse shoulder arthroplasty (RSA) has been shown to have loosening rates and outcomes similar to a cemented technique; however, increased value has not been reported. The purpose of this study was to determine whether the press-fit technique could improve the value of RSA using the procedure value index (PVI).
Methods:
Primary RSA patients with complete hospitalization cost data, preoperative and minimum 2-year postoperative Simple Shoulder Test (SST) scores, and postoperative satisfaction were included. The PVI was calculated as improvement in the SST score (in units of minimal clinically important difference) divided by total cost and normalized. Itemized cost data were obtained from hospital financial records and categorized. Radiographic complications, infections, and revisions were noted. Comparisons were made between the press-fit and cemented RSA cohorts.
Results:
A total of 176 primary RSA patients (83 cemented and 93 press fit) met the inclusion criteria (mean follow-up period, 44.6 months). Surgical indications (except failed rotator cuff repair), baseline SST scores, and demographic characteristics were similar. The calculated minimal clinically important difference for the SST score was 3.98. The average PVI was significantly greater in the press-fit cohort (1.51 vs 1.03, P <.001), representing a 47% difference. SST score improvement was not significantly different (P = .23). However, total hospitalization costs were significantly lower for the press-fit cohort ($10,048.89 vs $13,601.14; P < .001).
Conclusion:
Use of a press-fit technique led to a 47% increase in value over a cemented technique. This appeared to be a function of decreased total costs rather than increased outcome scores.
Level of evidence:
Level IV; Economic Analysis
Keywords: Reverse shoulder arthroplasty (RSA), press fit, cemented, procedure value index (PVI), value, cost, SST, radiographic outcomes
In response to favorable clinical outcomes15,24 and recent expansion of indications,6,13,20,23 the use of reverse shoulder arthroplasty (RSA) has seen rapid growth.25,29 Early techniques primarily used cement fixation of the humeral stem.14 However, press-fit (uncemented) humeral techniques have gained popularity in recent years, with several studies showing no difference in loosening rates or outcomes.8,30 Potential advantages of the press-fit technique include a shorter operating room time, ease of revision, decrease in the effective joint space, longer-lasting biological fixation, and lower cementation-related equipment costs.14 Although studies comparing clinical outcomes of cemented and press-fit humeral techniques are limited, no differences in loosening rates have been observed for both anatomic total shoulder arthroplasty18,28 and reverse total shoulder arthroplasty (ie, RSA).8,9,11,31
With an ever-increasing emphasis on cost-effective use of resources in today’s health care systems, new technology is often criticized for increasing cost without a justified improvement in outcomes or value. Discussions on the importance of value in health care interventions have focused on measuring value as the ratio of outcomes over cost.22 The procedure value index (PVI) is a method for tracking value within a specific patient population and is calculated as the ratio of outcome improvement in units of minimal clinically important difference (MCID) over cost. With the overall lower costs associated with elimination of cement-related equipment and decreasing operating room time, it is possible that a press-fit humeral fixation technique in RSA can actually increase overall value. However, to date, this has not been evaluated.
The purpose of this study was to determine whether the introduction of a press-fit humeral technique has a positive impact on the value of RSA. A secondary analysis was performed to determine whether change in either outcome or cost influenced differences in the PVI. The hypothesis was that the press-fit humeral technique would create an overall improvement in the PVI based on improvements in hospitalization costs.
Methods
A retrospective query of all patients undergoing primary RSA from 2007–2015 was performed using our institutional shoulder and elbow surgical repository. The inclusion criteria for the study consisted of cost data (total hospitalization costs) as well as complete preoperative and minimum 2-year postoperative Simple Shoulder Test (SST) scores and postoperative satisfaction. Patients using both Medicare and private insurance companies as third-party payers were included in the study. Revision procedures and acute proximal humeral fractures were excluded. Patients were divided into 2 groups based on whether a cemented or press-fit humeral stem fixation technique was used at the time of surgery. The surgical indications (Table I) and demographic characteristics (age, sex, body mass index [BMI], and baseline preoperative SST score; Table II) of the 2 cohorts were compared.
Table I.
