Abstract
Aims:
To evaluate the use of relatively low levels of hydrogen peroxide vapour (HPV) for the inactivation of Bacillus anthracis spores within an indoor environment.
Methods and Results:
Laboratory-scale decontamination tests were conducted using bacterial spores of both B. anthracis Ames and Bacillus atrophaeus inoculated onto several types of materials. Pilot-scale tests were also conducted using a larger chamber furnished as an indoor office. Commercial off-the-shelf (COTS) humidifiers filled with aqueous solutions of 3 or 8% hydrogen peroxide (H2O2) were used to generate the HPV inside the mock office. The spores were exposed to HPV for periods ranging from 8 h up to 1 week.
Conclusions:
Four- to seven-day exposures to low levels of HPV (average air concentrations of approx. 5–10 parts per million) were effective in inactivating B. anthracis spores on multiple materials. The HPV can be generated with COTS humidifiers and household H2O2 solutions. With the exception of one test/material, B. atrophaeus spores were equally or more resistant to HPV inactivation compared to those from B. anthracis Ames.
Significance and Impact of the Study:
This simple and effective decontamination method is another option that could be widely applied in the event of a B. anthracis spore release.
Keywords: antimicrobials, Bacillus anthracis, bacterial spores, biocides, hydrogen peroxide vapour, sterilization
Introduction
Deliberate dissemination of Bacillus anthracis (Ames strain) endospores (referred to as spores for the rest of this manuscript) through letters processed by the US Postal Service in the fall of 2001 led to the contamination of numerous offices, buildings and residences across Florida, New Jersey, New York and Washington DC. Hydrogen peroxide vapour (HPV) was used to decontaminate two of the affected buildings (Canter 2005). At that time, the optimal application conditions (concentration, contact time, temperature and relative humidity (RH)) for use of HPV to inactivate B. anthracis spores in a building were unknown. For one of the contaminated buildings (Department of State SA-32), it was decided to fumigate using a target HPV concentration of 216 parts per million (ppm) for 4 h, with temperature held above 21 °C (US EPA 2005). Special efforts were required (e.g. complete removal of all interior materials and equipment to reduce demand for the HPV fumigant, subdividing the building into 10 separate decontamination zones to reduce needed capacity to generate the HPV, the use of several modified HPV generators), and difficulties were encountered, in order to reach and maintain the target HPV concentration.
HPV has been widely used for decontamination of healthcare, pharmaceutical, animal and food industry facilities (Klapes and Vesley 1990; McDonnell and Russell 1999; Krause et al. 2001; Johnston et al. 2005; Barbut et al. 2009). Effective decontamination using HPV has been demonstrated against a wide range of micro-organisms, including vegetative bacteria (French et al. 2004; Kahnert et al. 2005; Rogers et al. 2008), viruses (Heckert et al. 1997), and bacterial spores (Johnston et al. 2005; Rogers et al. 2005; Rastogi et al. 2009; Lawley et al. 2010; Malik et al. 2013). HPV has also been shown to inactivate prions (Fichet et al. 2007).
Laboratory testing of HPV as a sterilant has typically focused on exposure of relatively short durations (2–4 h) at high concentration (>200 ppm) using specialized equipment and concentrated liquid feedstock, for example, 35% concentration of H2O2 in aqueous solution. While this approach may be appropriate for routine decontamination of facilities in regular use, implementation on a large scale and in a field setting would be problematic. It is also difficult to attain and maintain high concentrations of HPV in a building without large generating equipment (this is actually a problem for any fumigant), and isolation of the fumigant poses a safety challenge. In addition, high concentrations were found to pose a risk of material incompatibility and resulted in off-gassing of HPV for extended periods in lined ventilation duct (Meyer et al. 2014). These results, and reports of other HPV outgassing research (Baron et al. 2007), led to the present study, which investigated the sporicidal effects of relatively long durations of low concentration HPV generated with simple, readily available commercial off-the-shelf (COTS) humidifiers.
Decontamination tests were conducted at EPA’s Research Triangle Park (NC) laboratories using Bacillus atrophaeus spores, with the HPV disseminated using COTS humidifiers in a pilot-scale chamber. Laboratory (bench-scale) tests were also conducted at the Edgewood Chemical and Biological Center (ECBC) facility in Edgewood, MD, with spores of both B. anthracis Ames and B. atrophaeus. Tests were conducted to assess the effect of operational variables such as the type of humidifier; quantity and concentration of the aqueous H2O2 solution; and contact time, on decontamination efficacy. In addition, the tests in the pilot-scale chamber allowed us to assess the effect of location within the chamber on decontamination efficacy, while the bench-scale tests allowed us to compare the degree of inactivation between the two species.
Materials and methods
Test organisms and inoculation procedures
Dried spores of B. atrophaeus (ATCC 9372; formerly Bacillus subtilis var. niger and Bacillus globigii) were obtained from the US Army Dugway Proving Ground Life Science Division, and were prepared as described previously (Brown et al. 2007). Briefly, B. atrophaeus was cultivated, then allowed to sporulate, centrifuged, then spray dried. This spore product was then blended with silicon dioxide particles. Refer to Brown et al. (2007) for further details. The surfaces of the materials were inoculated with B. atrophaeus spores via a metered dose inhaler (MDI) according to the aerosol deposition-based inoculation methods described previously (Lee et al. 2011), yielding approx. 1 × 107 spores over a 18 mm diameter coupon surface. Each inoculation event consisted of one actuation from the MDI.
The B. anthracis Ames spores were prepared as detailed in Rastogi et al. (2009). Briefly, an overnight tryptic soy broth culture was seeded on Lab Lemko agar plates and incubated at 37 ± 2°C. The plates were daily monitored microscopically for sporulation progression for a period of 7–9 days. When the sporulation reached ≥95%, the spores were harvested from the plates using cold sterile water. The suspension was washed three times in cold sterile water by repeated centrifugations (9 300 g for 30 min) to remove cell debris and media co-contaminants. The spore suspension was heat-treated at 65°C for 30 min before use. The master stock was enumerated and diluted to a working stock of 2 × 108 CFU ml−1 in sterile distilled water containing 0·1% Tween-80 and stored at 4°C until use, within 1 month.
The B. anthracis Ames spores were inoculated onto test coupons the afternoon before each experiment as follows. Test coupons were placed flat in a biological safety cabinet (BSC) and inoculated at approx. 107 CFU per coupon. A 50 μl aliquot of the well-mixed stock suspension of spores was dispensed with a micropipette via five droplets across the surface of the test coupon. This approach provided more uniform distribution of spores across the coupon surface, as opposed to application of a single drop of the suspension. After inoculation, the test coupons remained undisturbed for an hour in the BSC to initially dry under ambient conditions. The coupons, in Petri plates, were covered and then moved to an incubator at room temperature to finish drying overnight.
