Abstract
Objective
Multiple and specific types of childhood adverse events are risk factors for chronic pain conditions. Although both can covary, no study has evaluated one aspect while controlling for the other. Therefore, the current study examined whether more adverse events would be a risk factor for common chronic pain conditions and pain medication use in young adults after controlling for different adversity types such as physical, emotional, and sexual traumatic events or vice versa.
Methods
This cross-sectional study recruited 3,073 undergraduates (72% female, mean age = 18.8 years, SD = 1.4 years) who completed the survey for current health status and early life traumatic events.
Results
More adverse events were associated with a 1.2–1.3-fold increase in the odds of any chronic pain, chronic back pain, headache, and dysmenorrhea with adjusting for adversity types, but they were not associated with the risk of comorbid pain conditions and use of pain medications. In contrast, specific adversity types were unrelated to chronic pain conditions when controlling for the number of adverse events.
Conclusions
Cumulative childhood adverse events may be a more relevant risk factor for chronic pain conditions than the experience of a specific type of adverse event. Clinicians and researchers need to evaluate cumulative childhood adversity when assessing its link to chronic pain.
Keywords: Childhood Adversity, Low Back Pain, Headache, Dysmenorrhea, Odd Ratio
Different aspects of childhood adversity have been identified as risk factors for chronic pain conditions. One aspect is the type or nature of the trauma. For example, studies have found that childhood physical, sexual, or emotional abuse is associated with an increased risk for fibromyalgia [1,2], chronic pelvic pain [3], migraine [4], and neck/back pain [5,6]. A birth cohort study has also shown that other general stressful life events (e.g., maternal separation, household dysfunction, financial difficulties) by age seven increased the risk of chronic widespread pain by 1.5–2.0-fold in middle-aged adults [7].
Another line of study has found that cumulative childhood adversity, as measured by the number of different adverse events, is a risk factor for chronic pain. The Adverse Childhood Experiences (ACE) study is an epidemiological investigation of the long-term relationship between adverse childhood experiences (ACEs) and a variety of health outcomes in adulthood, including chronic pain. Several ACE studies report a dose-dependent relationship between the number of adverse events and chronic pain. Specifically, the risk of frequent headaches was increased by at least twofold in individuals who reported four or more adverse experiences in childhood [8]. Others reported that one adverse event increased the risk of back pain and headaches by 13–40% and two or more events increased the risk by up to 63% [6,9]. Moreover, individuals with fibromyalgia reported more ACEs compared with healthy controls [10]. Interestingly, more childhood adverse events were associated with worse pain during late pregnancy [11]. Taken together, the impact of cumulative childhood adversity on pain may be more wide-ranging.
So far, studies have examined different aspects of childhood adversity separately, although the experience of different types of trauma may covary with levels of cumulative stress. To better understand the relationship between one aspect of childhood adversity and the risk of chronic pain conditions, a study should examine the relationship while holding the other aspect constant. Therefore, the current study examined whether more childhood adverse events would be associated with an increased risk of chronic pain conditions even when controlling for individual differences in experience of different trauma types. The current study also examined the alternative model, whether different types of childhood trauma would also be associated with an increased risk for chronic pain conditions when controlling for individual differences in the number of adverse events. This approach allows one to determine which aspects of childhood adversity are relevant and more clinically meaningful in evaluating the risk of chronic pain conditions above and beyond well-known risk factors such as female gender, substance use (cigarettes or alcohol), depression, anxiety, and somatization [12–15]. Finally, exploratory analyses examined whether childhood adversity was associated with multiple chronic pain conditions, as opposed to a single pain condition, and use of pain medications.
It was hypothesized that the experience of more childhood adverse events or the nature of specific types of trauma would increase the risk of common chronic pain conditions in young adults: any chronic pain, chronic back pain, chronic headache, and dysmenorrhea. It was also hypothesized that childhood adversity would be associated with more chronic pain conditions and use of pain medication.
Method
The Institutional Review Board at Texas A&M University reviewed and approved the study procedures. This online survey was advertised through the SONA System, the university’s research subject pool system that is used for prescreening and survey research involving undergraduate students. Regarding the informed consent process, before the survey questionnaire, participants read the purpose and nature of the survey and provided an electronic signature by typing their names and date. Participants received a course credit. Anyone interested could complete the survey as there were no eligibility criteria.
Self-Reports
Participants were asked to report current physical and mental health problems as well as current medications (prescription and nonprescription). Additionally, health risk behaviors such as current smoking status and drinking history for the past 30 days were assessed. The Early Traumatic Inventory Self-Report (ETISR) was administered to assess traumatic life events before age 18 years [16]. The ETISR is a 27-item questionnaire to assess traumatic life events in four domains (Table 1): general (Cronbach α = 0.70), physical (α = 0.75), emotional (α = 0.86), and sexual trauma (α = 0.87) [16]. The Pennebaker Inventory of Limbic Languidness (PILL) was also administered to assess the frequency of noticing and endorsing 54 common physical symptoms and sensations (α = 0.91) [17]. Example symptoms include itchy eyes or skin, ringing in ears, temporary deafness or hard of hearing, lump in throat, and choking sensations. The PILL scores were summed to assess levels of somatization, with higher scores indicating more somatic complaints.