Indications for surgery in patients undergoing reverse shoulder arthroplasty in press-fit and cemented cohorts
| Press-fit cohort (93 patients) |
Cemented cohort (83 patients) |
P value | |||
|---|---|---|---|---|---|
| Indication | No. of patients (91 total with indication data)* | % | No. of patients (81 total with indication data)* | % | |
| Osteoarthritis with rotator cuff pathology | 80 | 87.9 | 70 | 86.4 | .770 |
| Osteoarthritis without rotator cuff tear | 16 | 17.6 | 8 | 9.9 | .147 |
| Failed RCR | 11 | 12.1 | 2 | 2.5 | .018 |
| Malunion or nonunion | 9 | 9.9 | 9 | 11.1 | .795 |
| Avascular necrosis | 6 | 6.6 | 1 | 1.2 | .077 |
| Glenoid fracture | 5 | 5.5 | 8 | 9.9 | .279 |
| Inflammatory arthritis | 3 | 3.3 | 3 | 3.7 | .885 |
| Locked anterior dislocation | 1 | 1.1 | 4 | 4.9 | .136 |
| Massive rotator cuff tear with pseudoparalysis | 0 | 0.0 | 3 | 3.7 | NA |
RCR, rotator cuff repair; NA, not applicable.
Some patients had more than 1 listed surgical indication and were thus included in multiple categories.
Table II.
Demographic data for patients undergoing RSA in press-fit and cemented cohorts
| Cemented cohort (n = 83) | Press-fit cohort (n = 93) | P value | All primary RSA (n = 176) | |
|---|---|---|---|---|
| Sex, M:F | 30:53 | 39:54 | .433 | 69:107 |
| Age, yr | 76.49 ± 5.96 | 74.25 ± 8.82 | .048 | 75.30 ± 7.67 |
| BMI | 28.45 ± 5.99 | 29.59 ± 6.23 | .221 | 29.05 ± 6.13 |
| Preoperative SST score | 2.23 ± 1.68 | 2.18 ± 1.71 | .857 | 2.20 ± 1.69 |
RSA, reverse shoulder arthroplasty; M, male; F, female; BMI, body mass index; SST, Simple Shoulder Test.
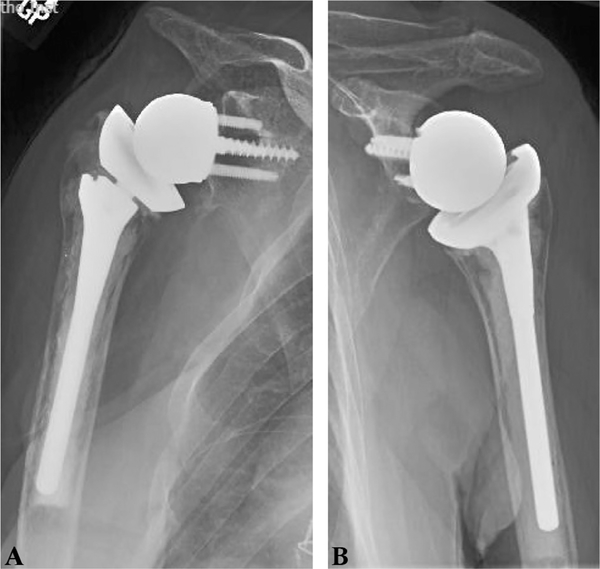
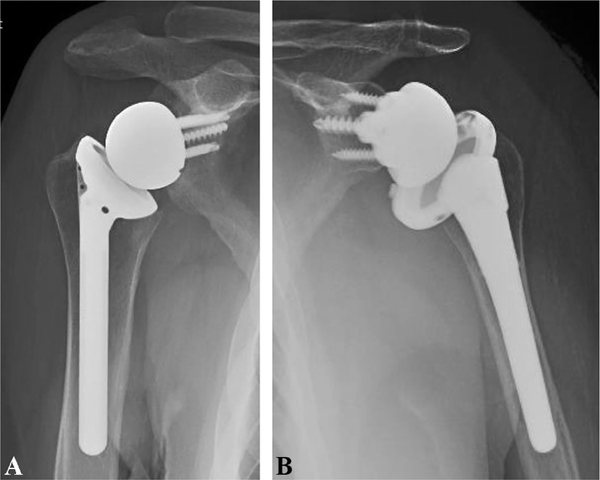
All procedures were performed by a single shoulder and elbow fellowship–trained surgeon who performs high-volume shoulder arthroplasty annually at a single institution. The press-fit technique for the RSA humeral stem became routinely performed at our institution in 2013. Once this technique was introduced, a press-fit technique was initially attempted in all patients. When a press fit was not believed to have been achieved, the cemented technique was used. All cemented humeral components were implanted with a Stryker cement gun system using Stryker Simplex P with tobramycin cement (Stryker, Mahwah, NJ, USA) and a Clear-Cut cement restrictor (DJO, Austin, TX, USA). There were 70 modular (RSP; DJO) and 13 Monoblock (DJO) cemented humeral components (Fig. 1). Press-fit humeral stems were implanted with a preferential metaphyseal press fit using an inset humeral component (DJO Monoblock in 89 and DJO AltiVate in 2) in 91 patients (Fig. 2, A) and with a diaphyseal press fit using a modular onset humeral component (Comprehensive Reverse; Biomet, Warsaw, IN, USA) in 2 patients (Fig. 2, B). The humeral stem fixation technique was noted by the surgeon in the operative report and entered into the surgical repository. In several cases in which a press-fit humeral technique was used, cement equipment was previously opened during the procedure.
