Abstract
Objective
High proportions of post-9/11 veterans have musculoskeletal disorders (MSDs), but engaging them in care early in their course of illness has been challenging. The service connection application is an ideal point of contact for referring veterans to early interventions for their conditions.
Design
Among MSD claimants who reported risky substance use, we pilot-tested a counseling intervention targeting pain and risky substance use called Screening Brief Intervention and Referral to Treatment–Pain Module (SBIRT-PM). Veterans were randomly assigned in a 2:1:1 ratio to SBIRT-PM, Pain Module counseling only, or treatment as usual (TAU).
Methods
Participants assigned to either counseling arm were offered a single meeting with a study therapist with two follow-up telephone calls as needed. Participants completed outcome assessments at four and 12 weeks after randomization.
Results
Of 257 veterans evaluated, 101 reported risky substance use and were randomized. Counseling was attended by 75% of veterans offered it and was well received. VA pain-related services were used by 51% of participants in either of the pain-focused conditions but only by 27% in TAU (P < 0.04). Starting with average pain severity ratings of 5.1/10 at baseline, only minimal changes in mean pain severity were noted regardless of condition. Self-reported risky substance use was significantly lower over time in the SBIRT-PM condition relative to the two other conditions (P < 0.02). At week 12, proportions of veterans reporting risky substance use were 0.39, 0.69, and 0.71 for the SBIRT-PM, Pain Module counseling, and TAU conditions, respectively.
Conclusions
SBIRT-PM shows promise as a way to engage veterans in pain treatment and reduce substance use.
Keywords: Pain, Addiction, Chronic Pain, Veterans, Disability, Musculoskeletal Disorder
Introduction
Veterans [1] and other populations [2] with musculoskeletal disorders (MSDs) often develop chronic pain [3] and are at high risk for substance misuse [4–8]. More than half of post-9/11 veterans have MSD and typically experience significant pain-related distress, sometimes exacerbated by substance misuse [9]. Early intervention is needed to ameliorate worsening pain and the initiation or exacerbation of risky substance use.
Veterans’ applications for compensation for injuries caused or worsened by their military service are an opportunity for early intervention. While in active service or immediately after separating from the service, veterans often interact with the Department of Veterans Affairs (VA) when applying for compensation for injuries connected to their military service but are not necessarily focused on seeking VA-provided or other treatment. As of 2015, there were 559,999 post-9/11 veterans being compensated for back or neck conditions, and 596,250 for limitation of flexion in joints [10]. In the 2015 fiscal year, 313,052 veterans were newly awarded service connection, and 80,748 newly awarded claims were for back and/or neck conditions.
Veterans who have submitted a claim for a service-connected condition are promised a fair evaluation of their claim and, if offered treatment for the claimed or other conditions, may wonder if the treatment offer will impact the results of their claim. For example, many veterans believe that having a substance use problem decreases the likelihood that their MSD claim will be approved (Black, Perez-Ortiz, and Rosen, unpublished data). Therefore, counseling at the time of a service connection examination must be transparent regarding the extent to which information disclosed during counseling might impact a decision about the claim and, as much as possible, minimize the impact of the counseling information on the claim award or denial [11]. Veterans may also feel coerced to participate in counseling if the examiner for an MSD claim suggests treatment as part of his/her examination. It is advised, therefore, that any treatment recommendations be provided apart from the service connection examination by an independent clinician. Using these essential elements along with an independent clinician delivering a Motivational Interviewing (MI)–based intervention, our group has previously shown that veterans presenting for post-traumatic stress disorder (PTSD) service connection claims can be effectively counseled about the sensitive issue of working for pay while receiving service connection [12].
In this current study, we developed an MI-based intervention to promote engagement in treatment for pain along with brief substance use counseling for veterans applying for MSD service connection. Multiple meta-analyses have shown that MI facilitates engagement in chronic pain treatment [13,14] and other treatments [15–17]. The MI framework was adopted to minimize the extent to which recommended treatments were perceived as coercive or related to the service connection claim.
The developed intervention, Screening Brief Intervention and Referral to Treatment–Pain Module (SBIRT-PM) involves first discussing pain associated with the veterans’ MSD, and then transitioning to a discussion of pain coping behaviors, and, ultimately, to veteran substance use. Substance use is addressed through the SBIRT, an extensively studied approach to identify and briefly intervene with patients with risky substance use in settings not typically associated with addiction treatment [18,19]. SBIRT has been efficacious for reducing unhealthy alcohol [20,21] and tobacco use [22–24], although its efficacy is less well established for decreasing illicit drug use [25,26] or improving drinking outcomes for people with severe alcohol dependence [27,28].
We conducted a pilot clinical trial to describe the feasibility, acceptability, and preliminary efficacy of SBIRT-PM among veterans applying for service connection for MSD. Because of the possibility that the SBIRT component of the SBIRT-PM might raise potentially problematic substance use issues that could interfere with a salutary effect of the SBIRT-PM’s pain module, we also included the delivery of the pain module only (without the subsequent substance use–focused SBIRT) as a standalone comparison condition.
Methods
Study Design
This was a single-blind (assessors were blinded) randomized controlled clinical trial that compared SBIRT-PM, Pain Module only, and treatment as usual (TAU), with the primary outcomes being change in pain severity and change in weekly risky substance use over 12 weeks postrandomization. Recruitment was conducted at the VA Connecticut Healthcare System’s service connection clinic. Study procedures were approved by the VA Connecticut Healthcare System and Yale University Institutional Review Boards, and participants consented in writing.
Participants
All veterans serving post-9/11 and scheduled for service connection claim examinations related to their back, neck, shoulder, or knee problems were potentially eligible. To omit veterans whose condition was quiescent, enrollment was limited to veterans who self-reported peak joint pain in the last 28 days of at least 2 on a numerical rating scale (NRS) of 0 (no pain) to 10 (worst pain imaginable). We also excluded participants who had attended specialized substance abuse treatment during the three months prior to randomization or who described physiological dependence on alcohol or illicit drugs because people with more severe dependence have not benefited from SBIRT in prior studies [28] and SBIRT is not intended for people already in intensive substance abuse treatment.
Recruitment and Randomization
Potentially eligible veterans were mailed letters alerting them of a forthcoming recruitment phone call and were given the opportunity to opt out of being called. Those who did not opt out were called by a research assistant, informed about the study, and preliminarily screened. All others were invited for in-person enrollment, consent, and completion of baseline assessments.
At the baseline assessment, veterans reporting risky substance use in the 28 days prior to enrollment were assigned to a treatment condition and continued in the study. All others were compensated for the baseline assessment but not further followed. Risky substance use was defined as at least one week with illicit drug use, and/or use of ≥14 drinks in a week or five or more drinks on an occasion by a man, and use of seven or more drinks/week or four or more drinks on an occasion by a woman. Using an urn randomization program, veterans were randomized in a 2:1:1 ratio to either SBIRT-PM, Pain Module–only counseling, or TAU [29]. The urn balanced treatment allocation on factors likely to be related to outcomes: gender [30–32], self-reported illicit drug use within 28 days, and current enrollment in VA psychiatric treatment.
After baseline, veterans were directed to a research coordinator, who notified each veteran of his/her treatment assignment, and for those assigned to an active condition, contact was facilitated with counselors to schedule a face-to-face visit.
