Abstract
Acute kidney injury (AKI) is a frequent complication in ST-elevation myocardial infarction (STEMI) patients. Factors other than contrast exposure have been suggested as major contributors to renal dysfunction in patients undergoing primary percutaneous coronary intervention (PPCI). Our aim was to assess the incidence and risk factors of AKI in high-risk STEMI patients, mostly treated by PPCI with implemented measures to prevent contrast-induced AKI. We retrospectively analyzed data of 245 STEMI patients (165 men, mean age 63.9 ± 11.9 years) admitted to the Department of Medical Intensive Care Unit. Demographic, clinical, and mortality data were compared between AKI and non-AKI group. AKI was defined as a 1.5-fold increase in serum creatinine from baseline level within 24–48 hours. AKI developed in 34/245 (13.9%) patients. PPCI was performed in 226/245 (92.2%) of all STEMI cases, with no difference between AKI and non-AKI group. There were significant differences between AKI and non-AKI group in diabetes mellitus (41.2% vs. 20.9%), prior MI (26.5% vs. 11.8%), prior resuscitation (38.2% vs. 12.4%), admission acute heart failure [AHF] (44.1% vs. 12.8%), in-hospital AHF (70.6% vs. 17.5%), and hospital-acquired infection [HAI] (79.4% vs. 18.0%). Significantly more AKI patients had increased admission CRP ≥25 mg/L (38.2% vs. 11.8%), peak CRP ≥50 mg/L (91.2% vs. 36%), admission troponin I ≥10 µg/L (44.1% vs. 24.6%), peak troponin I ≥50 µg/L (64.7% vs. 44.1%), peak NT-proBNP ≥400 pmol/L (82.4% vs. 27.5%), and ejection fraction <45% (76.5% vs. 33.6%). Mortality was significantly increased in AKI group, including in-hospital (52.9% vs. 7.1%), 30-day (64.7% vs. 10.7%) and 6-month mortality (70.6% vs. 13.7%). Significant independent predictors of AKI were prior resuscitation (OR 4.171, 95% CI 1.088–15.998), HAI (OR 7.974, 95% CI 1.992–31.912), and peak NT-proBNP (OR 21.261, 95% CI 2.357–191.795). To reduce the risk of AKI in STEMI patients, early diagnosis and treatment of AHF and HAIs are advisable.
Keywords: ST-elevation myocardial infarction, STEMI, acute kidney injury, AKI, predictors, mortality, acute heart failure, infection
INTRODUCTION
Acute kidney injury (AKI) is a frequent complication in patients with ST-elevation myocardial infarction (STEMI), leading to high morbidity and mortality in this subset of STEMI population [1-3]. The risk of AKI is particularly increased in STEMI patients who are older, have comorbidities, have pulmonary edema or cardiogenic shock on admission, were resuscitated before admission, in whom primary percutaneous coronary intervention (PPCI) was delayed, who have complex coronary artery disease (CAD) and/or who required multistage procedures during PPCI [4,5].
AKI is characterized by a rapid loss of kidney function. AKIN (Acute Kidney Injury Network) and KDIGO (Kidney Disease Improving Global Guidelines) define AKI as a percentage increase in serum creatinine of more than or equal to 50% (1.5-fold from baseline), with or without oliguria. Different studies have shown that even small changes in serum creatinine concentration affect the prognosis of STEMI patients [6,7].
The incidence of AKI in STEMI patients ranges from 5% to 30%, depending on the diagnostic criteria utilized [1]. Currently used diagnostic measures for AKI include glomerular filtration rate (GFR), serum creatinine and urinary output, where decreased GFR, decreased urine output and/or increased serum creatinine are indicative of renal dysfunction [6,7].
Structural and functional changes in the kidneys leading to AKI may be due to different pathological mechanisms, including renal hypoperfusion, ischemia and nephrotoxicity [1,8,9]. In STEMI patients, systemic hypoperfusion, which occurs as a consequence of acute left ventricular (LV) systolic dysfunction and results in renal ischemia, appears to be important pathological mechanism underlying AKI [2,10,11]. Other factors that contribute to AKI in STEMI patients are contrast media volume (contrast-induced nephrotoxicity), increased sympathetic activity and neurohumoral activation (e.g., upregulation of angiotensin II, epinephrine and norepinephrine), enhanced inflammatory response, oxidative stress, hyperglycemia, bleeding, hypovolemia, and nephrotoxic drugs [1,2,8,9,12]. Risk factors for the development of AKI include, among others, older age, diabetes mellitus, prior or baseline chronic kidney disease, dehydration, and anemia [1,13].
Early PPCI in STEMI patients can protect myocardium, increase hemodynamic stability, and prevent AKI [5]. Current guidelines provide a number of recommendations to prevent contrast-induced AKI, including the use of iso-osmolar or low-osmolar (water-soluble) contrast media in the lowest possible dose, avoidance of nephrotoxic drugs, and hydration with intravenous (I.V.) crystalloid fluids [5,7,14].
In this study, we aimed to assess the incidence and risk factors of AKI in high-risk STEMI patients mostly treated by PPCI, for which the recommended preventive measures were implemented.
MATERIALS AND METHODS
Study design and protocol
We performed a retrospective observational study. The Institutional Medical Ethics Committee (UKC-MB-KME-23-02/17) approved the study and waived the need for informed consent due to the retrospective nature of the study. The personal data of patients were protected according to the Law on Personal Data Protection.
