Abstract
Objectives:
Insomnia is an important clinical problem affecting the elderly. We examined trends in insomnia diagnosis and treatment among Medicare beneficiaries over an eight-year period.
Design:
Time series
Setting and Participants:
5% sample of Medicare administrative data for years 2006–2013 Measurements: Insomnia was defined as the presence of at least one claim containing International Classification of Disease, Version 9, Clinical Modification (ICD-9-CM) codes 307.41, 307.42, 307.49, 327.00, 327.01, 327.09, 780.52, V69.4 in any given year. Insomnia medications were identified by searching the Part D prescription drug files in each year for barbiturates, benzodiazepines, chloral hydrate, hydroxyzine, non-benzodiazepine sedative hypnotics, and sedating antidepressants.
Results:
Prevalence of physician-assigned insomnia diagnoses increased from 3.9% in 2006 to 6.2% in 2013. Prevalence of any insomnia medication use ranged from 21.0% in 2006 to 29.6% in 2013 but remained steady. A sharp increase in use of benzodiazepines from 2012–2013 (1.1% to 17.6%) drove up total insomnia medication use for 2013. Prevalence of both insomnia diagnosis and medication use ranged from 3.5% in 2006 to 5.5% in 2013, while prevalence of either insomnia diagnosis or medication use ranged from 22.7% in 2006 to 31.0% in 2013.
Conclusions:
In this large national analysis of Medicare beneficiaries, prevalence of physician-assigned insomnia diagnoses was low but increased over time. Prevalence of insomnia medication use was up to four-times higher than insomnia diagnoses and remained steady over time. Notably, prevalence of benzodiazepine use increased dramatically from 2012–2013 after these medications were included in the Medicare Part D formulary.
Keywords: Insomnia, Insomnia medication, Medicare, Older adults
Introduction
Sleep complaints increase across the lifespan and are omnipresent among older adults, with half of older adults reporting poor sleep quality.(1–4) The most common diagnosis is insomnia disorder, defined as difficulty initiating or maintaining sleep with associated daytime impairment. Among the general population, lifetime prevalence estimates for chronic insomnia have historically ranged from 9–12%.(5) Among older adults, the annual prevalence of insomnia ranges from 25–40%.(1) Among older adults, insomnia disorder is associated with increased morbidity, mortality, diminished quality of life, and increased health care utilization.(6, 7) The most common treatment for insomnia remains pharmacotherapy, and a number of FDA-approved medications are available.(8) However, in spite of clinical effectiveness, many sedative hypnotic compounds, including traditional benzodiazepines as well as newer non-benzodiazepine sedative hypnotics (NBSH, e.g., newer “z-drugs” such as eszopiclone, zaleplon, and zolpidem, as well as a melatonin receptor agonist, ramelteon), have been associated with increased risk of falls, fractures, and cognitive side effects among older adults.(9–12) Thus, sleep medications must be used with caution in this population, and older benzodiazepines should be avoided whenever possible, due to unfavorable risk-benefit ratios.(9) Despite the high prevalence and substantial adverse consequences of the condition, as well as the need for careful treatment of insomnia among older adults, few population-level studies have characterized longitudinal trends in insomnia diagnosis or treatment in the US.(9) In light of the aging US population, such insight could provide valuable guidance to payers, policy-makers, and health systems leaders seeking to optimize outcomes, allocate scare resources, and manage health for the future.(13)
Most of what is known regarding insomnia-related trends among older adults stems from analyses of data from the National Ambulatory Medical Care Survey (NAMCS). Using this dataset, Moloney and colleagues found that between the years 1993 to 2007, insomnia diagnoses among older adults increased from 21.9 to 53.0 per 10,000 office visits.(14) Similarly, Maust and colleagues reported that between the years 2003–2012, insomnia diagnoses continued to increase during both primary care and psychiatric office visits.(3) Finally, Ford and colleagues reported that sleep-related diagnoses among adults aged 65 and older increased from 0.5% of office visits in 1999 to 1.3% of office visits in 2010.(15) In terms of insomnia treatment, population-level analyses of data from the NAMCS and National Health and Nutrition Examination Survey (NHANES) have found increases in prescriptions for sleep medications during the 1990s and 2000s.(2, 16) For example, in an analysis of the NAMCS, Ford and colleagues found that between the years 1999 to 2010, prescriptions for NBSH for older adults increased from 0.7% of office visits to 2.0% of office visits.(15) In terms of traditional benzodiazipine receptor agonists, some studies have shown an increase in prescriptions among older adults during this time interval, while others have found no increase over time.(3, 15) From both epidemiologic and clinical perspectives, the use of benzodiazipines among older adults is of particular interest given their well-documented risks and recent (2012) addition to the Centers for Medicare and Medicaid prescription drug formulary.