Test material coupons
All materials used for decontamination testing were fabricated into circular coupons 18 mm in diameter (Fig. 1) as follows. Oak wood coupons were 8-mm-thick plugs (part SPO750; Woodworks Ltd, Haltom City, TX), while the borosilicate glass coupons were 3·3-mm-thick plugs (Prism Research Glass, Inc., Research Triangle Park, NC). The 18 mm discs were cut from 26-gauge galvanized steel (East Coast Metal, Durham, NC), carpet (Multiplicity 54594; Shaw Industries Group, Dalton, GA), laminate flooring (Pergo Estate Oak Laminate Flooring from Home Depot, Atlanta, GA; SKU 257063 – no longer available) and ceiling tile (Armstrong, Lancaster, PA; P/N 949, Lowes SKU 40684). Concrete coupons were cast from sand and cement mix (Quikrete Model 110360, Atlanta, GA). The front facing of the wallboard (Gold-Bond, Mooresville, NC; P/N GB00090800, Lowes SKU 34137) was primed (Kilz, Masterchem Industries, Imperial, MO; 2-gal, P/N 20005; Home Depot SKU 317390) and painted (Behr Premium Plus Flat White Latex, Atlanta, GA, P/N 105001, Home Depot SKU 923827). The paper was then removed from the gypsum before 18mm discs were cut from the paper. All aforementioned materials were then mounted to 18 mm aluminium stubs (P/N 16119; Ted Pella, Inc., Redding, CA) using doublesided adhesive tape (P/N 16073-2; Ted Pella, Inc.) and placed in holder trays. To prevent contamination and bias of results due to nontarget organisms, all coupons and stubs were sterilized prior to tests by exposure to ethylene oxide per procedures specified by manufacturer (Anderson EOGas AN333 Sterilization System, Haw River, NC).
Figure 1.
Photograph of 18 mm diameter coupons of materials mounted on stubs and placed in holder trays. [Colour figure can be viewed at wileyonlinelibrary.com]
Pilot-scale decontamination chamber and mock office test environment
Decontamination tests using only B. atrophaeus spores were conducted in a pilot-scale stainless steel-lined chamber built specifically for decontamination testing, with internal dimensions of approx. 3·4-m wide by 2·5-m deep by 2·8-m high. We have named this chamber the Consequence Management and Decontamination Evaluation Room, or COMMANDER. Refer to Wood et al. (2013) for additional details on the overall design and operation of COMMANDER. Briefly, at the entrance to the inner chamber is an airlock compartment, and enclosing the chamber and airlock is an exterior steel shell. All three components of COMMANDER are kept under slight cascading negative pressure (most negative within the innermost compartment) with the use of separate air streams, with valve controls on the inlet and outlet of each to minimize leakage of hazardous materials to occupational areas in proximity to the chamber. Air entering the decontamination chamber passes through a high efficiency particulate air (HEPA) filter, and exhaust air from the decontamination chamber is ducted to an activated carbon bed and HEPA filter prior to release to the facility exhaust system. Within the chamber, temperature and RH data are continuously monitored and logged using a supervisory control and data acquisition (SCADA) system. Other operational parameters of the chamber system, such as air pressures, flow rate, and air duct valves are controlled and/or their data logged via the SCADA system. Valves in the ducts at the inlet and outlet of the inner chamber were shut to prevent air flow during tests, except when air exchange was used (discussed later). The HPV levels within the chamber were measured continuously with an electrochemical sensor (Model B12; Analytical Technology Inc., Collegeville, PA), which was connected to the SCADA system. This HPV sensor had a range of 0–1000 ppm, and was calibrated prior to each test using ambient air as zero and the head space equilibrium concentration (varied between 250 and 300 ppm depending on ambient temperature) of an aqueous H2O2 solution. In the first test (Test C1), we used a similar sensor with a range of 0–10 ppm tied into a feedback loop set at 5 ppm, such that the humidifier would be shut off when the HPV concentration rose above the set point. Temperature and RH within the decontamination chamber were measured with a Vaisala Model 333 sensor and transmitter. This instrument was calibrated prior to each test by comparing its RH data with known RH values generated in the sealed headspace above individual saturated solutions of various salt compounds (Vaisala HMK15, Helsinki Finland).
The stainless steel surfaces of the decontamination chamber were covered by materials typical of an indoor office setting. The mock office arrangement allows for a realistic setting to conduct the tests, and in particular, the materials in the office may absorb or react with the HPV, thus creating a demand or challenge to maintaining desired concentration. The floor was covered with plywood and then carpet, the walls were finished with painted wallboard, and a drop ceiling was installed with acoustic ceiling tiles. The ‘office’ itself was furnished with equipment consisting of a laminated desk, an office chair, a file cabinet, pin cushion screen, books/catalogues and a computer with monitor and keyboard. A small oscillating fan was also included in the office to assist with distribution of the HPV. Refer to US EPA (2014) for further details on the mock office. For the pilot-scale tests, a set of four coupons (three test coupons, and one negative coupon) of each material was inserted at each testing location immediately before the start of the experiment. Coupon locations within the mock office were on the desk, on the floor beneath the desk, and in the plenum above the drop ceiling (with one ceiling tile panel removed). The humidifier was placed on the floor in the centre of the chamber. Positive controls (coupons of each material inoculated with the target organism but not exposed to the HPV) were kept undisturbed in a sealed container adjacent to but outside of the decontamination chamber.
Small chamber test environment
The chamber used for the ECBC tests using B. anthracis Ames is described in Rastogi et al. (2009). Briefly, the custom made 0·23 m3 volume chamber is constructed with 316L stainless steel with four sanitary ports and a sampling port. Temperature, RH and HPV concentration were measured and recorded using similar methods and equipment as described for the mock office tests. A small fan was installed in the chamber to facilitate air and HPV circulation. After the desired contact time, the coupons were withdrawn from the chamber and aerated in a BSL-2 hood before processing.
Test conditions
The test matrix for the pilot-scale experiments is shown in Table 1. All tests were conducted at the laboratory ambient temperature of approx. 21 °C. Three types of humidifiers were used to disperse the aqueous H2O2 feedstock into the air: an ultrasonic (Vicks P/N V5100NS; The Procter and Gamble Company, Cincinnati, OH), heated vaporizer (P/N 975CVS; CVS Corporation, Woonsocket, RI) and sponge evaporation (P/N HCM-6009; Honeywell, Morristown, NJ). These humidifiers have a capacity of approx. 4–6 l, and varying quantities of the aqueous H2O2 solution were disseminated into the mock office as an experimental variable. In Table 1, the amount of solution disseminated in each test is normalized by the chamber volume (24·4 m3) to allow for extrapolation/comparison of results from other tests. The amount of solution ranged from 128 to 224 ml m−3 for the pilot-scale tests. Two feedstocks of aqueous H2O2 solution were used in the study: 3% H2O2 (CVS, Woonsocket, RI) and 8% H2O2 (Family Health News, Miami Shores, FL). Both concentrations can be shipped without hazardous labelling, but 3% is more readily available. The contact time for all of the pilot-scale tests was 1 week, that is, the test coupons were recovered from the chamber 1 week after the humidifier was turned on. With the exception of the first test (C1) and Test C7, the humidifiers ran uncontrolled until the aqueous H2O2 feedstock solution was disseminated. In Test C1, the HPV level was held to 5 ppm by turning on and off the humidifier automatically as needed via a feedback loop controlled by the SCADA. The 5 ppm HPV level was selected in light of previous research, for example, Meyer et al. (2014), as well as observations of low HPV levels following facility reset operations. In Test C7, the humidifier was turned on and off every 30 min until the aqueous solution was vaporized. Finally, in a majority of the tests, the chamber was sealed and allowed for no air flow. However, in a few of the tests, air ducts at the inlet and outlet of the chamber were left slightly open, which allowed for some air flow. This is noted in Table 1 as air exchange, which is defined as the fraction of the volume of the chamber replaced each hour.