Table 1.
Prevalence of specific traumatic events and calculating women’s odds ratio for specific traumas
| Item | Total (n = 3,073) | Men (n = 851) | Women (n = 2,222) | OR | 95% CI | |
|---|---|---|---|---|---|---|
| General trauma | (%) | (%) | (%) | |||
| 1 | Life-threatening natural disaster | 24.4 | 28.3 | 22.9 | 0.75** | 0.64–0.90 |
| 2 | Serious accident | 16.0 | 19.4 | 14.8 | 0.72** | 0.59–0.89 |
| 3 | Serious personal injury or illness | 29.5 | 35.7 | 27.2 | 0.67*** | 0.57–0.80 |
| 4 | Death or serious illness of a parent | 10.6 | 9.2 | 11.2 | 1.25 | 0.95–1.63 |
| 5 | Divorce or separation of your parents | 23.9 | 20.9 | 25.0 | 1.26* | 1.04–1.52 |
| 6 | Death or serious injury of a sibling | 6.9 | 7.3 | 6.7 | 0.92 | 0.67–1.24 |
| 7 | Death or serious injury of a friend | 32.6 | 32.2 | 32.8 | 1.03 | 0.87–1.22 |
| 8 | Witness violence toward others | 30.3 | 33.3 | 29.2 | 0.83* | 0.70–0.98 |
| 9 | Family member suffers from mental or psychiatric illness or has a “breakdown” | 23.7 | 17.9 | 25.9 | 1.61*** | 1.32–1.96 |
| 10 | Parents have a problem with alcoholism or drug or drug abuse | 12.4 | 9.2 | 13.6 | 1.57** | 1.20–2.03 |
| 11 | Seeing someone murdered | 0.6 | 1.5 | 0.3 | 0.18*** | 0.07–0.46 |
| Physical punishment | ||||||
| 1 | Slapped in the face with an open hand | 36.4 | 51.7 | 30.6 | 0.41*** | 0.35–0.48 |
| 2 | Burned with hot water, a cigarette, etc. | 30.6 | 41.8 | 26.2 | 0.50*** | 0.42–0.58 |
| 3 | Punched or kicked | 39.5 | 62.9 | 30.6 | 0.26*** | 0.22–0.31 |
| 4 | Hit with an object that was thrown at you | 57.0 | 73.9 | 50.5 | 0.36*** | 0.30–0.43 |
| 5 | Pushed or shoved | 63.2 | 80.1 | 56.8 | 0.33*** | 0.27–0.39 |
| Emotional abuse | ||||||
| 1 | Often put down or ridiculed | 35.2 | 38.9 | 33.8 | 0.80** | 0.68–0.94 |
| 2 | Often ignored or made to feel that you didn’t count | 28.7 | 28.8 | 28.7 | 1.00 | 0.84–1.19 |
| 3 | Often told you were no good | 16.8 | 18.8 | 16.1 | 0.83 | 0.67–1.02 |
| 4 | Most of the time treated in a cold, uncaring way or made to feel like you were not loved | 29.7 | 9.6 | 9.8 | 1.02 | 0.78–1.33 |
| 5 | Parents often fail to understand you or your needs | 10.9 | 10.5 | 11.1 | 1.07 | 0.83–1.38 |
| Sexual trauma | ||||||
| 1 | Touched in an intimate or private part of your body in a way that surprised you or made you feel uncomfortable | 10.0 | 5.1 | 11.9 | 2.54*** | 1.83–3.55 |
| 2 | Someone rubbed their genitals against you | 15.0 | 15.3 | 14.9 | 0.97 | 0.78–1.21 |
| 3 | Forced or coerced to touch another person in an intimate or private part of their body | 5.5 | 2.6 | 6.6 | 2.65*** | 1.68–4.18 |
| 4 | Genital sex with you against your will | 2.0 | 0.5 | 2.6 | 5.68*** | 2.05–15.68 |
| 5 | Forced or coerced to perform oral sex | 2.4 | 1.2 | 2.9 | 2.53** | 1.30–4.96 |
| 6 | Forced or coerced to kiss someone in a sexual rather than an affectionate way | 4.8 | 1.3 | 6.1 | 4.94*** | 2.66–9.18 |
CI = confidence interval; OR = odds ratio.
P < 0.05; **P < 0.01; ***P < 0.001.
Statistical Analysis
Odds ratios (ORs) were calculated to evaluate increased or decreased risk for the chronic pain conditions, given exposure to levels of traumatic experiences [18]. An OR of 1 indicates that early life stressors would not affect odds of health problems, whereas an OR of >1 or <1 indicates that early life stressors would increase or decrease risk of chronic pain problems, respectively. A hierarchical logistic regression model was used for multilevel analysis. Potential covariates were entered at the first level: gender (women = 1 and men = 0), health risk behaviors (current use of cigarettes and alcohol, yes = 1 or no = 0), psychiatric conditions (endorsement of current diagnosis of depression and anxiety disorders, yes = 1 or no = 0), and PILL scores. Then, at the second level, the total ETISR scores were entered to examine whether early life stressors would predict increased or decreased risk of chronic pain above and beyond gender differences, health risk behaviors, psychiatric conditions, and somatization. Next, trauma types at the third level were entered to examine whether trauma type would have any incremental value to risk prediction after adjusting for the levels of early life stressors. The ETISR total scores were standardized (z scores), and type of trauma was recoded into binary response (yes = 1 or no = 1). An alternative model entered trauma types in the second level and the total ETISR scores in the third level to examine whether more adverse events would still affect the odds of chronic pain conditions after controlling for different trauma types.
