Abstract
Young adults (18–39 year-olds) with hypertension have a higher lifetime risk for cardiovascular disease. However, less than 50% of young adults achieve hypertension control in the United States. Hypertension self-management programs are recommended to improve control, but have been targeted to middle-aged and older populations. Young adults need hypertension self-management programs (i.e., home blood pressure monitoring and lifestyle modifications) tailored to their unique needs to lower blood pressure and reduce the risks and medication burden they may face over a lifetime. To address the unmet need in hypertensive care for young adults, we developed MyHEART (My Hypertension Education And Reaching Target), a multi-component, theoretically-based intervention designed to achieve self-management among young adults with uncontrolled hypertension. MyHEART is a patient-centered program, based upon the Self-Determination Theory, that uses evidence-based health behavior approaches to lower blood pressure. Therefore, the objective of this study is to evaluate MyHEART’s impact on changes in systolic and diastolic blood pressure compared to usual care after 6 and 12 months in 310 geographically and racially/ethnically diverse young adults with uncontrolled hypertension. Secondary outcomes include MyHEART’s impact on behavioral outcomes at 6 and 12 months, compared to usual clinical care (increased physical activity, decreased sodium intake) and to examine whether MyHEART’s effects on self-management behavior are mediated through variables of perceived competence, autonomy, motivation, and activation (mediation outcomes). MyHEART is one of the first multicenter, randomized controlled hypertension trials tailored to young adults with primary care. The design and methodology will maximize the generalizability of this study.
Keywords: Hypertension, Young adults, Randomized controlled trial, Self-management, Health behavior change, Health coaching
1. Introduction
Uncontrolled hypertension in young adults is an enormous public health burden in the United States [1–3]. Over 10 million 18–39 year-olds (1 in 5 men; 1 in 6 women) have hypertension [4–6], increasing their risk of premature heart failure, stroke, and chronic kidney disease [7, 8]. Hypertension control reduces morbidity, mortality, and future healthcare costs [9–13]; yet, less than 50% of young adults with hypertension in the U.S. have achieved blood pressure control, even with the former blood pressure guidelines (<140/90 mmHg) [4, 14–17].
While hypertension self-management programs targeted towards adults ≥50 years old reduce blood pressure [18–36], they primarily focus on medication titration [37]. In contrast, lifestyle modifications are commonly the initial hypertension treatment step, rather than a medication, among young adults [4, 38]. Therefore, young adults need tailored hypertension self-management (home blood pressure monitoring and lifestyle modifications) to lower blood pressures and reduce the amount of medication they may need over a lifetime [39–42]. In contrast to older adults, young adulthood is a time of frequent healthcare and vocational transitions, new life responsibilities, and less interest in health-related goals (i.e., prevention of heart attack and stroke) [43, 44]. Thus, the content and method of delivery of hypertension self-management must be individualized to young adults and address barriers specific to this population [45–47].
To address the unmet need in hypertensive care for young adults, we developed MyHEART (My Hypertension Education And Reaching Target), a multi-component, theoretically-based intervention designed to achieve self-management among young adults with uncontrolled hypertension [48]. MyHEART is a patient-centered program that uses evidence-based health behavior approaches to lower blood pressure. MyHEART was developed by young adults and other stakeholders [44, 49], and differs from previous interventions by: 1) targeting barriers identified by young adults in our preliminary research, 2) tailoring the mode of delivery to preferences expressed by members of this age group, and 3) individualizing action plans to participants’ motivations and behavior goals. MyHEART is founded on the self-determination theory (SDT) [50], which is used to support chronic disease self-management and lifestyle modifications. SDT acknowledges that young adults are more likely to adopt and maintain health behaviors with: 1) autonomous (internal) motivation, instead of external motivation (i.e., external pressure), 2) relatedness (i.e., supportive healthcare interactions), and 3) perceived self-competence (i.e., perceived self-efficacy [51, 52]; confidence in starting and maintaining behaviors to reach a goal) [50, 53–59]. We successfully conducted a 3-month pilot study of MyHEART to establish feasibility and participant satisfaction [48], which informed the design of this multisite randomized controlled trial.
Therefore, the overall objective of this study is to evaluate MyHEART’s impact on blood pressure among 310 geographically and racially/ethnically diverse young adults within two large, Midwestern healthcare systems. Our co-primary outcomes are changes in systolic and diastolic blood pressure after 6 and 12 months in young adults (18–39 year-olds) with uncontrolled hypertension. In this article, we report on the study design, procedures, and development of the MyHEART intervention protocol.
2. Study Design
2.1. Overview of Study Design
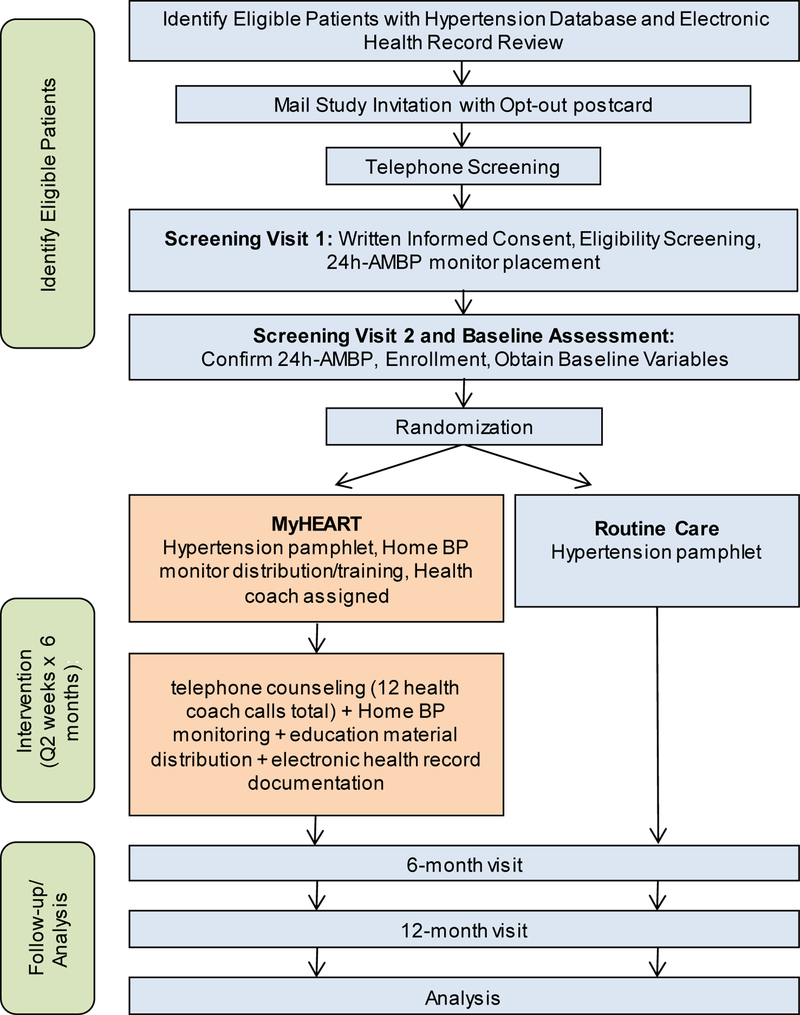
MyHEART is a randomized, controlled clinical trial, across two large, Midwestern healthcare systems: UW Health (Madison, WI; 25 academic and rural clinics) and Aurora Health Care (Milwaukee, WI; 31 urban community clinics). The primary objective is to evaluate the MyHEART intervention (hypertension self-management) compared to usual care on changes in systolic and diastolic blood pressure from baseline to 6 and 12 months in young adults (18–39 year-olds) with uncontrolled hypertension. The sites differ in patient demographics, races/ethnicities, and payor mix, supporting generalizability of the results. The study schema is presented in Figure 1. Prior to initiating the protocol, all study sites received institutional review board (IRB) approval from the University of Wisconsin-Madison Health Sciences IRB and the Wisconsin IRB Consortium.
Figure 1.
Eligibility, Enrollment, Randomization, Follow-up, and Analysis
2.2. Inclusion and Exclusion Criteria
Each healthcare system has an electronic health record (EHR) with a Wisconsin Collaborative for Healthcare Quality (WCHQ) hypertension registry that will be used to screen and identify potentially eligible patients [60]. Founded in 2003, WCHQ is a voluntary consortium of 37 Wisconsin healthcare organizations (physician groups, hospitals, health plans) that has led the nation in measuring and reporting healthcare quality. The WCHQ definition created for public reporting is based on the Healthcare Effectiveness Data and Information Set (HEDIS) metrics [60–62]. The research sites have reported metrics for complicated and uncomplicated hypertension to WCHQ since 2005.
The inclusion and exclusion criteria are summarized in Table 1. Potentially eligible patients in the EHR hypertension registry must: 1) be 18–39 years old at the start of the study, 2) have a minimum of two hypertension ICD-10 coded office visits with any provider (physician [MD or DO, including resident physician], physician assistant [PA], or nurse practitioner [NP]) on different dates in the last 24 months prior to eligibility assessment, with at least one code in the past 18 months, and 3) be medically homed (i.e., receiving routine primary care within the healthcare system) within their specific healthcare site [63]. The last two clinic blood pressures will determine eligibility for a study invitation; the blood pressures must include a systolic ≥140 mmHg and/or diastolic ≥90 mmHg [9], and the last blood pressure must be within the last 90 days. If multiple blood pressures were recorded on the same day of service, the average of the last two blood pressures on that date will be used. At the time of study design and protocol implementation, the diagnostic blood pressure threshold for hypertension was ≥140/90 mmHg [9, 15], which will be continued throughout the study. After publication of the 2017 AHA/ACC Guidelines [4], there were implementation delays across some health systems; therefore, a diagnostic threshold of ≥140/90 mmHg will be maintained for consistency. Blood pressures from inpatient, emergency room, and urgent care visits and self-reported blood pressures are excluded. Patients who are currently using antihypertensive medication or have initiated lifestyle modifications are also included. Due to limitations with administrative data [64], some exclusion criteria will be assessed by manual chart abstraction and self-report. Illegal drug use will not be reported.
Table 1.
Study Eligibility Criteria
| Inclusion Criteria |
|---|
| 1. Willing and capable of giving written informed consent |
| 2. Willing to comply with all study procedures and be available for the duration of the study |
| 3. Males and females ages 18–39 years old at the start of the study (inclusive) |
| 4. A minimum of two hypertension ICD-10 coded visits with a provider (MD, DO, PA, NP) on different dates in the last 24 months, with at least one code in the past 18 months |
| 5. Medically homed at UW Health or Aurora Health Care |
| Exclusion Criteria |
| 1. History of medically determined Congestive Heart Failure |
| 2. Unable to provide informed consent (i.e., activated healthcare power of attorney) |
| 3. Unable or unwilling to travel to local clinic for research visits |
| 4. Currently residing in a skilled nursing facility |
| 5. Diagnosed with sickle cell anemia or cystic fibrosis |
| 6. Diagnosed with stroke, myocardial infarction, and/or coronary artery revascularization in the past 2 years |
| 7. Syncope while exercising or doing strenuous activity within past 12 months |
| 8. Currently prescribed warfarin, novel oral anticoagulant, or insulin |
| 9. Planned organ transplant or prior transplant in the past 5 years |
| 10. Chemotherapy or radiation therapy within 6 the past months |
| 11. Severely impaired hearing, vision, or speech, as determined by study staff responsible for enrollment |
| 12. Current participation or planning to participate in another clinical trial in the next 12 months |
| 13. Pregnant or planning to become pregnant in the next 12 months |
| 14. Planning to leave the geographic area in the next 6 months |
| 15. Health condition that will limit both increasing physical activity and changing diet |
| 16. Illegal drug use (other than marijuana) in the past 30 days |
| 17. Unable to read or communicate in English |
| 18. Currently on dialysis or seeing a Nephrologist |
| 19. Between-arm blood pressure difference ≥20 mmHg |
| 20. White Coat Hypertension (24-hour ambulatory monitoring) |
| 21. Inability to comply with or complete the protocol or other reasons at the discretion of the principal and site investigators |
| 22. Currently residing in correctional facility |
2.3. Participant Recruitment and Eligibility Screening
The names and contact information of potentially eligible patients were made available to the respective study coordinators at each site. The site coordinators will mail an introductory research packet, which was designed by racially/ethnically diverse patient stakeholders, approved by primary care leaders, and used in the pilot study [48]. The introductory packet includes a flyer summarizing MyHEART and a pre-paid opt-out postcard. If an opt-out response is not received 2 weeks after the mailing, research staff will call patients to assess eligibility and subsequently invite them for a face-to-face visit at the research clinic within their medically homed region. Participants who answer the phone will be asked to provide verbal consent solely for the phone screening. We will recruit a total of 310 participants over 27 months. Additional IRB-approved recruitment efforts include community flyer distribution, print advertising, clinical panel review, and social media.