Table 1.
Pilot-scale test conditions
| Test ID | Humidifier type | Starting H2O2 concentration in aqueous solution (%) |
H2O2 solution disseminated, ml per m3 of chamber volume |
Air exchange used (fraction of chamber volume replaced each hour) |
Average HPV concentration ppm |
Max HPV concentration ppm |
HPV dose (ppm h) | Avg RH (%) | Max RH (%) |
|---|---|---|---|---|---|---|---|---|---|
| Test C1* | Ultrasonic | 8 | 128 | None | 5·5 | 7·3 | 889 | 74 | 81 |
| Test C2 | Ultrasonic | 8 | 164 | None | 11 | 78 | 1900 | 75 | 93 |
| Test C3 | Sponge evaporation | 8 | 154 | None | 9 | 43 | 1430 | 72 | 88 |
| Test C4 | Ultrasonic | 8 | 173 | 0.3 | 11 | 59 | 1716 | 54 | 91 |
| Test C5 | Heated vaporizer | 8 | 161 | None | 7·5 | 69 | 1224 | 77 | 94 |
| Test C6 | Sponge evaporation | 3 | 148 | None | 2·2 | 10 | 362 | 78 | 93 |
| Test C7† | Sponge evaporation | 3 | 148 | None | 2·5 | 11 | 428 | 72 | 85 |
| Test C8 | Sponge evaporation | 3 | 200 | None | 3·2 | 11 | 543 | 82 | 89 |
| Test C9 | Sponge evaporation | 3 | 224 | 0·3 | 6·4 | 24 | 1067 | 62 | 85 |
| Test C10 | Sponge evaporation | 3 | 224 | 0·5 | 3·55 | 21 | 597 | 50 | 89 |
HPV, hydrogen peroxide vapour; RH, relative humidity.
All air temperatures at 21 ± 2°C. All tests conducted with 1 week contact time
Used a set point of 5 ppm.
Humidifier turned off and on every 30 min using the SCADA system.
For the bench-scale tests (using spores of both B. atrophaeus and B. anthracis Ames), the HPV was produced by sparging air through a glass tube fritted at the end (Prism Research Glass, RTP, NC) and immersed in a 1 l Pyrex beaker containing an 8% aqueous solution of H2O2. A small pump was used to bubble air through the sparger (Aquaculture MX-1504). Similar to Test C1 described above, all tests at bench-scale used a target HPV concentration of either 5 or 10 ppm, which was maintained by turning on and off the air pump to the sparger via a feedback loop controlled by a SCADA system. Temperature, RH and HPV concentration data were logged continuously via the SCADA system. Although all of the pilot-scale tests used a week contact time (to focus on experimental variables other than contact time), the contact time was an experimental variable for the bench-scale test programme, and ranged from 8 h to 7 days. Table 2 summarizes of the bench-scale experimental matrix.
Table 2.
Bench-scale test conditions
| Test run |
HPV set point (ppm) |
Average actual HPV (ppm) |
Contact time (days) |
HPV dose (ppm h) |
Average RH (%) |
|---|---|---|---|---|---|
| 1 | 5 | 5·87 | 7 | 986 | 41·7 |
| 2 | 5 | 5·6 | 4 | 538 | 47·3 |
| 3 | 5 | 6·18 | 1 | 148 | 44·9 |
| 4 | 10 | 8·46 | 1 | 203 | 56·7 |
| 5 | 10 | 11·32 | 0·33 | 91 | 49·4 |
HPV, hydrogen peroxide vapour; RH, relative humidity.
All tests conducted with air temperatures at 26 ± 1°C
Recovery of bacterial spores from coupons
At the end of each decontamination test (either pilot-scale or bench-scale), the 18-mm test, procedural blank, and positive control coupons were recovered from the test chambers and sealed containers (for positive controls) and transferred aseptically into empty 50-ml sterile tubes. Bacterial spores were recovered from the coupons according to the methods described by Meyer et al. (2014). Briefly, the coupons in the sample vials were extracted in 10 ml of sterile Phosphate Buffered Saline plus Tween® 20 (PBST; Part number 3563; Sigma Aldrich, St. Louis, MO). The samples were then sonicated for 10 min using an 8510 Branson (Danbury, CT) ultrasonic cleaner at 44 kHz and 250 Watts. The sonication step was immediately followed by two continuous minutes of vortexing to further dislodge any viable spores from the coupons. Each vial was briefly re-vortexed immediately before any solution was withdrawn for analysis. The suspension was then subjected to a five-stage, 10-fold serial dilution. Each dilution (0·1 ml) was plated in triplicate on tryptic soy agar (TSA), spread using sterile cell spreaders (Model COPTS-01; Hardy Diagnostics, Santa Maria, CA) and incubated at 35 ± 2°C for 18–24 h. Plates with 30–300 CFU were enumerated manually or using an automated colony counter (Spiral Biotech Q-Count; Advanced Instruments, Norwood, MA). Any samples below enumerable criteria (30 CFU) on the primary dilution plates were filtered. The filters (0·2 μm; Nalgene Analytical, Thermo Scientific P/N 130-4020, Waltham, MA) were plated onto TSA and incubated at 35 ± 2°C for 18–24 h prior to manual enumeration. The number of CFU ml−1 was then determined by multiplying the average number of colonies per plate by the reciprocal of the dilution.
Recovery and decontamination efficacy calculations
Decontamination efficacy for a particular material was determined by comparing the number of recovered spores from positive control coupons (n = 3 for pilot-scale tests; n = 5 for bench-scale tests) and test coupons (n = 3 for pilot-scale tests; n = 5 for bench-scale tests). That is, efficacy was expressed as log10 reduction (LR) per Eqn (1):
| (1) |
where CFUc is the number of CFU recovered from the positive control coupons and CFUt is the number of CFU recovered from the test coupons. When filter plates had no CFU detected, a value of 1 CFU was inputted, resulting in a log value of 0. Many of the decontamination efficacy results are presented or discussed in terms of whether a 6 LR of the micro-organism population was obtained for a particular material and test condition. The 6 LR benchmark is used since a decontaminant that achieves a LR of 6 or greater (when a 6–7 log challenge is used) for a particular material is considered an effective sporicidal decontaminant (US EPA 2007). We caution, however, that effective decontamination in the laboratory setting may not always transfer to similar efficacy in a field- or full-scale, more realistic setting. Further, a 6 LR still might not be safe for a highly contaminated area. For example, a 6 LR of spores against a spore loading of 8 or 9 log CFU would leave significant remaining viable spores and could potentially present a health hazard.
