Abstract
BACKGROUND:
Mindfulness training is often used as a therapeutic intervention to manage stress and enhance emotional wellbeing, yet trials for MS are limited and few have used an active control.
OBJECTIVE:
Assess the feasibility of mindfulness-based stress reduction (MBSR) for people with MS and evaluate efficacy of MBSR compared to an education control.
METHODS:
We conducted a single-blind, randomized trial of MBSR vs. education control among 62 adults with MS. Primary outcomes were measures of feasibility. Secondary outcomes included perceived stress, anxiety, depression, fatigue, pain, resilience, and the Paced Auditory Serial Addition Test, assessed at baseline, 8 weeks, and 12 months. Mean scores for secondary outcome measures were compared between groups at each time point and within groups across time by analyses of covariance or paired t-tests, respectively.
RESULTS:
Successful recruitment and retention demonstrated feasibility. Improvements in several secondary outcomes were observed among both MBSR and control groups. However, differences between the groups were not statistically significant at either 8 weeks or 12 months.
CONCLUSION:
Emotional wellbeing improved with both MBSR and education. Spontaneous improvement cannot be ruled out as an explanation for findings and additional studies that evaluate the impact of mindfulness training to improve emotional health are warranted.
Keywords: Multiple sclerosis, quality of life, psychological stress, anxiety, mindfulness, resilience
INTRODUCTION
Psychological stress has a negative impact on the MS disease process. Stressful life events significantly increase the risk of MS exacerbation (1,2), and stress-management has been shown to reduce the risk of new lesion development on MRI (3). In addition to preceding physical symptoms, stress often precipitates mood disorders, of which people with MS are more prone. Compared to the general US population, people with MS have a higher lifetime prevalence of anxiety disorders (36% vs. 29%) and depression (36–54% vs. 16%)(4). Adverse consequences of mood disorders among people with MS include reduced functioning and quality of life, decreased treatment adherence, and increased risk of suicide (4). Thus, psychological stress and emotional wellbeing are important targets for MS research and clinical care.
Mindfulness training is increasingly used as a therapeutic intervention to manage stress and enhance emotional wellbeing. Mindfulness is defined as the capactity to notice one’s thoughts, emotions, and bodily sensations without engaging in physical or emotional reactivity to these experiences (5). The practice of distinguishing between experience (what one notices) and the response to experience (e.g. judgment, negative affect) helps participants identify and mitigate habitual reactions that contribute to emotional distress (5). Mindfulness-based interventions have shown benefit for a variety of symptoms associated with MS (anxiety, depression, pain, fatigue, physical function)(6,7); but their use with MS populations has been limited. Of the mindfulness-based intervention studies that have been conducted in MS, all have suggested the potential for improvements in emotional wellbeing, including anxiety, depression, stress, and mental health quality of life (8–15). However, to date, only one trial has used an active control and was conducted with MS patients with depression; Carletto et al. and showed that the mindfulness intervention was associated with reduced Beck Depression Scores at 6 months (16). Studies not limited to those with depression and with longer follow-up time to evaluate sustainability of outcomes are needed.
We conducted a single-blind, randomized, parallel group intervention of a well-studied mindfulness-based stress reduction (MBSR) program for adults with any type of MS and expanded disability status scale (EDSS) score ≤ 8.0. Our objectives were to assess 1) feasibility for a future trial, and 2) preliminary clinical efficacy of MBSR compared to a control intervention matched for class time and attention from a facilitator (time-and-attention control). We hypothesized that participants randomized to MBSR would show greater improvement in perceived stress and emotional wellbeing compared to an education control. Additional secondary outcome measures reflect some of the most commonly reported symptoms among people with MS, including anxiety, depression, pain, fatigue, and challenges in cognitive processing.
METHODS
Study Sample
Participants were recruited from the Portland, Oregon metropolitan area through advertisements with the National MS Society, mailers to patients of Oregon Health & Science University (OHSU), and during outpatient visits to the MS Center at OHSU. Inclusion criteria comprised adults ≥ 18 years of age with any type of MS; an Expanded Disability Status Scale (EDSS) score ≤ 8.0; stable on disease modifying therapies, anxiolytics, or antidepressants for 3 months; a score of at least 10 on the Perceived Stress Scale, and the ability to read and write in English. MS diagnosis was confirmed by chart review according to 2010 McDonald criteria (17). People were excluded if they were pregnant, received MBSR or MCBT training within the previous five years, maintained a ≥ weekly meditation or yoga practice, self-reported serious psychological disorders other than depression or anxiety, self-reported current cancer diagnosis other than basal or squamous cell skin cancer, experienced relapse within 30 days prior to baseline, or scored ≤ 26 on the Mini-mental Status Exam (18) or > 30 on the Beck Depression Inventory (19) on screening.
The study was approved by the OHSU Institutional Review Board and was registered at www.clinicaltrials.gov, NCT02340754. All participants provided written informed consent. The study was conducted from May 2015 to May 2017.
Sample Size
This study was powered to detect significant changes in perceived stress (20) and the SF-36 emotional wellbeing subscale (21) (described below) using results of previous studies of MBSR vs. usual care control (22,23). A minimum sample size of 22 participants per group was required for 80% power to detect a minimum difference between groups of 5.2 points in perceived stress and 10 points in SF-36 emotional wellbeing with a maximum allowable Type 1 error (α) of 5%.