Data from those who did not finish the survey were not included in the analysis. No missing values were observed in data from those who completed the survey, except that five women (0.2%) did not report dysmenorrhea status. Pairwise deletion was used. A P value of <0.05 was used for all analyses. ORs were considered significant only when the model was also significant at P value of <0.05 according to the model chi-square statistic.
Sample Characteristics
A total of 3,073 undergraduates (72% female, mean age = 18.8 years, SD = 1.4 years) completed the online survey for current health status and early life traumatic events from September 2012 to April 2015. The survey was administered to prescreen individuals for subsequent laboratory pain studies. The majority were Caucasian (73%), followed by Hispanic (18%) and African American (4%).
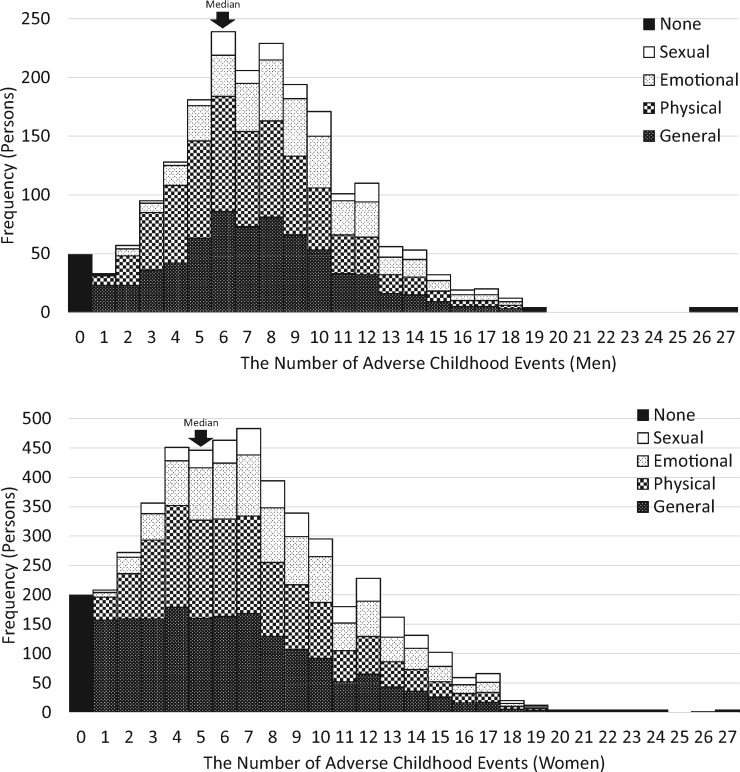
Participants reported on average 5.7 (SD = 4.1, IQR = 3–8, median = 5, mode = 4) traumatic life events during childhood and adolescence (Figure 1). Only 8% reported not experiencing any childhood traumas. Overall, general trauma was the most frequently endorsed trauma type (78%), followed by physical (73%), emotional (44%), and sexual (20%) traumas. The most frequent type was physical trauma for men (86% of men) and general trauma for women (78% of women). The likelihood of being exposed to any early life traumatic event was higher for men (OR = 1.61, P = 0.004, 95% confidence interval [CI] = 1.167–2.22), especially exposure to physical trauma (OR = 2.85, P < 0.001, 95% CI = 2.30–3.53), but less likely to sexual trauma (OR = 0.80, P < 0.001, 95% CI = 0.65–0.98). Table 1 describes the prevalence of specific traumas in early life and women’s odds of experiencing specific traumatic events. Except for sexual traumas, women were less likely to experience various traumatic events.
Figure 1.
Histogram of the number of adverse childhood events for men (upper) and women (lower).
Common mental and physical health problems (at least 1% prevalence) in our sample are listed in Table 2. Overall, women were more likely to report having mental and physical health problems (ORs = 1.45–3.66) except anxiety disorder, ADHD, allergy, asthma, and hypertension. Physical health problems were more common than mental health problems (29.0 vs 6.9%). Of physical health problems, chronic pain was the most frequently reported problem (21.5%), and chronic headache (9.8%) and chronic back pain (9.6%) were the two most common chronic pain conditions. Other endorsed chronic pain conditions (< 1% prevalence) were musculoskeletal pain other than back pain, arthritis, fibromyalgia, gastrointestinal pain, and genitourinary pain. Notably, a national study revealed a slightly higher prevalence rate of headache (15.4%) and low back pain (16.2%) in young adults aged 18 to 24 years compared with our sample [19]. On average, women in our sample reported more somatic symptoms on the PILL (β = 0.14, P < 0.001). Medication use was noted in the bottom part of Table 2. Less than one-third (31.8%) reported taking at least one medication. Use of any medication and any prescription medication were increased 2.98- and 1.47-fold for women, respectively. Notably, no gender difference was observed in the use of OTC and prescription medication for chronic pain. Dysmenorrhea was reported by 13% of women.