Statistical analyses
Statistical analyses were performed with sas 9.4 for Windows (SAS Institute Inc., Cary, NC). The null hypothesis testing was conducted at the 5% level of significance. Decontamination efficacies associated with study parameters were compared using one-way analysis of variance (anova) and the Least-Squares Means (LS Means) multiple comparison test. Diffograms were constructed to visualize pair-wise LS means differences. Linear mixed models were considered for assessing fixed and random effects of experimental variables. Interaction effects were as well analysed. The Wilcoxon rank-sum/Exact test and Kruskal–Wallis test were applied for statistical comparisons of groups of non-normal data. The P-value from two-sided (nondirectional) tests were used to test hypotheses. Correlations (Pearson product-moment correlation coefficient, r) were analysed using MS Excel, and only include materials that were common to all tests: carpet, ceiling tile, glass, painted wallboard and laminate.
Results
Pilot-scale tests with Bacillus atrophaeus spores
The results for the fumigation parameter measurements for the 10 decontamination tests conducted in COMMANDER are summarized in Table 1. Five of the tests were conducted using an 8% aqueous solution of H2O2, and the other five tests used a 3% aqueous solution. The average concentration of HPV for each test ranged from 2 to 11 ppm, with the highest HPV levels associated with the 8% aqueous solution (C2–C5). For a given aqueous H2O2 concentration, HPV levels generally increased with greater quantities of solution disseminated. For example, Test C2, which used 164 ml m−3 of 8% solution, resulted in the highest maximum HPV level of 78 ppm. In Test C9, 224 ml m−3 of the 3% aqueous solution was used, resulting in the highest HPV levels for the tests using the 3% solution (e.g. 24 ppm). The use of air exchange or increase in air exchange reduced HPV levels in COMMANDER when compared to similar tests without it, for example, compare C2 to C4; compare C9 to C10. However, in comparing Tests C8 and C9, the use of air exchange is accompanied by a higher HPV level. This unexpected result may be explained in part by an increase in H2O2 solution that was disseminated (In Test C9, we disseminated an additional 24 ml m−3 of solution compared to C8.), or may be due to erroneous measurement of an experimental parameter such as air flow.
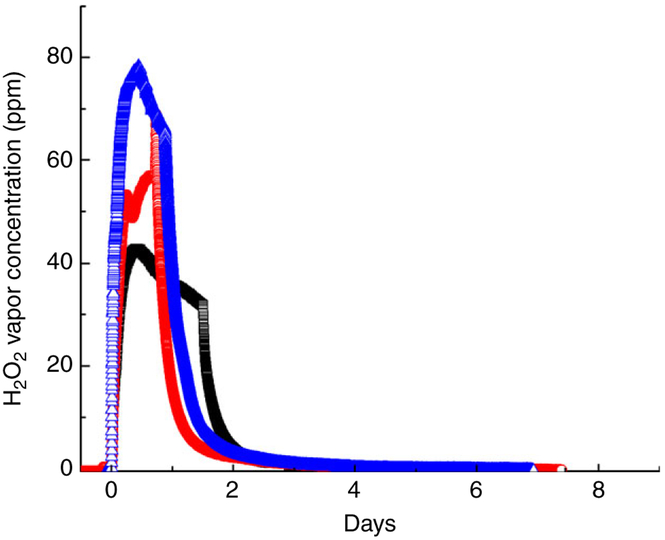
Figure 2 shows the HPV concentration profiles following dispersion of 8% H2O2 solution with the three humidifier types, from tests C2, C3 and C5. The general shape of these concentration profiles was typical of all the tests except C1 and C7. In C1, the HPV level was held to a constant level of 5 ppm for the entire week, and in Test C7, the HPV level fluctuated as the humidifier was turned on and off every 30 min. As illustrated in Fig. 2, the HPV concentration increased to its maximum level (data shown in Table 1) within approx. 12 h, and then gradually decayed back to nondetectable levels of HPV within the week’s contact time. The HPV dose (ppm HPV h) results reported in Table 1 were calculated by integrating the area under these HPV concentration profile curves. Of the three concentration profiles shown in Fig. 2, the ultrasonic humidifier produced the highest HPV dose (Test C2; 1900 ppm h), followed by the sponge evaporator, and then the heated vaporizer.
Figure 2.
Hydrogen peroxide vapour concentration profiles of the different humidifier types. Data are from Tests C2, C3 and C5. Ultrasonic = blue triangles; sponge evaporation = black squares; heated = red circles. [Colour figure can be viewed at wileyonlinelibrary.com]
Similar to the rise in HPV levels, with the start of the humidifiers, the RH levels in the decontamination chamber increased from ambient levels of between 40 and 50% to the maximum levels ranging between 81 and 94%. Air temperatures within the decontamination chamber were consistent throughout the study and averaged 21 ± 2°C.
Overall results and effect of material on efficacy
In Table 3 we present a summary of the decontamination efficacy results for the pilot-scale tests conducted in COMMANDER. The results are summarized by the average LR for each material for each test. At the bottom of Table 3 are the average LR values for each material for all of the pilot-scale tests. Because the concrete material was poorly decontaminated (1·90 average LR), we discontinued this material from further testing. In the place of concrete, we added wood and galvanized metal materials to the test matrix. With the exception of concrete (used only in the first test), all of the materials were decontaminated on average above 6 LR for the COMMANDER tests. The LR results shown in bold in Table 3 indicate that all test coupons for that particular material (3 replicates × 3 chamber locations = 9 total) were completely decontaminated, that is, there were no detectable spores following treatment. The laminate material had the greatest number of tests in which all of its coupons were completely decontaminated (7), while carpet had the fewest number of tests (only 3) in which all of its coupons were completely decontaminated. With the exception of concrete, ceiling tile had the lowest overall average LR (6·31) for the pilot test programme.
Table 3.
