Abstract
BACKGROUND:
Overall, cervical cancer survival in the United States has been reported to be among the highest in the world, despite slight decreases over the last decade. Objective of the current study was to describe cervical cancer survival trends among US women and examine differences by race and stage.
METHODS:
This study used data from the CONCORD-2 study to compare survival among women (aged 15–99 years) diagnosed in 37 states covering 80% of the US population. Survival was adjusted for background mortality (net survival) with state- and race-specific life tables and was age-standardized with the International Cancer Survival Standard weights. Five-year survival was compared by race (all races, blacks, and whites). Two time periods, 2001–2003 and 2004–2009, were considered because of changes in how the staging variable was collected.
RESULTS:
From 2001 to 2009, 90,620 women were diagnosed with invasive cervical cancer. The proportion of cancers diagnosed at a regional or distant stage increased over time in most states. Overall, the 5-year survival was 63.5% in 2001–2003 and 62.8% in 2004–2009. The survival was lower for black women versus white women in both calendar periods and in most states; black women had a higher proportion of distant-stage cancers.
CONCLUSIONS:
The stability of the overall survival over time and the persistent differences in survival between white and black women in all US states suggest that there is a need for targeted interventions and improved access to screening, timely treatment, and follow-up care, especially among black women. Cancer 2017;123:5119–37. Published 2017. This article is a U.S. Government work and is in the public domain in the USA.
Keywords: cervical neoplasms, population-based survival, prevention and control, trends
INTRODUCTION
Cervical cancer screening has resulted in well-documented declines in incidence and mortality in the United States.1 Despite evidence showing that screening is effective in preventing invasive cervical cancer and cervical cancer death, many women are not screened as recommended; this is especially true for women in populations with limited access to preventive health services and a usual source of care.2 More than half of all new cervical cancer cases are estimated to occur in women who have never or rarely been screened.3 One recent study of cervical cancer in a sample of the US population noted improvements in survival from 1983 through 2009 among women diagnosed at earlier stages, but there were no improvements in survival for patients with metastatic disease.4 Disparities by race/ethnicity include higher incidence and mortality rates among Hispanic and black women and poorer survival among black women versus white women.5 Population-based surveillance of cervical cancer survival trends by race and stage can provide insights into racial and geographic disparities that can be used to target cancer control efforts.
The CONCORD-2 study established worldwide cancer survival rates for 10 common cancers and produced estimates of 5-year survival for more than 25 million patients in 67 countries and 279 cancer registries from 1995 to 2009.6 Globally, the 5-year net survival for cervical cancer varied from less than 40% to more than 70%.6 CONCORD-2 reported a slight decrease in the 5-year net survival for cervical cancer in the United States (from 64.2% in 1995–1999 to 62.8% in 2005–2009). Similar patterns were observed in other high-income countries. Disparities in cervical cancer survival, such as those seen between countries, represent profound health inequities because invasive cervical cancer is both potentially preventable and treatable if it is detected early with screening and this is followed by appropriate care. The current study used the US data from CONCORD-2, which included the most comprehensive and up-to-date population-based data and covered 80% of the US population. Survival was analyzed by race, stage, and geographical area.
MATERIALS AND METHODS
Data Source
We used data from 37 statewide cancer registries funded by Center for Disease Control (CDC) National Program of Cancer Registry (NPCR) and National Cancer Institute Surveillance, Epidemiology, and End Results Summary (SEER) that participated in the CONCORD-2 study which covered 80% of the US population.6,7 The registries consented to the inclusion of their data in the more detailed analyses reported here. More details on the data and methods are provided in the accompanying article by Allemani et al.8 We analyzed individual tumor records for 90,620 women (aged 15–99 years) who were diagnosed with primary, invasive cancer of the cervix (International Classification of Diseases for Oncology, 3rd edition, codes C530-C531 and C538-C5399) from 2001 to 2009 and were followed through December 31, 2009. If a woman was diagnosed with 2 or more cancers of the cervix during the same time period, only the first was considered in the survival analyses.