Randomization and Blinding
The statistician generated a randomization scheme that was stratified by baseline Perceived Stress scores (≤ 20 or > 20) with a block size of four (SPSS random number generator). The randomization scheme was maintained by someone outside of the study who had no contact with participants; allocation was concealed from all study staff. All outcomes were collected by the PI and baseline data were collected prior to randomization. The PI, statistician, and personnel performing data entry were blinded to group assignment.
Intervention
The intervention followed the MBSR protocol developed by Jon Kabat-Zinn (24). Participants were asked to attend eight weekly two-hour classes and a six-hour retreat during week six. They learned how to bring mindfulness into their daily practice through meditation, movement, eating, and interacting with others. Instruction included a variety of techniques to facilitate this practice, including gentle yoga, breath work, and body scans (Supplementary Table 1). Participants were encouraged to practice 45 minutes daily. During the retreat participants practiced skills they had learned and were exposed to new exercises. The intervention was facilitated by a certified MBSR instructor with 16 years of experience.
Control
The MS Education protocol was matched to MBSR for time and attention but had no overlap with intervention content. Participants were asked to attend eight weekly two-hour classes and a six-hour retreat during week six. Classes were structured around pamphlets published by the National MS Society, with topics that included: medications and supplements, fatigue, pain, gait and balance, cognition and mood, knowing your rights, financial planning, and connecting with resources. During the retreat participants watched three brief documentaries about stress, mood, and self-efficacy and engaged in facilitated discussion. The program was facilitated by a Program Implementation and Engagement Coordinator from the National MS Society Oregon Chapter.
Assessment and Follow Up
Assessments were conducted at baseline (within one month prior to the first class), mid-intervention (after four weeks of class), immediately post intervention (after eight weeks of class), as well as four months, eight months, and 12 months after the intervention ended (Supplementary Table 2). The primary and secondary end points were eight weeks and 12 months, respectively; additional data collection points enhanced retention. The baseline, eight-week, and 12-month assessments included patient-reported outcomes and physical assessments and were conducted in-person by the PI. The mid-intervention, four-month, and eight-month assessments included only patient-reported outcomes that were collected online.
Outcome Measures
Primary: Feasibility.
Trial success was defined a priori by recruitment (60 participants enrolled within a ten-month period), adherence (≥ 85% of participants attended ≥ six of eight classes, MBSR participants practiced on ≥ 70% of the assigned days (25), and completion (≥ 70% of participants complete the 12-month post-intervention study visit). Feasibility was also assessed with focus groups and interviews; qualitative data will be presented in a separate paper.
Secondary: Clinical Measures Relevant to MS.
The Perceived Stress Scale (PSS) is a widely used measure of subjective psychological stress and is meant to capture how unpredictable and overloaded participants find their lives (24). The PSS has demonstrated good internal reliability (Cronbach’s α=0.89) (26) and is susceptible to change with MBSR interventions (27). The scale range is 0 – 40 and higher scores indicate higher levels of perceived stress.
The SF-36 is a generic measure of health-related quality of life (27). Eight subscales measure various aspects of health, such as emotional well-being, social functioning, energy/fatigue. Previous trials have shown MBSR to have the most impact on mental health quality of life (15), therefore the emotional wellbeing subscale was our primary outcome of interest for the SF-36.
The Patient Reported Outcomes Measurement Information System (PROMIS) is an online collection of validated patient-reported health status inventories (28). Assessments for anxiety, depression, fatigue, and pain interference were collected through an online platform. For a minority of participants who did not have online access, paper copies of PROMIS short forms were administered. Scores are reported on a T-score metric that is referenced to the general U.S. population with a mean of 50 and standard deviation of 10.
The Connor-Davidson Resilience Scale (CD-RISC) is a validated survey that draws on a number of resilient characteristics, including patience, recognition of limits to control, and adaptability (29). It has a high internal consistency and test-retest reliability (29) and has been shown to predict stress in diverse populations (30).
The 3’ Paced Auditory Serial Addition Test (PASAT) is a validated, measure of cognitive processing (31). Administered with a standardized audio recording, a single digit number is spoken every three seconds and participants are asked to add each new number to the one heard immediately prior. Several cognitive tasks are required for successful completion of the PASAT, including sustained attention and information processing ability and speed. PASAT forms A and B were alternated in this study to reduce familiarity with the task between study visits.
The Credibility/Expectancy Questionnaire (CEQ) is a validated questionnaire that measures the amount of benefit a participant expects to receive from a particular intervention (32). The CEQ was administered after participants learned of their group assignment but before the intervention began and was used in sensitivity analyses to control for the potential influence of expectancy on outcomes (33).
Missing Data
If a response on a paper questionnaire was left blank, missing items were imputed by last observation carried forward so that a summary score could be calculated (in total 27 items were imputed). Data for missing participants (n=3 at primary endpoint, n=6 at 12-mos follow up) were not imputed for the primary analyses.
Analyses
A modified intention-to-treat analysis is presented; participants with follow-up data who attended at least one class were included in the analysis. ANCOVA was performed (with baseline values as the covariate) to compare the mean change in outcome measures from baseline to 8 weeks and baseline to 12 months between groups (MBSR vs. Education). Cohen’s d were generated for between group effect sizes. Within-group effect sizes (dz) reflect the mean change from baseline to endpoint divided by the standard deviation of the change. All analyses were conducted in STATA 14.2 (StataCorp, College Station, Texas) with a two-sided significance level of 0.05.