The purpose of the current investigation was to examine trends in insomnia diagnosis and treatment among a randomly selected, nationally representative sample of older adult Medicare beneficiaries in the US. The primary hypotheses were: 1) insomnia diagnoses and insomnia-related prescriptions increased over time; and 2) an increase in prescriptions for benzodiazepines would be observed following their inclusion into the Medicare prescription drug formulary in 2012.
Methods
Data Source
A 5% random sample of Medicare administrative data obtained from the Centers for Medicare & Medicaid Services (CMS) Chronic Condition Data Warehouse (CCW) for years 2006–2013 was the primary source of data for this study.
Study design and procedures
A time-series analysis was conducted to estimate the prevalence of insomnia and use of insomnia-related medications among Medicare beneficiaries over an eight-year period. Statistical significance was defined as p<0.05. All analysis was performed with SAS version 9.4 (SAS Institute, Cary, NC). This study was approved by the Institutional Review Board of the University of Maryland, Baltimore.
Insomnia
Insomnia was defined as the presence at least one inpatient or outpatient claim with International Classification of Disease, Version 9, Clinical Modification (ICD-9-CM) codes 307.41, 307.42, 307.49, 327.00, 327.01, 327.09, 780.52, V69.4. In any given year, a beneficiary was required to receive at least one diagnosis of insomnia in any position on a claim to be counted toward the insomnia prevalence estimate for that year.
Insomnia Medications
Insomnia medications were identified by searching the Part D prescription drug files in each year. Specific classes and medications included barbiturates - amobarbital, butabarbital, pentobarbital, secobarbital, phenobarbital, mephobarbital; benzodiazepines – alprazolam, clonazepam, estazolam, flurazepam, lorazepam, oxazepam, quazepam, temazepam, triazolam; chloral hydrate; hydroxyzine; non-benzodiazepine sedative hypnotics (NBSH) - eszopiclone, zaleplon, zolpidem; ramelteon; sedating anti-depressants - amitriptyline, nortriptyline, doxepin, clomipramine, trazodone, nefazodone, mirtazapine. In any given year, insomnia medication use was defined by at least one prescription fill for any of the listed medications.
Data Analysis
Annual prevalence was calculated by dividing the numerator (number of beneficiaries with at least one ICD-9-CM diagnosis of insomnia or at least one fill of an insomnia medication) by an appropriate denominator. Specifically, the denominator for insomnia prevalence calculations was the number of beneficiaries with at least ten months of Medicare Parts A & B with no Part C (Medicare Advantage) coverage in each year. Medicare Advantage claims were not consistently available in the data. The denominator for insomnia medication prevalence estimates was the number of beneficiaries with at least ten months of continuous Medicare Parts A, B, and D (prescription drug plan) with no Part C coverage in each year.
Annual prevalence was calculated for any insomnia medication and for the four most prevalent classes or drugs (sedating antidepressants, hydroxyzine, NBSH, benzodiazepines). Individuals could contribute to the numerators of more than one class category but were not “double counted” for overall prevalence of insomnia medication use. To increase sensitivity and account for possible underdiagnosis of insomnia, we calculated prevalence of either an insomnia diagnosis or insomnia medication use using the denominator for insomnia medications. In this case, beneficiaries in the numerator with an insomnia diagnosis were required to have at least ten months of continuous Medicare Parts A, B, and D with no Part C coverage in each year. Finally, to increase specificity of the insomnia diagnosis, we calculated annual prevalence of an insomnia diagnosis and insomnia medication use using the same denominator. Annual prevalence by year and sex were plotted.