The stage at diagnosis was defined according to the SEER Summary Stage 2000 (SS2000) and was categorized as localized, regional, distant, or unknown. Women were grouped by the year of diagnosis into 2 calendar periods (2001–2003 and 2004–2009) to reflect changes in the methods used by US registries to collect data on the stage at diagnosis beginning in 2004. From 2001 to 2003, most registries coded SS2000 directly from the medical records.10 From 2004 to 2009, registries derived SS2000 with the Collaborative Staging System.11
Survival Analyses
We estimated the net survival by state, race (all, blacks, and whites), SS2000 (local, regional, distant, and unknown), and calendar period of diagnosis. The net survival is the probability of survival up to a given time after the diagnosis after controlling for other causes of death (background mortality). To control for wide differences in background mortality among participating states, we constructed life tables of all-cause mortality in the general population of each state from the number of deaths and the population by single year of age, sex, calendar year, and, where possible, race (black vs white).8
These life tables have been published elsewhere.12 We estimated net survival up to 5 years after diagnosis and 95% confidence intervals with the Pohar Perme estimator.13
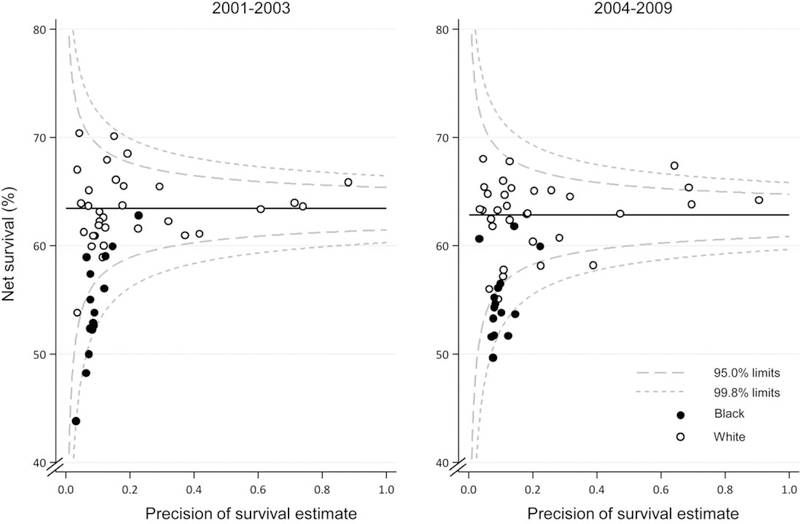
We estimated the net survival with the cohort approach for patients diagnosed from 2001 to 2003 because all the patients had been followed up for at least 5 years by December 31, 2009. We used the complete approach to estimate the net survival for patients diagnosed from 2004 to 2009 because 5 years of follow-up data was not available for all patients. Net survival was estimated for 5 age groups (15–44, 45–54, 55–64, 65–74, and 75–99 years). We obtained age-standardized survival estimates with the International Cancer Survival Standard weights.14 If 2 or more of the 5 age-specific estimates could not be obtained, we present only the pooled, unstandardized survival estimate for all ages combined. Trends, geographic variations, and differences in age-standardized survival by race are presented graphically in bar charts and funnel plots.15 Funnel plots of net survival for 2001–2003 and 2004–2009 provide insight into the variability of cancer survival in the United States by race and state and show how much a particular survival estimate deviates from the pooled estimate of US registries (horizontal line) given the precision of each estimate.
RESULTS
For 2001–2003, 48.8% of cervical cancers were diagnosed at a localized stage, 31.8% were diagnosed at a regional stage, and 9.6% were diagnosed at a distant stage. The proportion of cancers at the localized stage fell by 4% for 2004–2009 but increased for cancers at regional (35.5%) and distant stages (11.5%). The proportion at an unknown stage decreased from 9.8% to 8.4% (Table 1). The proportion of cervical cancers diagnosed at a local stage was 10% lower for black women versus white women, and this difference did not change over time (40.9% vs 50.4% for 2001–2003 and 36.6% vs 46.2% for 2004–2009). In comparison, higher proportions of cancers were diagnosed at regional (35.6% vs 31.2% for 2001–2003 and 38.6% vs 35.0% for 2004–2009) and distant stages (11.0% vs 9.4% for 2001–2003 and 13.5% vs 11.3% for 2004–2009).