Sensitivity Analyses
We conducted two sensitivity analyses. First, all analyses were rerun after missing data for participants at eight weeks (n=3) and 12 months (n=6) were imputed by linear regression that adjusted for age, sex, and baseline EDSS. Second, we used the imputed data set and reran ANCOVAs adding CEQ scores to the model to control for expectation effects.
RESULTS
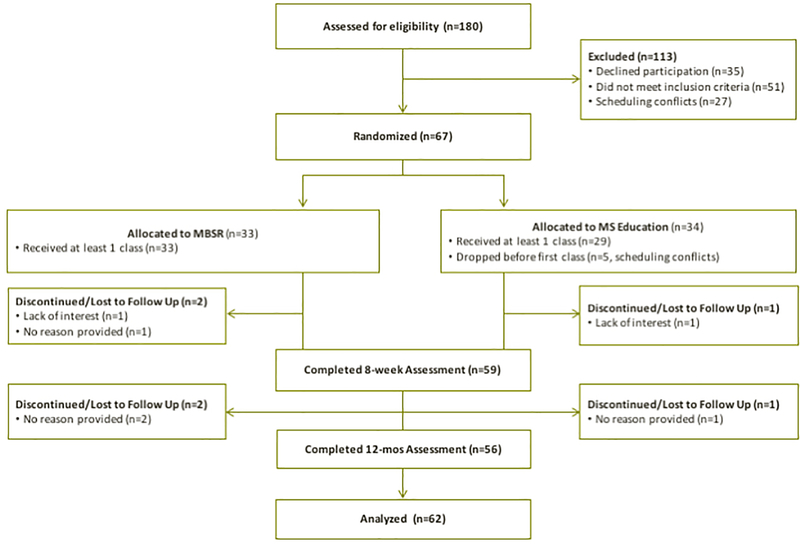
One hundred eighty people were assessed for eligibility (Figure 1). A total of 67 people were randomized to MBSR or Control; five people dropped the study before classes began and 62 participants attended at least one class. Fifty-nine participants (92%) completed the 8-week assessment and 55 participants (89%) completed the 12-month assessment.
Figure 1.
Flow of participants.
There were no significant demographic or clinical differences between groups at baseline (Table 1). The credibility questionnaire was administered after participants were randomized but before the intervention began. People who were randomized to MBSR had higher expectations for successful stress-management than those in the control group (p=0.02, Table 1). Baseline outcome scores did not differ between groups (Table 2).
Table 1.
Baseline demographic and clinical data by intervention status.
| Overall (n=62) | MBSR (n=33) | Education (n=29) | |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Age (years ± sd) | 52.94 ± 11.37 | 53.24 ± 10.66 | 52.59 ± 12.31 |
| Female | 48 (77.42) | 28 (84.85) | 20 (68.97) |
| Education | |||
| ≤ HS Diploma | 25 (40.32) | 16 (48.48) | 9 (31.04) |
| ≥ College Grad | 37 (59.67) | 17 (51.51) | 20 (68.96) |
| Race/Ethnicity | |||
| Hispanic or Latino | 4 (7.02) | 3 (10.34) | 1 (3.57) |
| Not Hispanic or Latino | 53 (92.98) | 26 (89.66) | 27 (96.43) |
| White | 60 (96.77) | 32 (96.97) | 28 (96.55) |
| Type of MS | |||
| Relapsing Remitting | 41 (66.13) | 24 (72.73) | 17 (58.62) |
| Secondary Progressive | 15 (24.19) | 7 (21.21) | 8 (27.59) |
| Primary Progressive | 4 (6.45) | 2 (6.06) | 2 (6.09) |
| Unknown | 2 (3.23) | - | 2 (6.90) |
| Time since diagnosis (years ± sd) | 16.16 ± 10.67 | 14.61 ± 10.10 | 17.93 ± 11.21 |
| EDSS (mean ± sd)a | 4.60 ± 1.93 | 4.48 ± 1.76 | 4.72 ± 2.14 |
| Using Disease Modifying Medicationb | 34 (54.84) | 17 (51.52) | 17 (58.62) |
| Using Psychotropic Medication | 35 (56.45) | 19 (57.58) | 16 (55.17) |
| Credibility (mean ± sd)c | 21.63 ± 4.07 | 18.62 ± 5.52 |
EDSS: Expanded Disability Severity Scale.
Number of people taking disease modifying medications: interferon beta-1a, 11; glatiramer acetate, 6; dimethyl fumarate, 9; natalizumab, 5; and fingolimod, 3.
Credibility Questionnaire was administered after group assignment and before intervention. There was a significant difference between groups (p=0.02).
Table 2.