Counselors
Three of the study counselors had Master’s degrees (one in social work and two in public health), and the fourth had a doctorate in clinical psychology. One counselor was a VA clinician, and the other three were research clinicians. Counseling was performed in a research setting. Counselors were trained in the both experimental interventions (crossed design) by the Principal Investigator (MIR). Training involved review of therapy manuals, role plays, and review of cases.
Experimental Interventions
Treatment as Usual
Usual practice is that examiners evaluating veterans’ service connection claims are instructed to tell veterans that the examination’s purpose is to evaluate the claim, not to provide treatment. Nevertheless, examiners can, on their own initiative, refer veterans to treatment after the examination.
SBIRT-PM
A manual describing SBIRT-PM is available online at http://www.behaviorchange.yale.edu/interventions/SBIRT-PM%20Therapy%20Manual%20v11.20.14_194012_284_5711.pdf. In brief, a single session intended to last approximately 60 minutes was scheduled. Two brief phone follow-ups were offered, consistent with literature suggesting the benefit of such follow-up [33,34]. Veterans were told the counseling session was to inform them of available services at the VA Connecticut Healthcare System and that the material discussed would not be shared with other providers unless they agreed.
The interview began with inquiries about the veteran’s pain and an explanation of multimodal pain treatment [35,36]. The counselor then explained that substance use sometimes serves as a form of coping with pain [37] that may offer temporary relief but ultimately is associated with worsening underlying pain and injuries. The counselor then transitioned to a traditional, MI-based substance use–focused SBIRT [38]. Substance use was quantified using the three-item version of the Alcohol Use Disorders Identification Test (the AUDIT-C) [39,40], questions from the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) [41,42], and two questions [43,44] concerning misuse of prescribed opioid medications in the preceding 28 days (“How often have you taken your pain medications in larger amounts than prescribed or for a longer period than prescribed?”, “How often have you used your pain medications to get high, to relax, or to make you feel more alert?”). Counselors provided feedback concerning the veteran’s substance use, administered a brief intervention to enhance motivation to reduce use, and made referrals to treatment if the veteran was interested.
After the session, the counselor offered up to two brief “check-in” phone calls (five to 10 minutes) to address any issues that arose in trying to implement plans made during the counseling session, such as issues in accessing VA care.
Pain Module–Only Condition
This involved the portions of SBIRT-PM focused on pain (inquiries about the veteran’s pain and an explanation of multimodal pain treatment) but not the latter portions focusing on substance use.
Assessment/Measures
Randomized veterans completed assessments at baseline and four- and 12-week follow-ups with a research assistant who was blind to counseling condition. Participants were paid $70 for the initial assessment and $50 for each of the two follow-up assessments.
Assessments Collected at Baseline
Participants were characterized based on results of a questionnaire covering demographics, military history, psychiatric history, substance use [45], employment, legal status, and perceived social support [46]. The presence of possible traumatic brain injury was inferred from a four-question screen used by Veterans Health Administration, which is intended to be sensitive but not specific, with a single positive answer interpreted as a positive screen [47]. PTSD severity was assessed using the Traumatic Life Events Questionnaire to determine trauma exposure [48], followed by the Post Traumatic Stress Disorder Checklist–Military Version [49]. The severity of depressive symptoms was assessed with the 21-item Beck Depression Inventory II [50]. Global Information System mapping was used to calculate the distance from each veteran’s home address to the nearest VA hospital (West Haven or Newington).
Questions have been raised about whether people seeking compensation for injuries also want treatment [51,52]. To assess treatment motivation, veterans rated their agreement with items drawn from the Pain Stages of Change Questionnaire [53] on a five-point scale anchored by “strongly disagree” and “strongly agree,” with “unsure” in the middle. Items included “I have been thinking that the way I cope with pain could improve” and “I have been wondering if there is something I could do to manage my pain better.” Motivation for changing substance use was measured with published items [54,55] rated on a 100-point scale of “how big of a problem is substance use for you” and “how interested are you in substance abuse treatment right now.”
Outcome Assessments
Self-reported pain and substance-related service use were collected using a timeline follow-back review of the preceding 60 days, with a further indicator of whether substance use was addressed. Service use was further verified by reviewing the VA electronic health record. Pain treatment was identified by clinic and procedure codes and by text in progress notes, in which pain was addressed at the end of the note in a summary of problems addressed. For analyses, pain and substance use–related service use during the 12 weeks postrandomization were each coded as having occurred (1) or not (0). Electronic medical record (EMR)–documented use of pain-related services was extracted by a blinded reviewer using a predefined algorithm. Clinic appointments and notes recorded during the targeted period were reviewed to determine whether pain was addressed in the summary sections of multipurpose visits (i.e., visits with pain assessed solely as part of history-taking were not classified as addressing pain). For analyses, chart-determined pain-related service use in the 12 weeks postrandomization was coded as occurring (1) or not (0).
Pain was measured using the Brief Pain Inventory (BPI), a validated instrument to assess chronic noncancer pain [56] that assesses pain intensity (four items on a 0–10 scale) and pain interference (seven items on a 0–10 scale) and is scored by taking the average of the scored items in each domain. Clinically significant change in pain intensity is demonstrated by a reduction of at least 15% of the baseline value [57].
Substance use in the preceding 60 days (baseline) and for the period between assessments (weeks 4 and 12) was measured using the timeline follow-back calendar [58], with specification of the number of drinks on drinking days. Urine toxicology tests (ToxCups, Branan Medical Corporation) for cocaine, opioids, cannabis, and amphetamines were conducted at the three data collection visits. Misuse of prescribed opioids was measured using the two screening prescription drug misuse questions described earlier.
Satisfaction with Counseling
Following the counseling session, veterans rated their agreement with three statements on a four-point scale anchored on the extremes by “strongly disagree” and “strongly agree.” The items included the following: “The counseling was helpful,” “I would recommend the counseling to a friend,” “The counselor was too ‘pushy.’” Responses were placed in a sealed envelope and handed to the counselor.
Fidelity to Assigned Counseling
Fidelity to the assigned counseling was assessed by independent ratings of therapy sessions on four constructs: Motivational Interviewing (MI) techniques, Substance Use focus, Pain focus, and Use of Pressure. The MI construct assessed the extent to which the therapist used each of five MI techniques. The substance use counseling construct (three items) assessed the extent to which the therapist screened for substance use, provided feedback about substance use, and referred the veteran to treatment. The pain construct (three items) assessed the extent to which the therapist asked about the veteran’s pain condition and discussed opiate medications and other pain treatments. The Use of Pressure (two items) assessed making value judgements and pressuring the veteran into doing things. The fidelity items’ content was derived from the Yale Adherence and Competence Scale, a reliable and valid system for assessing therapist adherence and competence [59,60]. The extent of each item was rated on a seven-point scale (1 = not at all to 7 = extensively). A total of 15 SBIRT-PM and seven Pain-only recordings (37% of veterans counseled) were randomly selected for rating. Ratings were conducted by a Bachelor’s-level rater blind to study design or conditions. The rater was trained by an expert rater and established interrater reliability by having independent ratings that were within 10% of the sums of each construct rated by the expert. Therapy types were compared on sums of the each of the four constructs.
Data Analysis
To describe differences between veterans with (N = 101) and without (N = 156) recent risky substance use, parametric and nonparametric group comparisons were conducted on demographic variables, military service history, psychiatric symptom severity, pain severity, traumatic brain injury (TBI) having medical insurance, and having baseline service connection.