Summary of pilot-scale decontamination efficacy results for Bacillus atrophaeus spores
| Test ID | Carpet | Ceiling tile | Unpainted concrete† |
Glass | Painted wallboard |
Laminate | Wood | Galvanized metal |
Avg by test* |
|---|---|---|---|---|---|---|---|---|---|
| Test C1 | 7·04 ± 1·21 | 6·46 ± 0·54 | 1·90 ± 1·10 | 6·45 ± 1·78 | 5·90 ± 0·71 | 6·82 ± 1·27 | 6·53 ± 0·43 | ||
| Test C2 | 7·61 ± 0·00 | 6·77 ± 0·00 | 7·17 ± 0·00 | 7·45 ± 0·00 | 7·54 ± 0·01 | 7·88 ± 0·02 | 7·46 ± 0·00 | 7·31 ± .34 | |
| Test C3 | 7·61 ± 0·00 | 6·66 ± 0 | 7·29 ± 0·07 | 7·63 ± 0·07 | 7·80 ± 0·01 | 7·78 ± 0·00 | 7·35 ± 0·00 | 7·40 ± .45 | |
| Test C4 | 7·50 ± 0·01 | 6·56 ± 0 | 7·48 ± 0·07 | 7·36 ± 0 | 7·46 ± 0 | 7·76 ± 0·02 | 7·43 ± 0 | 7·27 ± .4 | |
| Test C5 | 7·25 ± 0·23 | 6·62 ± 0 | 7·28 ± 0·08 | 7·19 ± 0·01 | 7·54 ± 0 | 7·36 ± 0·31 | 7·47 ± 0 | 7·18 ± .34 | |
| Test C6 | 6·89 ± 0·68 | 4·85 ± 0·41 | 7·74 ± 0 | 7·50 ± 0·07 | 7·13 ± 0·37 | 7·89 ± 0·01 | 6·62 ± 1·48 | 6·82 ± 1·15 | |
| Test C7 | 5·83 ± 1·02 | 5·71 ± 0·92 | 6·70 ± 0·82 | 5·53 ± 1·39 | 7·02 ± 0·76 | 7·62 ± 0·27 | 4·04 ± 2·29 | 6·16 ± .66 | |
| Test C8 | 7·70 ± 0·17 | 6·35 ± 0·48 | 7·19 ± 0·07 | 6·89 ± 0·81 | 7·55 ± 0 | 7·65 ± 0·09 | 6·79 ± 0·98 | 7·14 ± .54 | |
| Test C9 | 6·08 ± 2·13 | 6·64 ± 0·07 | 6·16 ± 1·19 | 6·59 ± 1·01 | 7·30 ± 0 | 7·31 ± 0·06 | 6·12 ± 1·32 | 6·55 ± .49 | |
| Test C10 | 7·75 ± 0 | 6·52 ± 0·25 | 6·76 ± 0·73 | 6·48 ± 0·85 | 7·63 ± 0 | 7·64 ± 0·02 | 5·54 ± 2·02 | 7·03 ± .62 | |
| Avg by material | 7·13 ± 0·62 | 6·31 ± 0·68 | 1·09 ± 1·63 | 7·02 ± 0·50 | 6·85 ± 0·71 | 7·38 ± 0·30 | 7·65 ± 0·19 | 6·45 ± 1·12 |
Results are average of log reductions ± SD on coupons for each of the three locations where coupons were placed: above ceiling tile, on desk and below desk. Log reduction results in bold indicate all test coupons (n = 9; 3 replicates at each location) for that material were completely decontaminated.
Average LR by test calculated using materials common for all tests (carpet, ceiling tile, glass, painted wallboard and laminate).
Unpainted concrete was only included in first test.
Biological indicators (BIs) comprised of Geobacillus stearothermophilus on steel discs were also used in the COMMANDER tests as another tool to assess the efficacy of HPV generated via the humidifiers. Only two out of the 81 BIs used in the overall study exhibited growth following HPV exposure. Further information and detailed results for this additional assay are presented in the Supporting Information.
Effect of HPV levels and quantity of solution disseminated on efficacy
The average LR values across all materials that were common for each test (carpet, ceiling tile, glass, painted wallboard and laminate) are shown in the last column in Table 3, and were all greater than 6·0 for every test (We note that some materials within a particular test may have been decontaminated at an average level <6 LR, while the overall average for all the materials in a test was >6 LR. In addition, replicates of a material placed at a particular location within the chamber may have been decontaminated at a level <6 LR while the overall average for that material may be >6 LR. Indeed, coupons placed at the ceiling location tended to be decontaminated to a lesser degree than the two other locations, and this is discussed in more detail below. Summary data for the average LR values for each material/test/chamber location are provided in Supporting Information.) Tests C1, C6 and C7 each had at least one material which was decontaminated at an average LR level less than 6·0. From this result, we observe that approx. 160 ml m−3 was the minimum amount of 8% solution needed for effective decontamination (>6 LR) for all materials used in our study; similarly, 200 ml m−3 was the minimum amount of the 3% solution needed to effectively decontaminate the materials included in our study. In terms of HPV dose, Test C1 had the highest dose (889 ppm h) in which not all of the materials were decontaminated with a LR >6·0, suggesting that a dose higher than this would be needed for effective decontamination across a range of materials. Test C2 was the only test in which every test coupon for every material was completely decontaminated, and this test also had the highest HPV values (in terms of average and maximum concentration, as well as dose). The average LR value for a test correlated with HPV dose (r = 0·63), but was lesser correlated with maximum HPV (r = 0·48) and average HPV (r = 0·41). The average LR for each test was minimally but negatively correlated with average RH (r = −0·24).
Effect of humidifier type on efficacy
Comparison of the LR results for Tests C2, C3 and C5 could potentially allow one to interpret the effect of humidifier type on decontamination efficacy, since a different humidifier type was used in each of these three tests, all three tests used an 8% solution with similar quantity of the H2O2 solution disseminated (154–164 ml m−3), with no air exchange. While many of the materials from these three tests were completely decontaminated, and all of the materials were effectively decontaminated, significance testing found that the decontamination efficacy of the heated vaporizer (irrespective of material) was statistically lower than the other two types of humidifiers. (As mentioned previously, the heated vaporizer (Test C5) also resulted in the lowest HPV dose of the three tests being compared.) We do acknowledge, however, that the maximum difference in efficacy between the humidifier types was less than 0·5 LR, and that the heated vaporizer was only tested once. No other significant differences in decontamination efficiency by type of humidifier were found. For this reason, in all of the subsequent tests using the 3% solution, we used the sponge evaporator humidifier, which had a higher reservoir capacity and thus allowed us to disseminate greater amounts of the aqueous solution.
Effect of test coupon location on efficacy
In Table 4, we show decontamination efficacy results as a function of the test coupon location in the COMMANDER test chamber. The results are shown in terms of the fraction (per cent) of the number of samples in which no viable spores were detected, as well as fraction of instances when the LR <6·0. Coupons located on the desk were easiest to decontaminate, as indicated by having the highest percentage (75%) of samples with no detectable spores. Coupons located above the ceiling tiles were the most difficult to decontaminate, exemplified by having the lowest percentage of occurrences in which a material had no detectable spores (52%), as well as by having the most number of occurrences in which the decontamination efficacy was not effective (LR <6·0). Statistical analysis confirmed that the overall efficacy for the coupons located above the ceiling tiles is statistically lower (α = 0·05) than the other two locations.
Table 4.
Effect of location of decontamination efficacy in COMMANDER
| Above ceiling |
On desk | Under desk |
|
|---|---|---|---|
| Per cent of occurrences in which all three replicates for a material in a given test had no detectable spores | 52 | 75 | 72 |
| Per cent of occurrences in which the average LR for a material in a given test was <6.0 | 32 | 23 | 17 |
Small chamber results using spores of Bacillus anthracis Ames and Bacillus atrophaeus
The decontamination efficacy results for the laboratory-scale tests using both B. anthracis Ames and B. atrophaeus spores are summarized in Table 5. Five tests were conducted with both species, with average actual HPV levels ranging from approx. 5 to 11 ppm; contact times ranged from 8 h to 1 week, and actual RH levels ranged from 45 to 57%; refer to Table 2 for actual fumigation conditions.
Table 5.