TABLE 1.
Cervix Cancer: Number of Females (15–99 Years Old) Diagnosed in 2001–2009 and Distribution by SEER Summary Stage 2000 at Diagnosis, Race, and Calendar Period of Diagnosis
| Summary Stage 2000 | 2001–2003 |
2004–2009 |
||||
|---|---|---|---|---|---|---|
| All Races | Whites | Blacks | All Races | Whites | Blacks | |
| No. of patients | 30,357 | 23,547 | 4882 | 60,263 | 46,563 | 9576 |
| Localized, % | 48.8 | 50.4 | 40.9 | 44.7 | 46.2 | 36.6 |
| Regional, % | 31.8 | 31.2 | 35.6 | 35.5 | 35.0 | 38.6 |
| Distant, % | 9.6 | 9.4 | 11.0 | 11.5 | 11.3 | 13.5 |
| Unknown, % | 9.8 | 9.0 | 12.5 | 8.4 | 7.5 | 11.3 |
Abbreviation: SEER, Surveillance, Epidemiology, and End Results.
For all women diagnosed with cervical cancer, the 1-, 3-, and 5-year net survival estimates are presented in Table 2 by race and calendar period. The 1- and 5-year net survival were 83.4% and 63.5%, respectively, for 2001–2003 and 82.9% and 62.8%, respectively, for 2004–2009. Net survival was lower among black women than white women overall and in the majority of the US states (Table 2 and Supporting Table 1). Among women diagnosed between 2004–2009, the 1-year survival was 3.5% lower for black women than white women, and the survival was 8.0% lower at 5 years.
TABLE 2.
Cervix Cancer: 5-Year Age-Standardized NS for Females (15–99 Years Old) Diagnosed in 2001–2009 by SEER Summary Stage at Diagnosis, Race, and Calendar Period of Diagnosis
| Summary Stage 2000 | 2001–2003 |
2004–2009 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Races |
Whites |
Blacks |
All Races |
Whites |
Blacks |
|||||||
| NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | |
| All stages | 63.5 | 62.8–64.1 | 64.0 | 63.2–64.7 | 56.6 | 55.0–58.2 | 62.8 | 62.2–63.5 | 63.5 | 62.7–64.2 | 55.5 | 53.9–57.1 |
| Localized | 84.5 | 83.4–85.5 | 84.9 | 83.7–86.0 | 79.1 | 76.4–81.7 | 85.9 | 84.7–87.0 | 86.6 | 85.3–87.9 | 79.2 | 76.4–82.1 |
| Regional | 53.2 | 52.1–54.3 | 53.6 | 52.4–54.9 | 47.4 | 44.7–50.1 | 55.8 | 54.8–56.9 | 56.1 | 54.9–57.3 | 51.1 | 48.4–53.7 |
| Distant | 16.0 | 14.6–17.4 | 16.3 | 14.7–17.9 | 13.4 | 10.4–16.4 | 16.3 | 15.0–17.6 | 16.6 | 15.1–18.2 | 14.4 | 11.8–17.0 |
| Unknown | 58.3 | 56.3–60.3 | 58.1 | 55.8–60.4 | 52.3 | 47.9–56.7 | 56.2 | 54.3–58.2 | 56.6 | 54.3–58.9 | 49.0 | 44.9–53.2 |
Abbreviations: CI, confidence interval; NS, net survival; SEER, Surveillance, Epidemiology, and End Results.