Within the randomized sample (N = 101), all outcome models adjusted for factors used in the urn randomization process: gender, any illicit drug use within 28 days, and current enrollment in VA psychiatric treatment. Additionally, group differences across the three treatment conditions were assessed using the subset of variables that significantly differentiated veterans with and without recent risky substance use in the full sample at alpha = 0.05 to control for any group difference variables in outcome models. Finally, factors potentially associated with attrition were identified a priori and assessed: baseline use of services, distance from VA, social support, last month income, employment status, baseline pain intensity, and weeks (in the last four) of risky substance use. Except for EMR-documented service use for which full-sample data were available, any factors significantly associated with attrition were included in models to increase the plausibility of a missing at random condition.
The primary pain outcomes were the linear slopes of pain intensity and pain interference on the Brief Pain Inventory over the three measurement occasions (weeks 0, 4, and 12). A secondary pain outcome was the proportion of veterans achieving the published mean clinically important difference (MCID) in pain intensity, a 15% reduction [57]. The primary substance use outcomes were linear slopes of any weekly self-reported risky substance use, as defined previously. Secondary substance use outcomes included any urine toxicology–verified substance use and days of opioid misuse at week 12. Primary service use outcomes were the proportion of participants engaging in any EMR-documented VA pain-related services, the proportion self-reporting use of any VA or non-VA pain-related services, and the proportion self-reporting use of any VA or non-VA substance use–related services during the 12 weeks postrandomization.
Analyses of pain and pain service outcomes compared combined results for the two interventions addressing pain with results for TAU. Analyses for substance use and substance use–related service use compared outcomes for SBIRT-PM with the combined results for the two conditions not directly addressing substance use (i.e., Pain-only counseling and TAU).
The group-by-time effects of counseling (SBIRT-PM or Pain only) on slopes of pain intensity and pain interference were estimated using hierarchical linear regression modeling. The effect of counseling on probability of achieving an MCID in pain intensity was estimating using logistic regression, controlling for baseline differences in pain intensity. The group-by-time effect of SBIRT-PM counseling on weekly risky substance use was estimated using hierarchical logistic regression modeling. Separate logistic regression models assessed the effect of counseling (SBIRT-PM or Pain only) on use of pain and substance use–related services, controlling for baseline differences in the use of those services.
Results
Sampling, Enrollment, and Baseline Characteristics
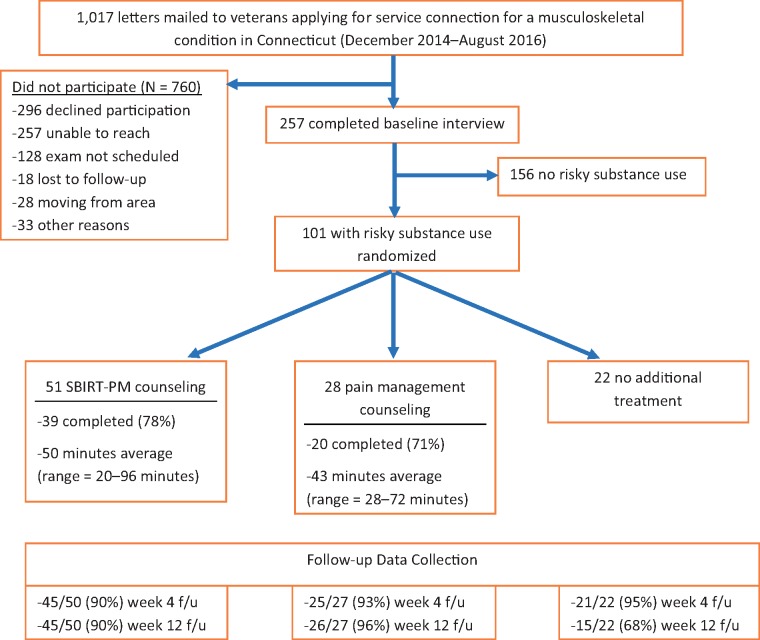
Altogether, 1,017 letters were mailed to veterans applying for service connection for an MSD at VA Connecticut between December 2014 and August 2016 (CONSORT Diagram, Figure 1). In total, 760 did not participate, mostly because they could not be reached or declined to participate (N for both = 553). Another 128 veterans were excluded because their service connection examinations had not been scheduled. An additional 28 veterans were excluded for moving from the area, and 33 for other reasons.
Figure 1.
CONSORT diagram. SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module.
The baseline interview was completed by 257 veterans. Of these, 39.3% (101/257) had had risky substance use in the preceding four weeks and thus qualified for randomization. Table 1 compares the veterans with risky substance use with those without. Those with risky substance use were significantly younger, had completed fewer years of school, had spent fewer years on active duty, and were less likely to be married. They had more psychiatric conditions, as evidenced by a higher likelihood of having been hospitalized for a psychiatric condition, of being prescribed psychiatric medication, and having higher PTSD and depression severity scores. They had lower incomes and were less likely to have private medical insurance. Notwithstanding these differences, veterans with and those without risky substance use had similar mean pain severity ratings on the BPI of approximately 5 out of 10.
Table 1.
Baseline characteristics of veterans without vs with risky substance use
| Not Randomized | Randomized | Randomized |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No Risky Substance Use (N = 156) | With Risky Substance Use (N = 101) | No Treatment (N = 22) | Pain Management (N = 28) | SBIRT-Pain (N = 51) | |||||
| Characteristic | No. (%) | No. (%) | df | Statistic | No. (%) | No. (%) | No. (%) | df | Statistic |
| Age, mean ± SD, y | 37.8 ± 10.7 | 32.3 ± 8.4 | 246 | t = –4.6** | 30.4 ± 6.4 | 32.4 ± 9.3 | 33.0 ± 8.7 |
|
F = 0.77 |
| Male | 137 (88) | 82 (81) | 1 | X2 = 2.1 | 19 (86) | 22 (79) | 41 (80) | 2 | X2 = 0.53 |
| Race/ethnicity | 6 | X2 = 10.98 | |||||||
| White | 91 (58) | 62 (61) | 3 | X2 = 1.3 | 10 (46) | 14 (50) | 38 (75) | ||
| African American | 22 (14) | 16 (16) | 4 (18) | 7 (25) | 5 (9) | ||||
| Hispanic | 32 (20) | 19 (19) | 6 (27) | 5 (18) | 8 (16) | ||||
| Other | 11 (7) | 4 (4) | 2 (9) | 2 (7) | 0 (0) | ||||
| Marital status | 4 | X2 = 3.77 | |||||||
| Married | 99 (63) | 44 (44) | 2 | X2 = 9.6** | 6 (27) | 13 (46) | 25 (50) | ||
| Single (past married) | 24 (15) | 21 (21) | 7 (32) | 5 (18) | 9 (18) | ||||
| Single (no marriages) | 33 (21) | 35 (35) | 9 (41) | 10 (36) | 16 (32) | ||||
| Education, median (IQR) | 14.5 (13.0–16.0) | 14.0 (12.5–16.0) | MWU = 6,364** | 14.5 (12.0–16.0) | 14.0 (12.3–15.0) | 14.0 (13.0–16.0) | 2 | X2 = 0.31 | |
| Years active duty, median (IQR) | 7.00 (4.00–15.31) | 4.50 (3.25–8.00) | MWU = 5,959** | 4.0 (1.9–6.3) | 5.3 (3.7–10.0) | 5.0 (3.5–8.5) | 2 | X2 = 2.68 | |
| Deployed to war zone | 109 (70) | 68 (67) | 1 | X2 = 0.19 | 14 (64) | 20 (71) | 34 (67) | 2 | X2 = 0.36 |
| Employment | 4 | X2 = 4.66 | |||||||