Intention-to-treat analysis for participants with data receiving either Mindfulness-based Stress Reduction (MBSR) or Education Control.
| Baseline Levels | Immediately Post-intervention | 12-mos Follow-up | Intervention Effects (Δ baseline to immediately post)a | 12-mos Follow-up Effects ( Δ baseline to 12-mos Follow-up)a | |||||
|---|---|---|---|---|---|---|---|---|---|
| MBSR n=33 | MBSR n=31 | MBSR n=29 | MBSR n=31 | MBSR n=29 | |||||
| EDU n=29 | EDU n=28 | EDU n=27 | EDU n=28 | EDU n=27 | |||||
| Secondary Measures | mean ± sd | mean change (95% CI) | mean change (95%CI) | F | p | ES (95% CI) | F | p | ES (95% CI) |
| Perceived Stress Scale | 1.10 | 0.30 | −0.21 (−.72 to 0.30) | 1.53 | 0.22 | −0.25 (−0.78 to 0.28) | |||
| MBSR | 17.76 ± 6.06 | −5.29 (−2.46 to −8.12) | −4.34 (−1.96 to −6.73) | ||||||
| Education | 18.0 ± 5.71 | −3.89 (−1.9 to −5.86) | −2.74 (−0.14 to −5.34) | ||||||
| SF-36 Emotional Wellbeing | 0.50 | 0.48 | 0.15 (−0.36 to 0.66) | 0.36 | 0.55 | 0.09 (−0.44 to 0.61) | |||
| MBSR | 63.39 ± 16.97 | 11.74 (4.50 to 18.98) | 6.76 (−1.06 to 14.58) | ||||||
| Education | 63.31 ± 16.25 | 9.14 (3.36 to 14.93) | 5.04 (−1.92 to 12.00) | ||||||
| PROMIS Anxiety | 2.41 | 0.13 | −0.48 (−0.99 to 0.04) | 0.01 | 0.91 | 0.01 (−0.52 to 0.53) | |||
| MBSR | 59.81 ± 6.76 | −6.26 (−3.53 to −9.0) | −5.36 (−2.63 to −8.09) | ||||||
| Education | 58.06 ± 6.04 | −3.26 (−1.45 to −5.08) | −5.40 (−2.47 to −8.32) | ||||||
| PROMIS Depression | 1.84 | 0.18 | −0.39 (−0.90 to 0.13) | 0.34 | 0.56 | −0.16 (− 0.68 to 0.37) | |||
| MBSR | 55.21 ± 6.47 | −4.77 (−2.15 to −7.38) | −4.49 (−1.48 to −7.50) | ||||||
| Education | 54.28 ± 5.51 | −2.47 (−0.81 to −4.13) | −3.33 (−0.72 to −5.94) | ||||||
| PROMIS Fatigue | 0.71 | 0.40 | −0.18 (−0.69 to 0.33) | 0.8 | 0.37 | −0.21 (−0.74 to 0.31) | |||
| MBSR | 60.74 ± 8.29 | −4.57 (−1.49 to −7.64) | −4.99 (−1.94 to −8.04) | ||||||
| Education | 60.23 ± 7.63 | −3.28 (−1.18 to −5.37) | −3.55 (−1.61 to −5.49) | ||||||
| PROMIS Pain Interference | 0.07 | 0.79 | −0.03 (−0.54 to 0.48) | 3.03 | 0.09 | 0.45 (−0.08 to 0.98) | |||
| MBSR | 55.48 ± 10.47 | −2.21 (0.02 to −4.45) | 1.09 (3.70 to −1.51) | ||||||
| Education | 55.17 ± 9.10 | −1.96 (1.49 to −5.40) | −1.95 (0.65 to −4.55) | ||||||
| Resilience | 1.14 | 0.30 | 0.35 (−0.16 to 0.87) | 0.72 | 0.40 | 0.29 (− 0.24 to 0.82) | |||
| MBSR | 63.76 ± 9.15 | 8.10 (4.29 to 11.91) | 7.55 (2.14 to 12.97) | ||||||
| Education | 67.10 ± 12.2 | 4.61 (0.99 to 8.23) | 3.93 (−0.18 to 8.03) | ||||||
| PASAT 3' | 0.30 | 0.59 | 0.03 (−0.49 to 0.54) | 0.3 | 0.59 | 0.12 (−0.41 to 0.65) | |||
| MBSR | 44.67 ± 11.07 | 2.51 (0.84 to 4.19) | 2.59 (−1.06 to 6.24) | ||||||
| Education | 39.93 ± 10.38 | 2.39 (0.38 to 4.41) | 1.56 (−1.59 to 4.70) | ||||||
Acronyms: EDU (education control); ES (effect size); PASAT (Paced Auditory Serial Addition Test); PROMIS (Patient Reported Outcomes Information System); CAT (Computerized Adaptive Test)
ANCOVA adjusting for baseline levels. F statistic and p value are for the group effect. ES is Cohen’s d comparing changes from baseline between groups.
For PROMIS surveys, higher scores indicate more of the construct being measured. For SF-36 subscales, higher scores indicate better health. PASAT scores are number of correct answers out of 60, higher scores are better.
Primary Outcome: Feasibility.
Our recruitment target was met; 60 participants were enrolled within 10 months. Eighty-five percent of MBSR participants and 90% of Education participants attended at least 6 out of 8 classes. During the intervention, 30 MBSR participants turned in practice logs indicating that they practiced on 55% of assigned days, and that daily practices had a median duration of 38 minutes (range 14 to 80 minutes). Practice patterns were unrelated to baseline levels of perceived stress, emotional wellbeing, or fatigue.
Secondary Outcomes.