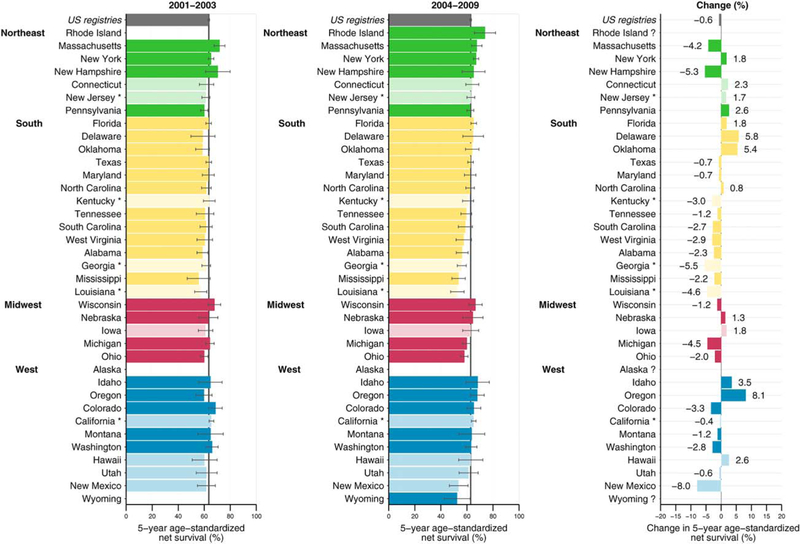
Figure 1 depicts the 5-year net survival among states grouped by US Census region. The survival ranged from 55.7% to 71.8% for 2001–2003 and from 52.5% to 73.9% for 2004–2009 (Fig. 1 and Supporting Table 1). Survival decreased in 22 states and increased in 13 states. In the southern US Census region, 12 of 14 states in 2001–2003 and 10 of 14 states in 2004–2009 showed a 5-year net survival lower than the US value.
Figure 1.
Five-year age-standardized net survival for females (15–99 years old) diagnosed between 2001–2003 and 2004–2009 and absolute changes. The states are grouped by US Census region. States are ranked within the US Census region by the survival estimate for 2004–2009. Dark colors denote states affiliated with the National Program of Cancer Registries; pale colors denote states affiliated with the Surveillance, Epidemiology, and End Results Program; and an asterisk denotes registries affiliated with both federal surveillance programs. Changes were not plotted if at least 1 calendar period estimate was not age-standardized.
Figure 2 presents funnel plots of net survival for 2001–2003 and 2004–2009 to provide further insight into the variability of cervical cancer survival in the United States by race and state. These plots show striking racial and geographical variations in survival. Five-year survival with cervical cancer was lower for black women than white women in most states in both 2001–2003 and 2004–2009. In all 15 states for which a survival estimate could be obtained for black women, survival was systematically lower than the US value.
Figure 2.
Cervical cancer: 5-year age-standardized net survival for females (15–99 years old) by state (circles), race, and calendar period of diagnosis. The pooled (US) survival estimates for each calendar period are shown by the horizontal (solid) line with corresponding 95.0% and 99.8% control limits (dotted lines).
Table 2 provides the 5-year net survival by stage, race, and calendar year. There was a slight increase observed for women diagnosed with a localized (from 84.5% to 85.9%) or regional cancer (from 53.2% to 55.8%). Survival for women diagnosed with a distant cervical cancer remained constant (Table 2). Survival trends were similar for white women in the 2 time periods. Survival for black women was steady for cancers diagnosed at a localized stage (from 79.1% to 79.2%) and increased slightly for cancers diagnosed at regional (from 47.4% to 51.1%) and distant stages (from 13.4% to 14.4%). However, black women had lower survival than white women for all stages and in both time periods (Table 3 and Fig. 2). Substantial variations in 5-year net survival by stage were observed among states and regions over time (Supporting Tables 2 and 3). For 2004–2009, the 5-year survival range was 69.3% to 97.1% for localized-stage cancers, 38.9% to 68.3% for regional-stage cancers, and 8.1% to 25.7% for distant-stage cancers (Supporting Table 1).
TABLE 3.
Cervix Cancer: Age-Standardized NS at 1, 3, and 5 Years for Females (15–99 Years Old) Diagnosed in 2001–2009 by Race and Calendar Period of Diagnosis
| 2001–2003 |
2004–2009 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Races |
Whites |
Blacks |
All Races |
Whites |
Blacks |
|||||||
| Years | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI |
| 1 | 83.4 | 82.9–83.9 | 83.8 | 83.3–84.4 | 79.0 | 77.7–80.2 | 82.9 | 82.5–83.3 | 83.0 | 82.6–83.5 | 79.5 | 78.6–80.5 |
| 3 | 68.7 | 68.0–69.3 | 69.2 | 68.5–69.9 | 61.8 | 60.2–63.3 | 68.0 | 67.5–68.5 | 68.7 | 68.1–69.3 | 60.9 | 59.6–62.1 |
| 5 | 63.5 | 62.8–64.1 | 64.0 | 63.2–64.7 | 56.6 | 55.0–58.2 | 62.8 | 62.2–63.5 | 63.5 | 62.7–64.2 | 55.5 | 53.9–57.1 |
Abbreviations: CI, confidence interval; NS, net survival.