Study population
We initially assessed 330 patients who were admitted to the University Medical Centre Maribor (either to the coronary care unit [CCU] of the Department of Cardiology or to the Department of Medical Intensive Care Unit [ICU]) between December 2014 and December 2015, and were discharged with a diagnosis of acute STEMI. A total of 245 consecutive STEMI patients (165 men and 80 women, mean age 63.9 ± 11.9 years), all from the Department of Medical ICU, were finally included in the study. STEMI patients were admitted to the Department of Medical ICU if they had a high-risk profile due to older age, frequent comorbidities, pulmonary edema or cardiogenic shock on admission, resuscitation before admission, delays in PPCI, complex CAD, or due to multistage procedures during PPCI.
Demographic, clinical, and mortality data
We obtained demographic, clinical, and mortality data of 245 patients from the institutional medical information system, that were in accordance with the standard criteria for STEMI. Demographic data, clinical data on admission and during hospital stay, data related to in-hospital treatment, and in-hospital, 30-day and 6-month mortality data were collected.
Demographic data included age, gender, comorbidities (arterial hypertension, diabetes mellitus, prior myocardial infarction [MI]), and cigarette smoking. Admission data included the incidence of admission acute heart failure (AHF) and resuscitation before admission. Laboratory data included troponin I, serum creatinine, C-reactive protein (CRP), and N-terminal pro-brain natriuretic peptide (NT-proBNP). In-hospital treatments comprised PPCI and antithrombotic therapy (acetylsalicylic acid [ASA] and clopidogrel or prasugrel or ticagrelor). For in-hospital complications, we evaluated the incidence of AHF, arrhythmia, reinfarction, bleeding, infections, and AKI at any time point during hospital stay.
Arrhythmias were detected using continuous and standard electrocardiogram (ECG) recording, and were classified as atrial, ventricular or conduction disturbances.
The severity of heart failure was quantified using the Killip classification; patients were categorized in Killip class II, III or IV if they had pulmonary congestion, pulmonary edema or cardiogenic shock, respectively [15].
Reinfarction was defined as recurrence of chest pain with new abnormalities detected on ECG and recurring increase/decrease of serum troponin I [5].
Hospital-acquired infection (HAI) was defined as the presence of microorganisms in otherwise sterile body fluids/tissue samples (blood, cerebrospinal fluid, lung tissue, urinary tract, etc.) with or without clinical symptoms (fever, increased CRP, leukocytosis, or leukocytopenia), or based on antibiotic administration due to strong clinical suspicion of infection [16].
According to the Thrombolysis in Myocardial Infarction (TIMI) criteria, major bleeding was defined as intracranial bleeding or symptomatic bleeding in other location with a drop in hemoglobin level of >50 g/L or the need for transfusion of ≥2 units of blood products. Minor bleeding was defined as symptomatic with a drop in hemoglobin level of 30–50 g/L. Minimal bleeding was defined as symptomatic with a drop in hemoglobin level of <30 g/L [17].
AKI was defined as an increase in serum creatinine of at least 50% within 24–48 hours [18].
In the case of complications, patients were treated according to standard protocols at the discretion of the treating physician (e.g., by vasopressors, inotropic agents, mechanical ventilation (MV), intra-aortic balloon pump (IABP), red blood cell [RBC] transfusions, antibiotics, antiarrhythmic drugs, or pacing) [5].
Initial diagnosis of STEMI
In emergency medical services, STEMI was diagnosed based on the following criteria: ischemic symptoms with or without dyspnea with ST-segment elevation in at least two contiguous leads or presumed new left bundle branch block (LBBB) on ECG.
Treatment of STEMI patients
At the first medical contact, according to the current European Society of Cardiology (ESC) guidelines, patients received dual antiplatelet therapy consisting of ASA and clopidogrel or ticagrelor or prasugrel, I.V. heparin up to 5000 IU, oxygen if SaO2 was <90% to reach target SaO2 95%, morphine with an I.V. antiemetic and sublingual nitroglycerin if they had chest pain [5]. Patients with pulmonary edema received diuretics and those with cardiogenic shock were treated with vasopressors, inotropes (dobutamine or levosimendan) and occasionally by IABP [5]. Patients with severe acute respiratory failure were intubated and, if necessary, mechanically ventilated. If patients had cardiac arrest, they were resuscitated and, in most cases, intubated and mechanically ventilated [5].
Upon arrival to the University Clinical Centre, PPCI was performed in the Catheterization Laboratory as soon as possible and, in most cases, before admission to the Department of Medical ICU. Iomeron 300 mg/L, a new generation of non-ionic, water-soluble tri-iodinated contrast medium with low osmolality and viscosity, was used for coronary angiography [5]. We recorded standard ECG and carried out basic lab tests before PPCI and thereafter on a daily basis. After PPCI, STEMI patients, admitted to the Department of Medical ICU, were non-invasively monitored by continuous ECG, pulse oximetry and hourly by non-invasive blood pressure measurements, for at least 24 hours. Invasive monitoring was started if necessary.
Patients with hypoxemia (SaO2 < 90%) received oxygen by face mask or nasal cannula, within few hours of admission. Those with severe respiratory failure were intubated and mechanically ventilated [5].