Potential participants who completed the telephone screen will be invited for a screening visit (Visit 1) for additional eligibility assessment. Written informed consent for this study will be obtained at the start of this in-person visit, which will include authorization for additional screening/eligibility assessment [65]. After obtaining written informed consent, blood pressures will be measured during the visit after the patient rests for 5 minutes in the seated position. An appropriately sized [66] blood pressure cuff will be connected to an automated sphygmomanometer (Dinamap; GE). Each site will have the following cuff sizes available: small adult (for arm circumference of 17–22 cm), regular adult (22–32 cm), large adult (32–42 cm), and extra-large adult (42–50 cm). A blood pressure will be obtained on the right upper arm, then the left upper arm, for the initial assessment. Right arm blood pressures will be subsequently used for the initial and follow-up visits unless the left arm systolic blood pressure is ≥10 mmHg higher. If a participant’s body habitus is not compatible with the cuff sizes, the individual will be excluded. The average of the second and third systolic and diastolic pressures will define the baseline clinic blood pressure [67]. The primary care provider will be notified if the between-arm blood pressure difference is ≥20 mmHg [68], and the participant will be excluded. All remaining eligible patients who complete clinic blood pressures will receive their clinic blood pressure in written format from Visit 1 and will then receive an ambulatory blood pressure (AMBP) monitor (SpaceLabs 90277) [69] for 24-hour blood pressure monitoring. AMBP monitoring is recommended to confirm a hypertension diagnosis (i.e., exclude white coat hypertension) [4, 17, 70, 71]. The U.S. Preventive Services Task Force noted up to 65% of patients with high office blood pressures were not diagnosed with hypertension after AMBP monitoring [71].
2.4. Participant Enrollment and Randomization
Patients will return the AMBP monitor the next business day (Visit 2). Patients are eligible if the mean 24-hour AMBP is a systolic ≥130 mmHg and/or diastolic ≥80 mmHg and/or the mean awake AMBP is a systolic ≥135 mmHg and/or diastolic ≥85 mmHg [71, 72]. If there is white coat hypertension, the patient is ineligible and their primary care provider will be notified; the patient is also ineligible if on blood pressure medication(s) with controlled hypertension. Remaining eligible patients will be enrolled, randomized to MyHEART or usual care, and will complete the baseline assessment. The primary care provider will also be notified of all enrolled patients via the EHR; provider permission for study participation is not needed given the broad exclusion criteria, lack of device/medication administration, and ongoing follow-up assessment. All participants will receive copies of their baseline, 6-, and 12-month average clinic blood pressures to share with their provider [31].
Randomization assignments will be generated by the University of Wisconsin-Madison Biostatistics Data Coordinating Center using permuted block in random block sizes, stratified by health system to ensure equal allocation. Study data will be collected and managed using the REDCap system hosted at the University of Wisconsin-Madison [73, 74]. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry, 2) audit trails for tracking data manipulation and export procedures, 3) automated export procedures for seamless data downloads to common statistical packages, and 4) procedures for importing data from external sources. The REDCap system will be used to verify eligibility prior to randomization.
To reduce bias, MyHEART assessors will be blinded to treatment assignments [75, 76]. Assessors will be trained to treat patients in both study groups identically per protocol [77]. Ambulatory monitoring will be the gold standard for blood pressure measurements. Primary care providers cannot be blinded since health coaches will document in the participants’ EHRs.
Usual care participants will receive hypertension clinical care per their primary care provider. This includes the possibility of receiving untailored self-management resources (i.e., dietician referral) at their provider’s discretion, but this is not systematically tailored to young adults’ needs. We will assess the number of healthcare team contacts in the usual care arm based on the number of primary care and specialty visits and dietician and exercise referrals after study enrollment [38, 43]. Usual care participants will receive a handout providing an overview of high blood pressure based upon the American Heart Association [77, 78]. It is usual care for patients to receive hypertension educational material when presenting for a hypertension visit. They will not receive home blood pressure monitors. Usual care participants will have the same 6- and 12-month assessments as the intervention arm.
3. The MyHEART intervention
3.1. MyHEART Theoretical Framework
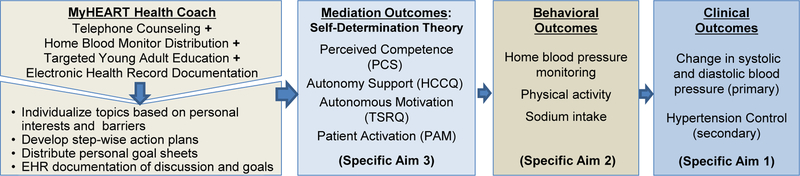
The conceptual model of MyHEART (Figure 1) is founded on the self-determination theory (SDT), which has been used in behavioral interventions across races/ethnicities and with young adults [79, 80]. To reduce the risk of negative sequelae from long-term hypertension, the goal is to not only initiate behaviors for blood pressure control, but also foster maintenance of new behaviors. Therefore, MyHEART incorporates important hypertension education components implemented by a health coach (Figure 2): 1) telephone-based self-management counseling, 2) home blood pressure monitoring, and 3) young adult-focused hypertension education. These components are recommended by the Institute of Medicine [81] and the American Heart Association [1]. Health coaching provides informational and emotional support for chronic disease management [82–84]. Telephone interventions increase contacts between patients and their healthcare teams [85–88]. MyHEART uses telephone as the primary mode of communication between participants and coaches because young adult community stakeholders indicated a preference for this mode of delivery compared to text messaging [44]. Young adults felt that it was easier to control the location and time of day they received health coaching by phone, in contrast to text messaging [44]. MyHEART will not initiate or titrate blood pressure medication. Participants randomized to the MyHEART intervention will continue to receive hypertension care from their primary care provider, including medication initiation and adjustments as clinically indicated. Intervention participants will receive the same hypertension overview [77] handout as the usual care participants.
Figure 2.
MyHEART Conceptual Model
3.2. MyHEART Health Coach
There will be four health coaches (two for each site) for telephone-based self-management counseling. MyHEART health coach certification options include an exercise physiologist (American College of Sports Medicine certification) with outpatient cardiovascular rehabilitation experience, or a cardiovascular registered nurse with at least 3 years of clinical experience including chronic disease management and adult education/counseling. The health coach will perform telephone counseling every 2 weeks over 6 months (12 calls total).
Based upon the self-determination theory, the interpersonal interaction between the coach and participant in MyHEART promotes relatedness and humanistic principles consistent with motivational interviewing [89]. The coaches’ goal over the 6 months of calls is to help participants establish self-management skills and maintain behaviors after MyHEART, i.e., sustainability of MyHEART. The content of coach-participant interactions will focus on: 1) highlighting discrepancies between participants’ current health behaviors and their desired behavior goals to promote internal motivation, 2) sharing reference points for guideline-recommended behaviors to lower blood pressure, and 3) discussing short-term goals and developing congruent action plans [90]. Coaches will promote autonomy by individualizing the order and depth of educational content based on the behavioral goals chosen by the participant [91–94]. Participants will have practical skill-building (e.g., label reading [95]) and coaches will encourage patients to set goals that are motivating but not overwhelming.
3.3. MyHEART Hypertension Education Modules
There are ten hypertension self-management modules (Table 2) for MyHEART that are based on our young adult focus groups [44], pilot study [48], previous interventions [21, 93, 96, 97], and hypertension guidelines [4, 9, 17]. All intervention participants will start with the home blood pressure monitoring module during the initial health coach session. The first follow-up phone call will address hypertension knowledge and review home blood pressure monitoring. Home blood pressure monitoring education will also be provided during all follow-up phone calls. The order of the remaining modules will be guided by participant’s choice and tailored to their goals [98, 99]. Fewer modules than calls allows some topics to be repeated as needed and per the participants’ requests. Current tobacco users will be referred to the Wisconsin Tobacco Quit Line (http://www.ctri.wisc.edu/quitline.html) when ready to attempt cessation and their primary care provider will be notified of their intention to quit via the EHR. The primary care provider will also be notified if the participant consumes >14 alcohol beverages/week for referral and follow-up [85]. The MyHEART team created handouts to include specific topics requested by our young adult focus groups [44]; additional handouts are from national organizations (e.g., NIH, American Heart Association, etc.). The MyHEART handouts were formatted with a Flesch-Kincaid readability of ≤6th grade [100]; the MyHEART modules and handouts were tailored to address cultural differences [101] given the higher prevalence of hypertension in Black young adults [102, 103].
Table 2.
MyHEART Educational Modules (Bold = young adult focused topics)
| Module | Topics |
|---|---|
| Home Blood Pressure Monitoring | How to measure blood pressure, include members in household to avoid isolation |
| Hypertension Knowledge | Define blood pressure, goal blood pressure, long-term health consequences |
| Low Sodium | Reading labels, effects of sodium on blood pressure, culturally appropriate cooking alternatives, eating with peers, meal planning, shopping on a budget |
| Dietary Approaches to Stop Hypertension (DASH) Eating Plan | DASH components, meal planning, grocery shopping on a budget, DASH with peers; Cultural and personal food preferences; Discuss cultural meaning of dietary practices |
| Weight Loss/Maintenance | Relationship of weight with hypertension, dietary and activity options to lose weight, time management, social support to assist with weight loss, fitness apps |
| Smoking Cessation* | Negative effects of tobacco on heart health, social/peer influence |
| Moderate Alcohol Consumption | Binge drinking**, negative effects on heart health; define quantity for types of alcohol [104] |
| Blood Pressure Medicine | Why medications may be needed, side effects, adherence, possible lifelong commitment, remembering medication, cost |
| Social Support | Local resources for support, reducing clinic no-shows, peer/social support [105] |
| Stress Management [106] | Identifying ways to reduce stress, stress with life’s transitions and new challenges |
Only for active tobacco users;
Only for participants identified as having alcohol consumption beyond AHA guidelines [107]
Following each health coach call, hypertension education handouts and personalized goal sheets with stepwise action plans will be available via email [108] and/or postal mail according to the participant’s preference [22]. Distribution of written educational materials is effective in multi-component interventions by reinforcing verbal discussions and supporting learning style differences [109]. Telephone encounters between the health coach and participants will be documented by the coach using our piloted EHR template. This is accessible by primary care providers and the patient’s care team [110] to review home blood pressures and lifestyle modifications which may reinforce participation.