In time series data, error terms are often serially correlated which can lead to biased standard errors when typical regression methods are used. Thus, to assess annual trends in prevalence, we used a first-order linear autoregressive model which corrects for autocorrelated error terms. The impact of sex was evaluated by stratifying the autoregressive models by sex.
Results
Insomnia
The number of beneficiaries in the 5% sample with at least ten months of Medicare Parts A & B with no Part C coverage ranged from 1,732,766 in 2006 to 1,717,642 in 2013. Annual prevalence of insomnia diagnoses increased from 3.9% in 2006 to 6.2% in 2013 (Figure 1). There was a significant increasing trend in diagnoses over time (t=8.9, df=5, p<0.001).
Figure 1.
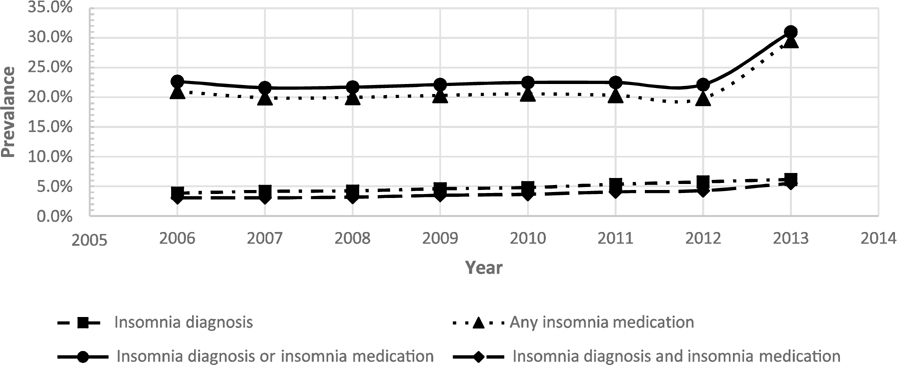
Annual prevalence of insomnia diagnosis, by International Classification of Disease code, medication use, either, or both, 2006–2013
Insomnia Medication
The number of beneficiaries in the 5% sample with at least ten months of Medicare Parts A, B, & D with no Part C coverage increased from 617,877 (2006) to 1,079,432 (2013). Annual prevalence of any insomnia medication use ranged from 21.0% in 2006 to 29.6% in 2013 (Figure 1). The trend test was not significant (t=1.0, df=5, p=0.37).
Sedating antidepressants, NBSH, hydroxyzine, and benzodiazepines were the most prevalent insomnia medications (Figure 2). Use of hydroxyzine (t=−3.2, df=5, p=0.03), ramelteon (t=−4.7, df=5, p=0.01), and chloral hydrate (t=−4.2, df=5, p=0.01) decreased slightly over time. Annual prevalence of other insomnia medications remained relatively stable until 2012. Between 2012 and 2013, annual prevalence of benzodiazepines increased from 1.1% to 17.6%.
Figure 2.
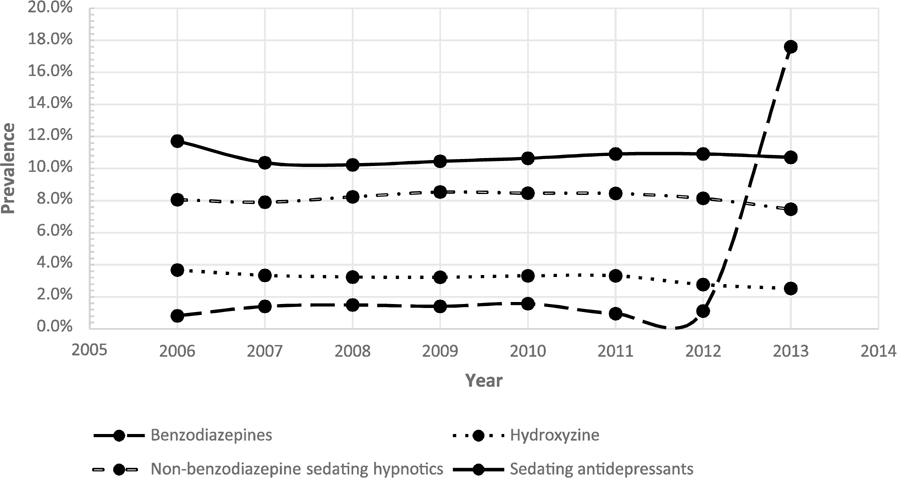
Annual prevalence of insomnia medication use, 2006–2013
Insomnia and/or insomnia medication
Annual prevalence of both insomnia diagnosis and medication use was low, ranging from 3.5% in 2006 to 5.5% in 2013. There was a significant increasing trend over time (t=3.1, df=5, p=0.03). Annual prevalence of either insomnia diagnosis or medication use ranged from 22.7% (2006) to 31.0% (2013)(See Figure 1). The time trend was not significant (t=1.2, df=5, p=0.27).