Summary of bench-scale decontamination efficacy results
| Carpet |
Ceiling tile |
Wood |
Glass |
Painted wallboard |
Laminate |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test ID | Ames | Bg | Ames | Bg | Ames | Bg | Ames | Bg | Ames | Bg | Ames | Bg |
| 1 | 7·33 ± 0 | 7·42 ± 0 | 7·25 ± 0 | 7·48 ± 0 | 7·09 ± 0 | 7·47 ± 0 | 6·35 ± 0 | 7·07 ± 0·41 | 7·13 ± 0 | 7·45 ± 0 | 7·05 ± 0·4 | 6·29 ± 1·26 |
| 2 | 6·53 ± 0·49 | 6·28 ± 1·0 | 7·18 ± 0 | 6·74 ± 0·57 | 07·24 ± 0 | 6·50 ± 1·0 | 7·21 ± 0 | 7·65 ± 0·17 | 7·13 ± 0·13 | 6·59 ± 0·51 | NA | 6·98 ± 0·69 |
| 3 | 2·28 ± 0·19 | 1·88 ± 0·44 | 6·75 ± 0·76 | 2·48 ± 0·69 | 5·80 ± 1·74 | 2·29 ± 0·55 | 7·02 ± 0 | 2·74 ± 0·75 | 5·18 ± 1·93 | 2·15 ± 0·4 | 6·48 ± 0 | 2·53 ± 0·48 |
| 4 | 4·89 ± 1·01 | 6·96 ± 0·77 | 7·37 ± 0 | 6·96 ± 0·63 | 7·28 ± 0 | 7·12 ± 0·68 | 7·63 ± 0 | 7·53 ± 0·23 | 6·85 ± 1·88 | 6·12 ± 0·91 | 7·51 ± 0 | 6·83 ± 1·09 |
| 5 | 2·90 ± 0·05 | 0·79 ± 0·16 | 4·25 ± 1·30 | 1·17 ± 0·19 | 5·83 ± 1·64 | 1·33 ± 0·19 | 5·11 ± 2·32 | 1·68 ± 0·33 | 3·15 ± 0·29 | 3·02 ± 0·4 | 6·20 ± 2·01 | 2·58 ± 0·31 |
Results are presented as average LR ± SD, with values in bold indicating complete inactivation. Ames refers to Bacillus anthracis Ames; Bg refers to Bacillus globigii aka B. atrophaeus.
In the first three tests, we used a target HPV concentration of 5 ppm, but varied the contact time to assess the effect of this parameter. In Test 1, with a 1-week contact time, nearly every material, for both species, was completely decontaminated. After reducing the contact time to 4 days (Test 2), efficacy remained high, with greater than 6 LR for both species and material. In Test 3, using a target concentration of 5 ppm HPV and 1 day contact time, B. anthracis spores were inactivated at a LR >6·0 for three of the six materials. But maintaining the 1-day contact time and raising the target HPV level to 10 ppm (Test 4), decontamination efficacy was significantly improved compared to Test 3, for all materials for both species. In particular, with an actual average HPV concentration of 8·5 ppm held for 24 h, we were able to achieve over 6 LR in B. anthracis spores on all materials except carpet (average LR for this material was 4·89). With Test 5, the actual HPV level was 11·32 ppm, and with a contact time of 8 h, this resulted in the lowest HPV dose of the bench-scale tests, at approx. 91 ppm h. Correspondingly, the LR results for Test 5 were generally the lowest for the bench-scale tests, with the majority of LR values less than 5·0.
Excluding tests in which one or both species were completely inactivated on all replicates for a particular material (e.g. this occurred for every material in Test 1 except laminate), the LR values were all higher for B. anthracis compared to B. atrophaeus with the exception of the carpet material in Test 4. Comparing the decontamination efficacy results for the two species for the two tests in which the kill was incomplete (Tests 3 and 5) allows us to more readily analyse statistical differences. In these two tests, statistical analyses showed that the LR values for the materials inoculated with B. atrophaeus spores were significantly less than for B. anthracis Ames spores. In the tests where there was sufficient HPV dosing (Tests 1, 2 and 4), that is, the HPV treatment was effective in most cases, there was no significant difference in efficacy between the two species.
Statistical comparisons of the effect of material on efficacy were also conducted for Tests 3 and 5, in which fractionated kill was observed. With respect to the Ames strain, decontamination efficacy was significantly lower for carpet compared to the rest of the materials. Wallboard was the next most difficult material to decontaminate for B. anthracis Ames: the painted wallboard LR values were not significantly different compared to ceiling tile, but were significantly lower than the rest of the materials. With respect to B. atrophaeus, carpet, ceiling tile and wood, were significantly more difficult to decontaminate compared to glass, laminate, and wallboard.
Comparing B. atrophaeus efficacy results for Test 1 of the bench-scale tests and Test C1 for the pilot-scale tests allows us to confirm any differences that may have arisen due to differences in test venue or scale, since both tests were conducted at constant 5 ppm HPV for 1 week. The materials in common for both these tests were carpet, ceiling tile, glass, painted wallboard and laminate. In Test 1 of the bench-scale tests, four of the five materials (carpet, ceiling tile, glass and wallboard) were completely decontaminated of B. atrophaeus, while none of the materials in pilot-scale Test C1 were completely decontaminated. Nevertheless, statistical comparisons provide evidence to suggest that both test environments were equally effective for all materials, with the exception that ceiling tile and painted wallboard were significantly more difficult to decontaminate at the pilot-scale. That said, these minor differences in efficacy between test venues may be due to differences in the venues’ HPV dissemination techniques, or due to differences in temperature. For example, the average temperature for testing at the bench-scale was 26°C, while the average temperature of the pilot-scale tests was 21 °C.
Discussion
Several studies have demonstrated the use of HPV for inactivating virulent bacterial spores from species such as B. anthracis and Clostridium difficile (Johnston et al. 2005; Rogers et al. 2005; Rastogi et al. 2009; Lawley et al. 2010). However, these studies and the actual use of HPV in practice typically require sophisticated and expensive equipment to generate the HPV, and usually at relatively high levels (200–500 ppm). In contrast, our study demonstrated that generating relatively low levels of HPV with easy to use equipment and readily available H2O2 solutions is an effective and inexpensive technique for inactivating B. anthracis spores on a number of materials. Average HPV levels of 5–10 ppm, coupled with contact times between 4 and 7 days, were shown to be effective in inactivating B. anthracis and B. atrophaeus spores at levels greater than 6 LR for all of the materials tested except for concrete. Studies by Meyer et al. (2014) and Baron et al. (2007) provided initial evidence suggesting that desorption of HPV from materials results in the production of low levels of HPV over extended time periods, and leads to inactivation of spores. Our robust test programme and research, through the use of several materials and other experimental variables, builds on and corroborates these studies. We are not aware of any other peer reviewed scientific literature reporting the use of such low levels of HPV for bacterial spore inactivation.