To prevent contrast-induced kidney injury patients received I.V. infusion of 50–100 ml/h of crystalloids. Fluid responsiveness was assessed by 2D echocardiography measuring left ventricular contractility and inspiratory collapse of the inferior vena cava [5].
Statins, beta receptor blockers, and angiotensin-converting enzyme (ACE) inhibitors were prescribed after 24 hours of admission. To prevent stent thrombosis, we continued dual antiplatelet therapy (ASA and clopidogrel or prasugrel or ticagrelor) at maintenance dose [5].
Echocardiography was performed on admission and before discharge. Other diagnostic procedures were performed in case of complications and included chest radiograph, coronary angiography, ECG, and laboratory tests among others [5].
ECG abnormalities (i.e., ST-segment elevation with or without Q waves, new LBBB) and changes in the level of troponin I confirmed the diagnosis of STEMI [5].
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows Version 19.0 (IBM Corp., Armonk, NY, USA). The results were expressed as mean ± standard deviation (SD) or percentages. To test the differences between groups, we used two-sided Student’s t-test for mean values and Chi-square test for percentages. A value of p < 0.05 was considered statistically significant. We used logistic regression analysis (Wald statistic) to assess the independent predictors of AKI in STEMI patients.
RESULTS
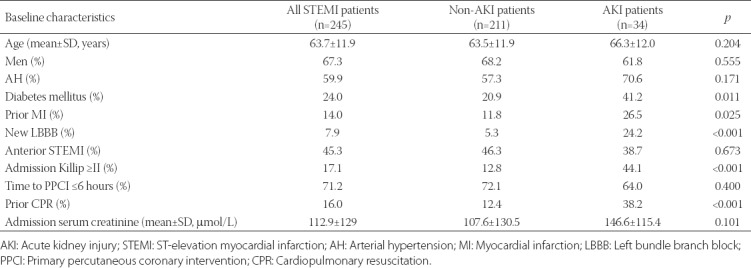
Baseline characteristics of 245 high-risk STEMI patients admitted to the Department of Medical ICU are shown in Table 1. Out of 245 STEMI patients 34 (13.9%) developed AKI, while 211 patients (86.1%) did not develop AKI. Significant differences were observed between AKI and non-AKI group in comorbidities (i.e. diabetes mellitus [41.2% vs. 20.9%, p = 0.011] and prior MI [26.5% vs. 11.8%, p = 0.025]), presumed new LBBB (24.2% vs. 5.3%, p < 0.001), admission AHF (44.1% vs. 12.8%, p < 0.001), and prior resuscitation [38.2% vs. 12.4%, p < 0.001] (Table 1).
TABLE 1.
Baseline characteristics of 245 STEMI patients with/without AKI
Laboratory results on admission and during hospital stay of 245 STEMI patients with/without AKI are shown in Table 2. Admission and peak CRP, admission and peak troponin I, and peak NT-proBNP levels were significantly increased in AKI compared to non-AKI group (admission CRP ≥25mg/L: 38.2% vs. 11.8%, p < 0.001; peak CRP ≥50 mg/L: 91.2% vs. 36%, p < 0.001; admission troponin I ≥10 µg/L: 44.1% vs. 24.6%, p = 0.02; peak troponin I ≥50 mg/L: 64.7% vs. 44.1%, p = 0.028; peak NT-proBNP ≥400 pmol/L: 82.4% vs. 27.5%, p < 0.001).
TABLE 2.
Laboratory results of 245 STEMI patients with/without AKI on admission and during hospital stay
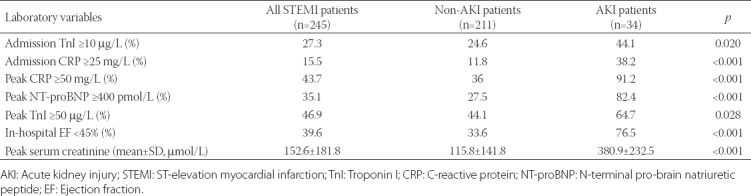
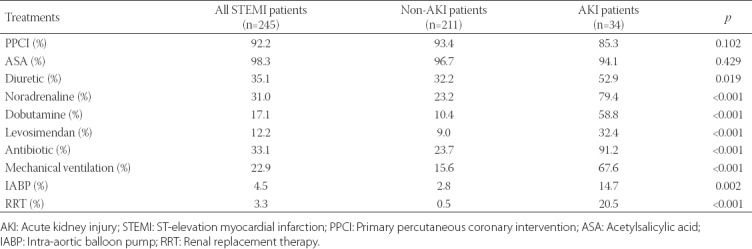
Table 3 shows treatments in 245 STEMI patients with/without AKI. PPCI was performed in 226/245 (92.2%) of STEMI patients. While there were no significant differences in the use of PPCI and ASA between AKI and non-AKI groups, significant differences were observed in the use of other medications and procedures, such as in the use of diuretics (52.9% vs. 32.2%, p = 0.019), noradrenaline (79.4% vs. 23.2%, p < 0.001), dobutamine (58.8% vs. 10.4%, p < 0.001), levosimendan (32.4% vs. 9%, p < 0.001), antibiotics (91.2% vs. 23.7%, p < 0.001), IABP (14.7% vs. 2.8%, p = 0.002), and renal replacement therapy (20.5% vs. 0.5%, p < 0.001).