Figure 1.
Cemented humeral stem. (A) Anteroposterior radiograph of a right shoulder showing an example of a cemented modular humeral stem. (B) Anteroposterior radiograph of a left shoulder showing an example of a cemented Monoblock humeral stem.
Figure 2.
Press-fit humeral stem. (A) Anteroposterior radiograph of a right shoulder showing an example of a metaphyseal press-fit inset humeral stem. (B) Anteroposterior radiograph of a left shoulder showing an example of a diaphyseal press-fit humeral stem.
SST scores were recorded at preoperative and postoperative intervals as a part of the standard registry protocol. Patient satisfaction with surgery was reported at follow-up intervals as excellent, good, satisfactory, or unsatisfactory.
The MCID for the study cohort was calculated as the difference between the mean SST score improvement in patients reporting satisfaction as good or satisfactory and that of patients reporting satisfaction as unsatisfactory, according to previous methods.27 Patients with excellent satisfaction were not included in the MCID analysis because they were said to be beyond minimal change.27
The initial and most recent postoperative radiographs were evaluated for signs of humeral stem loosening and subsidence using the Sperling classification.26 A stem was considered grossly loose if radiolucent lines greater than 2 mm were present around 3 or more zones of the implant.26 Acromial stress fractures were identified, confirmed to not have been present before surgery, and classified according to the system described by Levy et al.17 In addition, all cases that required reoperation or revision at a later date were noted.
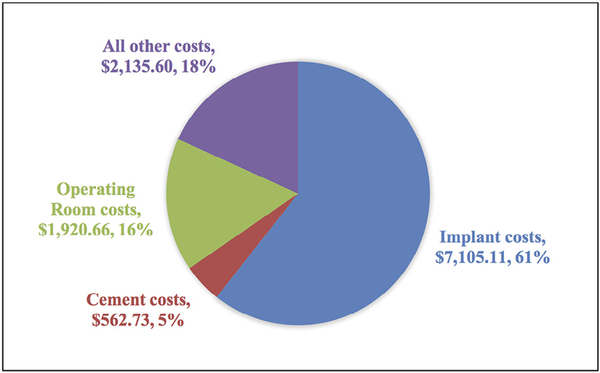
Hospital financial records were used to obtain itemized costs accrued during each hospitalization related to the index shoulder operation. These costs were grouped into the following categories: implant costs, cementing equipment costs, operating room costs, and other costs. The total hospitalization cost was calculated as the sum of all itemized costs during the hospitalization for each patient. Operating room costs were established based on units of time. Cost data were entered into the surgical data repository and queried retrospectively.
The PVI was used to measure value for each patient. The PVI uses the “value equation” proposed by Porter22 and incorporates the MCID into the numerator in an effort to define value as a measure of meaningful improvement. We calculated the PVI as the ratio of mean change in SST score (in units of MCID) over total hospitalization cost. This value was subsequently normalized by multiplying by 104: PVISST/Cost measurement = (Mean ΔMCIDSST × 104)/Mean costTotal hospitalization costs.