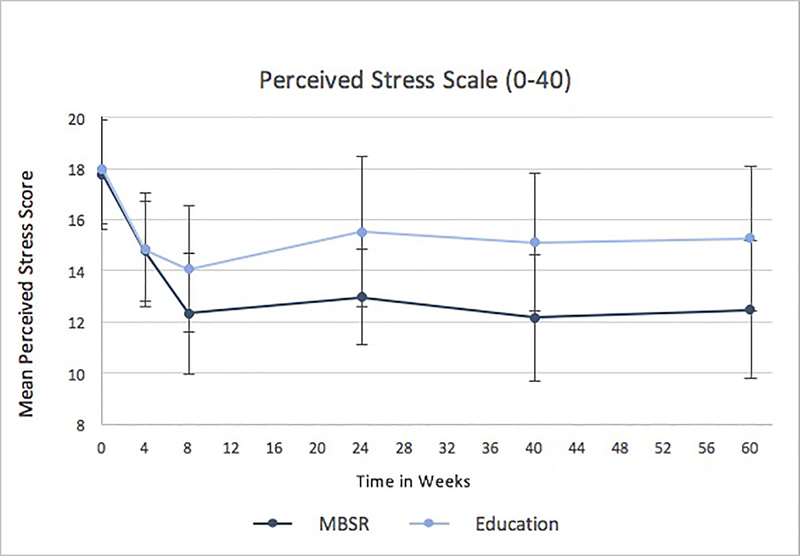
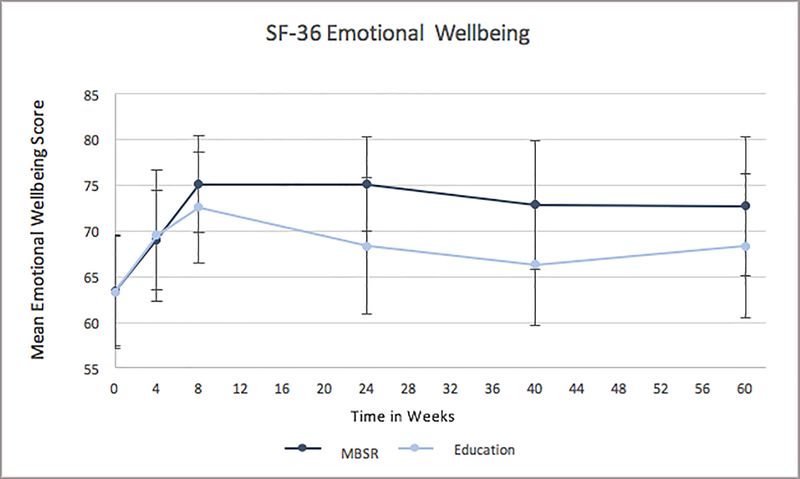
While MBSR participants generally showed greater improvement in secondary outcomes compared to control, differences in scores between the groups group were not statistically significant at either time point (Table 2). Both MBSR and Education groups showed statistically significant improvements in perceived stress, anxiety, depression, fatigue, and resilience scores from baseline at 8-weeks and at 12-months. Both groups experienced significant positive change in emotional wellbeing and the PASAT at 8 weeks, but the effect for both of these outcomes was no longer statistically significant at 12-months. We did not find significant between- or within-group change for pain interference. Effect sizes of within-group change are presented in Table 3. To aid participant retention, data were also collected mid-intervention (four weeks) and at four and eight months post-intervention. Data using all time points were plotted for perceived stress (Figure 2) and emotional wellbeing (Figure 3) and visually confirm patterns seen in Table 2.
Table 3.
Within-group effect sizes (dz) and 95% confidence intervals for the Mindfulness-based Stress Reduction (MBSR) intervention and the Education control.
| Effect Size of MBSR Intervention | Effect Size of Education Control | |||
|---|---|---|---|---|
| Secondary Measures | Δ baseline to immediately post | Δ baseline to 12 months | Δ baseline to immediately post | Δ baseline to 12 months |
| Perceived Stress | −0.71 (−1.10, −0.28) | −0.69 (−1.10, −0.28) | −0.73 (−1.15, −0.30) | −0.42 (−0.81, −0.02) |
| SF-36 Emotional Wellbeing | 0.52 (0.13, 0.91) | 0.33 (−0.05, 0.70) | 0.58 (0.17, 0.98) | 0.29 (−0.10. 0.67) |
| PROMIS Anxiety | −0.77 (−.18, −.035) | −0.75 (−1.15, −0.33) | −0.66 (−1.07, −0.24) | −0.73 (−1.15, −0.30) |
| PROMIS Depression | −0.61 (−1.00, −0.21) | −0.57 (−0.96, −0.17) | −0.57 (−0.97, −0.16) | −0.50 (−0.90, −0.10) |
| PROMIS Fatigue | −0.51 (−0.89, −0.12) | −0.62 (−1.02, −0.22) | −0.58 (−0.99, −0.17) | −0.72 (−1.14, −0.30) |
| PROMIS Pain Interference | −0.38 (−0.75, 0.00) | 0.16 (−0.21, 0.52) | −0.19 (−0.57, 0.19) | −0.27 (−0.68, 0.09) |
| Resilience | 0.72 (0.30, 1.12) | 0.53 (0.14, 0.92) | 0.47 (0.07, 0.86) | 0.38 (−0.02, 0.77) |
| PASAT 3' | 0.56 (0.15, 0.96) | 0.28 (−0.11, 0.66) | 0.44 (0.04,0.83) | 0.20 (−0.19, 0.57) |
Acronyms: PASAT (Paced Auditory Serial Addition Test); PROMIS (Patient Reported Outcomes Information System);
Negative effect sizes indicate improvement for perceived stress, anxiety, depression, fatigue, pain interference. Positive effect sizes indicate improvement for emotional wellbeing, resilience and the PASAT.