Table 2.
Prevalence of health problems and women’s odds ratio for health problems
| Total (n = 3,073), % | Men (n = 851), % | Women (n = 2,222), % | OR | 95% CI | |
|---|---|---|---|---|---|
| Mental health problems | |||||
| Any mental health problems | 6.9 | 5.3 | 7.5 | 1.45* | 1.03–2.03 |
| Depression | 3.3 | 1.4 | 4.1 | 2.95*** | 1.61–5.42 |
| Anxiety | 1.1 | 0.5 | 1.3 | 2.80 | 0.98–7.99 |
| ADHD | 3.8 | 4.1 | 3.6 | 0.88 | 0.59–1.32 |
| Physical health problems | |||||
| Any physical health problems | 29.0 | 19.6 | 32.6 | 1.98*** | 1.64–2.40 |
| Any chronic pain problems | 21.5 | 12.7 | 24.9 | 2.29*** | 1.83–2.86 |
| Headache or migraine | 9.8 | 3.6 | 12.2 | 3.66*** | 2.50–5.35 |
| Back pain | 9.6 | 5.8 | 11.1 | 2.05*** | 1.49–2.81 |
| Allergy | 5.0 | 5.5 | 4.8 | 0.87 | 0.61–1.23 |
| Hypotension | 2.6 | 1.3 | 3.1 | 2.45** | 1.29–4.65 |
| Hypertension | 1.3 | 2.5 | 0.9 | 0.34** | 0.18–0.64 |
| Asthma | 1.7 | 1.5 | 1.7 | 1.12 | 0.60–2.12 |
| Dysmenorrhea | N/A | N/A | 12.9 | ||
| Medication use | |||||
| Any medications | 31.8 | 16.8 | 37.5 | 2.98*** | 2.44–3.63 |
| Any prescription medication | 15.0 | 11.6 | 16.2 | 1.47** | 1.16–1.87 |
| Any psychiatric medication | 6.2 | 4.8 | 6.7 | 1.41 | 0.99–2.01 |
| Antidepressant | 3.2 | 1.4 | 3.8 | 2.78** | 1.51–5.11 |
| Anxiolytics | 0.6 | 0.5 | 0.6 | 1.34 | 0.44–4.09 |
| Stimulants (ADHD) | 3.6 | 4.0 | 3.5 | 0.86 | 0.57–1.30 |
| OTC pain medication | 1.2 | 1.2 | 1.2 | 1.00 | 0.48–2.07 |
| Prescription pain medication | 0.8 | 0.8 | 0.8 | 0.99 | 0.41–2.37 |
ADHD = attention deficit hyperactivity disorder; CI = confidence interval; OR = odds ratio; OTC = over the counter.
P < 0.05; **P < 0.01; ***P < 0.001.
Cigarettes and alcohol use were assessed as health risk behaviors. In our sample, 3.6% reported using cigarettes and 35% endorsed drinking alcohol. Binge drinking was defined by typical drinking as four (women) or five (men) drinks per occasion, and heavy drinking was defined by five or more drinks on one occasion and five or more days of drinking in the past 30 days. The prevalence of binge and heavy drinking was 4.9% and 5.6%, respectively. Gender differences were observed for all health risk behaviors, with women being less likely to use cigarettes (OR = 0.15, P < 0.001) and alcohol (OR = 0.76, P = 0.001), and less likely to binge drink (OR = 0.02, P < 0.001) to drink heavily (OR = 0.29, P < 0.001). The results of Point-Biserial correlations indicated that among the three alcohol-drinking behaviors, ETISR total scores were more strongly associated with overall alcohol drinking (r = 0.12, P < 0.001) than binge (r = 0.08, P < 0.001) or heavy drinking (r = 0.05, P = 0.006).
Results
Predicting Chronic Pain Conditions
Table 3 (left) shows the results of hierarchical logistic regression analysis in predicting any chronic pain condition. At level 1, female gender and higher PILL Z scores were associated with a 2.06- and 1.95-fold increase in the odds of having any chronic pain problem. A 1 SD increase in ETISR scores was associated with a 1.22-fold increase in the odds of any chronic pain problem regardless of controlling for trauma types (Model 2) or not (Model 1). However, trauma types did not add any incremental value in predicting any chronic pain problems when controlling for ETISR Z scores. Without controlling for the ETISR Z scores in Model 2, only general trauma was associated with a 1.50-fold increase in the odds of having any chronic pain disorder.
Table 3.