Insomnia and insomnia medication use by sex
Figure 3 displays insomnia diagnosis, medication use, diagnosis or medication use, and diagnosis and medication use, stratified by sex. Women had higher annual prevalence of insomnia diagnosis and medication use, whether alone or in combination. There was a significant increasing trend for insomnia diagnosis for women (t=8.5, df=5, p<0.001) and men (t=9.7, df=5, p<0.001). Similarly there was a significant increasing trend for insomnia diagnosis and medication use for women (t=2.9, df=5, p=0.03) and men (t=3.6, df=5, p=0.02).
Figure 3.
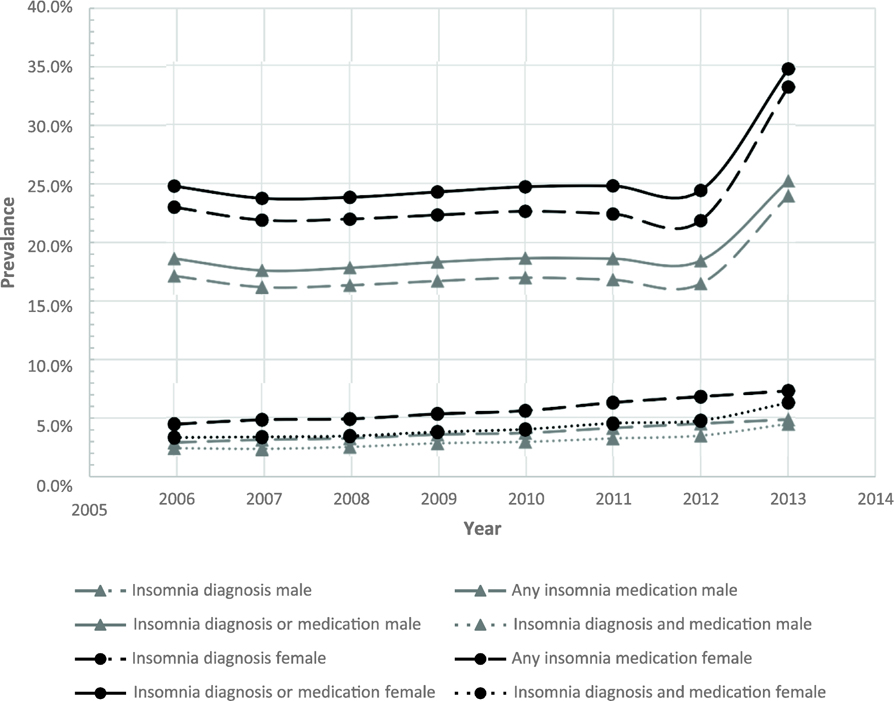
Annual prevalence of insomnia diagnosis, by International Classification of Disease code, medication use, either, or both, by sex, 2006–2013
Figure 4 displays prevalence of insomnia medication classes over time, stratified by sex. Annual prevalence of use of sedating antidepressants, NBSH, and hydroxyzine was higher among women.
Figure 4.