Figure 2.
Mean Perceived Stress Scale (PSS) scores and 95% confidence intervals for participants of an eight-week mindfulness-based stress reduction (MBSR) intervention or a multiple sclerosis education control. Both groups experienced significant within-group change at each time point; no significant between-group differences were found. Lower PSS scores are preferred. Primary data assessments were baseline, immediately post intervention (8 weeks), and 12-months post-intervention (60 weeks). Additional data assessments helped with retention.
Figure 3.
Mean scores for the SF-36 Emotional Wellbeing subscale for participants of an eight-week mindfulness-based stress reduction (MBSR) intervention or a multiple sclerosis education control. Both groups experienced significant within-group change at each time point; no significant between-group differences were found. Higher SF-36 scores are preferred. Primary data assessments were baseline, immediately post intervention (8 weeks), and 12-months post-intervention (60 weeks). Additional data assessments helped with retention.
Adverse Events.
Two adverse events were likely related to the intervention: one MBSR participant experienced leg spasticity of moderate severity after a guided progressive muscle relaxation exercise in class, another person experienced increased levels of anxiety and a migraine after the MBSR retreat.
Sensitivity Analyses.
Results using imputed data (not shown) were not materially different from those presented. Adjusting for participant expectation with the CER score did not noticeably change results (data not shown).
DISCUSSION
This study demonstrates that MBSR is feasible for people with MS across a range of physical abilities. In general, improvements for MBSR participants were of a greater magnitude compared to control participants for a variety of outcomes, although between-group differences were not statistically significant. Preliminary findings suggest that either MBSR or MS Education may improve perceived stress, emotional wellbeing, depression, anxiety, fatigue, and resilience in the short-term, and that most of these improvements could be sustained for a full year without additional intervention. Our trial adds to previous mindfulness studies in MS by including participants with EDSS ≤ 8.0, likely increasing generalizability of findings for a broader population. We assessed outcomes over 12-months, providing new evidence that the impact of MBSR may have fairly long-lasting effects for this population. Finally, we used an active comparator that was structurally similar to the intervention, allowing us to control for non-specific effects of MBSR.
Previous mindfulness-based interventions for people with MS are limited, and we are aware of only one other study that has used an active control. Carletto et al. randomized 90 people with symptoms of depression and EDSS ≤ 6.5 to either a mindfulness intervention or a time-and-attention psychoeducation control (16). In contrast to our findings, mindfulness led to a significantly greater reduction in stress than psychoeducation that was sustained at 6-month follow up (intention-to-treat analysis p=0.01). In the Carletto et al. study, the mindfulness group improved approximately 5 points on the Perceived Stress Scale immediately post-intervention and approximately 4 points at the 6-month follow-up, a finding that mirrors our results. Control participants, however, improved approximately 1.5 points on the PSS immediately post-intervention whereas our control group reported almost a 4-point improvement (with a similar trend at follow-up). Thus, differences in intervention effect size across the studies may be due to differences in control program content or delivery, or target popoulation. Additionally, on average our participants were older, had a higher EDSS score, and had been living with MS for almost twice as many years as the Carletto study participants. It is possible that these characteristics might help differentiate people who would benefit from educational interventions from those who would not, and further investigation is warranted.
The improvements we observed in additional secondary outcomes reflect what others have reported. Grossman et al. compared MBSR to a waitlist control (n=150; EDSS <= 6.0) and found significant improvements in quality of life, anxiety, depression, and fatigue immediately post intervention; positive outcomes were sustained at 6-month follow up (15). Other studies have shown improvements in measures of anxiety, depression, and fatigue, although methodological differences make direct comparisons difficult (12–14).
Our study was powered on previous trials that used a usual care control, thus we may have been underpowered to detect between-group differences. Visually it seems there may be additional benefit of MBSR compared to education, but because our observed effect size was small, a future trial powered on these data would need several hundred participants in each arm to detect a significant difference of this magnitude, should it exist. This highlights the challenge of designing appropriate active comparators for complex behavioral interventions and the need for future work in this area (34).
It is unclear what aspects of our control program may have led to improvement. Participants reported enjoying each other’s company and the group functioned much like a facilitated peer support group. Data on peer support interventions in MS are limited and inconsistent. A small (n=33) pre-post, eight-week peer support intervention with class content and structure comparable to ours found short-term significant improvements in depression, anxiety, and stress (35). In contrast, Uccelli et al. found eight weeks of peer support did not result in improvements in quality of life or depression. Like most behavioral interventions, some people will find benefit where others do not. For these types of studies, randomization may obscure the magnitude of benefit that could be achieved if people were to select interventions that are of interest to them.