Hierarchical logistic regression to predict the odds of chronic pain conditions
| Level | Any Chronic Pain |
Chronic Back Pain |
Chronic Headache |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | χ2 | OR | 95% CI | χ2 | OR | 95% CI | χ2 | ||
| 1 | Gender (1 = female) | 2.06*** | 1.63–2.62 | 307.9*** | 1.72** | 1.23–2.39 | 141.2*** | 3.15*** | 2.12–4.67 | 189.3*** |
| Drinking alcohol | 1.19 | 0.98–1.44 | 1.15 | 0.89–1.48 | 1.13 | 0.87–1.47 | ||||
| Cigarette use | 1.66* | 1.02–2.69 | 1.05 | 0.53–2.07 | 1.27 | 0.63–2.54 | ||||
| Depression | 1.27 | 0.87–2.03 | 1.31 | 0.73–2.36 | 2.18** | 1.29–3.69 | ||||
| Anxiety | 1.92 | 0.87–4.23 | 1.89 | 0.77–4.62 | 0.88 | 0.33–2.33 | ||||
| PILL Z scores | 1.95*** | 1.78–2.14 | 1.81*** | 1.62–2.03 | 1.84*** | 1.64–2.06 | ||||
| Model 1 | ||||||||||
| 2 | ETISR Z scores | 1.22*** | 1.11–1.33 | 17.1*** | 1.31*** | 1.16–1.48 | 19.2*** | 1.13 | 1.00–1.28 | 3.7 |
| 3 | ETISR–general trauma | 1.34 | 1.01–1.76 | 4.9 | 1.01 | 0.69–1.47 | 1.5 | 1.41 | 0.95–2.09 | 9.0 |
| ETSR–physical trauma | 0.95 | 0.73–1.24 | 0.97 | 0.67–1.41 | 0.80 | 0.56–1.13 | ||||
| ETISR–emotional trauma | 0.98 | 0.78–1.23 | 1.21 | 0.89–1.66 | 0.84 | 0.61–1.16 | ||||
| ETSR–sexual trauma | 1.02 | 0.80–1.32 | 1.06 | 0.76–1.47 | 0.77 | 0.54–1.09 | ||||
| Model 2 | ||||||||||
| 2 | ETISR–general trauma | 1.50** | 1.17–1.94 | 17.9** | 1.18 | 0.84–1.67 | 16.5** | 1.66 | 1.15–2.38 | 8.2 |
| ETSR–physical trauma | 1.08 | 0.85–1.36 | 1.14 | 0.82–1.60 | 0.94 | 0.69–1.29 | ||||
| ETISR–emotional trauma | 1.11 | 0.91–1.35 | 1.42* | 1.08–1.87 | 1.03 | 0.76–1.32 | ||||
| ETSR–sexual trauma | 1.15 | 0.92–1.44 | 1.24 | 0.93–1.66 | 0.91 | 0.67–1.25 | ||||
| 3 | ETISR Z scores | 1.18* | 1.01–1.38 | 4.2* | 1.23* | 1.01–1.51 | 4.2* | 1.25* | 1.02–1.54 | 4.5* |
CI = confidence interval; ETISR = Early Trauma Inventory Self-Report; OR = odds ratio; PILL = Pennebaker Inventory of Limbic Languidness.
P < 0.05; **P < 0.01; ***P < 0.001, χ2 for the block.
Table 3 (middle) depicts the results in predicting chronic back pain. Female gender and PILL z scores were associated with a 1.72- and a 1.81-fold increase in the odds of having chronic back pain, respectively. A 1 SD increase in ETISR scores was associated with a 31% increase in the odds of chronic back pain in Model 1 and a 23% increase in Model 2. Trauma types did not add any incremental value in predicting chronic back pain in Model 1, whereas emotional trauma was associated with a 1.42-times increase in the odds of chronic back pain in Model 2.
Table 3 (right) depicts the results in predicting chronic headaches. At level 1, female gender, depression, and PILL z scores were associated with a 1.84–3.15-fold increase in the odds of chronic headache. In Model 1, ETISR Z scores and trauma types did not predict chronic headache. In contrast, ETISR Z scores were associated with a 1.25-fold increase in the odds of chronic headache when controlling for trauma types.
Taken together, female gender and greater somatization were associated with an increase in the odds of back pain, headache, and any chronic pain condition. Depression was associated with risk of chronic headache. In comparing the two aspects of childhood adversity, more childhood adverse events predicted increased risks of any chronic pain condition and back pain, regardless of trauma type. More childhood adverse events were associated with an increased risk of headache only when controlling for trauma type. However, trauma type did not predict any of the above chronic pain conditions when controlling for the number of childhood adverse events.
Predicting Dysmenorrhea in Women
At level 1, only PILL Z scores were associated with the odds of dysmenorrhea, with higher somatization being related to greater risk (OR = 1.35, 95% CI = 1.20–1.51, P < 0.001; χ2 = 31.6, P < 0.001). At level 2, a 1 SD increase in ETISR scores was associated with a 39% increase in the odds of dysmenorrhea (OR = 1.39, 95% CI = 1.24–1.57, P < 0.001; χ2 = 28.2, P < 0.001). When controlling for the number of childhood adverse events, trauma type was unrelated to the risk of dysmenorrhea (level 3, Ps > 0.190). In Model 2, only sexual trauma was associated with an increase in the odds of dysmenorrhea (level 2, OR = 1.58, 95% CI = 1.21–2.11, P = 0.002; χ2 = 19.8, P = 0.001). Even when controlling for trauma type, a 1-SD increase in ETISR scores was associated with a 44% increase in the odds of dysmenorrhea (level 3, OR = 1.44, 95% CI = 1.17–1.76, P < 0.001; χ2 = 12.1, P = 0.001).