We have also demonstrated in pilot-scale experiments that simply disseminating aqueous solutions of H2O2 via COTS humidifiers, without control of the HPV concentration, is an effective decontamination technique. This approach is effective provided that a sufficient quantity of solution is disseminated as vapour and/or a high enough dose of HPV is obtained, coupled with sufficient contact time. For example, 200 ml m−3 was the minimum amount of 3% H2O2 solution found to be effective (>6 LR) on the all materials tested, while a minimum of approx. 160 ml m−3 of 8% solution was effective on all materials – with both tests using a 7-day contact time. While we did not vary contact time for the pilot-scale tests using humidifiers (all tests were conducted with a 7-day contact time), most likely similar decontamination efficacy results would have been obtained had we used a shorter contact time such as 4 days, consistent with the small chamber tests. In addition, Fig. 2 shows that 99% of the HPV dose is obtained within 4 days, further indication that a full week contact time may not have been needed. Relative to the HPV dose, the results suggest that a dose of at least 1000 ppm h HPV would be effective for a range of materials, under the conditions tested in our experiments.
We also found that the three types of COTS humidifiers we tested (ultrasonic, heated vaporizer, and sponge evaporation) were generally similarly effective in decontamination at the conditions we tested them, for example, using an 8% aqueous solution. We do note, however, that when we compare the results for Tests C2, C3 and C5, in which the three different types of humidifiers were used with similar amounts of 8% solution, the heated vaporizer was slightly (but statistically significant) less efficacious. In comparing these same three tests, the HPV concentration (in terms of average, maximum and dose) for the ultrasonic type (Test C2) was the highest among the three tests, while the heated vaporizer resulted in the lowest HPV concentrations. Although we do not have enough data to definitively conclude that the ultrasonic device is more effective in producing the HPV, further research may be warranted to investigate this matter. Additional experiments at less than ideal conditions may also produce additional data to better characterize or elucidate differences in efficacy by the type of humidifier.
With the exception of unpainted concrete, low levels of HPV were predominantly effective on all the materials we tested. While there was some variation in decontamination efficacy among some of the materials, as would be expected, the variation was relatively minor. For example, ceiling tile and galvanized metal were slightly more difficult to decontaminate in pilot test experiments, a result consistent with Rogers et al. (2005). Inactivation of B. atrophaeus on ceiling tile, carpet and wood was slightly but significantly more difficult compared to the other materials in the laboratory-scale tests.
With respect to unpainted concrete being the most difficult to decontaminate, this result is consistent with Rastogi et al. (2009), who found that the LR on concrete via HPV was less than 1·0 under variable spore loadings. Rogers et al. (2005) did achieve effective inactivation of B. anthracis spores on concrete using HPV, but the concrete was painted. The low efficacy of HPV on unpainted concrete may be due to the high demand this material places on HPV concentration (US EPA, 2010). Although it is conceivable that HPV would be efficacious on concrete provided a sufficiently high enough concentration and contact time is allowed, finding these required conditions was beyond the scope of this study.
While most materials were effectively decontaminated, decontamination of the materials placed above the ceiling tile panels was not as effective as those placed at other locations. This is most likely due to insufficient mixing of the heavier-than-air HPV. Full removal of the ceiling panels, as well as raising the humidifier outlet, may be warranted to facilitate exposure at all elevations within a room.
One purpose of this study was to compare the small-scale decontamination results between the virulent B. anthracis (Ames) and B. atrophaeus, to confirm the latter micro-organism as an appropriate surrogate in the pilot-scale COMMANDER experiments, as well as future decontamination studies. For spore inactivation studies, the nonpathogenic substitute organism should possess resistance to the decontamination treatment equivalent to or greater than the virulent species (Wood et al. 2011). Our results show that B. atrophaeus may be a suitable surrogate for B. anthracis Ames in HPV decontamination studies. In this study, there was only one case (material/test combination) in which B. atrophaeus was inactivated to a significantly greater degree than B. anthracis. We acknowledge that each species was inoculated on coupons using a different technique, and that this difference in spore inoculation method may confound comparison of efficacy between the two species. The B. anthracis spores were deposited onto coupons using a liquid inoculation method, while B. atrophaeus spores were deposited onto coupons as an aerosol via the use of an MDI. Ryan et al. (2014) found that the spore inoculation method did affect decontamination efficacy results, but the effect varied by material and decontaminant. Nevertheless, our B. anthracis Ames and B. atrophaeus decontamination efficacy results agree well with Rogers et al. (2005), who showed that with the exception of just a few instances, B. subtilis was inactivated to a lesser degree than B. anthracis Ames when exposed to HPV on a number of materials. While we were unable to find any study in the literature specifically comparing the resistance of B. anthracis Ames to B. atrophaeus (aka B. subtilis var Niger) upon exposure to HPV, B. atrophaeus is phenotypically similar to B. subtilis except for the production of pigment (Sella et al. 2014).
From the bench-scale experiments in which contact time was varied, we found that 4 days was the minimum contact time needed for effective decontamination with HPV at an average level of 5 ppm. Based on this result and the fact that all but one material was effectively decontaminated at 10 ppm HPV with 1-day exposure, this would suggest that a contact time of between 2 and 3 days should be sufficient for effective decontamination at 10 ppm HPV at the bench-scale.
In summary, the use of relatively low levels of HPV coupled with extended contact times (e.g. 4–7 days) represents a new, straightforward methodology for the decontamination of many types of surfaces contaminated with B. anthracis spores. The approach can be implemented by holding HPV levels constant at 5–10 ppm, or by simply disseminating the vapour with COTS humidifiers using readily available (e.g. 3–8% concentration) aqueous solutions of H2O2. This is a practical, safe and economical decontamination technique useful for when financial resources may be limited, and when the volume being decontaminated is not overly large and can be left undisturbed for a few days. We also foresee this easy to use decontamination method applied to the inactivation of other pathogenic micro-organisms that have already been demonstrated to be susceptible to HPV, although further research is needed to confirm required contact times for the different types of materials and biological agents. In conclusion, we caution that effective decontamination in the laboratory setting may not always transfer to similar efficacy in a field- or full-scale, more realistic setting. Therefore, further testing of this low-level HPV decontamination approach, using a larger, more realistic test bed, is recommended.
Supplementary Material
Figure S1 Photos of humidifiers.
Table S1 Biological indicator test results.
Table S2 Decontamination efficacy results for the large test chamber, average ± SD log reduction values, by test number/material/chamber location.
Acknowledgements
The authors gratefully acknowledge the statistical analyses provided by Patrick Pancras and the dedicated microbiological laboratory support provided by Christina Slone. Expert technical assistance of LTC (retired) Laura Burton is also gratefully acknowledged for experimental preparation and processing the B. atrophaeus samples at the ECBC facility.
Footnotes
Disclaimer
The US Environmental Protection Agency (EPA) through its Office of Research and Development funded and directed the research described herein under contract EP-C-09-027 with ARCADIS, Inc. It has been subjected to the Agency’s review and has been approved for publication. Note that approval does not signify that the contents necessarily reflect the views of the Agency. Mention of trade names, products or services does not convey official EPA approval, endorsement or recommendation.
Conflict of Interest
The authors declare no conflict of interest.