Results should be interpreted in the context of study limitations. Wihtout a usual care or waitlist control, sponatenous improvement or regression to the mean cannot be ruled out as alternative explanations for our findings. Participants could not be blinded to the intervention, making it difficult to control for placebo or expectancy effects. Nevertheless, our sensitivity analysis showed that participant expectation of benefit based on the group they were assigned did not influence outcomes. We are limited by a mostly white, middle aged, study sample and our findings may not generalize to more ethnically, racially, or geographically diverse populations, or to younger people with more recent diagnoses. Adaptations of the intervention and control may increase cultural relevance and applicability for those not represented in our study sample (36).
This study has many strengths. The control group was structurally equivalent in time and attention to the intervention. Participants had varied levels of physical abilities, and results may generalize to a broader population of people with MS than earlier findings. Levels of attendance and follow-up were high; missing data was limited and had no detectable influence on study findings. Overall this was a safe intervention. In the future, establishing a more robust baseline for primary clinical outcomes (e.g. regular assessment for 1–2 months prior to randomization) would help detect regression to the mean, were it present. In addition, designing adequate control programs for behavioral interventions is complex, and future trials that employ both active and passive control arms will have greater ability to infer causation than we did here.
CONCLUSIONS
We found a randomized trial of MBSR is feasible for adults with MS across a broad range of physical abilities. We observed similar short- and long-term mean improvements in emotional wellbeing with both MBSR and MS education interventions. Spontaneous improvement cannot be ruled out as an explanation for improvement with either intervention, and larger studies to determine efficiacy that simultaneously compare mindfulness training to both active and passive controls appear to be warranted.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the participants who shared their time, experience, and data for this study; Kimberly Carson, MPH, C-IAYT, E-RYT for facilitating the MBSR intervention and Carol Choutka with the National MS Society for facilitating the MS education group; and Sara Pavao, Jan Taylor, and Heather Schiffke for invaluable study support.
FUNDING ACKNOWLEDGEMENTS
This work was supported by the Oregon Clinical and Translational Research Institute [Grant number UL1 RR024140 from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health]; the National Center for Complementary and Integrative Health of the National Institutes of Health [Grant number K23AT008211]. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding statement
Funding was received from the U.S. Department of Health and Human Services, National Institutes of Health, National Center for Advancing Translational Sciences (UL1 RR024140) and the U.S. Department of Health and Human Services, National Institutes of Health, National Center for Complementary and Integrative Health (K23AT008211).
Footnotes
Disclosures
The authors declare no conflicts of interest relating to this paper.
This study is registered at www.clinicaltrials.gov, NCT02340754.
REFERENCES
- 1.Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004. March 27;328(7442):731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohr DC, Goodkin DE, Bacchetti P, Boudewyn AC, Huang L, Marrietta P, et al. Psychological stress and the subsequent appearance of new brain MRI lesions in MS. Neurology. 2000. July 12;55(1):55–61. [DOI] [PubMed] [Google Scholar]
- 3.Mohr DC, Lovera J, Brown T, Cohen B, Neylan T, Henry R, et al. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. 2012. July 31;79(5):412–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minden SL, Feinstein A, Kalb RC, Miller D, Mohr DC, Patten SB, et al. Evidence-based guideline: Assessment and management of psychiatric disorders in individuals with MS: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013. December 27;82(2):174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.San José AM, Oreja-Guevara C, Lorenzo SC, Notario LC, Vega BR, Pérez CB. Psychotherapeutic and psychosocial interventions for managing stress in multiple sclerosis: The contribution of mindfulness-based interventions. Neurol Engl Ed. 2016;31(2):113–120. [DOI] [PubMed] [Google Scholar]
- 6.Gotink RA, Chu P, Busschbach JJV, Benson H, Fricchione GL, Hunink MGM. Standardised Mindfulness-Based Interventions in Healthcare: An Overview of Systematic Reviews and Meta-Analyses of RCTs. PLoS ONE [Internet]. 2015. April 16 [cited 2018 Apr 15];10(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4400080/ [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Ulrichsen KM, Kaufmann T, Dørum ES, Kolskår KK, Richard G, Alnaes D, et al. Clinical Utility of Mindfulness Training in the Treatment of Fatigue After Stroke, Traumatic Brain Injury and Multiple Sclerosis: A Systematic Literature Review and Meta-analysis. Front Psychol [Internet]. 2016. June 23 [cited 2018 Apr 29];7 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4917545/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simpson R, Mair FS, Mercer SW. Mindfulness-based stress reduction for people with multiple sclerosis – a feasibility randomised controlled trial. BMC Neurol [Internet]. 2017. [cited 2017 Jun 4];17 Available from: https://www-ncbi-nlm-nih-gov.liboff.ohsu.edu/pmc/articles/PMC5434553/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilbertson RM, Klatt MD. Mindfulness in Motion for People with Multiple Sclerosis: A Feasibility Study. Int J MS Care. 2017;19(5):225–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blankespoor RJ, Schellekens MPJ, Vos SH, Speckens AEM, de Jong BA. The Effectiveness of Mindfulness-Based Stress Reduction on Psychological Distress and Cognitive Functioning in Patients with Multiple Sclerosis: a Pilot Study. Mindfulness. 2017;8(5):1251–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoogerwerf AEW, Bol Y, Lobbestael J, Hupperts R, van Heugten CM. Mindfulness-based cognitive therapy for severely fatigued multiple sclerosis patients: A waiting list controlled study. J Rehabil Med. 2017. June 28;49(6):497–504. [DOI] [PubMed] [Google Scholar]