Predicting Multiple Chronic Pain Conditions
Using the data from 662 participants with at least one pain condition, hierarchical logistic regression was conducted to examine the number of adverse events and specific trauma types as a risk factor for multiple chronic pain conditions, as opposed to a single pain condition. When gender, use of alcohol and cigarettes, depression and anxiety disorders, and PILL scores were entered at level 1, smoking (OR = 2.56, 95% CI = 1.12–5.85, P = 0.026), depression (OR = 2.15, 95% CI = 1.01–4.57, P = 0.046), and PILL Z scores (OR = 1.54, 95% CI = 1.30–1.81, P < 0.001) were associated with an increase in the odds of having multiple pain conditions (χ2 = 53.0, P < 0.001). In both Models 1 and 2, ETISR Z scores and type of trauma were unrelated to multiple chronic pain conditions (Ps > 0.148).
Predicting Use of Pain Medications
Depression and PILL z scores were associated with a 7.11-fold (P < 0.001) and 1.53-fold (P = 0.012) increase in using prescription pain medications, respectively. All the other predictors were nonsignificant (Ps > 0.476) at level 1. In both Models 1 and 2, ETISR Z scores and trauma type were unrelated to use of prescription pain medication (Ps > 0.075). In predicting use of OTC pain medication (n = 3,073), no significant results were observed across 1–3 level analyses (Ps > 0.050).
Discussion
The current study investigated whether adverse childhood events increase the risk of common pain disorders in young adults. We evaluated the contribution of two aspects of childhood adversity in predicting the odds of having chronic pain: 1) the number of events and 2) the nature of the events. Specifically, we examined whether one aspect was associated with an increase in the odds of having a chronic pain condition while controlling for the other aspect. Our results suggest that the number, as opposed to the nature, of the adverse events may be a better predictor of chronic pain in young adults. In particular, we found that individuals reporting multiple adverse events had a 1.2–1.4-fold increase in the odds of having any chronic pain condition, chronic back pain, chronic headache, and/or dysmenorrhea, even after controlling for individual differences in the nature of their trauma type. However, when controlling for the number of adverse events, trauma type was unrelated to the risk of having a chronic pain condition. Therefore, evaluating the number of childhood adverse events appears to be more relevant in predicting the risk of chronic pain than exposure to a specific type of trauma. Notably, the number of adverse events predicted the odds of having a chronic pain condition even when controlling for other risk factors such as female gender, depression, anxiety, alcohol use, smoking, and somatization. Finally, childhood adversity was unrelated to multiple pain conditions and use of pain medications.
Controversy of Childhood Adversity as a Risk Factor for Chronic Pain
Previous studies investigating the relationship between the type of adverse childhood events and chronic pain risk have yielded inconsistent findings. Data from cross-sectional studies have shown a significant relationship between childhood experience of specific traumas and adulthood chronic pain conditions such as fibromyalgia [1,2], chronic pelvic pain [3], migraine [4], and neck/back pain [5,6]. A prospective birth cohort study has observed an elevated risk of chronic widespread pain in adults who have experienced maternal separation, household dysfunction, or financial difficulties by age seven [7]. However, other studies report no significant associations [20]. Of our participants, experience of any type of childhood adversity was quite common. Only 8% reported not experiencing any types of trauma. The most common trauma types were general (family dysfunction, 78%), physical (73%), emotional (44%), and sexual events (20%). In contrast, the prevalence of chronic pain was only about 10–22%. Consequently, most participants who reported experiencing a specific type of trauma endorsed no chronic pain conditions.
Cumulative Childhood Stress as a Risk Factor for Chronic Pain
Our results suggest that even after controlling for trauma type, the number of childhood adverse events predicted the odds of having a chronic pain condition. Our results are consistent with previous studies observing an increased risk of frequent headaches [6,8] and back pain [6,9] in adults with more childhood adverse events. However, the cross-sectional nature of this work limits our ability to infer the direction of causality. To date, no prospective studies have examined whether the number of childhood adverse events is a risk factor in humans. Although a prospective study would be ideal, assessing without intervening in cumulative stressors from birth to the end of the childhood period and monitoring the development of chronic pain conditions may not be ethical or practical. Instead, several animal studies have demonstrated the possibility of cumulative childhood stress as a cause for chronic pain conditions. For example, repeated exposure to neonatal stress results in pain hypersensitivity in adult rats [21–25].
Another way of investigating the number of adverse events as a vulnerability factor for chronic pain is to examine laboratory pain responses in healthy and pain-free individuals. Consistent with the current results, others have not observed pain hypersensitivity in healthy individuals endorsing childhood physical or sexual abuse alone [26], whereas our laboratory has observed pain hypersensitivity in healthy individuals reporting more childhood adverse events [27,28]. Hence, evaluating cumulative childhood stress either by exposure to the number of same or different childhood adverse events may be a more relevant aspect of childhood adversity in investigating its link to chronic pain conditions.