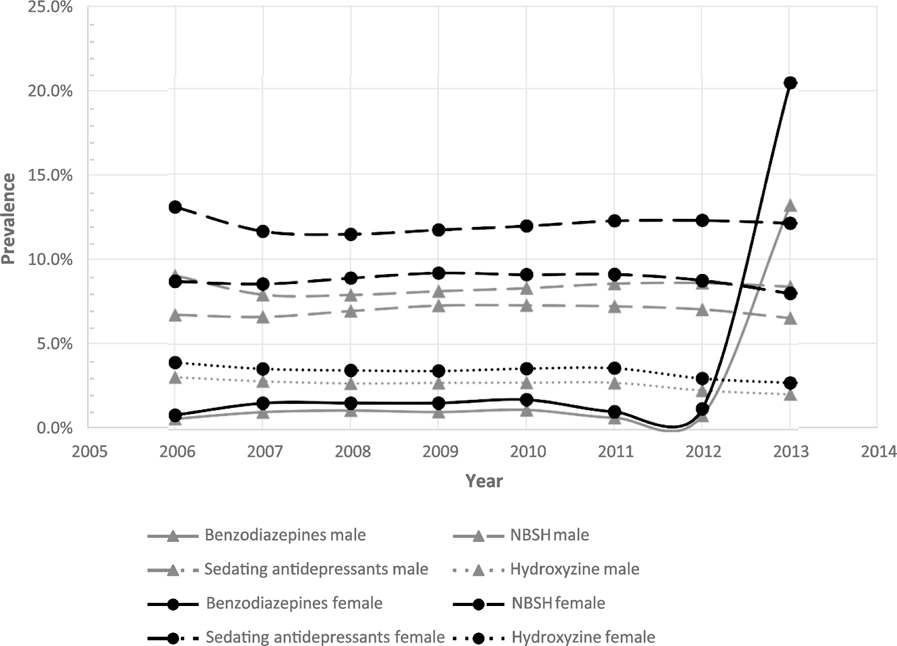
Annual prevalence of insomnia medication use by sex, 2006–2013
Discussion
In this national analysis of a large sample of Medicare beneficiaries conducted from 2006 – 2013, prevalence of insomnia diagnoses was low but increased over time. Annual prevalence of insomnia medication use was up to four-times higher than insomnia diagnoses and remained steady over time. Notably, annual prevalence of benzodiazepine use increased dramatically from 2012–2013 after Medicare extended Part D coverage to include them.
Prior estimates of insomnia disorder prevalence among older adults have ranged from 25%−40%.(1) Our study’s much lower estimates (4%−6%) are likely due to our operational definition of insomnia. Whereas previous studies were based on survey assessments, we defined insomnia using provider-assigned ICD-9-CM codes. In a study that used multiple methods to ascertain insomnia diagnosis, Roth and colleagues reported population prevalence of insomnia in 2009 to be 3.9% based ICD-10-CM criteria, 14.7% based on International Classification of Sleep Disorders – Second Edition criteria, and 22.1% based on Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition.(17) Our results are consistent with those of Roth et al, accounting for the increasing time trend, and suggest that insomnia continues to be underdiagnosed.(17)
Conversely, prevalence of insomnia medication use among Medicare beneficiaries was high and remained steady from 2006–2012. These results contrast with prior studies in mixed age populations that have reported increases in NBSH use over time.(2, 16) Although no prior studies have estimated annual prevalence of insomnia medication use among older adults, Bertisch et al. (2014) reported that monthly NBSH use among adults ≥18 years increased from <1% in 1999 to almost 2% in 2009.(16) Similarly, Ford at el (2014) reported that annual office visits associated with a prescription for NBSH among adults age 20 and older increased from 0.5% in 1999 to 2.3% in 2009.(15) Unlike these prior studies, our study focused specifically on older adults and examined annual prevalence which could explain our higher estimates (8%) for NBSH use.
The increase in prevalence of benzodiazepine use from 2012–2013 came at a time when nursing homes were mandated to reduce antipsychotic use and may reflect substitution of benzodiazepines for antipsychotics to control behavioral symptoms in that population.(18) Medicare’s decision to include benzodiazepines in their formulary could also have shifted the payment structure, but not necessarily use among most beneficiaries. However, the prevalence of benzodiazepine use that we observed in 2013 was double that reported using a dataset of retail pharmacies from 2008 among those age 65 – 80 years, suggesting that this hypothesis does not fully explain the observed increase.(4) Nonetheless, benzodiazepines are on the Beer’s list of medications to be avoided in older adults and their use should be monitored closely in this population.(9)
The strengths of this study include a large national sample and eight years of data. Much of the previous literature on this topic has relied on the NAMCS, which uses the office visit as the unit of observation. In contrast, this study uses the person as the unit of analysis, allowing for the estimation of prevalence of physician-assigned insomnia diagnoses and medication use among Medicare beneficiaries. In contrast with the NAMCS, which assesses provider prescribing behavior, and the NHANES, which relies on patient self-report of medication use, our study required filled prescriptions for insomnia medications. Finally, this study is among the first to quantify the increase in prevalence of benzodiazepine use following their 2012 placement on Medicare formulary.