| Employed | 81 (52) | 49 (49) | 2 | X2 = 4.5 | 14 (64) | 11 (39) | 24 (48) | ||
| Military service | 39 (25) | 17 (17) | 1 (5) | 7 (25) | 9 (18) | ||||
| Unemployed | 36 (23) | 34 (34) | 7 (32) | 10 (36) | 17 (34) | ||||
| Last month income, median (IQR) | $4,703 ($2,500–$7,383) | $2,562 ($1,519–$4,475) | MWU = 5,289** |
|
|
|
2 | X2 = 1.26 | |
| Distance from VA, median (IQR) | 24.3 (14.7–45.3) | 16.6 (9.5–35.1) | MWU = 6,031** |
|
|
|
2 | X2 = 1.82 | |
| Social supports (0–30), mean ± SD | 10.1 ± 5.1 | 9.6 ± 4.7 | 225 | t = –0.82 | 7.9 ± 5.0 | 9.7 ± 4.4 | 10.3 ± 4.6 |
|
F = 2.09 |
| Health insurance | n = 154 | n = 95 | X2 = 10.70** | N = 22 | N = 25 | N = 48 | |||
| Private | 99 (64) | 43 (45) | 2 | 9 (41) | 11 (44) | 23 (48) | 4 | X2 = 2.12 | |
| VA w/o private | 46 (30) | 48 (51) | 13 (59) | 13 (52) | 22 (46) | ||||
| Public w/o other | 9 (6) | 4 (4) | 0 (0) | 1 (4) | 3 (6) | ||||
| Ever hospitalized psych | 10 (6) | 16 (16) | 1 | X2 = 6.10* | 6 (27) | 4 (14) | 6 (12) | 2 | X2 = 2.74 |
| Positive TBI screen | 58 (37) | 39 (39) | 1 | X2 = 0.05 | 9 (41) | 11 (39) | 19 (37) | 2 | X2 = 0.09 |
| On med for psych | 29 (19) | 36 (36) | 1 | X2 = 9.75** | 8 (36) | 9 (32) | 19 (38) | 2 | X2 = 0.27 |
| PCL-M, mean ± SD | (N = 154) 18.4±17.1 | (N = 100) 27.0 ± 17.8 | 252 | t = 3.86** | 29.86 ± 20.71 | 26.04 ± 16.23 | (N = 50) 26.22 ± 17.40 | 2, 97 | F = 0.37 |
| BDI, mean ± SD | (N = 154) 13.1 ± 11.6 | (N = 100) 17.0 ± 11.4 | 252 | t = 2.70** |
|
16.2 ± 11.1 | 16.8 ± 8.6 |
|
F = 0.34 |
| Service connected | 83 (53) | 58 (58%) | 1 | X2 = 0.57 | 12 (54) | 15 (54) | 31 (62) | 2 | X2 = 0.66 |
| BPI pain intensity, mean ± SD | 4.5 ± 1.8 | 4.8 ± 1.7 | 255 | t = 1.05 | 4.7 ± 1.7 | 4.7 ± 1.7 | 4.8 ± 1.8 |
|
F = 0.05 |
| BPI interference, mean ± SD | 5.0 ± 2.3 | 5.3 ± 2.2 | 255 | t = 1.28 | 4.8 ± 2.5 | 5.3 ± 2.2 | 5.5 ± 2.1 |
|
F = 0.81 |
BDI = Beck Depression Inventory; BPI = Brief Pain Inventory; IQR = interquartile range; PCL-M = Post Traumatic Stress Disorder Checklist–Military Version; SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module; TBI = Traumatic Brain Injury; VA = Department of Veterans Affairs.
* P < 0.05; ** P < .01.
Randomized Sample
The 101 randomized post-9/11 veterans presented with back (N = 67), neck (N = 19), knee (N = 57) and shoulder (N = 31) claims (Table 1). A little over half (N = 54) of participants were applying for more than one condition. Participants’ average age was 32.3 ± 8.4 years, and 81% were male. Altogether, 61% self-identified as Caucasian, 16% as African American, and 19% as Hispanic. They had served in the military an average of 6.7 years, and 67% had been deployed to a war zone. Veterans characterized their past-year employment patterns as employed (49%), military service (17%), and unemployed (34%). Only 43% had private health insurance. Their mean baseline pain intensity on the Brief Pain Inventory was 4.8 ± 1.7, and their mean baseline pain interference on the Brief Pain Inventory was 5.3 ± 2.2.
Overall, most randomized veterans were motivated to change their pain management, but few were motivated to change their substance use. Of the 101 participants, 71% agreed that the way they coped with pain could improve and 70% agreed with the statement that they had been wondering if they could do something to manage their pain better. However, most substance use attitudes indicated low motivation to change this behavior; 76% rated substance use at or below 20 on the 0–100 scale of problem severity, and 90% rated their interest in treatment at 20 or less on the same scale.
Randomization and Follow-up
The 101 participants were assigned by urn randomization 2:1:1 to SBIRT-PM (N = 51), Pain Module only (N = 28), or TAU (N = 22) (CONSORT Diagram, Figure 1). Treatment group comparisons revealed no significant baseline differences on any of the tested variables (Table 1).
Follow-up rates were high; 91/101 (90%) completed the week 4 follow-up, and 86/101 (85%) completed week 12. Participants in the TAU group were significantly more likely than SBIRT-PM or Pain Counseling participants to have withdrawn from the study at week 12 (32% vs 12% and 11%, respectively; P < 0.05). Attrition was associated with significantly lower pain intensity at baseline (5.00 ±1.61 vs 5.50 ±2.20, t (99) = 3.04, P < 0.01). Thus, to reduce the risk of bias associated with nonrandom attrition, differences in baseline pain intensity were controlled for in all outcome models, except for models using chart-documented, full-sample data and the model of pain intensity itself, which already included baseline pain intensity in the model of change.
To determine if the blind was maintained, research assistants were asked what condition each veteran was assigned to, and their guesses as to TAU or an active condition were almost exactly at chance (52% correct).
Counseling Participation and Processes
Of the 79 veterans assigned to counseling, 59 attended it, with the SBIRT-PM session lasting on average 50 minutes and the Pain Module–only session lasting on average 43 minutes. Counseling sessions occurred an average (SD) of 11 (7.6) days after baseline appointments. Ratings of satisfaction with both counseling sessions were high. Most (83% in SBIRT-PM and 68% in Pain Module only) rated strong agreement that meeting with the study counselor was helpful. The clear majority (91% in SBIRT-PM and 74% in Pain Module only) strongly agreed that they would recommend the counseling to other people they know. Only one participant in each group agreed with a statement that the counselor was “pushy.”
Fidelity to SBIRT-PM in Rated Audiotapes of Counseling
Compared with Pain Module–only sessions, the SBIRT-PM therapy sessions were rated significantly higher on the substance use construct (mean rank = 15.0 vs 4.1, MWU = 0.5, P < 0.000), as expected. They were also rated higher on MI (mean rank = 14.4 vs 5.36, MWU = 9.5, P = 0.001), reflecting that counseling concerning pain required little motivational enhancement for these already motivated patients, but substance use counseling involved more use of MI. As expected, SBIRT-PM and Pain Module–only sessions were rated similarly on the pain construct (P = 0.407) and in the therapists’ Use of Pressure (P = 1.0, all were rated at “not at all”).