Mechanisms Linking Cumulative Childhood Stress and Adulthood Chronic Pain
One way to explain the link between adverse childhood events and adulthood chronic pain is allostatic load. The allostasis model suggests that adverse events activate integrative–adaptive systems such as the endocrine, immune, and nervous systems, and this active adjustment process is called “allostasis,” maintaining stability through change [29]. Insufficient or prolonged activity of certain mediators of allostasis creates dysregulation of the adaptive systems [29,30]. Over time, multiple adverse events lead to allostatic overload, which can cause detrimental consequences, and this is particularly important during development when systems are maturing [30]. A population study has examined the relationships between biomarkers of allostatic load and the prevalence of severe headache, pain lasting at least 24 hours, and widespread pain [31]. Their results indicated that higher allostatic load indices were associated with greater prevalence of the three pain conditions.
Implications
Our study suggests that multiple childhood adverse events, as opposed to exposure to a specific adverse event, are associated with greater risk of chronic pain in young adults. Therefore, assessing the number of childhood adversity types may help clinicians identify individuals at risk for developing chronic pain conditions and offer them preventive interventions. Several measures, such as the ETISR-SF and the ACE questionnaires, are available and can be easily administered in busy clinics to evaluate multiple types of childhood adversity. For researchers, we recommend evaluating the cumulative or chronic nature of childhood stress—such as the number of event types or frequency of events—when investigating its link to adult chronic pain. We also recommend that a general trauma subscale (e.g., natural disaster, divorce, sickness of close friend, etc.) be included in assessments as general adversity was commonly endorsed in our sample and contributed to the risk of chronic pain.
Limitations
A large sample size is a major strength of the current study. However, using self-reported childhood adversity is subject to recall bias. Notably, a review of the reliability and validity of adult reporting of childhood adverse events indicated that while retrospective reporting involves the issue of false negatives and false positives, it is sufficiently reliable and valid, particularly when data are collected from nonclinical and nonjudicial groups, as in the current study [32]. Additionally, generalizability may be limited because the current participants were highly functioning undergraduates. According to a national survey, about 37% of young adults reported persistent pain problems in the past 30 days, which is higher than our sample (e.g., 22% for any chronic pain conditions) [33]. Yet, our results suggested that childhood adversity is a risk factor for chronic pain conditions even in high-functioning young adults and college students and, therefore, highlight the importance of assessing young adults’ childhood adversity in primary and student health clinics. Lastly, our data only allowed us to examine the risk of chronic back pain, chronic headache, and dysmenorrhea. The prevalence rates of other chronic pain conditions that are associated with childhood adversity, such as fibromyalgia [1,2], chronic pelvic pain [3], arthritis [34], and irritable bowel syndrome [35], were low in our sample.
Conclusion
Our results showed that cumulative adverse childhood events increased the risk for chronic pain conditions in young adults. After controlling for gender, substance use, psychiatric conditions, and somatization tendency, more childhood adverse events were associated with an increased risk of any chronic pain condition, chronic back pain, chronic headache, and dysmenorrhea, but were not associated with the risk of comorbid pain conditions and use of pain medications. These relationships remained significant when controlling for different types of trauma. However, experience of specific traumas was unrelated to chronic pain conditions when controlling for the number of childhood adverse events. Thus, cumulative stress during childhood may increase the risk of chronic pain conditions, specifically for any chronic pain conditions, chronic back pain, chronic headache, and dysmenorrhea in young adults. Therefore, evaluating the number of childhood adverse events may be more relevant in investigating childhood adversity as a risk factor for chronic pain conditions than evaluating different types of trauma.
Funding sources: Dokyoung Sophia You received an F31 NRSA predoctoral fellowship training grant from the National Institute on Alcohol Abuse and Alcoholism (Grant No. 1F31AA023709-01A1).
Conflicts of interest: All authors report no conflicts of interest regarding this publication.
Participant consent: Written informed consent was obtained from all participants.