The outcome measure at the core of the PVI metric used (SST score) has previously been validated for shoulder arthroplasty.12 The PVI was compared between patients in the cemented and press-fit humeral cohorts. To determine which component of the PVI contributed most significantly to any PVI differences, SST score improvement and cost categories were compared between the groups. Means were compared using independent-samples t tests (Microsoft Excel Analysis ToolPak, version 15; Microsoft, Redmond, WA, USA) with the P value set at .05. We used χ2 analyses for comparisons of proportions (MedCalc Software, Ostend, Belgium). PVI, SST, and cost category data were plotted over time according to date of surgery, and moving averages were shown.
Results
A total of 176 primary RSA patients met the inclusion criteria. The mean follow-up period was 44.6 months (range, 24–113 months). There were 83 patients in the cemented cohort (mean follow-up, 54.0 months; range, 24–113 months) and 93 patients in the press-fit cohort (mean follow-up, 36.3 months; range, 24–78 months). Surgical indications were similar for each group (Table I). Sex, BMI, and preoperative SST scores were not significantly different between groups (Table II).
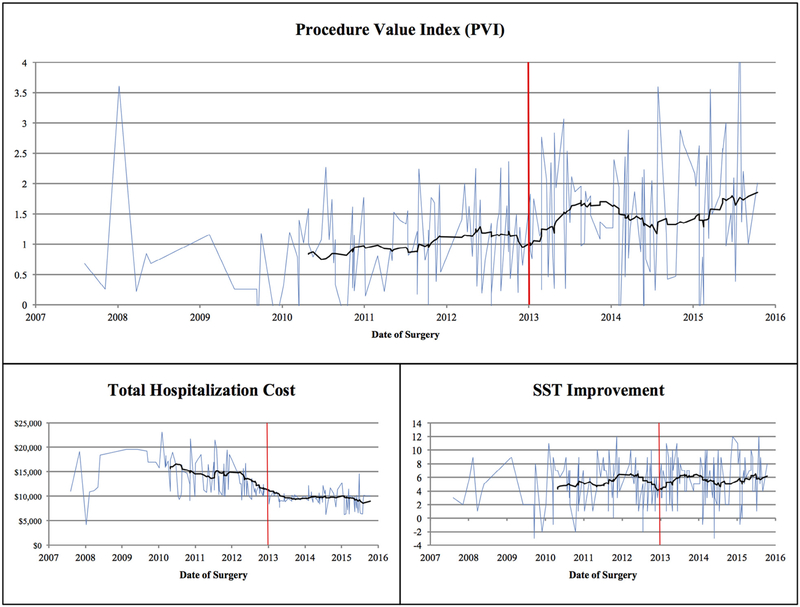
As noted earlier, the press-fit technique for the RSA humeral stem was routinely performed at our institution beginning in 2013. Of the 87 patients in the study who underwent surgery before 2013, 78 (89.7%) were treated with a cemented technique; of the 89 patients who underwent surgery after 2013, 84 (94.4%) were treated with a press-fit technique. Among all patients, implant costs accounted for the largest proportion of total hospitalization costs (60.6%, Fig. 3).
Figure 3.
Mean cost categories per patient shown as a percentage of total costs. RSA, reverse shoulder arthroplasty.
There were 117 patients (66.47%) who reported excellent satisfaction with surgery, with a mean SST score improvement of 6.27. The 52 patients (29.55%) who reported satisfaction as good or satisfactory had a mean SST score improvement of 4.27. The 7 patients (3.98%) who reported unsatisfactory satisfaction had a mean SST score improvement of 0.29. The MCID in the SST score for this population was thus calculated to be 3.98.
The PVI was significantly greater in the press-fit humeral cohort (1.51 vs 1.03, P < .001), representing a 47% difference in average value. Analysis of the components of the PVI showed that SST score improvement (in units of MCID) was not significantly different between the 2 cohorts (P = .23). However, total hospitalization costs were significantly higher for the cemented cohort ($13,601.14 vs $10,048.89, P < .001; Table III).
Table III.
Comparison of PVI, SST score improvement, and total cost for cemented and press-fit cohorts
| PVI | SST score improvement | Total cost | |
|---|---|---|---|
| Cemented | 1.03 | 5.12 | $13,601.14 |
| Press fit | 1.51 | 5.73 | $10,048.89 |
| P value | <.001 | .23 | <.001 |
PVI, procedure value index; SST, Simple Shoulder Test.