3.4. MyHEART Home Blood Pressure Monitoring
Intervention participants will be provided an Omron BP760N home blood pressure monitor with an appropriate cuff size [111, 112]; it has been validated in young adults and across BMI categories [113]. Participants will receive training and practice on proper cuff placement and monitor use [24]. They will be asked to take their blood pressure at least three days a week, 2 measurements each time [19, 24]. To decrease missing data, participants will be able to read the recorded blood pressures to their health coach during phone calls [114] for entry into their EHR. Although all clinics have an EHR, automatic upload of home blood pressures into the EHR is not an active functionality with either healthcare system. Health coaches will review and discuss blood pressures during each telephone call. MyHEART coaches will also encourage clinic follow-up [115] based on the 2-week average home blood pressure. Participants will keep the blood pressure monitor after study completion. Malfunctioned monitors will be replaced during the study.
4. MyHEART Health Coach Training
Health coaches will receive training that builds on their prior education in motivational interviewing [89] and hypertension management, using self-determination theory concepts. Training intensity is based on prior studies [116] and resources from our pilot [48]. Trainers will observe health coaches with role playing and score adherence according to an a priori skills checklist, followed by problem solving and debriefing [117–119]. All health coaches will train together via in-person (8-hour session) and web-based (1-hour) sessions [120]. There will be two health coach trainers; the same trainers will be at all sessions to avoid degradation of instructional information, bias, and to accommodate trainee differences [117]. As with our pilot, required credentials of the lead health coach trainer include a doctorate-level degree in areas of behavior theory and motivational interviewing, with at least 3 years of clinical experience.
5. Study Fidelity
To ensure fidelity and reproducibility, research staff fidelity of data acquisition will be assessed by audits of clinic and ambulatory blood pressure techniques and review of REDCap data entry. Health coach fidelity will be evaluated using digital audio-recordings [121] of the coaches’ communications and review of their study documentation. Our health coach fidelity evaluation will include assessment of intervention delivery (content and dose), adherence to protocol, and the use of MyHEART’s coaching manual [122, 123]. Randomly, 10% of each type of call (i.e., baseline, follow-up, final) will be selected for assessment. Coaches will be evaluated using a modified Behavior Change Counseling Index (BECCI) to assess “how” the coach related to participants [124], a critical component of MyHEART. Questions were added from the Motivational Interviewing Treatment Integrity Measure 3.0 to include variables known to correlate with behavior change (i.e., goal setting, monitoring) [125, 126]. Fidelity will be assessed by doctorate-level nursing students. Fidelity assessment training will include one month of weekly meetings, with additional review of materials between meetings and practice with coding existing audio-visual files. Health coaches and research staff will receive monthly feedback to maintain or improve fidelity and minimize drift from protocol adherence [117–119, 124, 127–130].
6. Study Outcomes
6.1. Specific Aims and Hypotheses
The overall objective of this study is to evaluate MyHEART’s impact on blood pressure among 310 geographically and racially/ethnically diverse young adults. The co-primary outcomes are changes in systolic and diastolic blood pressure after 6 and 12 months in young adults (18–39 year-olds) with uncontrolled hypertension. The specific study aims are as follows:
Specific Aim 1.
To evaluate the effect of MyHEART (home blood pressure monitor distribution and heath coaching) on clinical outcomes, the change in systolic and diastolic blood pressure (primary) and hypertension control (secondary) after 6 and 12 months, compared to usual clinical care. We hypothesize that MyHEART will significantly decrease systolic and diastolic blood pressures (clinic and 24-hour ambulatory) and increase hypertension control in young adults, compared to usual clinical care.
Specific Aim 2.
To evaluate the effect of MyHEART on hypertension self-management behavior (behavioral outcomes) at 6 and 12 months, compared to usual clinical care. We hypothesize that MyHEART will increase the frequency of home blood pressure monitoring and lifestyle modifications (increased physical activity, decreased sodium intake).
Specific Aim 3.
To examine whether MyHEART’s effects on self-management behavior are mediated through variables of perceived competence, autonomy, motivation, and activation (mediation outcomes). Based on our pilot study and theoretical framework, we hypothesize that MyHEART’s effects will be mediated through perceived competence, autonomy, motivation, and activation.
6.2. Primary outcome (Aim 1) Assessment
The co-primary clinical outcomes (Table 3) are a change in systolic and diastolic blood pressure at 6 and 12 months [9, 24]. The secondary clinical outcome is hypertension control at 6 and 12 months. Hypertension control will be defined using 24-hour ambulatory blood pressures as the gold standard (<130/80 mmHg), otherwise a clinic blood pressure of <140/90 mmHg. To reflect the 2017 ACC/AHA Hypertension Guidelines publication [4], we will include a secondary clinic blood pressure outcome of <130/80 mmHg. Follow-up clinic blood pressures will be measured per the screening visit protocol. The 6-month outcome assesses the end of the 6-month MyHEART intervention [31]. This follows guideline recommendations [4, 17], and adherence to lifestyle interventions usually peaks at 6 months [31]. The 12-month outcome (i.e., 6 months post-intervention) [131] assesses maintenance of blood pressure and sustainability of behavior change after study completion. In contrast to the baseline assessment, follow-up questionnaires and physiologic measurements will be conducted during Visit 1 to decrease missing data.
Table 3.
Baseline Assessment, 6-month, and 12-month Outcomes for All Participants (intervention & usual care)
| Time commitment = combined total across Visits 1 and 2 | Baseline Assessment (2½ hours) |
6-month* Outcomes (1½ hours) |
12-month* Outcomes (1½ hours) |
|||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 1 | Visit 2 | Visit 1 | Visit 2 | |
| Aim 1. Clinical Outcomes: Change in Systolic and Diastolic Blood Pressure (primary); Hypertension Control (secondary) | ||||||
| Study visit blood pressure | x | x | x | |||
| 24-hour Ambulatory Blood Pressure (gold standard) | x | x | x | |||
| Aim 2. Behavior Outcomes | ||||||
| 24-hour dietary recall [132] (in-person and phone administration) | x | x | x | |||
| 7-Day Physical Activity Recall** | x | x | x | |||
| Home Blood Pressure Monitoring Frequency** [133] | x | x | x | |||
| Weight (kilograms, kg) and Body mass index (kg/m2) [134] | x | x | x | |||
| Aim 3. Mediation Outcomes | ||||||
| Perceived Competence Scales** (PCS) | x | x | x | |||
| Health-Care Climate Questionnaire** (HCCQ) | x | x | x | |||
| Treatment Self-Regulation Questionnaires** (TSRQ) | x | x | x | |||
| Patient Activation Measure** (PAM) [135] | x | x | x | |||
Visits 1, 2 are consecutive days;
6- and 12-month visits are within 1 week after last phone call;
completed in-person at visit
6.3. Primary outcome (Aim 1) power estimates
A total of 310 eligible young adults will be enrolled into the study (155 participants per randomized arm) to result in an effective sample size of 264 under the assumption of 15% random drop-out at 6 months following randomization [136]. In Nidich et al. [137], the 3-month transcendental meditation program showed a mean difference of 6.3 and 4.0 in systolic and diastolic blood pressure change with a standard deviation of 13.6 and 9.7, respectively, as compared to usual care among young adults at hypertension risk. With an effective sample size of 264, there is power of 0.94 and 0.87 for systolic and diastolic blood pressure, respectively, for the same differences, each at a two-tailed 0.025 test for an overall significance level of 0.05.
6.4. Primary and Secondary Outcome (Aim 1) Statistical Analysis Plan
Data will be analyzed by intent to treat. Missing data will be imputed using multiple imputations along with sensitivity analyses for missingness according to the recommendations given in the National Research Council report [138, 139]. The primary comparisons for the co-primary outcomes of systolic and diastolic blood pressure change from baseline to 6 months will be done using analysis of covariance with MyHEART and baseline blood pressure as independent covariates. The primary comparisons for the secondary outcome of hypertension control at 6 months will be based on Fisher’s exact tests. If differences exist, they are likely to be largest at 6 months. Sequential hypothesis testing will be performed for hypertension control if blood pressure changes are shown to be statistically significantly different. Likewise, sequential hypothesis testing will be performed comparing the 6-month blood pressure change and hypertension control and only comparing 12-month success rates if the 6-month blood pressure change and hypertension control rates are shown to be statistically significantly different, using an alpha re-use approach [140]. The 12-month analysis will focus on maintenance of behavior change, to assess whether significant differences seen between baseline and 6 months are sustained. This will be achieved through a test for no difference between the baseline to 6-month change and the baseline to 12-month change [141]. Linear (for blood pressure) and generalized linear (for hypertension control) mixed-effects regression models will be fit to better understand the effects of MyHEART over time using longitudinal measurements. We will also assess the differential effectiveness of the intervention across subgroups (gender, race/ethnicity), which will guide future interventions, by developing exploratory regression models with interactions between MyHEART and baseline subject characteristics.
7. Explanatory Variable Assessment
Baseline explanatory variables, including demographic, clinical, and psychosocial variables, will be obtained for intervention and usual care participants (Table 4). The biological variables were selected based on our young adult studies [38, 43, 142, 143] and previously identified barriers and predictors of hypertension control and self-management [144–147]. For body mass index (kg/m2), weight will be measured to the nearest 0.1 kg in light clothing without shoes; height will be measured to the nearest 0.1 cm using a single, wall-mounted stadiometer [136, 148]. All scales will be calibrated quarterly by trained study personnel using standard weights. The selected questionnaires have been validated in young adults and across races/ethnicities [149, 150]. Alcohol consumption will be evaluated by alcohol beverage type and quantity as performed in the CARDIA (Coronary Artery Risk Development in Young Adults) study [151].
Table 4.
Baseline Biological & Explanatory Variables
| Data Source | |
|---|---|
| Age, Gender | EHR |
| Race/ethnicity, Marital Status, number of children in home | Self-report |
| Body mass index (kg/m2) [152, 153]; Waist circumference (cm) | Screening Visit 1 |
| Alcohol consumption [151] | Self-report |
| Highest level of education attained [154] | Self-report |
| Tobacco status [155] (current, former, never); cigarette packs/day [156]; e-cigarette use (yes/no) |
Self-report |
| Employment (full-time, part-time, other) | Self-report |
| Financial Status [20]; Annual household income [152] | Self-report |
| Self-rated health status [157–159] | Self-report |
| Health literacy [21, 160, 161] | Self-report |
| Comorbidities: dyslipidemia [162], anxiety [163–165], depression [166], diabetes mellitus [167], chronic kidney disease [168] | EHR [34] |
| Medical Outcomes Study Social Support Survey [169] | Self-report |
| John Hopkins Adjusted Clinical Group (ACG) Risk Score [170] | EHR |
| Primary care, specialty and urgent care visits over past 12 months prior to enrollment | EHR |
| Medication Adherence (Morisky) [171] | Self-report |
| Blood pressure medication classes (0,1,2,3, ≥4) and dose | EHR [34] |
| All other medication classes (i.e., oral contraceptives) | EHR |
EHR, electronic health record; AMA, American Medical Association
Participants will report their financial situation by selecting whether they: a) had enough money after paying bills for extra things (e.g., dining out), b) enough to pay bills but not to purchase extra things, c) enough money to pay bills by cutting back on things, or d) difficulty paying bills no matter what was done. The first two answer choices are categorized as “adequate income” and the last two choices as “inadequate income” [20]. This financial assessment accounts for varying income, which is more reflective of young adulthood. Single-item assessments of self-rated health status have a strong association with health outcomes and provide a broad assessment of health [157–159]. Self-rated health will be measured using the question: “In general, would you say your health is Excellent, Very Good, Good, Fair, or Poor?”, which has been used in nationally representative samples [157–159]. Health literacy (i.e., the ability to obtain, process, and understand basic information to make appropriate health decisions [172, 173]) will be evaluated using the Rapid Estimate of Adult Literacy in Medicine-Revised (REALM-R) instrument [160, 161]. Baseline comorbidities will be assessed using established administrative data algorithms per our previous research [38, 43, 142, 143]. The Medical Outcomes Study Social Support Survey [169] is a brief multi-dimensional evaluation validated for patients with chronic illnesses [159, 169, 174, 175]. Healthcare utilization will be evaluated using the Johns Hopkins Adjusted Clinical Group Case-Mix System (version 10.0), which assesses morbidity burden based on patient age, gender, and patterns of disease [38, 43, 142, 170]; we will also measure the number of clinic visits. To account for varying hypertension treatment at baseline, we will adjust for number of antihypertensive medication classes. In addition to using the EHR, participants will be asked to report all prescription and non-prescription medications. Global medication adherence will be assessed using the 4-item Morisky Scale [171, 176]. Provider characteristics will be obtained from the EHR, human resources, and the American Medical Association Masterfile data [38, 43].