References
- 1. Häuser W, Kosseva M, Üceyler N, Klose P, Sommer C.. Emotional, physical, and sexual abuse in fibromyalgia syndrome: A systematic review with meta‐analysis. Arthritis Care Res 2011;636:808–20. [DOI] [PubMed] [Google Scholar]
- 2. Boisset-Pioro MH, Esdaile JM, Fitzcharles MA.. Sexual and physical abuse in women with fibromyalgia syndrome. Arthritis Rheum 1995;382:235–41. [DOI] [PubMed] [Google Scholar]
- 3. Walling MK, Reiter RC, O’hara MW, et al. Abuse history and chronic pain in women: I. Prevalences of sexual abuse and physical abuse. Obstet Gynecol 1994;842:193–9. [PubMed] [Google Scholar]
- 4. Tietjen GE, Brandes JL, Peterlin BL, et al. Childhood maltreatment and migraine (part II). Emotional abuse as a risk factor for headache chronification. Headache 2010;501:32–41. [DOI] [PubMed] [Google Scholar]
- 5. Stickley A, Koyanagi A, Kawakami N.. WHO World Health Mental Health Japan Survey Group. Childhood adversities and adult-onset chronic pain: Results from the World Mental Health Survey, Japan. Eur J Pain 2015;1910:1418–27. [DOI] [PubMed] [Google Scholar]
- 6. Scott KM, Von Korff M, Angermeyer MC, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatry 2011;688:838–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jones GT, Power C, Macfarlane GJ.. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain 2009;143(1–2):92–6. [DOI] [PubMed] [Google Scholar]
- 8. Anda R, Tietjen G, Schulman E, Felitti V, Croft J.. Adverse childhood experiences and frequent headaches in adults. Headache 2010;509:1473–81. [DOI] [PubMed] [Google Scholar]
- 9. Kopec JA, Sayre EC.. Stressful experiences in childhood and chronic back pain in the general population. Clin J Pain 2005;216:478–83. [DOI] [PubMed] [Google Scholar]
- 10. Imbierowicz K, Egle UT.. Childhood adversities in patients with fibromyalgia and somatoform pain disorder. Eur J Pain 2003;72:113–9. [DOI] [PubMed] [Google Scholar]
- 11. Drevin J, Stern J, Annerbäck E-M, et al. Adverse childhood experiences influence development of pain during pregnancy. Acta Obstet Gynecol Scand 2015;948:840–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McBeth J, Macfarlane GJ, Benjamin S, Silman AJ.. Features of somatization predict the onset of chronic widespread pain: Results of a large population‐based study. Arthritis Rheum 2001;444:940–6. [DOI] [PubMed] [Google Scholar]
- 13. Magni G, Moreschi C, Rigatti-Luchini S, Merskey H.. Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain 1994;563:289–97. [DOI] [PubMed] [Google Scholar]
- 14. Gupta A, Silman A, Ray D, et al. The role of psychosocial factors in predicting the onset of chronic widespread pain: Results from a prospective population-based study. Rheumatology 2007;464:666–71. [DOI] [PubMed] [Google Scholar]
- 15. Strine TW, Hootman JM.. US national prevalence and correlates of low back and neck pain among adults. Arthritis Care Res 2007;574:656–65. [DOI] [PubMed] [Google Scholar]
- 16. Bremner JD, Bolus R, Mayer EA.. Psychometric properties of the early trauma inventory–self report. J Nerv Ment Dis 2007;1953:211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pennebaker JW. The Psychology of Physical Symptoms. New York Heidelberg Berline: Springer-Verlag; 1982. [Google Scholar]
- 18. Szumilas M. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry 2010;193:227–9. [PMC free article] [PubMed] [Google Scholar]
- 19. National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 20. Raphael KG, Chandler HK, Ciccone DS.. Is childhood abuse a risk factor for chronic pain in adulthood? Curr Pain Headache Rep 2004;82:99–110. [DOI] [PubMed] [Google Scholar]
- 21. Green PG, Chen X, Alvarez P, Ferrari LF, Levine JD.. Early-life stress produces muscle hyperalgesia and nociceptor sensitization in the adult rat. Pain 2011;15211:2549–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alvarez P, Green PG, Levine JD.. Stress in the adult rat exacerbates muscle pain induced by early-life stress. Biol Psychiatry 2013;749:688–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moloney RD, O'Leary OF, Felice D, et al. Early-life stress induces visceral hypersensitivity in mice. Neurosci Lett 2012;5122:99–102. [DOI] [PubMed] [Google Scholar]
- 24. Holschneider D, Guo Y, Mayer E, Wang Z.. Early life stress elicits visceral hyperalgesia and functional reorganization of pain circuits in adult rats. Neurobiol Stress 2016;3:8–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guo Y, Wang Z, Mayer EA, Holschneider DP.. Neonatal stress from limited bedding elicits visceral hyperalgesia in adult rats. Neuroreport 2015;261:13–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fillingim RB, Edwards RR.. Is self-reported childhood abuse history associated with pain perception among healthy young women and men? Clin J Pain 2005;215:387–97. [DOI] [PubMed] [Google Scholar]
- 27. You DS, Meagher MW.. Childhood adversity and pain sensitization. Psychosom Med 2016;789:1084–93. [DOI] [PubMed] [Google Scholar]
- 28. You DS, Creech SK, Vichaya EG, et al. Effect of written emotional disclosure on secondary hyperalgesia in women with trauma history. Psychosom Med 2014;765:337–46. [DOI] [PubMed] [Google Scholar]
- 29. McEwen BS. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology 2000;222:108–24. [DOI] [PubMed] [Google Scholar]
- 30. Danese A, McEwen BS.. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav 2012;1061:29–39. [DOI] [PubMed] [Google Scholar]
- 31. Slade GD, Sanders AE, By K.. Role of allostatic load in sociodemographic patterns of pain prevalence in the U.S. Population. J Pain 2012;137:666–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hardt J, Rutter M.. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. J Child Psychol Psychiatry 2004;452:260–73. [DOI] [PubMed] [Google Scholar]
- 33. US Department of Health and Human Services. Health, United States, 2005: With Chartbook on Trends in the Health of Americans. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2005. [Google Scholar]
- 34. Von Korff M, Alonso J, Ormel J, et al. Childhood psychosocial stressors and adult onset arthritis: Broad spectrum risk factors and allostatic load. Pain 2009;143(1–2):76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol 2012;104:385–90. [DOI] [PMC free article] [PubMed] [Google Scholar]