TABLE 3.
Treatments in 245 STEMI patients with/without AKI
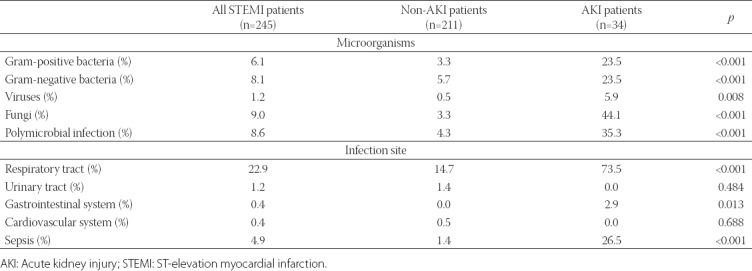
In-hospital complications of 245 STEMI patients with/without AKI are presented in Table 4. STEMI patients with AKI significantly more frequently developed in-hospital AHF (70.6% vs. 17.5%, p < 0.001) and acquired HAI [79.4% vs. 18%, p < 0.001] (Table 4). In addition, we analyzed the site and cause of infection. Different bacterial as well as fungal infections were recorded in STEMI patients. The respiratory system was the most frequent site of infection, especially in AKI group (Table 5).
TABLE 4.
In-hospital complications of 245 STEMI patients with/without AKI
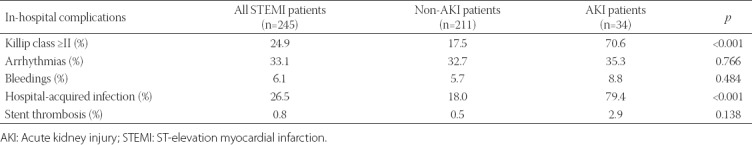
TABLE 5.
Cause and site of hospital-acquired infection in 245 STEMI patients with/without AKI
Among 245 STEMI patients, in-hospital mortality was 13.5%, 30-day was 18.4%, and 6-month was 21.6%. We observed significant differences in mortality between AKI and non-AKI group, as follows: 52.9% AKI vs.7.1% non-AKI for in-hospital mortality (p < 0.001), 64.7% vs.10.7% for 30-day mortality (p < 0.001), and 70.6% vs. 13.7% for 6-month mortality [p < 0.001] (Figure 1).
FIGURE 1.
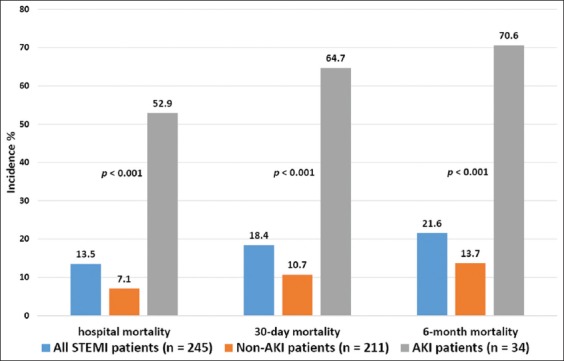
In-hospital, 30-day, and 6-month mortality in 245 STEMI patients with/without AKI. Significant differences were observed in mortality between AKI and non-AKI group, as follows: 52.9% AKI vs. 7.1% non-AKI for in-hospital mortality, 64.7% vs. 10.7% for 30-day mortality, and 70.6% vs. 13.7% for 6-month mortality (all p < 0.001). AKI: Acute kidney injury; STEMI: ST-elevation myocardial infarction.
The logistic regression analysis showed that significant independent predictors of AKI in STEMI patients were resuscitation before admission (OR 4.171, 95% CI 1.088–15.998, p = 0.037), HAI (OR 7.974, 95% CI 1.992–31.912, p = 0.003), and peak NT-proBNP ≥400 pmol/L (OR 21.261, 95% CI 2.357–191.795, p = 0.006) which is indicative of AHF (Table 6).
TABLE 6.
Logistic regression analysis (Wald statistics) of predictors of AKI in 245 STEMI patients
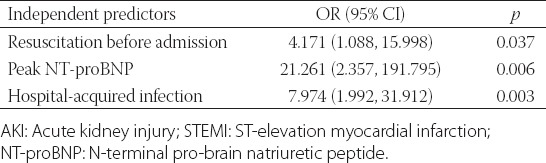
Table 7 shows clinical variables that were significantly associated with in-hospital mortality in 245 STEMI patients, which included: age ≥65 years (66.7% nonsurvivors vs. 40.1% survivors, p = 0.005), arterial hypertension (69.7% vs. 57.5%, p = 0.049), admission Killip class ≥II (51.5% vs. 11.8%, p < 0.001), in-hospital Killip class ≥II (75.8% vs. 17%, p < 0.001), resuscitation prior to admission (45.5% vs. 11.3%, p < 0.001), admission CRP ≥25 mg/L (51.5% vs. 9.9%, p < 0.001), peak CRP ≥50 mg/L (87.9% vs. 36.8%, p < 0.001), peak NT-proBNP ≥400 pmol/L (72.7% vs. 29.2%, p < 0.001), EF <45% (75.8% vs. 34%, p < 0.001), HAI (69.7% vs. 19.8%, p < 0.001), and AKI (54.5% vs. 7.5%, p < 0.001).