Subgroup analysis of the total hospitalization costs showed significant differences in cement and operating room costs (Table IV). Cement and cement-related equipment costs were significantly higher in the cemented cohort ($1075.06 vs $105.49, P < .001). Mean operating room costs (calculated in time units) were significantly lower in the press-fit cohort ($1758.82 vs $2101.99, P = .002). However, there was no significant difference in implant-related costs (P = .127). Moving averages of PVI, SST score improvement, and total hospitalization cost over time are shown in Figure 4.
Table IV.
Mean cost comparison by category for cemented versus press-fit cohorts
| Total cost | Cement costs | Implant costs | Operating room costs | |
|---|---|---|---|---|
| Cemented, $ | 13,601.14 | 1075.06 | 7382.58 | 2101.99 |
| Press fit, $ | 10,048.89 | 105.49 | 6857.48 | 1758.82 |
| P value | <.001 | <.001 | .127 | .002 |
| Cost difference, $ | 3552.25 | 969.57 | 525.09 | 343.16 |
| % of total cost difference | 100.00 | 27.29 | 14.78 | 9.66 |
The percentage of the total cost difference accounted for by each cost category is shown.
Figure 4.
Procedure value index (PVI), Simple Shoulder Test (SST) score improvement, and costs in US dollars plotted over time according to date of surgery. Black lines depict moving averages. Red lines indicate the approximate date of press-fit stem introduction at our institution.
No patients in the cemented cohort or the press-fit cohort were found to have radiographic loosening of the glenoid or humeral components based on review of the most recent post-operative radiographs (mean radiographic follow-up, 41.0 months; range, 3–113 months). Furthermore, there were no cases of humeral stem subsidence. Acromial stress fractures were found in 9 patients in the cemented cohort (type II in 6 and type III in 3) compared with 4 patients in the press-fit cohort (type II in 2 and type III in 2, P = .099). Three patients in the cemented cohort underwent revision at a later date (1 partial revision for acute infection, 1 open reduction and internal fixation for a periprosthetic humeral shaft fracture, and 1 partial revision for recurrent instability), whereas there were no revisions in the press-fit cohort.
Discussion
The introduction of new technology in health care is often met with initial criticism, as the incremental increase in cost is not always justified by an established increase in value. Over time, the added value of the innovation can be appreciated through analysis of the improvements in outcome or reduction in cost. This study is a clear illustration of how value can be enhanced with new technology. With the transition from cemented to press-fit humeral stem fixation, a 47% increase in value was observed, as the PVI for the press-fit cohort (1.51) was significantly greater than that for the cemented cohort (1.03) with no difference in revisions or complications. The enhanced value appears to be related to reduction in overall total hospitalization costs (influenced mostly by cementing equipment and operating room costs) rather than change in clinical outcomes, as the SST score improvement was not significantly different between the study cohorts.
RSA has gained popularity owing to predictability of outcomes and the ability to successfully manage the numerous permutations of the unstable arthritic and rotator cuff– deficient shoulder.6,13,20 Initially, RSA was performed using cemented humeral components because of concerns regarding the impact of rotational forces on the ability of stem ingrowth to occur.
Although the use of cement in other areas of arthroplasty such as hip and knee arthroplasty4,5,7 has a long track record of survivability, unique challenges arise when humeral components are cemented. Revision of well-fixed cemented humeral components can be challenging, as the humeral cortex is often quite thin and fractures are often created during stem extraction, complicating the reconstruction. Furthermore, removal of cement within the humeral canal can be challenging, with several reports of humeral fracture and nerve injury.10 Similar challenges are observed when loosening occurs around a previously cemented implant, as periprosthetic fractures become exponentially more challenging with associated bone loss.1
In addition to the challenges of revision, there are clear costs associated with the cementation process. Included are the costs of the cement, cement restrictor, and cement injection devices and the additional operating room time required for canal preparation and setting of cement. This study showed significantly lower costs for both cement-related equipment and total operating room costs (calculated based on total operating room time) for the press-fit cohort. This is consistent with the study by Wiater et al,30 who noted that RSA performed using uncemented humeral stems was completed 48 minutes faster than RSA using cemented stems. In our study, cement costs represented 27.3% of the overall total cost differences observed between cemented and press-fit procedures. This was greater than the difference in implant cost, which was not found to be significantly different between the 2 groups, likely related to institutional contractual agreements with the implant companies.