8. Secondary outcome (Aim 2: Self-Management Behavior) Assessment
Dietary intake data for 24-hour recalls will be collected and analyzed using the Automated Self-Administered 24-hour (ASA24) Dietary Assessment Tool, version (2016), developed by the National Cancer Institute, Bethesda, MD [177]. We will use the 7-Day Physical Activity Recall [178–183] to assess baseline and change in physical activity. Accelerometers will not be used due to compliance limitations in young adult populations [148]. Frequency of home blood pressure monitoring (defined as taking your own blood pressure or having someone check your blood pressure outside of your usual primary care clinic) will be assessed by a single response: at least once a day, once or twice a week, once a month, or less than once a month [133]. The accuracy and reliability of the intervention arm’s self-responses will be evaluated by comparing automatically stored home blood pressure monitor readings with self-report entries to analyze deletion (under-reporting), addition (over-reporting), and reporting precision [184]. The accuracy and reliability of the intervention arm will be applied to the usual care arm. Physiologic secondary endpoints (weight [kg] and body mass index [kg/m2]) will also be assessed.
8.1. Secondary outcome (Aim 2: Self-Management Behavior) Statistical Analysis Plan
Behavioral outcomes will be analyzed in a similar manner as with the clinical outcomes depending on whether they are continuous or categorical. Unlike the clinical outcomes, there is no reason to control for multiplicity of testing, and so no adjustment will be made, and any p-values <0.05 will be noted. For Aim 2, there are three continuous variables: dietary recall (focused on grams of sodium/day and number of fruit & vegetable servings/day per the DASH-sodium diet [185, 186]), 7-day physical activity recall, and one count variable (home blood pressure monitoring frequency). Missing data will be handled in a similar manner as with clinical outcomes above. Thus, the effective sample size of 264 subjects will provide 90% power to detect a difference in the mean change from baseline to 6 months between treatment groups of about 0.4 times the standard deviation of the differences (moderate effect size). Analyses (t-tests or Wilcoxon tests and ANCOVA for continuous variables; Fisher’s exact test for the categorical variable) will be performed for comparison of change from baseline to 6 months between treatment groups. Linear or generalized linear mixed-effects regression models will be fit to describe longitudinal behavioral measurements over time.
9. Secondary outcome (Aim 3: Mediation Analysis) Assessment
To complement the primary findings, we will explore how treatment effects occur. Mediators are the constructs that the intervention (MyHEART) works through to affect behavior change [187]. Results from this Aim will examine the intervention components that provide the greatest support for sustainable behavior change.
The Perceived Competence Scale will evaluate participants’ beliefs of their abilities to change behavior [118, 188]. Participants’ perceptions of their healthcare team’s autonomy support will be measured using the modified Health Care Climate Questionnaire [118]. The Treatment Self-Regulation Questionnaire will assess autonomous motivation (self-determined), external motivation, and amotivation. Based on SDT, we expect an increase in autonomous motivation and a decrease in external motivation [189]. The Patient Activation Measure [190–194] will assess participants’ knowledge, skill, and confidence in managing their health [195]. All surveys are validated in young adults [118, 188, 189].
9.1. Secondary outcome (Aim 3: Mediation Analysis) Statistical Analysis Plan
Analyses will examine four hypothesized mediators of the MyHEART intervention: (i) autonomy support, (ii) motivation, (iii) perceived competence [196], and (iv) activation. We will estimate mediation effects in multilevel models [197–201] where mediation is assessed by fitting two models. Similar to Aim 2, Model 1 estimates MyHEART’s intervention effect on the outcome (behavior change) but also includes the mediating variable as a time-dependent covariate. Model 2 estimates MyHEART’s effect on the mediator itself over time using linear mixed-effects modeling, with the same condition by time interactions. We will estimate a separate model for each mediation variable. Dividing the mediation effect by the overall intervention effect estimated in Aim 1 yields the percent mediated (the proportion of the intervention effect that is mediated by the mediator). Standard errors and 95% confidence intervals for the mediation effect and percent mediated estimates will be calculated using bootstrapping [202]. This analysis will be pivotal to guide future replication and dissemination of MyHEART.
10. Potential Study Limitations
As with any randomized controlled trial, potential problems may arise. These potential pitfalls will help guide study dissemination [203]. Our design limits our ability to analyze MyHEART’s effect compared to the effect of participants solely receiving greater attention from health coaches (i.e., greater number of care encounters). We believe this is reasonable, as usual care has proven ineffective for controlling hypertension in young adults. Lack of primary care provider blinding [204] could increase referrals in the usual care arm to hypertension self-management resources not targeted to young adults which may underestimate MyHEART’s effect. We will adjust for this by collecting data on all ambulatory visits for the usual care and intervention arms. Recruitment of young adults is an established challenge when conducting research studies [205]. In addition to our above methods, additional recruitment steps will include partnering with primary care providers to review weekly panels, posting announcements within primary care clinics, targeting more ethnically diverse clinics, communication venues (e.g., community boards, churches), and social media (e.g., Facebook, Instagram) [206, 207]. We will assess for attrition bias by analyzing for significant differences between usual care and intervention participants [208]. Low return of home blood pressures is a concern; however, we have provided multiple modalities to return blood pressure data. In addition, we have included incentives every three months to encourage program participation. Loss to follow-up is a concern in longitudinal studies. Young adults are a mobile population; some loss to follow-up is expected and accounted for in our sample size. We will minimize this risk with scheduled assessments, re-try calls, and participant-directed communication [209]. At enrollment, we will ask participants to provide contact information for two people who are close friends or family and would be aware of their location. We will contact all participants by telephone every 2 months to verify contact information [209]. Length of follow-up: Our study (intervention + maintenance) concludes after 12 months based on prior studies [77]; in addition, our preliminary data demonstrated changes in healthcare systems among young adults after a mean 15 months [77]. Self-report and recall bias [210] are limitations with surveys and questionnaires [211]. However, more robust assessment will likely result in greater missing data. We tried to avoid response burden; similar assessments have been conducted with this age range [212] and with comparable estimated completion times. EHR utilization is a limitation. All of the clinics in the included healthcare systems for this proposal use an EHR system. Finally, we require a diagnosis of hypertension to capture a population with known hypertension and ongoing uncontrolled blood pressures. Future studies will include young adults without a hypertension diagnosis to increase awareness.
11. Conclusion
The growing prevalence of uncontrolled hypertension among young adults is a significant public health burden in the United States. Although hypertension self-management (home blood pressure monitoring and lifestyle modifications) is recommended to lower and control blood pressure, current hypertension self-management programs do not meet the needs and barriers specific to young adults. MyHEART is the first multicomponent, theoretically-based randomized controlled trial tailored to diverse young adults with an established primary care team. This trial will provide data on the impact of MyHEART vs. usual care, and inform future dissemination and implementation initiatives in other healthcare systems.
Acknowledgments
Funding/Support
This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH), grant R01HL132148. The project described was also supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. None of the sponsors had a role in study design, in the collection, analysis or interpretation of data, in the writing of the report, or in the decision to submit the article for publication. Additional funding for the project was provided by the UW Health Innovation Program and the UW School of Medicine and Public Health from the Wisconsin Partnership Program.
Financial Disclosures
Patrick McBride is a minimal investment stockholder with Health Decisions. Heather Johnson is a co-investigator on Pfizer Grant Renewal ID # 30876619: Independent Grants for Leaning and Change (PI: Christie Bartels, MD, MS).
Abbreviations:
- SDT
self-determination theory
- EHR
electronic health record
- WCHQ
Wisconsin Collaborative for Healthcare Quality
- HEDIS
Healthcare Effectiveness Data and Information Set
- AMBP
ambulatory blood pressure
- PA
physician assistant
- NP
nurse practitioner
- REDCap
Research Electronic Data Capture
- BECCI
Behavior Change Counseling Index
- CARDIA
Coronary Artery Risk Development in Young Adults
- ACG
Adjusted Clinical Group
- AMA
American Medical Association
- REALM-R
Rapid Estimate of Adult Literacy in Medicine-Revised
- ASA24
Automated Self-Administered 24-hour Dietary Assessment Tool
- DASH
Dietary Approaches to Stop Hypertension
Footnotes
Trial registration
ClinicalTrials.gov Identifier: NCT03158051
Trial Status
Enrollment into this randomized controlled trial began in October 2017 and will conclude in June 2020.
None of the other authors declare any relevant conflicts of interest.
References
- [1].Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, Sanchez E, An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention, J Am Coll Cardiol 63(12) (2014) 1230–8. [DOI] [PubMed] [Google Scholar]
- [2].U.S. Department of Health and Human Services, Healthy People 2020: Heart Disease and Stroke - Increase the proportion of adults with hypertension whose blood pressure is under control, 2017. http://www.healthypeople.gov/node/4555/data_details. (Accessed June 27 2018).
- [3].Gooding HC, McGinty S, Richmond TK, Gillman MW, Field AE, Hypertension awareness and control among young adults in the national longitudinal study of adolescent health, J Gen Intern Med 29(8) (2014) 1098–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, Wright JT Jr., 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, J Am Coll Cardiol 71(19) (2018) e127–e248. [DOI] [PubMed] [Google Scholar]
- [5].Centers for Disease Control and Prevention, High Blood Pressure Facts, 2018. https://www.cdc.gov/bloodpressure/facts.htm. (Accessed June 27 2018).