TABLE 7.
Clinical variables significantly associated with in-hospital mortality in 245 STEMI patients
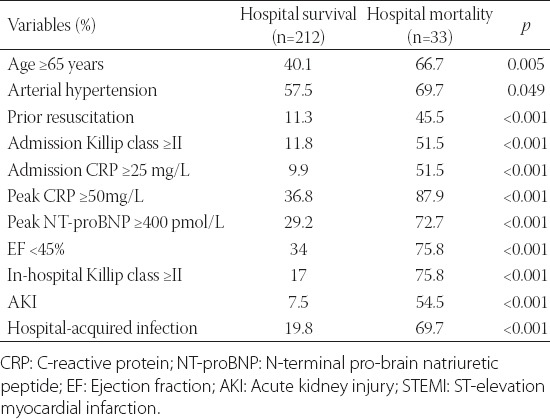
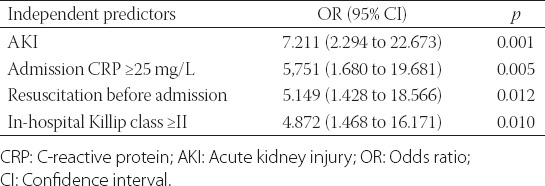
According to the logistic regression analysis, significant independent predictors of in-hospital mortality in STEMI patients were AKI (OR 7.211, 95% CI 2.294–22.673, p = 0.001), admission CRP ≥25 mg/L (OR 5.751, 95% CI 1.680–19.681, p = 0.005), successful resuscitation before admission (OR 5.149, 95% CI 1.428–18.566, p = 0.012) and in-hospital AHF categorized as Killip class ≥II [OR 4.872, 95% CI 1.468–16.171, p = 0.010] (Table 8).
TABLE 8.
Logistic regression analysis (Wald statistics) of predictors of in-hospital mortality in 245 STEMI patients
DISCUSSION
While contrast exposure has been considered as a primary risk factor for AKI in STEMI patients undergoing PPCI, recent studies have suggested that factors other than contrast media are major contributors to renal dysfunction in this patient population. Recommendations to prevent contrast-induced AKI include the use of iso-osmolar or low-osmolar contrast media in the lowest possible dose and hydration with I.V. crystalloid fluids [5,7,14]. The major finding of our study is that AKI developed in 13.9% of high-risk STEMI patients, despite the preventive measures were taken. We used a new generation of non-ionic, water-soluble iodinated contrast media with low osmolality and viscosity during early PPCI and I.V. crystalloid infusion after PPCI. Furthermore, we showed that AKI was significantly associated with increased early- and long-term mortality in high-risk STEMI patients. Variables identified as significant and independent predictors of AKI were peak NT-proBNP ≥400 pmol/L, which is indicative of AHF, as well as HAI and resuscitation before admission.
In previous studies, the incidence of AKI in STEMI or acute coronary syndrome (ACS) patients, based on the AKIN or KDIGO criteria, ranged between 10% and18% [3,11,12,19-21]. Moreover, Shacham et al. reported that the AKI incidence was 6.2% in STEMI patients with preserved EF before PPCI [10]. Consistent with previous studies, the incidence of AKI was 13.9% in our high-risk STEMI patients.
In the current study, AKI was significantly associated with AHF on admission or during hospital stay, assessed using the Killip classification. The clinical diagnosis of AHF was confirmed by increased levels of NT-proBNP and decreased EF (<45%). Reduced EF indicates the loss of contractility due to acute ischemia or myocardial necrosis [5,15]. In our STEMI patients, reduced EF was associated with Killip class ≥II, especially in the subset of patients who developed AKI. Clinical studies including STEMI patients showed that high NT-proBNP, associated with hypotension, hyponatremia, venous congestion and cardiorenal syndrome, is a risk factor for AKI [9,22,23]. AHF leads to reduced renal blood flow which activates the sympathetic and renin-angiotensin-aldosterone systems and induces ventricular remodeling [24]. In addition, low cardiac output, tubuloglomerular feedback, increased intra-abdominal pressure or increased venous pressure may result in kidney congestion [24]. Similar to our results, other studies on STEMI patients undergoing PPCI showed that AHF was an independent predictor of AKI [2,8,11,12,21,25,26].
Other frequent comorbidities in our patients with AKI were diabetes and prior MI, suggesting that they contribute to renal dysfunction in STEMI patients [5].
In this study, we confirmed the important role of infection in STEMI patients with AKI, as HAIs were significantly more common in AKI compared to non-AKI group. Annually, HAIs affect 5–10% of all inpatients and 25% of ICU patients. A study investigating the prevalence and clinical impact of major infections among 11,879 hospitalized STEMI patients in Florida, during 2006, showed that infections were present in 16% of those patients [27]. The most prevalent HAIs were urinary tract infections, pneumonia, surgical site infections, and bloodstream infections [27]. The risk of infections was increased by comorbidities, AKI, AHF, major surgical procedures, and indwelling catheters, among other factors. HAIs in STEMI patients resulted in prolonged hospital stays and adverse clinical outcomes, including in-hospital mortality [27].