Service Use Outcomes
As shown in Table 2, counseling (SBIRT-PM or Pain Management only) had a significant positive effect on EMR-documented use of VA pain-related care by week 12. Veterans assigned to counseling were over three times as likely to have used VA pain-related services postbaseline. This reflects both new engagement in treatment among veterans with no pain-related service use in the past 12 weeks at baseline and more sustained engagement for veterans already using services.
Table 2.
Service use by group before and after randomization, controlling for covariates
| Service Used and How Measured | Group | % Used at Baseline | % Used Weeks 0–12 | Treatment OR (95% CI) | P Value |
|---|---|---|---|---|---|
| Pain treatment/self-report | TAU | 62 (N = 21) | 38 | 3.37 (1.15–9.88) | 0.027 |
| Experimental | 60 (N = 72) | 64 | |||
| VA pain treatment/EMR | TAU | 46 | 27 | 3.42 (1.08–10.79) | 0.036 |
| Experimental | 48 | 51 | |||
| Substance use treatment/self-report | TAU and Pain Module Only | 36 | 45 | 0.83 (0.33–2.08) | 0.70 |
| SBIRT-PM | 41 | 41 |
CI = confidence interval; EMR = electronic medical record; OR = odds ratio; SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module; TAU = treatment as usual.
Baseline self-reported service use was elicited for the preceding 60 days on a timeline follow-back calendar. Chart data were extracted by a staff member blind to counseling condition. Self-report analyses were restricted to patients with data at baseline and at week 12.
Within the subgroup of 53 veterans who had not had any EMR-documented pain-related service use in the 12 weeks before baseline, veterans in the counseling groups were almost eight times as likely to have initiated pain-related service use in the 12 weeks after baseline (39% vs 8%, P = 0.05, conditional odds ratio [OR] = 7.76). The effect of counseling was similar for self-reported service use, which included both VA and non-VA pain-related care. Using complete cases and controlling for baseline pain intensity (the variable associated with attrition) and other planned covariates, veterans in counseling were over three times as likely to have used pain-related services in the 12 weeks postrandomization (P = 0.027).
The services newly used by veterans in the treatment groups were primary care consultation for pain (used by 11 veterans), physical therapy (by three), and an urgent care setting (by three). Other modalities that were used infrequently (by two or fewer veterans) included therapeutic exercise, electric stimulation therapy, pain-focused cognitive behavior therapy, rheumatology, mental health, chiropractic, and podiatry.
Controlling for planned covariates, SBIRT-PM was not associated with use of substance use treatment at the 12-week follow-up.
Seven veterans were prescribed opioids at baseline, and five still reported receiving opioid therapy at week 12. Three new veterans had prescriptions for opioids at week 12. The likelihood of being prescribed opioids was unrelated to treatment condition.
Pain Outcomes
As shown in Table 3, the slopes of the Brief Pain Inventory pain severity and pain interference subscales were not significantly different from zero, and slopes were not moderated by counseling. In a secondary analysis comparing the two interventions separately with TAU, neither type of counseling was associated with a significant difference in slope compared with TAU.
Table 3.
Pain outcomes over time by group
| Baseline |
Week 4 |
Week 12 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pain outcomes† | M | SD | M | SD | M | SD | Group × Time‡ | 95% CI | P Value | Effect Size§ |
| BPI intensity | ||||||||||
| TAU | 4.72 | 1.74 | 4.90 | 1.82 | 4.40 | 2.07 | 0.004 | 0.06–0.07 | 0.91 | 0.27 |
| Pain module | 4.74 | 1.70 | 4.54 | 1.37 | 4.20 | 1.71 | ||||
| SBIRT-PM | 4.84 | 1.81 | 4.59 | 1.75 | 4.59 | 1.72 | ||||
| BPI interference | ||||||||||
| TAU | 4.82 | 2.50 | 4.57 | 2.47 | 4.15 | 2.37 | –0.015 | 0.09–0.06 | 0.70 | –0.17 |
| Pain module | 5.30 | 2.21 | 4.73 | 2.58 | 4.04 | 2.49 | ||||
| SBIRT-PM | 5.55 | 2.16 | 5.02 | 2.33 | 4.89 | 2.24 | ||||
BPI=Brief Pain Inventory; SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module; TAU=treatment as usual.
Controlling for covariates associated with randomization to treatment.
Compared TAU vs other two groups combined. Negative coefficients reflect more negative linear slopes for combined pain counseling groups. Differences are not statistically significant.
Mean difference in group slope estimates/SD of unconditional slope.
In a secondary logistic regression analysis, we considered the proportion of veterans achieving the published MCID in pain intensity, a 15% reduction [57]. Controlling for baseline pain intensity, the proportion of veterans in the counseling groups achieving MCID at week 12 did not differ significantly (OR = 1.29, 95% CI = 0.40–4.17) from the proportion of TAU participants (39% vs 33%, respectively).
Substance Use Outcomes
Among the 101 randomized veterans, self-reported risky substance use in the 28 days before baseline was primarily of alcohol (N = 77) and cannabis (N = 28), with substantially smaller numbers of veterans using nonprescribed opioids (N = 4) and other drugs (N = 5).
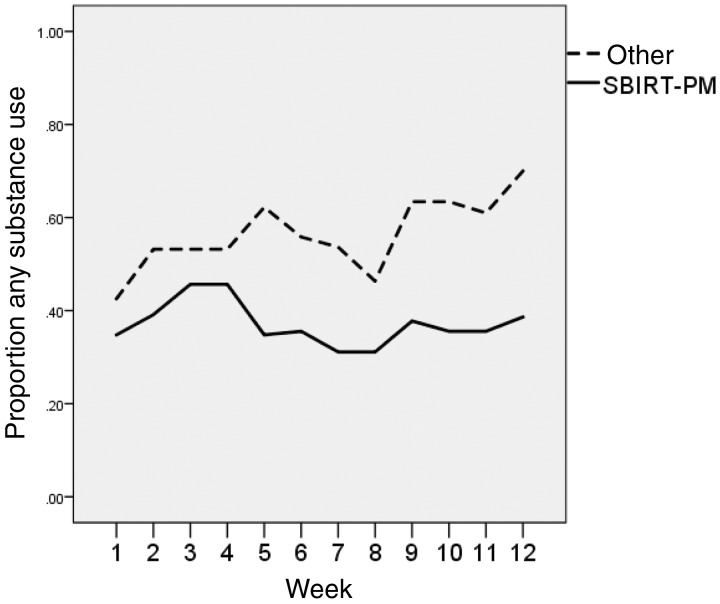
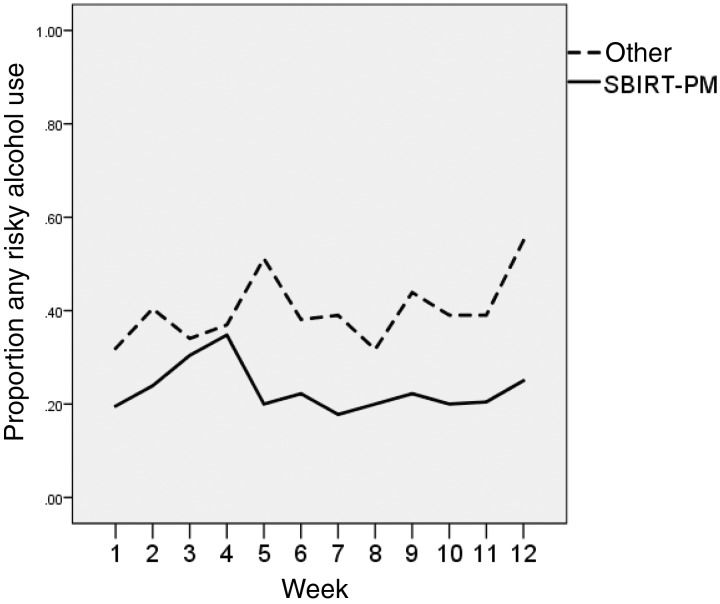
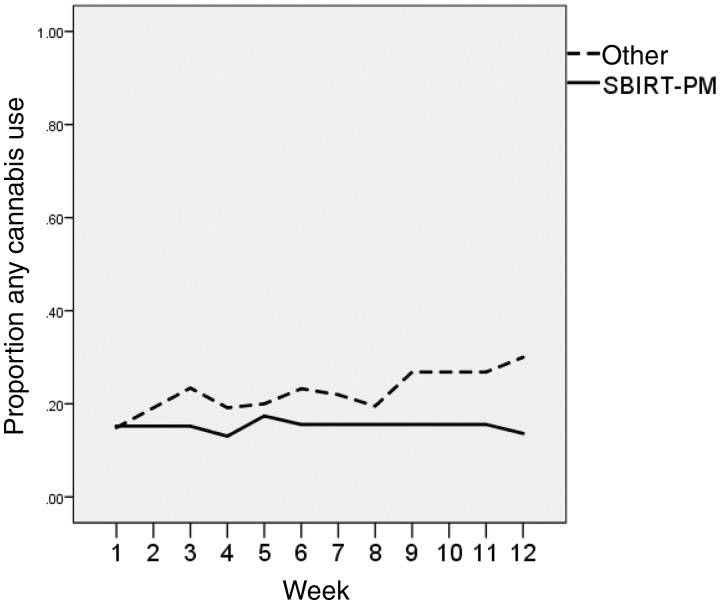
Postbaseline, the weekly probability of any risky substance use increased significantly over time for participants in the non-SBIRT-PM conditions, controlling for planned covariates (Figure 2). The time-by-SBIRT-PM interaction effect was significant and negative; participants in SBIRT-PM were significantly less likely to use substances over time (β = –0.13, P = 0.015, d = –0.84). Looking separately at individual substances, the SBIRT-PM-by-time effect was significant and negative for risky alcohol use (β = –0.11, P = 0.04, d = –0.96) and was negative but not statistically significant for less common cannabis use (β = –0.12, P = 0.269, d = –0.90) (Figures 3 and 4).