- [6].Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, E. American Heart Association Council on, C. Prevention Statistics, S. Stroke Statistics, Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association, Circulation 137(12) (2018) e67–e492. [DOI] [PubMed] [Google Scholar]
- [7].Grubbs V, Lin F, Vittinghoff E, Shlipak MG, Peralta CA, Bansal N, Jacobs DR, Siscovick DS, Lewis CE, Bibbins-Domingo K, Body mass index and early kidney function decline in young adults: a longitudinal analysis of the CARDIA (Coronary Artery Risk Development in Young Adults) study, Am J Kidney Dis 63(4) (2014) 590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mitchell AB, Cole JW, McArdle PF, Cheng YC, Ryan KA, Sparks MJ, Mitchell BD, Kittner SJ, Obesity increases risk of ischemic stroke in young adults, Stroke 46(6) (2015) 1690–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., Roccella EJ, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report, JAMA 289(19) (2003) 2560–72. [DOI] [PubMed] [Google Scholar]
- [10].Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S, Explaining the decrease in U.S. deaths from coronary disease, 1980–2000, N Engl J Med 356(23) (2007) 2388–98. [DOI] [PubMed] [Google Scholar]
- [11].Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD, Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond, Circulation 121(4) (2010) 586–613. [DOI] [PubMed] [Google Scholar]
- [12].Paramore LC, Halpern MT, Lapuerta P, Hurley JS, Frost FJ, Fairchild DG, Bates D, Impact of poorly controlled hypertension on healthcare resource utilization and cost, Am J Manag Care 7(4) (2001) 389–98. [PubMed] [Google Scholar]
- [13].Yano Y, Stamler J, Garside DB, Daviglus ML, Franklin SS, Carnethon MR, Liu K, Greenland P, Lloyd-Jones DM, Isolated Systolic Hypertension in Young and Middle-Aged Adults and 31-Year Risk for Cardiovascular Mortality: The Chicago Heart Association Detection Project in Industry Study, J Am Coll Cardiol 65(4) (2015) 327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Holland N, Segraves D, Nnadi VO, Belletti DA, Wogen J, Arcona S, Identifying barriers to hypertension care: implications for quality improvement initiatives, Dis Manag 11(2) (2008) 71–7. [DOI] [PubMed] [Google Scholar]
- [15].James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr., Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr., Narva AS, Ortiz E, 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8), JAMA 311(5) (2014) 507–20. [DOI] [PubMed] [Google Scholar]
- [16].Ma J, Urizar GG Jr., Alehegn T, Stafford RS, Diet and physical activity counseling during ambulatory care visits in the United States, Prev Med 39(4) (2004) 815–22. [DOI] [PubMed] [Google Scholar]
- [17].Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, Flack JM, Carter BL, Materson BJ, Ram CV, Cohen DL, Cadet JC, Jean-Charles RR, Taler S, Kountz D, Townsend RR, Chalmers J, Ramirez AJ, Bakris GL, Wang J, Schutte AE, Bisognano JD, Touyz RM, Sica D, Harrap SB, Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension, J Clin Hypertens (Greenwich) 16(1) (2014) 14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Artinian NT, Flack JM, Nordstrom CK, Hockman EM, Washington OG, Jen KL, Fathy M, Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans, Nurs Res 56(5) (2007) 312–22. [DOI] [PubMed] [Google Scholar]
- [19].Bosworth HB, Olsen MK, Grubber JM, Neary AM, Orr MM, Powers BJ, Adams MB, Svetkey LP, Reed SD, Li Y, Dolor RJ, Oddone EZ, Two self-management interventions to improve hypertension control: a randomized trial, Ann Intern Med 151(10) (2009) 687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bosworth HB, Olsen MK, Grubber JM, Powers BJ, Oddone EZ, Racial differences in two self-management hypertension interventions, Am J Med 124(5) (2011) 468 e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Bosworth HB, Olsen MK, Neary A, Orr M, Grubber J, Svetkey L, Adams M, Oddone EZ, Take Control of Your Blood Pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control, Patient Educ Couns 70(3) (2008) 338–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, Gentry PW, Rose C, Van Houtven C, Wang V, Goldstein MK, Oddone EZ, Home blood pressure management and improved blood pressure control: results from a randomized controlled trial, Arch Intern Med 171(13) (2011) 1173–80. [DOI] [PubMed] [Google Scholar]
- [23].Friedberg JP, Rodriguez MA, Watsula ME, Lin I, Wylie-Rosett J, Allegrante JP, Lipsitz SR, Natarajan S, Effectiveness of a tailored behavioral intervention to improve hypertension control: primary outcomes of a randomized controlled trial, Hypertension 65(2) (2015) 440–6. [DOI] [PubMed] [Google Scholar]
- [24].Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS, Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial, JAMA 299(24) (2008) 2857–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jackson GL, Oddone EZ, Olsen MK, Powers BJ, Grubber JM, McCant F, Bosworth HB, Racial differences in the effect of a telephone-delivered hypertension disease management program, J Gen Intern Med 27(12) (2012) 1682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kim KB, Han HR, Huh B, Nguyen T, Lee H, Kim MT, The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure, Am J Hypertens 27(9) (2014) 1199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Margolius D, Bodenheimer T, Bennett H, Wong J, Ngo V, Padilla G, Thom DH, Health coaching to improve hypertension treatment in a low-income, minority population, Ann Fam Med 10(3) (2012) 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mehos BM, Saseen JJ, MacLaughlin EJ, Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension, Pharmacotherapy 20(11) (2000) 1384–9. [DOI] [PubMed] [Google Scholar]
- [29].Ralston JD, Cook AJ, Anderson ML, Catz SL, Fishman PA, Carlson J, Johnson R, Green BB, Home blood pressure monitoring, secure electronic messaging and medication intensification for improving hypertension control: a mediation analysis, Appl Clin Inform 5(1) (2014) 232–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, Debusk RF, Nurse management for hypertension. A systems approach, Am J Hypertens 17(10) (2004) 921–7. [DOI] [PubMed] [Google Scholar]
- [31].Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR, Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial, JAMA 289(16) (2003) 2083–93. [DOI] [PubMed] [Google Scholar]
- [32].Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR, An evidence-based review of patient-centered behavioral interventions for hypertension, Am J Prev Med 21(3) (2001) 221–32. [DOI] [PubMed] [Google Scholar]
- [33].Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T, Interventions used to improve control of blood pressure in patients with hypertension, Cochrane Database Syst Rev (3) (2010) CD005182. [DOI] [PubMed]
- [34].Ogedegbe G, Tobin JN, Fernandez S, Gerin W, Diaz-Gloster M, Cassells A, Khalida C, Pickering T, Schoenthaler A, Ravenell J, Counseling African Americans to Control Hypertension (CAATCH) trial: a multi-level intervention to improve blood pressure control in hypertensive blacks, Circ Cardiovasc Qual Outcomes 2(3) (2009) 249–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Senesael E, Borgermans L, Van De Vijver E, Devroey D, Effectiveness of a quality improvement intervention targeting cardiovascular risk factors: are patients responsive to information and encouragement by mail or post?, Vasc Health Risk Manag 9 (2013) 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Watson AJ, Singh K, Myint UK, Grant RW, Jethwani K, Murachver E, Harris K, Lee TH, Kvedar JC, Evaluating a web-based self-management program for employees with hypertension and prehypertension: a randomized clinical trial, Am Heart J 164(4) (2012) 625–31. [DOI] [PubMed] [Google Scholar]
- [37].Magid DJ, Ho PM, Olson KL, Brand DW, Welch LK, Snow KE, Lambert-Kerzner AC, Plomondon ME, Havranek EP, A multimodal blood pressure control intervention in 3 healthcare systems, Am J Manag Care 17(4) (2011) e96–103. [PubMed] [Google Scholar]
- [38].Johnson HM, Thorpe CT, Bartels CM, Schumacher JR, Palta M, Pandhi N, Sheehy AM, Smith MA, Antihypertensive medication initiation among young adults with regular primary care use, J Gen Intern Med 29(5) (2014) 723–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, Jacobs DR Jr., Liu K, Lloyd-Jones D, Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age, JAMA 311(5) (2014) 490–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Michie S, Abraham C, Whittington C, McAteer J, Gupta S, Effective techniques in healthy eating and physical activity interventions: a meta-regression, Health Psychol 28(6) (2009) 690–701. [DOI] [PubMed] [Google Scholar]
- [41].Sher T, Braun L, Domas A, Bellg A, Baucom DH, Houle TT, The partners for life program: a couples approach to cardiac risk reduction, Fam Process 53(1) (2014) 131–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Voils CI, Gierisch JM, Yancy WS Jr., Sandelowski M, Smith R, Bolton J, Strauss JL, Differentiating behavior initiation and maintenance: theoretical framework and proof of concept, Health Educ Behav 41(3) (2014) 325–36. [DOI] [PubMed] [Google Scholar]
- [43].Johnson HM, Thorpe CT, Bartels CM, Schumacher JR, Palta M, Pandhi N, Sheehy AM, Smith MA, Undiagnosed hypertension among young adults with regular primary care use, J Hypertens 32(1) (2014) 65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Johnson HM, Warner RC, LaMantia JN, Bowers BJ, “I have to live like I’m old.” Young adults’ perspectives on managing hypertension: a multi-center qualitative study, BMC Fam Pract 17(1) (2016) 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].O’Brien K, Venn BJ, Perry T, Green TJ, Aitken W, Bradshaw A, Thomson R, Reasons for wanting to lose weight: different strokes for different folks, Eat Behav 8(1) (2007) 132–5. [DOI] [PubMed] [Google Scholar]
- [46].Underbakke G, McBride PE, Office systems for heart disease prevention, Prim Care 32(4) (2005) 883–900. [DOI] [PubMed] [Google Scholar]
- [47].Wolpert HA, Anderson BJ, Young adults with diabetes: need for a new treatment paradigm, Diabetes Care 24(9) (2001) 1513–4. [DOI] [PubMed] [Google Scholar]
- [48].Johnson HM, LaMantia JN, Warner RC, Pandhi N, Bartels CM, Smith MA, Lauver DR, MyHEART: A Non Randomized Feasibility Study of a Young Adult Hypertension Intervention, J Hypertens Manag 2(2) (2016) 016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Johnson HM, Warner RC, Bartels CM, LaMantia JN, “They’re younger... it’s harder.” Primary providers’ perspectives on hypertension management in young adults: a multicenter qualitative study, BMC Res Notes 10(1) (2017) 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Deci EL, Ryan RM, Self-determination theory: a macrotherapy of human motivation, development, and health, Can Psychol 49(3) (2008) 182–5. [Google Scholar]
- [51].Kupst MJ, Butt Z, Stoney CM, Griffith JW, Salsman JM, Folkman S, Cella D, Assessment of stress and self-efficacy for the NIH Toolbox for Neurological and Behavioral Function, Anxiety Stress Coping (2015) 1–14. [DOI] [PMC free article] [PubMed]
- [52].Molton IR, Jensen MP, Nielson W, Cardenas D, Ehde DM, A preliminary evaluation of the motivational model of pain self-management in persons with spinal cord injury-related pain, J Pain 9(7) (2008) 606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Bodenheimer T, Lorig K, Holman H, Grumbach K, Patient self-management of chronic disease in primary care, JAMA 288(19) (2002) 2469–75. [DOI] [PubMed] [Google Scholar]
- [54].Carroll JK, Fiscella K, Epstein RM, Sanders MR, Williams GC, A 5A’s communication intervention to promote physical activity in underserved populations, BMC Health Serv Res 12 (2012) 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Markland D, Ryan RM, Tobin VJ, Rollnick S, Motivational interviewing and self-determination theory, J Soc Clin Psychol 24(6) (2005) 811–31. [Google Scholar]
- [56].Li K, Iannotti RJ, Haynie DL, Perlus JG, Simons-Morton BG, Motivation and planning as mediators of the relation between social support and physical activity among U.S. adolescents: a nationally representative study, Int J Behav Nutr Phys Act 11(1) (2014) 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M, Effect of a self-management program on patients with chronic disease, Eff Clin Pract 4(6) (2001) 256–62. [PubMed] [Google Scholar]
- [58].Ryan RM, Frederick CM, Lepes D, Rubio N, Sheldon KM, Intrinsic motivation and exercise adherence, Int J Sport Psychol 28 (1997) 335–54. [Google Scholar]
- [59].Silva MN, Markland D, Minderico CS, Vieira PN, Castro MM, Coutinho SR, Santos TC, Matos MG, Sardinha LB, Teixeira PJ, A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description, BMC Public Health 8 (2008) 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Wisconsin Collaborative for Healthcare Quality, WCHQ website http://www.wchq.org/. (Accessed May 23 2018).