Increased inflammatory markers, such as white blood cell (WBC)/leukocyte count and CRP, in STEMI patients may be due to infection or, more often, due to recruitment of leukocytes to the site of injury in the myocardium [9]. Infiltrating leukocytes are the source of inflammatory cytokines such as interleukin (IL)-1β, IL-6, IL-10, and tumor necrosis factor (TNF)-α, where especially IL-1β and IL-6 are associated with higher CRP levels [9,28-30]. In AKI, activated inflammatory cells in the renal interstitium produce free oxygen radicals and potent vasoconstrictors leading to tubular or vascular injury. Another mechanism is direct endothelial injury via endothelin release and NO decrease [31]. Moreover, inflammation due to severe infection activates coagulation pathways, leading to microvascular dysfunction, endothelial, mitochondrial and tubular damage - all of which impair renal function [31]. Infection in AKI patients is also associated with more frequent use of antibiotics, including nephrotoxic drugs, which additionally worsen kidney function [13].
Diuretic therapy and MV, used in patients with AHF and respiratory failure, increase the risk of AKI [32], and similar was observed in our study. The underlying mechanisms may include hemodynamic factors, selective renal vasoconstriction activated by MV-induced sympathetic stimulation, and inflammatory response to ventilator-induced barotrauma, leading to renal hypoperfusion [32-34]. Moreover, HAIs of the lungs generally worsen pulmonary congestion. Additional studies are needed to determine to what extent MV and treatment of heart failure contribute to the development of AKI in hemodynamically unstable STEMI patients.
In addition to peak NT-proBNP ≥400 pmol/L and HAI, prior resuscitation was an independent predictor of AKI in our STEMI patients. In resuscitated patients, cardiogenic shock with systemic hypoperfusion contributes to the development of AKI. Similar findings were reported in other studies [19].
A quarter of all our STEMI patients and 40% of STEMI patients with AKI had a history of diabetes. Even in the absence of diabetes mellitus, acute hyperglycemia on admission was associated with increased in-hospital mortality in patients with acute myocardial infarction (AMI) [35]. Moreover, in those patients, admission acute hyperglycemia was an independent predictor of AKI [35] and, similarly, in patients with ACS preprocedural hyperglycemia was a predictor of contrast-induced AKI [35]. Hyperglycemia has a negative effect on ischemic myocardium through mechanisms such as oxidative stress, inflammation, apoptosis, endothelial dysfunction, and platelet aggregation [36].
Finally, we showed that AKI was associated with significantly increased mortality (i.e. in-hospital, 30-day, and 6-month mortality) in high-risk STEMI patients. Previous studies also reported the association of AKI with higher short- and long-term mortality rates in patients with MI or ACS [3,10,12,19], including higher 5-year all-cause mortality in STEMI patients with preserved left LV function [10]. Moreover, lower baseline GFR was associated with AKI and increased mortality in STEMI patients [10,12]. A meta-analysis analyzing the impact of AKI on mortality risk in patients with ACS showed more than a 3-fold and 2-fold increase in short- and long-term mortality, respectively [37].
Our study has several limitations. First, we acknowledge all limitations associated with the study design (i.e., single-center, retrospective study). Second, the incidence of AKI may have been underestimated in patients who died within the first few hours of hospital admission, as changes in serum creatinine levels were not assessed in those patients. Third, I.V. crystalloid infusion was based on the hemodynamic status of each STEMI patient individually. Finally, we generally defined AKI as at least 50% increase in serum creatinine, and did not classify patients according to AKI severity.
CONCLUSION
We showed that resuscitation before admission, HAI, and peak NT-proBNP ≥400 pmol/L were significant independent predictors of AKI in high-risk STEMI population. To prevent AKI in STEMI patients, the recommended measures should be implemented, including the use of iso-osmolar or low-osmolar contrast media in the lowest possible dose during PPCI and hydration with I.V. crystalloid fluids to achieve adequate intravascular volume. Additional measures include early diagnosis and treatment of AHF and HAIs in STEMI patients, especially lung infection.