The enhanced value of a press-fit technique could quickly be offset by early failures due to early loosening or failure of ingrowth. In this series, there were no cases of gross loosening of any humeral stem in either cohort, and no stem was revised because of aseptic loosening. Several studies have supported the use of press-fit humeral RSA stems with negligible rates of early failures.2,8,30 These findings were supported in this series.
Similarly, a higher infection rate could offset the overall value benefit of a press-fit humeral stem. Nowinski et al21 asserted that use of antibiotic-loaded cement was associated with lower infection rates after primary RSA. Use of a press-fit stem without antibiotic cement could thus be associated with an increased infection rate. Fortunately, this was not observed in our study. One acute infection was observed in the cemented cohort, and no infections were seen in the press-fit cohort.
In our study, no differences in radiographic loosening, revisions, or patient-reported outcomes were observed between the cemented and press-fit cohorts. Although limited, the literature supports this observation. Wiater et al30 found no clinical or radiographic differences between patients treated with RSA using uncemented porous-coated humeral stems and cemented stems. In a multicenter study, Gilot et al8 found no difference in the incidence of humeral loosening in cemented and press-fit humeral RSA stems. King et al16 reported no difference in outcomes or rates of humeral loosening between cemented and uncemented RSA humeral stems.
In contrast, a multicenter long-term follow-up review of Grammont RSA reported higher rates of humeral stem loosening for cemented stems compared with press-fit stems (11.8% vs 5.9%), although clinical outcomes were similar between the groups.19 Humeral stem loosening has further been suggested to be more common in patients with proximal humeral bone deficiency seen in cases of failed hemiarthroplasty for fracture as well as tumor reconstruction.3 With long-term follow-up, biological fixation achieved with modern press-fit humeral stem designs with osseous integration features may prove to be advantageous in avoiding humeral loosening.
There are several key strengths regarding our study. This is the first study to show the “value” of using a press-fit humeral technique during primary RSA. Further analysis was made to determine what specific components contributed to differences in value. Second, all procedures were performed by a single high-volume surgeon; thus, surgical techniques and protocols were well standardized, minimizing differences that could be explained by different techniques or implants. Finally, the press-fit and cemented cohorts were well matched as nearly all surgical indications and preoperative SST scores, sex, and BMI were not significantly different.
A number of potential limitations exist in the conduction of this study. Minor preoperative differences existed between the press-fit and cemented cohorts. There was a statistically significant difference in age but only by a mean of 2 years; therefore, this was not likely to have clinical significance. There were also significant differences in the percentage of patients with failed rotator cuff repair as the surgical indication. However, these patients constituted a small percentage of the total and likely did not affect the overall results. Moreover, changes in cost-reporting methods may have occurred over time and are highly dependent on proper reporting. In addition, cement-related costs for the cemented technique cohort may have been higher because of the use of antibiotic cement in all cases. Although other cement-related costs such as the cement restrictor, gun, and tower helped to drive the $969.57 difference, it is possible that the PVI difference could have been less with the use of standard antibiotic cement. Furthermore, surgeon experience increased over time and may have influenced the speed of surgery and clinical outcomes. This may have contributed to greater value in the press-fit stem group, as nearly all cases after 2013 were performed using a press-fit technique. However, clinical outcomes measured by SST score improvement were not significantly different between groups. Future prospective randomized studies would be beneficial in this regard. In addition, with all cases being performed by a single high-volume surgeon, the results may not be generalizable to low-volume surgeons or institutions. Because the press-fit technique only became routinely used in 2013, the cemented cohort had a longer follow-up. Differences between the 2 cohorts may have been seen with more equal follow-up periods. Finally, with an overall average follow-up period of 45 months, late radiographic failures similar to those observed by Melis et al19 may not have been captured, ultimately influencing long-term value. Longer-term follow-up studies incorporating a larger series of patients may establish differences in outcomes or radiographic observations over time.
Conclusion
Use of a press-fit technique for humeral components in RSA led to a 47% increase in value (measured as the PVI) compared with a cemented technique. This appeared to be a function of decreased total costs rather than increased outcome scores. Decreases in operating room and cement-related costs, rather than implant costs, were larger contributors to decreased overall hospitalization costs for press-fit cases. Humeral stem loosening and revision rates were negligible for both the cemented and press-fit cohorts.