DISCUSSION
The cervical cancer survival in the United States remained stable between 2001 to 2009 at approximately 63%. We documented persistent racial and geographical disparities with lower 5-year survival (55.5%) in 2004–2009 and proportionately more later stage cancers for black women versus white women.
Slight decreases6 or no changes in survival occurred despite decreasing incidence and death rates1,2 related to longstanding screening activities within the population. Cervical cancer screening mostly detects pre-invasive cervical cancers, and follow-up treatment of abnormal cells can prevent invasive cancers that otherwise would arise. As such, a decreasing incidence of cervical cancer can be used as a marker for effective screening because most cervical cancers are preventable with early detection and appropriate follow-up of pre-invasive lesions.16 Because most women with access to health services are screened and malignant lesions are removed before they become invasive, the incidence of invasive cervical cancer may become skewed toward cases arising in the unscreened population,3 interval cancers with a faster doubling time and thus a shorter sojourn time in the preclinical detectable phase, and those with a lack of adequate follow-up.17 This results in an increase in the proportion of women diagnosed at regional and distant stages and thus in a decrease in survival for all women with cervical cancer combined, as found in this study. In addition, as reported in this study and elsewhere, black women have higher incidence and mortality rates and lower survival than white women.4 As we noted, lower stage-specific survival and higher proportions of later stage cancers among black women contribute to these disparities.
Clinical Implications
Significant advances in cervical cancer prevention, screening, and treatment have occurred in the past decade. In the area of primary prevention, the first human papillomavirus (HPV) vaccine was approved for use in the United States in 2006.18 Both the quadrivalent and bivalent HPV vaccines target infections from 2 oncogenic types, HPV-16 and HPV-18, which are responsible for 66% of cervical cancers.19 In 2014, the 9-valent vaccine, which includes 5 additional oncogenic types, was approved for use, and it can potentially prevent an additional 14% of cervical cancers.20 HPV vaccines have the potential to lower the risk for a woman to ever develop and subsequently die of cervical cancer.21 However, the coverage in the United States in 2015 was less than optimal, with only approximately 62% of girls aged 13 to 17 years receiving at least 1 dose.22 Screening programs remain imperative for preventing cervical cancer as we move into an era of more HPV vaccine coverage.
During the past decade, several improvements, including a gradual paradigm shift from cytology-based screening to HPV-based screening, have also made in cervical cancer screening; this shift means greater sensitivity and the potential for less frequent screening.23 HPV-based screening has the potential to detect abnormal cervical lesions at an earlier stage, ideally before invasion. Significant developments in treatment (the addition of chemotherapy to radiation therapy for cervical cancer as a standard of treatment in the late 1990s, fertility-sparing surgery for early-stage disease, and the addition of bevacizumab for advanced or recurrent disease) can result in improved survival and better quality of life.24 Timely access to optimal treatment is important for increasing the chances of survival; these factors go beyond the treatment itself to address system and access barriers.25
Cancer Control Implications
Population-based survival trends are crucial for developing and prioritizing cancer control strategies and evaluating the impact of cancer control activities and progress toward meeting national objectives. Using surveillance data to plan interventions is one activity that the National Comprehensive Cancer Control Program of the Centers for Disease Control and Prevention is strongly encouraged to complete on a routine basis.7 These cancer control plans include using information about the region’s cancer burden to inform goals and potential activities for improving primary cancer prevention, such as increasing HPV vaccination, cervical cancer screening, and cervical cancer survival in the community. In addition, direct clinical services have been provided by the CDC’s National Breast and Cervical Cancer Early Detection Program for cervical cancer screening to low-income, uninsured, and underinsured women.7 Women diagnosed with cancer through this program are eligible for Medicaid coverage to cover treatment costs and other health care–related needs.26 This program reaches approximately 7% of all eligible women across the United States27 and has shown reductions in mortality from cervical cancer among low-income women.28
Many of these CDC programs have worked collaboratively to reach women in underserved populations. These collaborations have included 1) working with federally qualified health centers to monitor and increase cervical cancer screening utilization; 2) developing culturally competent action plans to reach African American, American Indian, and Latino women; 3) conducting group educational sessions and outreach; and 4) using community health workers or patient navigators to provide education and entry into screening (J. S. Town-send, MS, written communication, April, 2016). The CDC also funds national networks that serve racial/ethnic minorities, people living with mental illness and addictions, and rural residents to address cancer-related health disparities.29 One network is addressing the high cervical cancer incidence rates among Hispanic and Latina women by providing technical assistance on evidence-based programs to increase screening and vaccination rates.30 However, even with these comprehensive interventions, women continue to develop this largely preventable disease, and health disparities exist. The CDC is leading a national study to understand the barriers to timely screening and follow-up to help to understand these persistent disparities; study findings will be in the literature early next year.