DECLARATION OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
- 1.Marenzi G, Cosentino N, Bartorelli AL. Acute kidney injury in patients with acute coronary syndromes. Heart. 2015;101(22):1778–85. doi: 10.1136/heartjnl-2015-307773. https://doi.org/10.1136/heartjnl-2015-307773. [DOI] [PubMed] [Google Scholar]
- 2.Vavalle JP, van Diepen S, Clare RM, Hochman JS, Weaver WD, Mehta RH, et al. Renal failure in patients with ST-segment elevation acute myocardial infarction treated with primary percutaneous coronary intervention:Predictors, clinical and angiographic features, and outcomes. Am Heart J. 2016;173:57–66. doi: 10.1016/j.ahj.2015.12.001. https://doi.org/10.1016/j.ahj.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Wiviott SD. Short-term outcomes of acute myocardial infarction in patients with acute kidney injury:A report from the National Cardiovascular Data Registry. Circulation. 2012;125(3):497–504. doi: 10.1161/CIRCULATIONAHA.111.039909. https://doi.org/10.1161/CIRCULATIONAHA.111.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brogan RA, Malkin CJ, Batin PD, Simms AD, McLenachan JM, Gale CP. Risk stratification for ST segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. World J Cardiol. 2014;6(8):865–73. doi: 10.4330/wjc.v6.i8.865. https://doi.org/10.4330/wjc.v6.i8.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation:The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–77. doi: 10.1093/eurheartj/ehx393. https://doi.org/10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 6.Mehta RL, Kellum JA, V Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network:Report of an initiative to improve outcomes in acute kidney injury. Critical Care. 2007;11(2):R31. doi: 10.1186/cc5713. https://doi.org/10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84. doi: 10.1159/000339789. https://doi.org/10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 8.Narula A, Mehran R, Weisz G, Dangas GD, Yu J, Genereux P, et al. Contrast-induced acute kidney injury after primary percutaneous coronary intervention:Results from the HORIZONS-AMI substudy. Eur Heart J. 2014;35(23):1533–40. doi: 10.1093/eurheartj/ehu063. https://doi.org/10.1093/eurheartj/ehu063. [DOI] [PubMed] [Google Scholar]
- 9.Ortega-Hernandez J, Springall R, Sanchez-Munoz F, Arana-Martinez JC, Gonzalez-Pacheco H, Bojalil R. Acute coronary syndrome and acute kidney injury:Role of inflammation in worsening renal function. BMC Cardiovasc Disord. 2017;17(1):202. doi: 10.1186/s12872-017-0640-0. https://doi.org/10.1186/s12872-017-0640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shacham Y, Gal-Oz A, Ben-Shoshan J, Keren G, Arbel Y. Prognostic implications of acute renal impairment among ST elevation myocardial infarction patients with preserved left ventricular function. Cardiorenal Med. 2016;6(2):143–9. doi: 10.1159/000443621. https://doi.org/10.1159/000443621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matejka J, Varvarovsky I, Rozsival V, Herman A, Blaha K, Vecera J, et al. Heart failure is the strongest predictor of acute kidney injury in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction. Kardiol Pol. 2016;74(1):18–24. doi: 10.5603/KP.a2015.0115. https://doi.org/10.5603/KP.a2015.0115. [DOI] [PubMed] [Google Scholar]
- 12.Schmucker J, Fach A, Becker M, Seide S, Bunger S, Zabrocki R, et al. Predictors of acute kidney injury in patients admitted with ST-elevation myocardial infarction - results from the Bremen STEMI-Registry. Eur Heart J Acute Cardiovasc Care. 2017;7(8):710–22. doi: 10.1177/2048872617708975. https://doi.org/10.1177/2048∖17708975. [DOI] [PubMed] [Google Scholar]
- 13.Perazella MA, Luciano RL. Review of select causes of drug-induced AKI. Expert Rev Clin Pharmacol. 2015;8(4):367–71. doi: 10.1586/17512433.2015.1045489. https://doi.org/10.1586/17512433.2015.1045489. [DOI] [PubMed] [Google Scholar]
- 14.Kaltsas E, Chalikias G, Tziakas D. The incidence and the prognostic impact of acute kidney injury in acute myocardial infarction patients:Current preventive strategies. Cardiovasc Drugs Ther. 2018;32(1):81–98. doi: 10.1007/s10557-017-6766-6. https://doi.org/10.1007/s10557-017-6766-6. [DOI] [PubMed] [Google Scholar]
- 15.Mello BH, Oliveira GB, Ramos RF, Lopes BB, Barros CB, Carvalho Ede O, et al. Validation of the Killip-Kimball classification and late mortality after acute myocardial infarction. Arq Bras Cardiol. 2014;103(2):107–17. doi: 10.5935/abc.20140091. https://doi.org/10.5935/abc.20140091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calandra T, Cohen J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005;33(7):1538–48. doi: 10.1097/01.ccm.0000168253.91200.83. https://doi.org/10.1097/01.CCM.0000168253.91200.83. [DOI] [PubMed] [Google Scholar]
- 17.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials:A consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449. https://doi.org/10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 18.Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury:A critical and comprehensive review. Clin Kidney J. 2013;6(1):8–14. doi: 10.1093/ckj/sfs160. https://doi.org/10.1093/ckj/sfs160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marenzi G, Cabiati A, Bertoli SV, Assanelli E, Marana I, De Metrio M, et al. Incidence and relevance of acute kidney injury in patients hospitalized with acute coronary syndromes. Am J Cardiol. 2013;111(6):816–22. doi: 10.1016/j.amjcard.2012.11.046. https://doi.org/10.1016/j.amjcard.2012.11.046. [DOI] [PubMed] [Google Scholar]