- 12.Nejati S, Rajezi Esfahani S, Rahmani S, Afrookhteh G, Hoveida S. The Effect of Group Mindfulness-based Stress Reduction and Consciousness Yoga Program on Quality of Life and Fatigue Severity in Patients with MS. J Caring Sci. 2016. December 1;5(4):325–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolahkaj B, Zargar F. Effect of Mindfulness-Based Stress Reduction on Anxiety, Depression and Stress in Women With Multiple Sclerosis. Nurs Midwifery Stud. 2015. December;4(4):e29655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bogosian A, Chadwick P, Windgassen S, Norton S, McCrone P, Mosweu I, et al. Distress improves after mindfulness training for progressive MS: A pilot randomised trial. Mult Scler J. 2015;1352458515576261. [DOI] [PubMed] [Google Scholar]
- 15.Grossman P, Kappos L, Gensicke H, D’Souza M, Mohr DC, Penner IK, et al. MS quality of life, depression, and fatigue improve after mindfulness training: A randomized trial. Neurology. 2010. September 27;75(13):1141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carletto S, Tesio V, Borghi M, Francone D, Scavelli F, Bertino G, et al. The Effectiveness of a Body-Affective Mindfulness Intervention for Multiple Sclerosis Patients with Depressive Symptoms: A Randomized Controlled Clinical Trial. Front Psychol [Internet]. 2017. [cited 2017 Dec 19];8 Available from: https://www.frontiersin.org/articles/10.3389/fpsyg.2017.02083/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011. February;69(2):292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitrushina M, Satz P. Reliability and validity of the Mini-Mental State Exam in neurologically intact elderly. J Clin Psychol. 1991. July;47(4):537–43. [DOI] [PubMed] [Google Scholar]
- 19.Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961. June;4:561–71. [DOI] [PubMed] [Google Scholar]
- 20.Cohen S, Williamson G. Perceived Stress in a Probability Sample of the United States In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 21.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992. June;30(6):473–83. [PubMed] [Google Scholar]
- 22.Nyklícek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med Publ Soc Behav Med. 2008. June;35(3):331–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geary C, Rosenthal SL. Sustained Impact of MBSR on Stress, Well-Being, and Daily Spiritual Experiences for 1 Year in Academic Health Care Employees. J Altern Complement Med. 2011. October;17(10):939–44. [DOI] [PubMed] [Google Scholar]
- 24.Kabat-Zinn J An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982. April;4(1):33–47. [DOI] [PubMed] [Google Scholar]
- 25.Salmon P, Santorelli S, Sephton S, Kabat-Zinn J. Intervention Elements Promoting Adherence to MBSR Programs In: The Handbook of Health Behavior Change. Third New York, NY: Springer Publishing Company; 2009. p. 271–86. [Google Scholar]
- 26.Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale.(Report). J Coll Couns [Internet]. 2006. September 22 [cited 2012 Oct 5]; Available from: http://www.highbeam.com/doc/1G1-155240124.html [Google Scholar]
- 27.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008. February;31(1):23–33. [DOI] [PubMed] [Google Scholar]
- 28.Rothrock NE, Hays RD, Spritzer K, Yount SE, Riley W, Cella D. Relative to the general US population, chronic diseases are associated with poorer health-related quality of life as measured by the Patient-Reported Outcomes Measurement Information System (PROMIS). J Clin Epidemiol. 2010. November;63(11):1195–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 30.Sexton MB, Byrd MR, von Kluge S. Measuring resilience in women experiencing infertility using the CD-RISC: examining infertility-related stress, general distress, and coping styles. J Psychiatr Res. 2010. March;44(4):236–41. [DOI] [PubMed] [Google Scholar]
- 31.Tombaugh T A comprehensive review of the Paced Auditory Serial Addition Test (PASAT). Arch Clin Neuropsychol. 2006. January;21(1):53–76. [DOI] [PubMed] [Google Scholar]
- 32.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000. June;31(2):73–86. [DOI] [PubMed] [Google Scholar]
- 33.Caspi O, Burleson KO. Methodological challenges in meditation research. Adv Mind Body Med. 2005;21(1):4–11. [PubMed] [Google Scholar]
- 34.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, et al. The Selection and Design of Control Conditions for Randomized Controlled Trials of Psychological Interventions. Psychother Psychosom. 2009;78(5):275–84. [DOI] [PubMed] [Google Scholar]
- 35.Ng L, Amatya B, Khan F. Outcomes of a Peer Support Program in Multiple Sclerosis in an Australian Community Cohort: A Prospective Study. J Neurodegener Dis [Internet]. 2013. [cited 2017 Dec 12];2013 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437345/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fuchs C, Lee JK, Roemer L, Orsillo SM. Using Mindfulness- and Acceptance-Based Treatments With Clients From Nondominant Cultural and/or Marginalized Backgrounds: Clinical Considerations, Meta-Analysis Findings, and Introduction to the Special Series: Clinical Considerations in using Acceptance- and Mindfulness-based Treatments With Diverse Populations. Cogn Behav Pract. 2013. February 1;20(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.