Figure 2.
Risky substance use by condition. SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module.
Figure 3.
Risky alcohol use by condition. SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module.
Figure 4.
Cannabis use by condition. SBIRT-Pain = Screening Brief Intervention and Referral to Treatment–Pain Module.
Because so much risky substance use was alcohol (which was not laboratory tested), cannabis (which remains in the urine for several weeks after last use), and opioids that had been prescribed, urine toxicology testing did not add much to the self-reported data. There was little change in the proportion positive for THC from baseline to week 12 in the non-SBIRT condition (from 10/45 to 10/40 were positive), and the proportion slightly decreased in the SBIRT-PM condition (from 6/46 to 4/41). In a logistic regression model of week 12 toxicology values (positive screen or not), controlling for planned covariates and baseline THC toxicology values, SBIRT-PM was not a statistically significant predictor.
Thirteen veterans reported having misused prescription opioids in the past 28 days on one of the two items, with 11 having used more than prescribed and two having used them for reasons not prescribed. The proportion of veterans reporting misuse of prescribed opioids in the SBIRT-PM group decreased from 0.14 (N = 51) at baseline to 0.07 (N = 45) at week 12, but in the other groups it slightly increased from 0.12 (N = 50) to 0.17 (N = 41).
Conclusions
The main findings were the feasibility and acceptability of early intervention among veterans applying for service connection for MSD and preliminary evidence of SBIRT-PM’s efficacy for engaging them in pain treatment and reducing risky substance use.
The remarkably large number of veterans applying for service connection allowed for a substantial number to receive SBIRT-PM, even if only a relatively small proportion of those evaluated for MSD (257/1017) were enrolled in the study. The enrolled veterans presented with substantial symptomatology. For example, our studies’ participating veterans’ overall pain severity (mean pain over the past week of 5.1) was higher than average NRS ratings from the MSD Cohort Study veterans, whose mean pain NRS scores were 3.4 in 2011 [61]. We are only aware of one other published study describing veterans seeking service connection for MSD, which also found high rates of pain-related impairment, substance use, and psychiatric comorbidity [62].
Among those enrolled who were offered an active intervention, 74.7% (59/79) received counseling, and ratings of satisfaction with the counseling were quite high. The feasibility and acceptability of this approach to veterans is further buttressed by the efficacy data, suggesting that veterans followed counselors’ suggestions that they attend pain treatment and reduce their substance use. The feasibility for the VA might be increased by having more of SBIRT-PM conducted by phone, as has been done effectively for other SBIRT interventions. Requiring a face-to-face visit for SBIRT-PM was largely accomplished by accommodating veterans’ schedules for when they would be at the VA for service connection exams or other reasons.
The feasibility of SBIRT-PM in this clinical trial might differ (in either direction) from that in nonresearch settings. Although veterans were not paid for attending SBIRT-PM, they were paid for their data collection visits, and it is possible that these payments predisposed them to attend the unpaid counseling visits as well. Another circumstance that may not apply outside experimental settings is that the study counseling was described in a general way in the study consent form and, because it was an experimental part of a research study, was not entered into the medical record. Participants gave specific permission for treatment referrals to be made on their behalf only after attending the experimental counseling. Veterans may be more reluctant to attend counseling if it is described as substance use focused, with the expectation that participation will be recorded in veterans’ electronic health records. On the other hand, attendance at counseling may have been negatively impacted by logistic factors in this study, and likely would have been better if it had been possible to more closely coordinate counseling with the service connection examination (e.g., on the same day). That was not possible because of the multiple steps involved in calling veterans to enroll them, consent them, complete assessments, and only then, after randomization, to schedule counseling.
SBIRT-PM was associated with more engagement in pain treatment. Most veterans indicated that they had been thinking of ways to better manage their pain, and more veterans in the intervention groups attended pain treatments than in the control group. The finding of more pain treatment involvement after counseling is consistent with veterans’ self-reported willingness to find new ways to cope with their painful conditions. Our group found in another study of veterans applying for service connection that counseling encouraging use of VA services was associated with increased use of those services [12].
It is noteworthy that use of VA services decreased in the treatment as usual condition after the compensation examination. Although there are no published data on the relationship between MSD service connection claims and use of pain services, there have been frequent assertions [63] and rebuttals [64,65] that veterans applying for service connection for PTSD are more likely to attend PTSD treatment prior to evaluation of a claim and to discontinue the treatment afterwards. It is also consistent with other data from our group suggesting that veterans believe that attending pain treatment facilitates having a claim approved (Black, Perez-Ortiz, and Rosen, unpublished data).