Our study is limited in that we were not able to ascertain indications for the prescribed medications. Because some medications used for the treatment of insomnia (e.g. sedating antidepressants, benzodiazepines) have other indications, it is possible that our results overestimate insomnia medication use. That said, our methodology is well-established in the literature. Further, our time-series design did not enable longitudinal analysis of individuals over time. Thus, we are unable to draw conclusions regarding duration of insomnia or insomnia medication use. We used linear regression within an autoregressive model to evaluate the significance of time trends of proportions. This may have introduced some error in test statistic estimation. Finally, an inherent limitation of administrative data is the inability to provide insight into severity of insomnia symptoms, objective measures of sleep, or other clinical variables of interest.
The objective of the current investigation was to describe overall patterns in insomnia diagnosis and prescription sleep aid use. Our data suggest that insomnia is commonly treated, but infrequently diagnosed. Future research should seek to understand the consequences and causes of this discrepancy. For example, perhaps coding practices are related to quality of clinical care and thus associated with patient outcomes. Modern conceptualizations of insomnia, including the nosology of the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition(19), eschew outdated distinctions of primary and secondary insomnia in favor of the more accurate and accepted insomnia disorder, which can occur in isolation or comorbid with other medical and psychiatric disorders. In this vein, the role of provider specialty should also be explored in support of tailored provider insomnia education and treatment implementation efforts. Finally, given that nearly 20% of the Medicare population uses a prescription sleep aid, other relevant questions include polypharmacy and safety. For example, previous studies have found an association between concomitant use of benzodiazepines or NBSH and opioids and increased risk of overdose death.(20–22) This study raises important questions about insomnia diagnosis, prescribing practices, and medication interactions. From a clinical perspective, comprehensive sleep evaluation, careful treatment planning, and close follow-up are essential, especially when treating older adults.
In conclusion, in this national sample of Medicare beneficiaries, prevalence of insomnia diagnoses was low and increased over an eight-year period. Conversely, prevalence of insomnia medication usage, while much higher, remained steady over time. Our results confirm those of other studies suggesting that insomnia remains significantly underdiagnosed, despite active insomnia treatment.
Highlights.
This study assessed trends in insomnia diagnosis and treatment in the US using a 5% sample of Medicare administrative data for years 2006–2013.
Prevalence of physician-assigned insomnia diagnoses increased from 3.9% in 2006 to 6.2% in 2013. Prevalence of any insomnia medication use ranged from 21.0% in 2006 to 29.6% in 2013 but remained steady through 2012.
This study highlights the disparity between insomnia diagnosis and treatment and raises important questions regarding clinical evaluation and management of insomnia among older adults.
Acknowledgements
Sources of Funding
This research was supported by an investigator-initiated grant awarded from Merck & Co to The University of Maryland. Baltimore (PI: Wickwire). JSA is supported by Agency for Healthcare Research and Quality grant K01HS024560. SET is supported by National Institute on Aging grant K01AG050723. JSA, EMW, and SMS’s institution has received research funding from Merck and ResMed. EMW has served as a scientific consultant to Merck and is an equity shareholder in WellTap. AV is supported by National Institutes of Health grant T32AG000262.
This research was supported by an investigator-initiated grant awarded from Merck & Co to The University of Maryland. Baltimore (PI: Wickwire). JSA is supported by Agency for Healthcare Research and Quality grant K01HS024560. SET is supported by National Institute on Aging grant 1K01AG050723. JSA, EMW, and SMS’s institution has received research funding from Merck and ResMed. EMW has served as a scientific consultant to Merck and is an equity shareholder in WellTap. AV is supported by National Institutes of Health grant T32AG000262.
Sponsor’s Role: The sponsor had no role in the design of the study, reporting of results or preparation of the paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
No other conflicts of interests are declared. Results from this study were presented at SLEEP, June 2018, Baltimore, MD.