- [61].Hatahet MA, Bowhan J, Clough EA, Wisconsin Collaborative for Healthcare Quality (WCHQ): lessons learned, WMJ 103(3) (2004) 45–8. [PubMed] [Google Scholar]
- [62].Sheehy A, Pandhi N, Coursin DB, Flood GE, Kraft SA, Johnson HM, Smith MA, Minority status and diabetes screening in an ambulatory population, Diabetes Care 34(6) (2011) 1289–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Sheehy AM, Flood GE, Tuan WJ, Liou JI, Coursin DB, Smith MA, Analysis of guidelines for screening diabetes mellitus in an ambulatory population, Mayo Clin Proc 85(1) (2010) 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Nesbitt SD, Amerena JV, Grant E, Jamerson KA, Lu H, Weder A, Julius S, Home blood pressure as a predictor of future blood pressure stability in borderline hypertension. The Tecumseh Study, Am J Hypertens 10(11) (1997) 1270–80. [DOI] [PubMed] [Google Scholar]
- [65].Fielding RA, Rejeski WJ, Blair S, Church T, Espeland MA, Gill TM, Guralnik JM, Hsu FC, Katula J, King AC, Kritchevsky SB, McDermott MM, Miller ME, Nayfield S, Newman AB, Williamson JD, Bonds D, Romashkan S, Hadley E, Pahor M, LIFE Research Group, The Lifestyle Interventions and Independence for Elders Study: design and methods, J Gerontol A Biol Sci Med Sci 66(11) (2011) 1226–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ, Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research, Circulation 111(5) (2005) 697–716. [DOI] [PubMed] [Google Scholar]
- [67].Unger E, Diez-Roux AV, Lloyd-Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB, Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis, Circ Cardiovasc Qual Outcomes 7(4) (2014) 524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Agarwal R, Bunaye Z, Bekele DM, Prognostic significance of between-arm blood pressure differences, Hypertension 51(3) (2008) 657–62. [DOI] [PubMed] [Google Scholar]
- [69].Spacelabs Healthcare, OnTrak, the NEW Evolution of ABPM from Spacelabs Healthcare, 2013. https://www.spacelabshealthcare.com/diagnostic-cardiology/abp-monitoring/ontrak#.W894h2hKjct. (Accessed September 27 2018).
- [70].Pickering TG, 24 Hour Ambulatory Blood Pressure Monitoring: Is it Necessary to Establish a Diagnosis Before Instituting Treatment of Hypertension?, J Clin Hypertens (Greenwich) 1(1) (1999) 33–40. [PubMed] [Google Scholar]
- [71].U.S. Preventive Services Task Force, Final Recommendation Statement: High Blood Pressure in Adults: Screening, 2015. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/high-blood-pressure-in-adults-screening. (Accessed March 23 2017).
- [72].Pickering TG, Shimbo D, Haas D, Ambulatory blood-pressure monitoring, N Engl J Med 354(22) (2006) 2368–74. [DOI] [PubMed] [Google Scholar]
- [73].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform 42(2) (2009) 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Vanderbilt University Medical Center, Project REDCap, 2018. https://projectredcap.org/. (Accessed June 27 2018).
- [75].Friedberg JP, Lipsitz SR, Natarajan S, Challenges and recommendations for blinding in behavioral interventions illustrated using a case study of a behavioral intervention to lower blood pressure, Patient Educ Couns 78(1) (2010) 5–11. [DOI] [PubMed] [Google Scholar]
- [76].Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, Lin PH, Champagne C, Harsha DW, Svetkey LP, Ard J, Brantley PJ, Proschan MA, Erlinger TP, Appel LJ, Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial, Ann Intern Med 144(7) (2006) 485–95. [DOI] [PubMed] [Google Scholar]
- [77].Margolis KL, Kerby TJ, Asche SE, Bergdall AR, Maciosek MV, O’Connor PJ, Sperl-Hillen JM, Design and rationale for Home Blood Pressure Telemonitoring and Case Management to Control Hypertension (HyperLink): a cluster randomized trial, Contemp Clin Trials 33(4) (2012) 794–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Department of Health and Human Services, Interventions to Improve Hypertension Control Rates in African Americans, 2003. http://grants.nih.gov/grants/guide/rfa-files/RFA-HL-04-007.html. (Accessed March 23 2017).
- [79].Maciejewski ML, Bosworth HB, Olsen MK, Smith VA, Edelman D, Powers BJ, Kaufman MA, Oddone EZ, Jackson GL, Do the benefits of participation in a hypertension self-management trial persist after patients resume usual care?, Circ Cardiovasc Qual Outcomes 7(2) (2014) 269–75. [DOI] [PubMed] [Google Scholar]
- [80].Walsh JM, Sundaram V, McDonald K, Owens DK, Goldstein MK, Implementing effective hypertension quality improvement strategies: barriers and potential solutions, J Clin Hypertens (Greenwich) 10(4) (2008) 311–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Institute of Medicine (US) Committee on Public Health Priorities to Reduce and Control Hypertension, A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension, National Academies Press (US), Washington, D.C., 2010. [PubMed] [Google Scholar]
- [82].The Diabetes Prevention Program (DPP): description of lifestyle intervention, Diabetes Care 25(12) (2002) 2165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Bokhour BG, Cohn ES, Cortes DE, Solomon JL, Fix GM, Elwy AR, Mueller N, Katz LA, Haidet P, Green AR, Borzecki AM, Kressin NR, The role of patients’ explanatory models and daily-lived experience in hypertension self-management, J Gen Intern Med 27(12) (2012) 1626–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Willard-Grace R, DeVore D, Chen EH, Hessler D, Bodenheimer T, Thom DH, The effectiveness of medical assistant health coaching for low-income patients with uncontrolled diabetes, hypertension, and hyperlipidemia: protocol for a randomized controlled trial and baseline characteristics of the study population, BMC Fam Pract 14 (2013) 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, Oddone EZ, Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention, Patient Educ Couns 57(1) (2005) 5–14. [DOI] [PubMed] [Google Scholar]
- [86].Lovejoy TI, Heckman TG, Suhr JA, Anderson T, Heckman BD, France CR, Telephone-administered motivational interviewing reduces risky sexual behavior in HIV-positive late middle-age and older adults: a pilot randomized controlled trial, AIDS Behav 15(8) (2011) 1623–34. [DOI] [PubMed] [Google Scholar]
- [87].Madlensky L, Natarajan L, Flatt SW, Faerber S, Newman VA, Pierce JP, Timing of dietary change in response to a telephone counseling intervention: evidence from the WHEL study, Health Psychol 27(5) (2008) 539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Miller SM, Hui SK, Wen KY, Scarpato J, Zhu F, Buzaglo J, Hernandez EE, Tailored telephone counseling to improve adherence to follow-up regimens after an abnormal pap smear among minority, underserved women, Patient Educ Couns 93(3) (2013) 488–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Miller WR, Rose GS, Toward a theory of motivational interviewing, Am Psychol 64(6) (2009) 527–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Lehr AL, Driver SL, Stone NJ, The ABCDs of lifestyle counseling, JAMA Cardiol 1(5) (2016) 505–6. [DOI] [PubMed] [Google Scholar]
- [91].Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH, Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams, Ann Behav Med 24(2) (2002) 80–7. [DOI] [PubMed] [Google Scholar]
- [92].Whitlock EP, Orleans CT, Pender N, Allan J, Evaluating primary care behavioral counseling interventions: an evidence-based approach, Am J Prev Med 22(4) (2002) 267–84. [DOI] [PubMed] [Google Scholar]
- [93].Gutnick D, Reims K, Davis C, Gainforth H, Jay M, Cole S, Brief action planning to facilitate behavior change and support patient self-management, J Clin Outcomes Manag 21(1) (2014) 17–29. [Google Scholar]
- [94].Ritholz MD, Beverly EA, Brooks KM, Abrahamson MJ, Weinger K, Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes, Chronic Illn 10(4) (2014) 303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Schwarzer R, Self-regulatory Processes in the Adoption and Maintenance of Health Behaviors, J Health Psychol 4(2) (1999) 115–27. [DOI] [PubMed] [Google Scholar]
- [96].Poobalan AS, Pitchforth E, Imamura M, Tucker JS, Philip K, Spratt J, Mandava L, van Teijlingen E, Characteristics of effective interventions in improving young people’s sexual health: a review of reviews, Sex Educ 9(3) (2009) 319–36. [Google Scholar]
- [97].Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O, Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes, N Engl J Med 348(5) (2003) 383–93. [DOI] [PubMed] [Google Scholar]
- [98].Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, Dornelas E, Duer-Hefele J, Frasure-Smith N, Freedland KE, Haas DC, Jaffe AS, Ladapo JA, Lesperance F, Medina V, Newman JD, Osorio GA, Parsons F, Schwartz JE, Shaffer JA, Shapiro PA, Sheps DS, Vaccarino V, Whang W, Ye S, Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial, JAMA Intern Med 173(11) (2013) 997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, Brancati FL, Krishnan JA, Tailored education may reduce health literacy disparities in asthma self-management, Am J Respir Crit Care Med 172(8) (2005) 980–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Kincaid JP, Fishburne RP, Rogers RL, Chissom BS, Derivation of New Readability Formulas (Automated Readability Index, Fog Count and Flesch Reading Ease Formula) for Navy Enlisted Personnel, in: C.o.N.T. Training (Ed.) Naval Air Station Memphis, Naval Air Station Memphis, Millington, TN, 1975. [Google Scholar]
- [101].Castro M, Zimmermann NA, Crocker S, Bradley J, Leven C, Schechtman KB, Asthma intervention program prevents readmissions in high healthcare users, Am J Respir Crit Care Med 168(9) (2003) 1095–9. [DOI] [PubMed] [Google Scholar]
- [102].Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB, Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association, Circulation 133(4) (2016) e38–e360. [DOI] [PubMed] [Google Scholar]
- [103].Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH Jr., Hall WD, Jones WE, Kountz DS, Lea JP, Nasser S, Nesbitt SD, Saunders E, Scisney-Matlock M, Jamerson KA, Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement, Hypertension 56(5) (2010) 780–800. [DOI] [PubMed] [Google Scholar]
- [104].Harder VS, Ayer LA, Rose GL, Naylor MR, Helzer JE, Alcohol, moods and male-female differences: daily interactive voice response over 6 months, Alcohol Alcohol 49(1) (2014) 60–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Wheeler L, Buckley R, Gerald LB, Merkle S, A.M.T., Working with schools to improve pediatric asthma management, Pediatr Asthma Allergy Immunol 22(4) (2010) 197–208. [Google Scholar]
- [106].Isasi CR, Parrinello CM, Jung MM, Carnethon MR, Birnbaum-Weitzman O, Espinoza RA, Penedo FJ, Perreira KM, Schneiderman N, Sotres-Alvarez D, Van Horn L, Gallo LC, Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults, Ann Epidemiol 25(2) (2015) 84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].American Heart Association, Alcohol and Heart Health: AHA Recommendation, 2015. http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/Alcohol-and-Heart-Health_UCM_305173_Article.jsp. (Accessed June 29 2016).