There were no significant differences in pain intensity or pain interference ratings between conditions. The lack of effect of SBIRT-PM on pain itself might reflect that engagement in new pain treatments was insufficient, or that those treatments had limited efficacy. The lack of effect may also reflect the sample’s heterogeneity regarding baseline pain intensity, although post hoc analyses testing moderation of the treatment effect by baseline pain intensity showed no evidence of an interaction. Efficacy might have been greater with longer follow-up. There was some delay between when veterans were seen for experimental counseling and when they obtained available treatments because obtaining those treatments required a consult to be placed (at the VA), appointments to be made, and treatment to begin. Thus, 12 weeks may not have been enough time to detect an effect of the newly embarked-upon treatments.
The efficacy of SBIRT-PM in reducing risky substance use in this study was larger than that seen in most other brief intervention studies [66–68]. To avoid falsely rejecting the null hypothesis in this pilot study, we excluded veterans with more severe substance use (need for detoxification or already in specialized substance use treatment) from study participation. This procedure left a treatment-responsive group, with many veterans being open enough to reducing their substance use to be impacted by brief counseling, and not having such severe use that SBIRT-PM was insufficient. Most of the veterans who reported risky substance use, and thus went on to randomization, reported risky use of alcohol, the substance for which SBIRT’s efficacy has been most consistently described. The mechanism by which veterans reduced their substance use was not determined; there were no differences between the groups in engagement in formal addiction treatment, and it is possible that veterans simply followed counselors’ suggestions to reduce alcohol use so that it was no longer risky use.
An important caveat is that the main substance use outcome data were self-reported and might reflect a social desirability bias in that veterans counseled to reduce their substance use in SBIRT-PM might have been inclined to underreport their use. Otherwise, the effects were robust. The reduction in risky substance use with SBIRT-PM was more robust if missing data were imputed to be risky use, because this imputed relatively more risky weeks to the usual care group, from whom there were the largest proportion of missing data. Such imputation, treating missing weeks as reflecting substance use, has been proposed for sensitivity analyses of substance use in clinical trials when there was, as in this case, differential completion of study assessments [69].
Overall, the findings suggest great promise for enlisting veterans applying for service connection in treatment. Should the results be replicated and extended, SBIRT-PM has the potential to benefit a population at high risk for worsening pain and substance use. In the 2015 fiscal year, 97,223 veterans under the age of 35 were newly awarded compensation [10], many for MSD, and SBIRT-PM offers an opportunity for early intervention for these vulnerable veterans. Although we tested an MI approach, the findings of an at-risk, treatment-receptive cohort suggest the promise of offering other modalities (e.g., web-based treatments) around the time of the service compensation examination and turning what is often an adversarial encounter into a treatment-promoting one.
Acknowledgments
We thank the following colleagues who contributed to the study: Christina Lazar, Heather Fries, and Thomas Thornhill, who recruited participants and conducted assessments; Deepa Mavani, Karen Ablondi, Anna Sullivan, and Robert MacLean, who delivered the study therapies; Helene White, who assisted with study design; and Jacqueline Cook, who facilitated access to the compensation clinic from which participants were recruited.
Funding sources: Supported by the National Institutes of Health R34AT008318 (MIR) and the VISN 1 Mental Illness Research Education and Clinical Center (MIRECC). The funders had no role in the study design or in any aspect of data collection, data analysis, or article writing.
Disclosure and conflicts of interest: No conflicts of interest to report.
Trial registration: This study was registered on ClinicalTrials.gov (NCT 02049086).
References
- 1. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevalence, correlates, and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorder. Pain 2011;1523:488–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dersh J, Gatchel RJ, Polatin P, Mayer T.. Prevalence of psychiatric disorders in patients with chronic work-related musculoskeletal pain disability. J Occup Environ Med 2002;445:459.. [DOI] [PubMed] [Google Scholar]
- 3. Institute of Medicine, Committee on Advancing Pain Research Care and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 4. Zvolensky MJ, McMillan K, Gonzalez A, Asmundson GJ.. Chronic pain and cigarette smoking and nicotine dependence among a representative sample of adults. Nicotine Tob Res 2009;1112:1407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seal K, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA 2012;3079:940–7. [DOI] [PubMed] [Google Scholar]
- 6. Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA 2008;3006:663–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine Committee on Prevention, Diagnosis, Treatment, and Management. Substance Use Disorders in the U.S. Armed Forces. Washington, DC: The National Academic Press; 2012.
- 8. Milliken CS, Auchterlonie JL, Hoge CW.. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq War. JAMA 2007;29818:2141–8. [DOI] [PubMed] [Google Scholar]
- 9. Morasco BJ, Corson K, Turk DC, Dobscha SK.. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain 2011;123:352–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Veterans Benefits Administration. Annual Benefits Report Fiscal Year 2015. Veterans Benefits Administration; Washington, DC: 2016.
- 11. Rosen M. Compensation examinations for PTSD—an opportunity for treatment? J Rehabil Res Dev 2010;475:xv–xxii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rosen MI, Ablondi K, Black AC, et al. Work outcomes after benefits counseling among veterans applying for service connection for a psychiatric condition. Psychiatr Serv 2014;6512:1426–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Friedrich M, Gittler G, Halberstadt Y, Cermak T, Heiller I.. Combined exercise and motivation program: Effect on the compliance and level of disability of patients with chronic low back pain: A randomized controlled trial. Arch Phys Med Rehabil 1998;795:475–87. [DOI] [PubMed] [Google Scholar]
- 14. Habib S, Morrissey S, Helmes E.. Preparing for pain management: A pilot study to enhance engagement. J Pain 2005;61:48–54. [DOI] [PubMed] [Google Scholar]
- 15. Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns 2013;932:157–68. [DOI] [PubMed] [Google Scholar]
- 16. Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL.. A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Res Soc Work Pract 2010;202:137–60. [Google Scholar]
- 17. VanBuskirk KA, Wetherell JL.. Motivational interviewing with primary care populations: A systematic review and meta-analysis. J Behav Med 2014;374:768–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Babor TF, Biddle-Higgins TC. Brief Intervention For Hazardous and Harmful Drinking: A Manual for Use in Primary Care. World Health Organization, Department of Mental Health and Substance Abuse; 2001. Available at: http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6b.pdf (Accessed April 26, 2018).