References
- 1.Ancoli-Israel S: Sleep and its disorders in aging populations. Sleep medicine 2009; 10 Suppl 1:S7–11 [DOI] [PubMed] [Google Scholar]
- 2.Kaufmann CN, Spira AP, Alexander GC, et al. : Trends in prescribing of sedative-hypnotic medications in the USA: 1993–2010. Pharmacoepidemiology and drug safety 2016; 25:637–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maust DT, Blow FC, Wiechers IR, et al. : National Trends in Antidepressant, Benzodiazepine, and Other Sedative-Hypnotic Treatment of Older Adults in Psychiatric and Primary Care. The Journal of clinical psychiatry 2017; 78:e363–e371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olfson M, King M,Schoenbaum M: Benzodiazepine use in the United States. JAMA psychiatry 2015; 72:136–142 [DOI] [PubMed] [Google Scholar]
- 5.Ford DE,Kamerow DB: Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama 1989; 262:1479–1484 [DOI] [PubMed] [Google Scholar]
- 6.Pollack M, Seal B, Joish VN, et al. : Insomnia-related comorbidities and economic costs among a commercially insured population in the United States. Current medical research and opinion 2009; 25:1901–1911 [DOI] [PubMed] [Google Scholar]
- 7.Wickwire EM, Shaya FT,Scharf SM: Health economics of insomnia treatments: The return on investment for a good night’s sleep. Sleep medicine reviews 2016; 30:72–82 [DOI] [PubMed] [Google Scholar]
- 8.Neubauer DN: New and emerging pharmacotherapeutic approaches for insomnia. International review of psychiatry (Abingdon, England) 2014; 26:214–224 [DOI] [PubMed] [Google Scholar]
- 9.Panel TAGSBCUE: American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society 2015; 63:2227–2246 [DOI] [PubMed] [Google Scholar]
- 10.Diaz-Gutierrez MJ, Martinez-Cengotitabengoa M, Saez de Adana E, et al. : Relationship between the use of benzodiazepines and falls in older adults: A systematic review. Maturitas 2017; 101:17–22 [DOI] [PubMed] [Google Scholar]
- 11.Stewart SA: The effects of benzodiazepines on cognition. The Journal of clinical psychiatry 2005; 66 Suppl 2:9–13 [PubMed] [Google Scholar]
- 12.Tom SE, Wickwire EM, Park Y, et al. : Nonbenzodiazepine Sedative Hypnotics and Risk of Fall-Related Injury. Sleep 2016; 39:1009–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaudette E, Tysinger B, Cassil A, et al. : Health and Health Care of Medicare Beneficiaries in 2030. Forum for health economics & policy 2015; 18:75–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moloney ME, Konrad TR,Zimmer CR: The medicalization of sleeplessness: a public health concern. American journal of public health 2011; 101:1429–1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford ES, Wheaton AG, Cunningham TJ, et al. : Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medications among US adults: findings from the National Ambulatory Medical Care survey 1999–2010. Sleep 2014; 37:1283–1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bertisch SM, Herzig SJ, Winkelman JW, et al. : National use of prescription medications for insomnia: NHANES 1999–2010. Sleep 2014; 37:343–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth T, Coulouvrat C, Hajak G, et al. : Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biological psychiatry 2011; 69:592–600 [DOI] [PubMed] [Google Scholar]
- 18.Services CfMM: CMS Announces Partnership to Imporve Dementia Care in Nurisng Homes, Baltimore, MD, Centers for Medicare & Medicaid Services, 2012 [Google Scholar]
- 19.Association AP: Diagnostic and Statistical Manual of Mental Disorders, 5th Washington, DC, American Psychiatric Association, 2013 [Google Scholar]
- 20.Abrahamsson T, Berge J, Ojehagen A, et al. : Benzodiazepine, z-drug and pregabalin prescriptions and mortality among patients in opioid maintenance treatment-A nation-wide register-based open cohort study. Drug and alcohol dependence 2017; 174:58–64 [DOI] [PubMed] [Google Scholar]
- 21.Park TW, Saitz R, Ganoczy D, et al. : Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ (Clinical research ed.) 2015; 350:h2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun EC, Dixit A, Humphreys K, et al. : Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ (Clinical research ed.) 2017; 356:j760. [DOI] [PMC free article] [PubMed] [Google Scholar]