- [108].Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH, Enhancing doctor-patient communication using email: a pilot study, J Am Board Fam Pract 18(3) (2005) 180–8. [DOI] [PubMed] [Google Scholar]
- [109].Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, Owens DK, Goldstein MK, Quality improvement strategies for hypertension management: a systematic review, Med Care 44(7) (2006) 646–57. [DOI] [PubMed] [Google Scholar]
- [110].Curley MA, Patient-nurse synergy: optimizing patients’ outcomes, Am J Crit Care 7(1) (1998) 64–72. [PubMed] [Google Scholar]
- [111].Coleman A, Freeman P, Steel S, Shennan A, Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol, Blood Press Monit 11(1) (2006) 27–32. [DOI] [PubMed] [Google Scholar]
- [112].O’Brien E, Waeber B, Parati G, Staessen J, Myers MG, Blood pressure measuring devices: recommendations of the European Society of Hypertension, BMJ 322(7285) (2001) 531–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Takahashi H, Yoshika M, Yokoi T, Validation of two automatic devices for the self-measurement of blood pressure according to the ANSI/AAMI/ISO81060–2:2009 guidelines: the Omron BP765 (HEM-7311-ZSA) and the Omron BP760N (HEM-7320-Z), Vasc Health Risk Manag 11 (2015) 49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Anthony CA, Polgreen LA, Chounramany J, Foster ED, Goerdt CJ, Miller ML, Suneja M, Segre AM, Carter BL, Polgreen PM, Outpatient blood pressure monitoring using bi-directional text messaging, J Am Soc Hypertens 9(5) (2015) 375–381. [DOI] [PubMed] [Google Scholar]
- [115].Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins-Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW, Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial, Arch Intern Med 171(4) (2011) 342–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Blonstein AC, Yank V, Stafford RS, Wilson SR, Rosas LG, Ma J, Translating an evidence-based lifestyle intervention program into primary care: lessons learned, Health Promot Pract 14(4) (2013) 491–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, Ogedegbe G, Orwig D, Ernst D, Czajkowski S, Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium, Health Psychol 23(5) (2004) 443–51. [DOI] [PubMed] [Google Scholar]
- [118].Carroll JK, Fiscella K, Epstein RM, Sanders MR, Winters PC, Moorhead SA, van Osch L, Williams GC, Physical activity counseling intervention at a federally qualified health center: improves autonomy-supportiveness, but not patients’ perceived competence, Patient Educ Couns 92(3) (2013) 432–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Spillane V, Byrne MC, Byrne M, Leathem CS, O’Malley M, Cupples ME, Monitoring treatment fidelity in a randomized controlled trial of a complex intervention, J Adv Nurs 60(3) (2007) 343–52. [DOI] [PubMed] [Google Scholar]
- [120].Willard-Grace R, Chen EH, Hessler D, DeVore D, Prado C, Bodenheimer T, Thom DH, Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial, Ann Fam Med 13(2) (2015) 130–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Antal H, Hossain MJ, Hassink S, Henry S, Fuzzell L, Taylor A, Wysocki T, Audio-video recording of health care encounters for pediatric chronic conditions: observational reactivity and its correlates, J Pediatr Psychol 40(1) (2015) 144–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Johnson-Kozlow M, Hovell MF, Rovniak LS, Sirikulvadhana L, Wahlgren DR, Zakarian JM, Fidelity issues in secondhand smoking interventions for children, Nicotine Tob Res 10(12) (2008) 1677–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Lambert JD, Greaves CJ, Farrand P, Cross R, Haase AM, Taylor AH, Assessment of fidelity in individual level behaviour change interventions promoting physical activity among adults: a systematic review, BMC Public Health 17(1) (2017) 765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Lane C, Huws-Thomas M, Hood K, Rollnick S, Edwards K, Robling M, Measuring adaptations of motivational interviewing: the development and validation of the behavior change counseling index (BECCI), Patient Educ Couns 56(2) (2005) 166–73. [DOI] [PubMed] [Google Scholar]
- [125].Madson MB, Loignon AC, Lane C, Training in motivational interviewing: a systematic review, J Subst Abuse Treat 36(1) (2009) 101–9. [DOI] [PubMed] [Google Scholar]
- [126].Rasmussen HN, Wrosch C, Scheier MF, Carver CS, Self-regulation processes and health: the importance of optimism and goal adjustment, J Pers 74(6) (2006) 1721–47. [DOI] [PubMed] [Google Scholar]
- [127].Baker AL, Turner A, Kelly PJ, Spring B, Callister R, Collins CE, Woodcock KL, Kay-Lambkin FJ, Devir H, Lewin TJ, ‘Better Health Choices’ by telephone: a feasibility trial of improving diet and physical activity in people diagnosed with psychotic disorders, Psychiatry Res 220(1–2) (2014) 63–70. [DOI] [PubMed] [Google Scholar]
- [128].Dane AV, Schneider BH, Program integrity in primary and early secondary prevention: are implementation effects out of control?, Clin Psychol Rev 18(1) (1998) 23–45. [DOI] [PubMed] [Google Scholar]
- [129].Santacroce SJ, Maccarelli LM, Grey M, Intervention fidelity, Nurs Res 53(1) (2004) 63–6. [DOI] [PubMed] [Google Scholar]
- [130].Lauver DR, Gross J, Ruff C, Wells TJ, Patient-centered interventions: implications for incontinence, Nurs Res 53(6 Suppl) (2004) S30–5. [DOI] [PubMed] [Google Scholar]
- [131].Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O’Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK, Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial, JAMA 310(1) (2013) 46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Svetkey LP, Harsha DW, Vollmer WM, Stevens VJ, Obarzanek E, Elmer PJ, Lin PH, Champagne C, Simons-Morton DG, Aickin M, Proschan MA, Appel LJ, Premier: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics, Ann Epidemiol 13(6) (2003) 462–71. [DOI] [PubMed] [Google Scholar]
- [133].Baral-Grant S, Haque MS, Nouwen A, Greenfield SM, McManus RJ, Self-Monitoring of Blood Pressure in Hypertension: A UK Primary Care Survey, Int J Hypertens 2012 (2012) 582068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, Hill JO, Brancati FL, Peters A, Wagenknecht L, Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes, Diabetes Care 34(7) (2011) 1481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Insignia Health, Insignia Health Patient Activation Measure®, 2015. http://insignia-health.herokuapp.com/products/pam-survey. (Accessed March 23 2017).
- [136].Wing RR, Tate DF, Espeland MA, Lewis CE, LaRose JG, Gorin AA, Bahnson J, Perdue LH, Hatley KE, Ferguson E, Garcia KR, Lang W, Innovative Self-Regulation Strategies to Reduce Weight Gain in Young Adults: The Study of Novel Approaches to Weight Gain Prevention (SNAP) Randomized Clinical Trial, JAMA Intern Med 176(6) (2016) 755–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Nidich SI, Rainforth MV, Haaga DA, Hagelin J, Salerno JW, Travis F, Tanner M, Gaylord-King C, Grosswald S, Schneider RH, A randomized controlled trial on effects of the Transcendental Meditation program on blood pressure, psychological distress, and coping in young adults, Am J Hypertens 22(12) (2009) 1326–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Panel on Handling Missing Data in Clinical Trials, Committee on National Statistics, Division of Behavioral and Social Sciences and Education, National Research Council, The Prevention and Treatment of Missing Data in Clinical Trials, The National Academies Press, Washington, D.C., 2010. [Google Scholar]
- [139].Rubin DB, Multiple Imputation for Nonresponse in Surveys, John Wiley & Sons, New York, NY, 1987. [Google Scholar]
- [140].Dmitrienko A, D’Agostino R Sr., Traditional multiplicity adjustment methods in clinical trials, Stat Med 32(29) (2013) 5172–218. [DOI] [PubMed] [Google Scholar]
- [141].Anand IS, Rector TS, Kuskowski M, Thomas S, Holwerda NJ, Cohn JN, Effect of baseline and changes in systolic blood pressure over time on the effectiveness of valsartan in the Valsartan Heart Failure Trial, Circ Heart Fail 1(1) (2008) 34–42. [DOI] [PubMed] [Google Scholar]
- [142].Johnson HM, Olson AG, LaMantia JN, Kind AJ, Pandhi N, Mendonca EA, Craven M, Smith MA, Documented lifestyle education among young adults with incident hypertension, J Gen Intern Med 30(5) (2014) 556–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Wallace ML, Magnan EM, Thorpe CT, Schumacher JR, Smith MA, Johnson HM, Diagnosis and treatment of incident hypertension among patients with diabetes: a U.S. multi-disciplinary group practice observational study, J Gen Intern Med 30(6) (2015) 768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Lawson EF, Hersh AO, Applebaum MA, Yelin EH, Okumura MJ, von Scheven E, Self-management skills in adolescents with chronic rheumatic disease: A cross-sectional survey, Pediatr Rheumatol Online J 9(1) (2011) 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Jerant AF, von Friederichs-Fitzwater MM, Moore M, Patients’ perceived barriers to active self-management of chronic conditions, Patient Educ Couns 57(3) (2005) 300–7. [DOI] [PubMed] [Google Scholar]
- [146].Lynch EB, Liebman R, Ventrelle J, Avery EF, Richardson D, A self-management intervention for African Americans with comorbid diabetes and hypertension: a pilot randomized controlled trial, Prev Chronic Dis 11 (2014) E90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Jelalian E, Boergers J, Alday CS, Frank R, Survey of physician attitudes and practices related to pediatric obesity, Clin Pediatr (Phila) 42(3) (2003) 235–45. [DOI] [PubMed] [Google Scholar]
- [148].Parra-Medina D, Wilcox S, Wilson DK, Addy CL, Felton G, Poston MB, Heart Healthy and Ethnically Relevant (HHER) Lifestyle trial for improving diet and physical activity in underserved African American women, Contemp Clin Trials 31(1) (2010) 92–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149].Davis SD, Brody AS, Emond MJ, Brumback LC, Rosenfeld M, Endpoints for clinical trials in young children with cystic fibrosis, Proc Am Thorac Soc 4(4) (2007) 418–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Beckstead JW, Yang CY, Lengacher CA, Assessing cross-cultural validity of scales: a methodological review and illustrative example, Int J Nurs Stud 45(1) (2008) 110–9. [DOI] [PubMed] [Google Scholar]
- [151].Gaffo AL, Roseman JM, Jacobs DR Jr., Lewis CE, Shikany JM, Mikuls TR, Jolly PE, Saag KG, Serum urate and its relationship with alcoholic beverage intake in men and women: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort, Ann Rheum Dis 69(11) (2010) 1965–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Tsai SA, Lv N, Xiao L, Ma J, Gender Differences in Weight-Related Attitudes and Behaviors Among Overweight and Obese Adults in the United States, Am J Mens Health E-pub ahead of print (2015). [DOI] [PubMed]
- [153].Burke GL, Bertoni AG, Shea S, Tracy R, Watson KE, Blumenthal RS, Chung H, Carnethon MR, The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis, Arch Intern Med 168(9) (2008) 928–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Matthews KA, Kelsey SF, Meilahn EN, Kuller LH, Wing RR, Educational attainment and behavioral and biologic risk factors for coronary heart disease in middle-aged women, Am J Epidemiol 129(6) (1989) 1132–44. [DOI] [PubMed] [Google Scholar]
- [155].Vriz O, Nesbitt S, Krause L, Majahalme S, Lu H, Julius S, Smoking is associated with higher cardiovascular risk in young women than in men: the Tecumseh Blood Pressure Study, J Hypertens 15(2) (1997) 127–34. [DOI] [PubMed] [Google Scholar]
- [156].O’Donnell DE, Hernandez P, Kaplan A, Aaron S, Bourbeau J, Marciniuk D, Balter M, Ford G, Gervais A, Lacasse Y, Maltais F, Road J, Rocker G, Sin D, Sinuff T, Voduc N, Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease - 2008 update - highlights for primary care, Can Respir J 15 Suppl A (2008) 1A–8A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].DeSalvo KB, Jones TM, Peabody J, McDonald J, Fihn S, Fan V, He J, Muntner P, Health care expenditure prediction with a single item, self-rated health measure, Med Care 47(4) (2009) 440–7. [DOI] [PubMed] [Google Scholar]