Acknowledgments
The authors thank M. Russell Giveans, PhD, Paul Papagni, JD, Shanell Disla, BS, Elizabeth Hudak, PhD, Sloan Stein, BS, Justin Amato, MS, Gabriel Delgado, Emmanuel McNeely, MS, and Rushabh Vakharia, MD, for their help with the conduction of this study.
Disclaimer
This study was supported by Trinity Health under the Trinity Health Innovation Grant (Series 2).
Jonathan C. Levy is a paid consultant for DJO Orthopaedics and Globus Medical. He receives royalties from DJO Orthopaedics and Innomed. All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
This study was approved by the Western Institutional Review Board (study No. 1153694, Western Institutional Review Board approval No. 20150493) before its conduction.
All work was performed at the Holy Cross Orthopedic Institute and Holy Cross Hospital, Fort Lauderdale, FL.
References
- 1.Andersen JR, Williams CD, Cain R, Mighell M, Frankle M. Surgically treated humeral shaft fractures following shoulder arthroplasty. J Bone Joint Surg Am 2013;95:9–18. 10.2106/JBJS.K.00863 [DOI] [PubMed] [Google Scholar]
- 2.Bogle A, Budge M, Richman A, Miller RJ, Wiater JM, Voloshin I. Radiographic results of fully uncemented trabecular metal reverse shoulder system at 1 and 2 years’ follow-up. J Shoulder Elbow Surg 2013;22:e20–5. 10.1016/j.jse.2012.08.019 [DOI] [PubMed] [Google Scholar]
- 3.Boileau P and Complications revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res 2016;102(Suppl):S33–43. 10.1016/j.otsr.2015.06.031 [DOI] [PubMed] [Google Scholar]
- 4.Coomber R, Porteous M, Hubble MJW, Parker MJ. Total hip replacement for hip fracture: surgical techniques and concepts. Injury 2016;47:2060–4. 10.1016/j.injury.2016.06.034 [DOI] [PubMed] [Google Scholar]
- 5.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review . PLoS One 2010;5:e13520 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res 2010;468:1526–33. 10.1007/s11999-009-1188-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandhi R, Tsvetkov D, Davey JR, Mahomed NN. Survival and clinical function of cemented and uncemented prostheses in total knee replacement: a meta-analysis. J Bone Joint Surg Br 2009;91:889–95. 10.1302/0301-620X.91B7.21702 [DOI] [PubMed] [Google Scholar]
- 8.Gilot G, Alvarez-Pinzon AM, Wright TW, Flurin PH, Krill M, Routman HD, et al. The incidence of radiographic aseptic loosening of the humeral component in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2015;24:1555–9. 10.1016/j.jse.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 9.Giuseffi SA, Streubel P, Sperling J, Sanchez-Sotelo J. Short-stem uncemented primary reverse shoulder arthroplasty: clinical and radiological outcomes. Bone Joint J 2014;96-B:526–9. 10.1302/0301-620X.96B3.32702 [DOI] [PubMed] [Google Scholar]
- 10.Goldberg SH, Cohen MS, Young M, Bradnock B. Thermal tissue damage caused by ultrasonic cement removal from the humerus. J Bone Joint Surg Am 2005;87:583–91. 10.2106/JBJS.D.01966 [DOI] [PubMed] [Google Scholar]
- 11.Harmsen SM, Norris TR. Radiographic changes and clinical outcomes associated with an adjustable diaphyseal press-fit humeral stem in primary reverse shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:1589–97. http://dx.doi.org/S1058-2746(17)30113-1 [DOI] [PubMed] [Google Scholar]
- 12.Hsu JE, Russ SM, Somerson JS, Tang A, Warme WJ, Matsen FA III Is the Simple Shoulder Test a valid outcome instrument for shoulder arthroplasty? J Shoulder Elbow Surg 2017;26:1693–700. http://dx.doi.org/S1058-2746(17)30209-4 [DOI] [PubMed] [Google Scholar]
- 13.Hyun YS, Huri G, Garbis NG, McFarland EG. Uncommon indications for reverse total shoulder arthroplasty. Clin Orthop Surg 2013;5:243–55. 10.4055/cios.2013.5.4.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keener JD, Chalmers PN, Yamaguchi K. The humeral implant in shoulder arthroplasty. J Am Acad Orthop Surg 2017;25:427–38. 10.5435/JAAOS-D-15-00682 [DOI] [PubMed] [Google Scholar]