References
- Barbut F, Menuet D, Verachten M and Girou E (2009) Comparison of the efficacy of a hydrogen peroxide drymist disinfection system and sodium hypochlorite solution for eradication of Clostridium difficile spores. Infect Control Hosp Epidemiol 30, 507–514. [DOI] [PubMed] [Google Scholar]
- Baron PA, Estill CF, Beard JK, Hein MJ and Larsen L (2007) Bacterial endospore inactivation caused by outgassing of vapourous hydrogen peroxide from polymethyl methacrylate (Plexiglas). Lett Appl Microbiol 45, 485–490. [DOI] [PubMed] [Google Scholar]
- Brown GS, Betty RG, Brockmann JE, Lucero DA, Souza CA, Walsh KS, Boucher RM, Tezak M et al. (2007) Evaluation of a wipe surface sample method for collection of Bacillus spores from nonporous surfaces. Appl Environ Microbiol 73, 706–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canter DA (2005) Remediating anthrax-contaminated sites: learning from the past to protect the future. Chem Health Saf 12, 13–19. [Google Scholar]
- Fichet G, Antloga K, Comoy E, Deslys JP and McDonnell G (2007) Prion inactivation using a new gaseous hydrogen peroxide sterilisation process. J Hosp Infect 67, 278–286. [DOI] [PubMed] [Google Scholar]
- French GL, Otter JA, Shannon KP, Adams NMT, Watling D and Parks MJ (2004) Tackling contamination of the hospital environment by methicillin-resistant Staphylococcus aureus (MRSA): a comparison between conventional terminal cleaning and hydrogen peroxide vapour decontamination. J Hosp Infect 57, 31–37. [DOI] [PubMed] [Google Scholar]
- Heckert RA, Best M, Jordan LT, Dulac GC, Eddington DL and Sterritt WG (1997) Efficacy of vaporized hydrogen peroxide against exotic animal viruses. Appl Environ Microbiol 63, 3916–3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston MD, Lawson S and Otter JA (2005) Evaluation of hydrogen peroxide vapour as a method for the decontamination of surfaces contaminated with Clostridium botulinum spores. J Microbiol Methods 60, 403–411. [DOI] [PubMed] [Google Scholar]
- Kahnert A, Seiler P, Stein M, Aze B, McDonnell G and Kaufmann SHE (2005) Decontamination with vaporized hydrogen peroxide is effective against Mycobacterium tuberculosis. Lett Appl Microbiol 40, 448–452. [DOI] [PubMed] [Google Scholar]
- Klapes NA and Vesley D (1990) Vapor-phase hydrogen peroxide as a surface decontaminant and sterilant. Appl Environ Microbiol 56, 503–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause J, McDonnell G and Riedesel H (2001) Biodecontamination of animal rooms and heat-sensitive equipment with vaporized hydrogen peroxide. Contemp Top Lab Anim Sci 40, 18–21. [PubMed] [Google Scholar]
- Lawley TD, Clare S, Deakin LJ, Goulding D, Yen JL, Raisen C and Brandt C (2010) Use of purified Clostridium difficile spores to facilitate evaluation of health care disinfection regimens. Appl Environ Microbiol 76, 6895–6900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SD, Ryan SP and Snyder EG (2011) Development of an aerosol surface inoculation method for Bacillus spores. Appl Environ Microbiol 77, 1638–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik DJ, Shaw CM, Rielly CD and Shama G (2013) The inactivation of Bacillus subtilis spores at low concentrations of hydrogen peroxide vapour. J Food Eng 114, 391–396. [Google Scholar]
- McDonnell G and Russell AD (1999) Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev 12, 147–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer KM, Calfee MW, Wood JP, Mickelsen L, Attwood B, Clayton M, Touati A and Delafield R (2014) Fumigation of a laboratory-scale HVAC system with hydrogen peroxide for decontamination following a biological contamination incident. J Appl Microbiol 116, 533–541. [DOI] [PubMed] [Google Scholar]
- Rastogi VK, Wallace L, Smith LS, Ryan SP and Martin B (2009) Quantitative method to determine sporicidal decontamination of building surfaces by gaseous fumigants, and issues related to laboratory-scale studies. Appl Environ Microbiol 75, 3688–3694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers JV, Sabourin CL, Choi YW, Richter WR, Rudnicki DC, Riggs KB, Taylor ML and Chang J (2005) Decontamination assessment of Bacillus anthracis, Bacillus subtilis, and Geobacillus stearothermophilus spores on indoor surfaces using a hydrogen peroxide gas generator. J Appl Microbiol 99, 739–748. [DOI] [PubMed] [Google Scholar]
- Rogers JV, Richter WR, Shaw MQ and Choi YW (2008) Vapour-phase hydrogen peroxide inactivates Yersinia pestis dried on polymers, steel, and glass surfaces. Lett Appl Microbiol 47, 279–285. [DOI] [PubMed] [Google Scholar]
- Ryan SP, Lee SD, Calfee MW, Wood JP, McDonald S, Clayton M, Griffin-Gatchalian N, Touati A et al. (2014) Effect of inoculation method on the determination of decontamination effiacy against Bacillus spores. World J Microbiol Biotechnol 30, 2609–2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sella SRBR, Vandenberghe LPS and Soccol CR (2014) Bacillus atrophaeus: main characteristics and biotechnological applications-a review. Crit Rev Biotechnol 1–13. [DOI] [PubMed] [Google Scholar]
- U.S. Environmental Protection Agency (2005) Compilation of available data on building decontamination alternatives. Washington, DC: EPA Report 600/R-05/036, March 2005. [Google Scholar]
- U.S. Environmental Protection Agency (2007) Transmittal of meeting minutes of the FIFRA scientfic advisory panel meeting held July 17–18, 2007 on guidance on test methods for demonstrating the efficacy of antimicrobial products for inactivating Bacillus anthracis spores on environmental surfaces. http://archive.epa.gov/scipoly/sap/meetings/web/pdffjuly2007_sap_finalreport.pdf (Accessed from the World Wide Web on February 22, 2016).
- U.S. Environmental Protection Agency (2010) Material Demand Studies: Materials Sorption of Vaporized Hydrogen Peroxide. Washington, DC: US EPA Report EPA/600/R-10/002, May 2010. [Google Scholar]
- U.S. Environmental Protection Agency (2014) Decontamination of a mock office using chlorine dioxide gas. Washington, DC: US EPA, report EPA/600/R-14/208, August 2014. [Google Scholar]
- Wood JP, Choi YW, Rogers JV, Kelly TJ, Riggs KB and Willenberg ZJ (2011) Efficacy of liquid spray decontaminants for inactivation of Bacillus anthracis spores on building and outdoor materials. J Appl Microbiol 110, 1262–1273. [DOI] [PubMed] [Google Scholar]
- Wood JP, Calfee MW, Clayton M, Griffin-Gatchalian N, Touati A and Egler K (2013) Evaluation of peracetic acid fog for the inactivation of Bacillus anthracis spore surrogates in a large decontamination chamber. J Hazard Mater 250, 61–67. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Photos of humidifiers.
Table S1 Biological indicator test results.
Table S2 Decontamination efficacy results for the large test chamber, average ± SD log reduction values, by test number/material/chamber location.