- [158].DeSalvo KB, Fan VS, McDonell MB, Fihn SD, Predicting mortality and healthcare utilization with a single question, Health Serv Res 40(4) (2005) 1234–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].McDowell I, Measuring Health: A Guide to Rating Scales and Questionnaires, 3rd ed, Oxford University Press, New York, NY, 2006. [Google Scholar]
- [160].Bass PF 3rd, Wilson JF, Griffith CH, A shortened instrument for literacy screening, J Gen Intern Med 18(12) (2003) 1036–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [161].Bass SB, Wolak C, Rovito GM, Gordon TF, Ward L, Use of REALM-R vs. S-TOFHLA in an urban African American clinic population to assess health literacy: Practical implications, American Public Health Association 138th Annual Meeting & Expo: Social Justice, Denver, CO, 2010. [Google Scholar]
- [162].Borzecki AM, Wong AT, Hickey EC, Ash AS, Berlowitz DR, Identifying hypertension-related comorbidities from administrative data: what’s the optimal approach?, Am J Med Qual 19(5) (2004) 201–6. [DOI] [PubMed] [Google Scholar]
- [163].Marciniak MD, Lage MJ, Dunayevich E, Russell JM, Bowman L, Landbloom RP, Levine LR, The cost of treating anxiety: the medical and demographic correlates that impact total medical costs, Depress Anxiety 21(4) (2005) 178–84. [DOI] [PubMed] [Google Scholar]
- [164].Sadock E, Auerbach SM, Rybarczyk B, Aggarwal A, Evaluation of integrated psychological services in a university-based primary care clinic, J Clin Psychol Med Settings 21(1) (2014) 19–32. [DOI] [PubMed] [Google Scholar]
- [165].Ahern DK, Gorkin L, Anderson JL, Tierney C, Hallstrom A, Ewart C, Capone RJ, Schron E, Kornfeld D, Herd JA, et al. , Biobehavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS), Am J Cardiol 66(1) (1990) 59–62. [DOI] [PubMed] [Google Scholar]
- [166].Elixhauser A, Steiner C, Harris DR, Coffey RM, Comorbidity measures for use with administrative data, Med Care 36(1) (1998) 8–27. [DOI] [PubMed] [Google Scholar]
- [167].Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM, Identifying persons with diabetes using Medicare claims data, Am J Med Qual 14(6) (1999) 270–7. [DOI] [PubMed] [Google Scholar]
- [168].Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ, Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999, J Am Soc Nephrol 16(2) (2005) 489–495. [DOI] [PubMed] [Google Scholar]
- [169].Sherbourne CD, Stewart AL, The MOS social support survey, Soc Sci Med 32(6) (1991) 705–14. [DOI] [PubMed] [Google Scholar]
- [170].Starfield B, Weiner J, Mumford L, Steinwachs D, Ambulatory care groups: a categorization of diagnoses for research and management, Health Serv Res 26(1) (1991) 53–74. [PMC free article] [PubMed] [Google Scholar]
- [171].Morisky DE, Green LW, Levine DM, Concurrent and predictive validity of a self-reported measure of medication adherence, Med Care 24(1) (1986) 67–74. [DOI] [PubMed] [Google Scholar]
- [172].Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA, Predictors of medication self-management skill in a low-literacy population, J Gen Intern Med 21(8) (2006) 852–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].DeWalt DA, Pignone MP, Reading is fundamental: the relationship between literacy and health, Arch Intern Med 165(17) (2005) 1943–4. [DOI] [PubMed] [Google Scholar]
- [174].Shelbourne CD, Social Functioning: Social Activity Limitations Measure, in: Stewart AL, Ware JE Jr. (Eds.), Measuring Functioning and Well-Being: The Medical Outcomes Study Approach, Duke University Press, Durham, NC, 1992, pp. 173–181. [Google Scholar]
- [175].Shelbourne CD, Stewart AL, Wells KB, Role Functioning Measures, in: Stewart AL, Ware JE Jr. (Eds.), Measuring Functioning and Well-Being: The Medical Outcomes Study Approach, Duke University Press, Durham, NC, 1992, pp. 205–219. [Google Scholar]
- [176].Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ, Racial differences in blood pressure control: potential explanatory factors, J Gen Intern Med 23(5) (2008) 692–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [177].Thompson FE, Dixit-Joshi S, Potischman N, Dodd KW, Kirkpatrick SI, Kushi LH, Alexander GL, Coleman LA, Zimmerman TP, Sundaram ME, Clancy HA, Groesbeck M, Douglass D, George SM, Schap TE, Subar AF, Comparison of Interviewer-Administered and Automated Self-Administered 24-Hour Dietary Recalls in 3 Diverse Integrated Health Systems, Am J Epidemiol 181(12) (2015) 970–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Blair SN, Haskell WL, Ho P, Paffenbarger RS Jr., Vranizan KM, Farquhar JW, Wood PD, Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments, Am J Epidemiol 122(5) (1985) 794–804. [DOI] [PubMed] [Google Scholar]
- [179].Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS Jr., Physical activity assessment methodology in the Five-City Project, Am J Epidemiol 121(1) (1985) 91–106. [DOI] [PubMed] [Google Scholar]
- [180].Sidney S, Jacobs DR Jr., Haskell WL, Armstrong MA, Dimicco A, Oberman A, Savage PJ, Slattery ML, Sternfeld B, Van Horn L, Comparison of two methods of assessing physical activity in the Coronary Artery Risk Development in Young Adults (CARDIA) Study, Am J Epidemiol 133(12) (1991) 1231–45. [DOI] [PubMed] [Google Scholar]
- [181].Young DR, Haskell WL, Taylor CB, Fortmann SP, Effect of community health education on physical activity knowledge, attitudes, and behavior. The Stanford Five-City Project, Am J Epidemiol 144(3) (1996) 264–74. [DOI] [PubMed] [Google Scholar]
- [182].Blair SN, Applegate WB, Dunn AL, Ettinger WH, Haskell WL, King AC, Morgan TM, Shih JA, Simons-Morton DG, Activity Counseling Trial (ACT): rationale, design, and methods. Activity Counseling Trial Research Group, Med Sci Sports Exerc 30(7) (1998) 1097–106. [DOI] [PubMed] [Google Scholar]
- [183].Dolor RJ, Yancy WS Jr., Owen WF, Matchar DB, Samsa GP, Pollak KI, Lin PH, Ard JD, Prempeh M, McGuire HL, Batch BC, Fan W, Svetkey LP, Hypertension Improvement Project (HIP): study protocol and implementation challenges, Trials 10 (2009) 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184].Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H, Reliability of reporting self-measured blood pressure values by hypertensive patients, Am J Hypertens 11(12) (1998) 1413–7. [DOI] [PubMed] [Google Scholar]
- [185].Gunther AL, Liese AD, Bell RA, Dabelea D, Lawrence JM, Rodriguez BL, Standiford DA, Mayer-Davis EJ, Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus, Hypertension 53(1) (2009) 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr., Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004, Arch Intern Med 168(3) (2008) 308–14. [DOI] [PubMed] [Google Scholar]
- [187].Adams MA, Norman GJ, Hovell MF, Sallis JF, Patrick K, Reconceptualizing decisional balance in an adolescent sun protection intervention: mediating effects and theoretical interpretations, Health Psychol 28(2) (2009) 217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [188].Ryan RM, Patrick H, Deci EL, Williams GC, Facilitating health behaviour change and its maintenance: Interventions based on Self-Determination Theory, Eur Health Psychologist 10 (2008) 2–5. [Google Scholar]
- [189].Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ, Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors, Health Educ Res 22(5) (2007) 691–702. [DOI] [PubMed] [Google Scholar]
- [190].Hibbard JH, Stockard J, Mahoney ER, Tusler M, Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers, Health Serv Res 39(4 Pt 1) (2004) 1005–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [191].Hibbard JH, Mahoney ER, Stockard J, Tusler M, Development and testing of a short form of the patient activation measure, Health Serv Res 40(6 Pt 1) (2005) 1918–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J, Is patient activation associated with outcomes of care for adults with chronic conditions?, J Ambul Care Manage 30(1) (2007) 21–9. [DOI] [PubMed] [Google Scholar]
- [193].Hibbard JH, Tusler M, Assessing activation stage and employing a “next steps” approach to supporting patient self-management, J Ambul Care Manage 30(1) (2007) 2–8. [DOI] [PubMed] [Google Scholar]
- [194].Becker ER, Roblin DW, Translating primary care practice climate into patient activation: the role of patient trust in physician, Med Care 46(8) (2008) 795–805. [DOI] [PubMed] [Google Scholar]
- [195].Zill JM, Dwinger S, Kriston L, Rohenkohl A, Harter M, Dirmaier J, Psychometric evaluation of the German version of the Patient Activation Measure (PAM13), BMC Public Health 13 (2013) 1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [196].Wilson DK, Evans AE, Williams J, Mixon G, Sirard JR, Pate R, A preliminary test of a student-centered intervention on increasing physical activity in underserved adolescents, Ann Behav Med 30(2) (2005) 119–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [197].Bauer DJ, Preacher KJ, Gil KM, Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: new procedures and recommendations, Psychol Methods 11(2) (2006) 142–63. [DOI] [PubMed] [Google Scholar]
- [198].Kenny DA, Korchmaros JD, Bolger N, Lower level mediation in multilevel models, Psychol Methods 8(2) (2003) 115–28. [DOI] [PubMed] [Google Scholar]
- [199].Krull JL, MacKinnon DP, Multilevel mediation modeling in group-based intervention studies, Eval Rev 23(4) (1999) 418–44. [DOI] [PubMed] [Google Scholar]
- [200].Krull JL, MacKinnon DP, Multilevel Modeling of Individual and Group Level Mediated Effects, Multivariate Behav Res 36(2) (2001) 249–77. [DOI] [PubMed] [Google Scholar]
- [201].Preacher KJ, Zyphur MJ, Zhang Z, A general multilevel SEM framework for assessing multilevel mediation, Psychol Methods 15(3) (2010) 209–33. [DOI] [PubMed] [Google Scholar]
- [202].Pituch KA, Stapleton LM, Kang JY, A Comparison of Single Sample and Bootstrap Methods to Assess Mediation in Cluster Randomized Trials, Multivariate Behav Res 41(3) (2006) 367–400. [DOI] [PubMed] [Google Scholar]
- [203].Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH, Self-management education programs in chronic disease: a systematic review and methodological critique of the literature, Arch Intern Med 164(15) (2004) 1641–9. [DOI] [PubMed] [Google Scholar]
- [204].Eccleston C, Fisher E, Law E, Bartlett J, Palermo TM, Psychological interventions for parents of children and adolescents with chronic illness, Cochrane Database Syst Rev 4 (2015) CD009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Cantrell J, Hair EC, Smith A, Bennett M, Rath JM, Thomas RK, Fahimi M, Dennis JM, Vallone D, Recruiting and retaining youth and young adults: challenges and opportunities in survey research for tobacco control, Tob Control 27(2) (2018) 147–154. [DOI] [PubMed] [Google Scholar]
- [206].Rocha-Goldberg Mdel P, Corsino L, Batch B, Voils CI, Thorpe CT, Bosworth HB, Svetkey LP, Hypertension Improvement Project (HIP) Latino: results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults, Ethn Health 15(3) (2010) 269–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [207].Pedersen ER, Naranjo D, Marshall GN, Recruitment and retention of young adult veteran drinkers using Facebook, PLoS One 12(3) (2017) e0172972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208].Norris SL, Engelgau MM, Narayan KM, Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials, Diabetes Care 24(3) (2001) 561–87. [DOI] [PubMed] [Google Scholar]
- [209].Buscemi J, Blumstein L, Kong A, Stolley MR, Schiffer L, Odoms-Young A, Bittner C, Fitzgibbon ML, Retaining traditionally hard to reach participants: Lessons learned from three childhood obesity studies, Contemp Clin Trials 42 (2015) 98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [210].Corser W, Sikorskii A, Olomu A, Stommel M, Proden C, Holmes-Rovner M, “Concordance between comorbidity data from patient self-report interviews and medical record documentation”, BMC Health Serv Res 8 (2008) 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [211].Taber DR, Stevens J, Murray DM, Elder JP, Webber LS, Jobe JB, Lytle LA, The effect of a physical activity intervention on bias in self-reported activity, Ann Epidemiol 19(5) (2009) 316–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [212].Ma J, King AC, Wilson SR, Xiao L, Stafford RS, Evaluation of lifestyle interventions to treat elevated cardiometabolic risk in primary care (E-LITE): a randomized controlled trial, BMC Fam Pract 10 (2009) 71. [DOI] [PMC free article] [PubMed] [Google Scholar]