Strengths and Limitations
This study of cervical cancer survival, which included high-quality data from 37 states covering 80% of the population in the United States, is the most comprehensive study of population-based cancer survival in the United States to date. We have also documented racial disparities in the stage at diagnosis and 5-year survival and highlighted areas for future public health interventions to achieve health equity. Net survival was estimated with state- and race-specific life tables. However, we were able to construct only white- and black-specific life tables and, therefore, were not able to report data for other races or ethnic groups. In addition, unusually high survival in some areas may have resulted from incorrect vital status information due to data quality variations related to data linkages.31
In conclusion, although cervical cancer survival has been relatively stable over time and this reflects improvements in screening,32 racial and geographical disparities in survival still exist. By understanding the status of cervical cancer survival and the opportunities available for continuing to decrease the incidence and improve survival, CDC programs are working to determine the most effective ways to close the gaps and ensure that all women benefit from the latest advances in cervical cancer prevention, early diagnosis, and timely treatment.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the CDC.
FUNDING SUPPORT
Funding for Rhea Harewood and Claudia Allemani is supported by US Centers for Disease Control and Prevention (CDC; 12FED03123, ACO12036).
Footnotes
This Supplement edition of Cancer has been sponsored by the U.S. Centers for Disease Control and Prevention (CDC), an Agency of the Department of Health and Human Services.
The CONCORD-2 study was approved by the Ethics and Confidentiality Committee of the UK’s statutory National Information Governance Board (now the Health Research Authority) (ref ECC 3–04(i)/2011) and by the National Health Service Research Ethics Service (Southeast; 11/LO/0331).
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2012 http://seer.cancer.gov/csr/1975_2012. [Google Scholar]
- 2.Benard VB, Thomas CC, King J, Massetti GM, Doria-Rose VP, Saraiya M. Vital signs: cervical cancer incidence, mortality, and screening—United States, 2007–2012. MMWR Morb Mortal Wkly Rep 2014;63:1004–1009. [PMC free article] [PubMed] [Google Scholar]
- 3.Leyden WA, Manos MM, Geiger AM, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst 2005;97:675–683. [DOI] [PubMed] [Google Scholar]
- 4.Wright JD, Chen L, Tergas AI, et al. Population-level trends in relative survival for cervical cancer. Am J Obstet Gynecol 2015;213: 670.e1–670.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheppard CS, El-Zein M, Ramanakumar AV, Ferenczy A, Franco EL. Assessment of mediators of racial disparities in cervical cancer survival in the United States. Int J Cancer 2016;138:2622–2630. [DOI] [PubMed] [Google Scholar]
- 6.Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 2015;385:977–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White MC, Babcock F, Hayes NS, et al. The history and use of cancer registry data by public health cancer control programs in the United States. Cancer 2017;123:4969–4976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allemani C, Harewood R, Johnson C, et al. Population-based cancer survival in the United States: data, quality control, and statistical methods. Cancer 2017;123:4982–4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fritz AG, Percy C, Jack A. International Classification of Disease Oncology (ICD-0) Geneva, Switzerland: World Health Organiza-tion; 2000. [Google Scholar]
- 10.Young JL, Roffers SD, Ries LAD, Fritz AG, Hurlbut AA. SEER Summary Staging Manual–2000: Codes and Coding Instructions Bethesda, MD: National Cancer Institute; 2001. [Google Scholar]
- 11.Surveillance, Epidemiology, and End Results Program. Collaborative stage http://seer.cancer.gov/tools/collabstaging. Accessed April, 2016.