- 20.Bruetto RG, Rodrigues FB, Torres US, Otaviano AP, Zanetta DM, Burdmann EA. Renal function at hospital admission and mortality due to acute kidney injury after myocardial infarction. PLoS One. 2012;7(4):e35496. doi: 10.1371/journal.pone.0035496. https://doi.org/10.1371/journal.pone.0035496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shacham Y, Steinvil A, Arbel Y. Acute kidney injury among ST elevation myocardial infarction patients treated by primary percutaneous coronary intervention:A multifactorial entity. J Nephrol. 2016;29(2):169–74. doi: 10.1007/s40620-015-0255-4. https://doi.org/10.1007/s40620-015-0255-4. [DOI] [PubMed] [Google Scholar]
- 22.Akgul O, Uyarel H, Pusuroglu H, Isiksacan N, Turen S, Erturk M, et al. High BNP level as risk factor for acute kidney injury and predictor of all-cause mortality in STEMI patients. Herz. 2014;39(4):507–14. doi: 10.1007/s00059-013-3853-8. https://doi.org/10.1007/s00059-013-3853-8. [DOI] [PubMed] [Google Scholar]
- 23.Han SW, Ryu KH. Renal dysfunction in acute heart failure. Korean Circ J. 2011;41(10):565–74. doi: 10.4070/kcj.2011.41.10.565. https://doi.org/10.4070/kcj.2011.41.10.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afsar B, Ortiz A, Covic A, Solak Y, Goldsmith D, Kanbay M. Focus on renal congestion in heart failure. Clin Kidney J. 2016;9(1):39–47. doi: 10.1093/ckj/sfv124. https://doi.org/10.1093/ckj/sfv124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ando G, Morabito G, de Gregorio C, Trio O, Saporito F, Oreto G. Age, glomerular filtration rate, ejection fraction, and the AGEF score predict contrast-induced nephropathy in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Catheter Cardiovasc Interv. 2013;82(6):878–85. doi: 10.1002/ccd.25023. https://doi.org/10.1002/ccd.25023. [DOI] [PubMed] [Google Scholar]
- 26.Tung YC, Chang CH, Chen YC, Chu PH. Combined biomarker analysis for risk of acute kidney injury in patients with ST-segment elevation myocardial infarction. PLoS One. 2015;10(4):e0125282. doi: 10.1371/journal.pone.0125282. https://doi.org/10.1371/journal.pone.0125282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nash MC, Strom JA, Pathak EB. Prevalence of major infections and adverse outcomes among hospitalized ST-elevation myocardial infarction patients in Florida, 2006. BMC Cardiovasc Disord. 2011;11:69. doi: 10.1186/1471-2261-11-69. https://doi.org/10.1186/1471-2261-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruparelia N, Digby JE, Jefferson A, Medway DJ, Neubauer S, Lygate CA, et al. Myocardial infarction causes inflammation and leukocyte recruitment at remote sites in the myocardium and in the renal glomerulus. Inflamm Res. 2013;62(5):515–25. doi: 10.1007/s00011-013-0605-4. https://doi.org/10.1007/s00011-013-0605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stuveling EM, Hillege HL, Bakker SJ, Gans RO, De Jong PE, De Zeeuw D. C-reactive protein is associated with renal function abnormalities in a non-diabetic population. Kidney Int. 2003;63(2):654–61. doi: 10.1046/j.1523-1755.2003.00762.x. https://doi.org/10.1046/j.1523-1755.2003.00762.x. [DOI] [PubMed] [Google Scholar]
- 30.Shacham Y, Leshem-Rubinow E, Steinvil A, Keren G, Roth A, Arbel Y. High sensitive C-reactive protein and the risk of acute kidney injury among ST elevation myocardial infarction patients undergoing primary percutaneous intervention. Clin Exp Nephrol. 2015;19(5):838–43. doi: 10.1007/s10157-014-1071-1. https://doi.org/10.1007/s10157-014-1071-1. [DOI] [PubMed] [Google Scholar]
- 31.Akcay A, Nguyen Q, Edelstein CL. Mediators of inflammation in acute kidney injury. Mediators Inflamm. 2009;2009:137072. doi: 10.1155/2009/137072. https://doi.org/10.1155/2009/137072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van den Akker JP, Egal M, Groeneveld AB. Invasive mechanical ventilation as a risk factor for acute kidney injury in the critically ill:A systematic review and meta-analysis. Crit Care. 2013;17(3):R98. doi: 10.1186/cc12743. https://doi.org/10.1186/cc12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Husain-Syed F, Slutsky AS, Ronco C. Lung-kidney cross-talk in the critically ill patient. Am J Respir Crit Care Med. 2016;194(4):402–14. doi: 10.1164/rccm.201602-0420CP. https://doi.org/10.1164/rccm.201602-0420CP. [DOI] [PubMed] [Google Scholar]
- 34.Liu KD, Matthay MA. Advances in critical care for the nephrologist:Acute lung injury/ARDS. Clin J Am Soc Nephrol. 2008;3(2):578–86. doi: 10.2215/CJN.01630407. https://doi.org/10.2215/CJN.01630407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin KY, Shang XL, Guo YS, Zhu PL, Wu ZY, Jiang H, et al. Association of preprocedural hyperglycemia with contrast-induced acute kidney injury and poor outcomes after emergency percutaneous coronary intervention. Angiology. 2018;69(9):770–8. doi: 10.1177/0003319718758140. https://doi.org/10.1177/0003319718758140. [DOI] [PubMed] [Google Scholar]
- 36.Moriyama N, Ishihara M, Noguchi T, Nakanishi M, Arakawa T, Asaumi Y, et al. Admission hyperglycemia is an independent predictor of acute kidney injury in patients with acute myocardial infarction. Circ J. 2014;78(6):1475–80. doi: 10.1253/circj.cj-14-0117. https://doi.org/10.1253/circj.CJ-14-0117. [DOI] [PubMed] [Google Scholar]
- 37.Pickering JW, Blunt IRH, Than MP. Acute kidney injury and mortality prognosis in acute coronary syndrome patients:A meta-analysis. Nephrology. 2018;23(3):237–46. doi: 10.1111/nep.12984. https://doi.org/10.1111/nep.12984. [DOI] [PubMed] [Google Scholar]