- 19. Babor TF, McRee BG, Kassebaum PA, et al. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Toward a public health approach to the management of substance abuse. Subst Abuse 2007;283:7–30. [DOI] [PubMed] [Google Scholar]
- 20. Bertholet N, Daeppen J-B, Wietlisbach V, Fleming M, Burnand B.. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Arch Intern Med 2005;1659:986–95. [DOI] [PubMed] [Google Scholar]
- 21. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J.. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2004;1407:557–68. [DOI] [PubMed] [Google Scholar]
- 22. Stead LF, Bergson G, Lancaster T.. Physician advice for smoking cessation. Cochrane Database Syst Rev 2008;162:CD000165. [DOI] [PubMed] [Google Scholar]
- 23. Hettema JE, Hendricks PS.. Motivational interviewing for smoking cessation: A meta-analytic review. J Consult Clin Psychol 2010;786:868–84. [DOI] [PubMed] [Google Scholar]
- 24. Lai DT, Cahill K, Qin Y, Tang JL.. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev 2010;201:CD006936. [DOI] [PubMed] [Google Scholar]
- 25. Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA 2014;3125:492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: The ASPIRE randomized clinical trial. JAMA 2014;3125:502–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moyer A, Finney JW, Swearingen CE, Vergun P.. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 2002;973:279–92. [DOI] [PubMed] [Google Scholar]
- 28. Saitz R. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev 2010;296:631–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stout RL, Wirtz PW, Carbonari JP, Del Boca FK.. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl 1994;12:70–5. [DOI] [PubMed] [Google Scholar]
- 30. Arfken CL, Borisova N, Klein C, et al. Women are less likely to be admitted to substance abuse treatment within 30 days of assessment. J Psychoactive Drugs 2002;341:33–8. [DOI] [PubMed] [Google Scholar]
- 31. Kimerling R, Gima K, Smith MW, et al. The Veterans Health Administration and military sexual trauma. Am J Public Health 2007;9712:2160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Haskell SG, Ning Y, Krebs E, et al. Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom. Clin J Pain 2012;282:163–7. [DOI] [PubMed] [Google Scholar]
- 33. Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol 2001;626:806–16. [DOI] [PubMed] [Google Scholar]
- 34. Brown RL, Saunders LA, Bobula JA, Mundt MP, Koch PE.. Randomized-controlled trial of a telephone and mail intervention for alcohol use disorders: Three-month drinking outcomes. Alcohol Clin Exp Res 2007;318:1372–9. [DOI] [PubMed] [Google Scholar]
- 35. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;1477:478–91. [DOI] [PubMed] [Google Scholar]
- 36. Dorflinger L, Kerns R, Auerbach S.. Providers’ roles in enhancing patients’ adherence to pain self management. Transl Behav Med 2013;31:39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McCarthy E, Richardson G, Ralevski E, et al. Pilot Study: The Use of a Modified Version of Cogntive Processing Therapy-Cognitive for the Treatment of Veterans Diagnosed with PTSD and Alcohol Dependence. San Francisco, CA: American Psychological Association; 2009. [Google Scholar]
- 38. Miller WR, Zweben A, DiClemente CC, Rychtarik RC.. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. U.S. Department of Health and Human Services; Rockville, Maryland; 1992. [Google Scholar]
- 39. Kriston L, Holzel L, Weiser AK, et al. Meta-analysis: Are 3 questions enough to detect unhealthy alcohol use? Ann Intern Med 2008;14912:879–88. [DOI] [PubMed] [Google Scholar]
- 40. Reinert DF, Allen JP, Reinert DF, Allen JP.. The alcohol use disorders identification test: An update of research findings. Alcohol Clin Exp Res 2007;312:185–99. [DOI] [PubMed] [Google Scholar]
- 41. WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction 2002;979:1183–94. [DOI] [PubMed] [Google Scholar]
- 42. Humeniuk R, Ali R, Babor TF, et al. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST). Addiction 2008;1036:1039–47. [DOI] [PubMed] [Google Scholar]
- 43. Potter J, Prather K, Kropp F, et al. A method to diagnose opioid dependence resulting from heroin versus prescription opioids using the Composite International Diagnostic Interview. Contemp Clin Trials 2010;312:185–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. World Health Organization. Composite International Diagnostic Interview (CIDI) Core Version 2.1. World Health Organization; 1997. Available at: https://pubs.niaaa.nih.gov/publications/assessingalcohol/InstrumentPDFs/20_CIDI.pdf (Accessed April 26, 2018).
- 45. McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat 1992;93:199–213. [DOI] [PubMed] [Google Scholar]
- 46. Lam JA, Rosenheck R.. Street outreach for homeless persons with serious mental illness—is it effective? Med Care 1999;379:894–907. [DOI] [PubMed] [Google Scholar]
- 47. Government Accountability Office. Mild Traumatic Brain Injury Screening and Evaluation Implemented for OEF/OIF Veterans, but Challenges Remain. Washington, DC: United States Government Accountability Office; 2008. [Google Scholar]
- 48. Kubany ES, Haynes SN, Leisen MB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychol Assess 2000;122:210–24. [DOI] [PubMed] [Google Scholar]
- 49. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA.. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996;348:669–73. [DOI] [PubMed] [Google Scholar]
- 50. Homaifar BY, Brenner LA, Gutierrez PM, et al. Sensitivity and specificity of the Beck Depression Inventory-II in persons with traumatic brain injury. Arch Phys Med Rehabil 2009;904:652–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. US Government Accountability Office. Review of State Variances in VA Disability Compensation Benefits. Contract No.: #05-00765-137. Washington, DC: Department of Veterans Affairs Office of Inspector General; 2005. [Google Scholar]
- 52. Harrington JT. Musculoskeletal pain and work disability. Wis Med J 1992;9110:579–80. [PubMed] [Google Scholar]
- 53. Kerns RD, Rosenberg R, Jamison RN, Caudill MA, Haythornthwaite J.. Readiness to adopt a self-management approach to chronic pain: The Pain Stages of Change Questionnaire (PSOCQ). Pain 1997;721:227–34. [DOI] [PubMed] [Google Scholar]
- 54. Ondersma SJ, Svikis DS, Schuster CR, et al. Computer-based brief intervention a randomized trial with postpartum women. Am J Prev Med 2007;323:231–8. Erratum in Am J Prev Med 2007;32(6):549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. LaBrie JW, Quinlan T, Schiffman JE, et al. Performance of alcohol and safer sex change rulers compared with readiness to change questionnaires. Psychol Addict Behav 2005;191:112–5. [DOI] [PubMed] [Google Scholar]
- 56. Tan G, Jensen MP, Thornby JI, Shanti BF.. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 2004;52:133–7. [DOI] [PubMed] [Google Scholar]
- 57. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 2008;92:105–21. [DOI] [PubMed] [Google Scholar]
- 58. Weiss RD, Najavits LM, Greenfield SF, et al. Validity of substance use self-reports in dually diagnosed outpatients. Am J Psychiatry 1998;1551:127–8. [DOI] [PubMed] [Google Scholar]
- 59. Carroll KM, Nich C, Sifry RL, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend 2000;573:225–38. [DOI] [PubMed] [Google Scholar]
- 60. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;1131:9–19. [DOI] [PubMed] [Google Scholar]
- 61. Goulet JL, Kerns RD, Bair M, et al. The musculoskeletal diagnosis cohort: Examining pain and pain care among veterans. Pain 2016;1578:1696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sakr C, Black A, Slade M, Calfo J, Rosen M.. Iraq/Afghanistan-era veterans with back pain: Characteristics and predictors of compensation and pension award. J Rehabil Res Dev 2016;536:659–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Frueh BC, Grubaugh AL, Elhai JD, Buckley TC.. US Department of Veterans Affairs disability policies for posttraumatic stress disorder: Administrative trends and implications for treatment, rehabilitation, and research. Am J Public Health 2007;9712:2143–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Sayer NA, Clothier B, Spoont M, Nelson DB.. Use of mental health treatment among veterans filing claims for posttraumatic stress disorder. J Trauma Stress 2007;201:15–25. [DOI] [PubMed] [Google Scholar]
- 65. Marx BP, Miller MW, Sloan DM, et al. Military-related PTSD, current disability policies, and malingering. Am J Public Health 2008;985:773–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hingson R, Compton WM.. Screening and brief intervention and referral to treatment for drug use in primary care: Back to the drawing board. JAMA 2014;3125:488–9. [DOI] [PubMed] [Google Scholar]
- 67. Jonas DE, Garbutt JC, Amick HR, et al. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2012;1579:645–54. [DOI] [PubMed] [Google Scholar]
- 68. Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;182:CD004148. [DOI] [PubMed] [Google Scholar]
- 69. Delucchi KL. Methods for the analysis of binary outcome results in the presence of missing data. J Consult Clin Psychol 1994;623:569–75. [PubMed] [Google Scholar]