- 12.Spika D, Bannon F, Bonaventure A, et al. Life tables for global surveillance of cancer survival (the CONCORD programme): data sources and methods. BMC Cancer 2017;17:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perme MP, Stare J, Esteve J. On estimation in relative survival. Bio-metrics 2012;68:113–120. [DOI] [PubMed] [Google Scholar]
- 14.Corazziari I, Quinn M, Capocaccia R. Standard cancer patient population for age standardising survival ratios. Eur J Cancer 2004;40: 2307–2316. [DOI] [PubMed] [Google Scholar]
- 15.Quaresma M, Coleman MP, Rachet B. Funnel plots for population-based cancer survival: principles, methods and applications. Stat Med 2014;33:1070–1080. [DOI] [PubMed] [Google Scholar]
- 16.Moyer VA. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;156: 880–891. [DOI] [PubMed] [Google Scholar]
- 17.Benard VB, Eheman CR, Lawson HW, et al. Cervical screening in the National Breast and Cervical Cancer Early Detection Program, 1995–2001. Obstet Gynecol 2004;103:564–571. [DOI] [PubMed] [Google Scholar]
- 18.Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2014;63: 1–30. [PubMed] [Google Scholar]
- 19.Saraiya M, Unger ER, Thompson TD, et al. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. J Natl Cancer Inst 2015;107: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petrosky E, Bocchini JA Jr, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep 2015;64:300–304. [PMC free article] [PubMed] [Google Scholar]
- 21.Burger EA, Lee K, Saraiya M, et al. Racial and ethnic disparities in human papillomavirus–associated cancer burden with first-generation and second-generation human papillomavirus vaccines. Cancer 2016;122:2057–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR Morb Mortal Wkly Rep 2016;65:850–858. [DOI] [PubMed] [Google Scholar]
- 23.Saraiya M, Watson M, Benard VB. Cervical cancer screening measures need to evolve to continue to tell the story. J Womens Health (Larchmt) 2012;21:1128–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pfaendler KS, Tewari KS. Changing paradigms in the systemic treatment of advanced cervical cancer. Am J Obstet Gynecol 2016;214: 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramondetta LM, Meyer LA, Schmeler KM, et al. Avoidable tragedies: disparities in healthcare access among medically underserved women diagnosed with cervical cancer. Gynecol Oncol 2015;139: 500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lantz PM, Mullen J. The National Breast and Cervical Cancer Early Detection Program: 25 years of public health service to low-income women. Cancer Causes Control 2015;26:653–656. [DOI] [PubMed] [Google Scholar]
- 27.Tangka FK, Howard DH, Royalty J, et al. Cervical cancer screening of underserved women in the United States: results from the National Breast and Cervical Cancer Early Detection Program, 1997–2012. Cancer Causes Control 2015;26:671–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ekwueme DU, Uzunangelov VJ, Hoerger TJ, et al. Impact of the National Breast and Cervical Cancer Early Detection Program on cervical cancer mortality among uninsured low-income women in the U.S., 1991–2007. Am J Prev Med 2014;47:300–308. [DOI] [PubMed] [Google Scholar]
- 29.National Comprehensive Cancer Control Program. Consortium of national networks to impact tobacco-related and cancer health disparities http://www.cdc.gov/cancer/ncccp/dp13-1314.htm. Accessed April, 2016.
- 30.Nuestras Voces. http://www.nuestrasvoces.org/. Accessed April, 2016.
- 31.Weir HK, Stewart S, Allemani C, et al. Population-based cancer survival (2001–2009) in the United States: findings from the CONCORD-2 study. Cancer 2017;123:4963–4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cho H, Mariotto AB, Schwartz LM, Luo J, Woloshin S. When do changes in cancer survival mean progress? The insight from population incidence and mortality. J Natl Cancer Inst Monogr 2014;2014: 187–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.