- 15.Kiet TK, Feeley BT, Naimark M, Gajiu T, Hall SL, Chung TT, et al. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg 2015;24:179–85. 10.1016/j.jse.2014.06.039 [DOI] [PubMed] [Google Scholar]
- 16.King JJ, Farmer KW, Struk AM, Wright TW. Uncemented versus cemented humeral stem fixation in reverse shoulder arthroplasty. Int Orthop 2015;39:291–8. 10.1007/s00264-014-2593-6 [DOI] [PubMed] [Google Scholar]
- 17.Levy JC, Anderson C, Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am 2013;95:e104 10.2106/JBJS.K.01516 [DOI] [PubMed] [Google Scholar]
- 18.Matsen FA III, Iannotti JP, Rockwood CA Jr. Humeral fixation by press-fitting of a tapered metaphyseal stem: a prospective radiographic study. J Bone Joint Surg Am 2003;85:304–8. [DOI] [PubMed] [Google Scholar]
- 19.Melis B, DeFranco M, Ladermann A, Mole D, Favard L, Nerot C, et al. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br 2011;93:1240–6. 10.1302/0301620X.93B9.25926 [DOI] [PubMed] [Google Scholar]
- 20.Mizuno N, Denard PJ, Raiss P, Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am 2013;95:1297–304. 10.2106/JBJS.L.00820 [DOI] [PubMed] [Google Scholar]
- 21.Nowinski RJ, Gillespie RJ, Shishani Y, Cohen B, Walch G, Gobezie R. Antibiotic-loaded bone cement reduces deep infection rates for primary reverse total shoulder arthroplasty: a retrospective, cohort study of 501 shoulders. J Shoulder Elbow Surg 2012;21:324–8. 10.1016/j.jse.2011.08.072 [DOI] [PubMed] [Google Scholar]
- 22.Porter ME. What is value in health care? N Engl J Med 2010;363:247781 10.1056/NEJMp1011024 [DOI] [PubMed] [Google Scholar]
- 23.Ross M, Hope B, Stokes A, Peters SE, McLeod I, Duke PF. Reverse shoulder arthroplasty for the treatment of three-part and four-part proximal humeral fractures in the elderly. J Shoulder Elbow Surg 2015;24:215–22. 10.1016/j.jse.2014.05.022 [DOI] [PubMed] [Google Scholar]
- 24.Samitier G, Alentorn-Geli E, Torrens C, Wright TW. Reverse shoulder arthroplasty. Part 1: systematic review of clinical and functional outcomes. Int J Shoulder Surg 2015;9:24–31. 10.4103/09736042.150226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2015;24:91–7. 10.1016/j.jse.2014.08.026 [DOI] [PubMed] [Google Scholar]
- 26.Sperling JW, Cofield RH, O’Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg 2000;9:507–13. [DOI] [PubMed] [Google Scholar]
- 27.Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, et al. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:144–8. http://dx.doi.org/S10582746(16)30191-4 [DOI] [PubMed] [Google Scholar]
- 28.Verborgt O, El-Abiad R, Gazielly DF. Long-term results of uncemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg 2007;16(Suppl):S13–8. http://dx.doi.org/S1058-2746(06)00091-7 [DOI] [PubMed] [Google Scholar]
- 29.Westermann RW, Pugely AJ, Martin CT, Gao Y, Wolf BR, Hettrich CM. Reverse shoulder arthroplasty in the United States: a comparison of national volume, patient demographics, complications, and surgical indications. Iowa Orthop J 2015;35:1–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Wiater JM, Moravek JE Jr, Budge MD, Koueiter DM, Marcantonio D, Wiater BP. Clinical and radiographic results of cementless reverse total shoulder arthroplasty: a comparative study with 2 to 5 years of follow-up. J Shoulder Elbow Surg 2014;23:1208–14. 10.1016/j.jse.2013.11.032 [DOI] [PubMed] [Google Scholar]
- 31.Youn SM, Deo S, Poon PC. Functional and radiologic outcomes of uncemented reverse shoulder arthroplasty in proximal humeral fractures: cementing the humeral component is not necessary. J Shoulder Elbow Surg 2016;25:e83–9. 10.1016/j.jse.2015.09.007 [DOI] [PubMed] [Google Scholar]