Abstract
Background:
Given the potential hidden nature of medial meniscal ramp lesions and the controversy regarding treatment, it is important to understand the current trends regarding the identification and treatment strategies of meniscal ramp lesions by the leading surgeons and educators in the field of sports medicine.
Purpose:
To better understand the current trends in orthopaedic surgery regarding arthroscopic identification and treatment of medial meniscal ramp lesions at the time of anterior cruciate ligament (ACL) surgery.
Study Design:
Cross-sectional study.
Methods:
An electronic questionnaire was sent in a blinded fashion to 91 directors of orthopaedic sports medicine fellowship training programs in the United States. Participants’ email addresses were obtained through the American Orthopaedic Society for Sports Medicine directory of current fellowship program directors. Inclusion criteria were only those surgeons who currently performed ACL reconstruction surgery. Exclusion criteria were those surgeons who did not perform ACL reconstruction or who chose to opt out of the survey.
Results:
Overall, 19 surgeons opted out of the survey; 36 responded from the remaining 72 surveys (50%). The majority (n = 31, 86%) reported routinely checking for a medial meniscal ramp lesion via inspection of the posteromedial meniscocapsular junction during an ACL reconstruction. The most common repair technique cited was all-inside (n = 24, 66.7%), followed by inside-out (n = 8, 22.2%). Three (8%) surgeons indicated that they did not repair meniscal ramp lesions. Regarding surgical treatment (repair vs no treatment), the majority reported using the extent of the tear (89%; partial vs full thickness) and the stability of the tear upon probing (81%) as the main criteria for intraoperative decision making. Nineteen (52.8%) surgeons required a mean time of <15 minutes for meniscal ramp repair; 16 surgeons (44.4%), 15 to 30 minutes; and 1 surgeon (2.8%), 30 to 45 minutes.
Conclusion:
This study provides insight regarding meniscal ramp tear identification, treatment, and repair strategies from the fellowship directors of sports medicine orthopaedic surgery in the United States. Such information may be useful for current orthopaedic surgeons to advance their practice according to the current trends surrounding ACL reconstruction and medial meniscal ramp repair.
Keywords: ramp lesion, medial meniscus, anterior cruciate ligament reconstruction, survey
Meniscal ramp lesions are becoming increasingly recognized. Ramp lesions have been described as tears at the posterior meniscocapsular junction and/or tears of the posterior meniscotibial ligament, and they have a reported incidence of 16% to 40% of all anterior cruciate ligament (ACL) tears.3,9,13,14 Based on their location, these lesions may be arthroscopically “hidden” during normal anterior viewing; thus, an accessory posteromedial portal is necessary to confirm or deny their presence. In addition, there is controversy regarding identification strategies and surgical treatment options (repair versus no treatment). Some authors have advocated for the surgical repair of all meniscal ramp lesions at the time of ACL reconstruction, owing to an increased risk of persistent instability and potential ACL reconstruction graft failure when not treated.4,5,11,15 However, given the vascularization of the capsule and the red-red zone of the meniscus,1,2 some clinical studies have cited the potential for these tears to heal without surgical treatment.6,10 Therefore, the purpose of this research survey was to better understand the current trends in orthopaedic surgery regarding arthroscopic identification and treatment of medial meniscal ramp lesions at the time of ACL surgery.
Methods
Questionnaire Development
A questionnaire was electronically sent in a blinded fashion to 91 directors of orthopaedic sports medicine fellowship training programs in the United States (Table 1). Participants’ email addresses were obtained through the American Orthopaedic Society for Sports Medicine directory of current fellowship program directors. A cover letter that accompanied the questionnaire stated the purpose of the questionnaire and ensured anonymity. All survey participants had the opportunity to decline the questionnaire. Inclusion criteria included only those surgeons who currently performed ACL reconstruction surgery. Exclusion criteria were those surgeons who did not perform ACL reconstruction or who chose to opt out of the survey. The survey was sent out and responses were collected from January 2018 to July 2018. We developed the questionnaire according to previous trends in the literature regarding meniscal ramp lesions and by expert opinion and knowledge from years of clinical practice. This study was deemed exempt from approval by an institutional review board.
TABLE 1.
Survey Questionnairea
|
aQuestions assessed the surgeon’s expertise in preoperative diagnosis, intraoperative identification, and treatment strategies of medial meniscal ramp lesions at the time of ACL surgery. Respondents’ answers are provided in the form of overall percentages in parentheses next to the corresponding answers. ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.
Statistical Analysis
Data were prospectively collected via an online survey tool (www.surveymonkey.com). Data were extracted from the online survey database and summarized. Standard descriptive statistics were performed.
Results
Overall, 19 surgeons opted out of the survey; 36 responded from the remaining 72 surveys (50%). A total of 14 (38.9%) surgeons reported that their recognition of meniscal ramp lesions began ≥7 years ago; 8 surgeons (22.2%), 5 to 6 years; 12 surgeons (33.3%), 2 to 4 years; and 2 surgeons (5.6%), 1 year ago. The majority (n = 31, 86%) indicated routinely checking for a medial meniscal ramp lesion during an ACL reconstruction via inspection of the posteromedial meniscocapsular junction. The most common inspection strategy cited for evaluation of a ramp tear was the modified Gillquist view (transnotch approach; n = 24, 67%). Three (8%) surgeons reported the use of an accessory posteromedial portal during evaluation of a ramp lesion.
Regarding diagnosis, 11% did not preoperatively diagnose ramp lesions, while 89% used magnetic resonance imaging (MRI) for diagnosis, with 56% identifying a posteromedial tibial bone bruise as a secondary sign of a ramp lesion. Eight (22.2%) surgeons reported that MRI was “rarely” accurate in diagnosing medial meniscal ramp lesions, as compared with 12 (33.3%) and 16 (44.4%) who indicated that MRI was “sometimes” accurate and “often” accurate, respectively. Twenty (55.5%) surgeons cited the preoperative use of physical examination findings as an indicator for potential medial meniscal ramp lesion. The most common physical examination findings reported were a grade III pivot shift (n = 9, 25%) and a grade III Lachman test (n = 8, 22.2%).
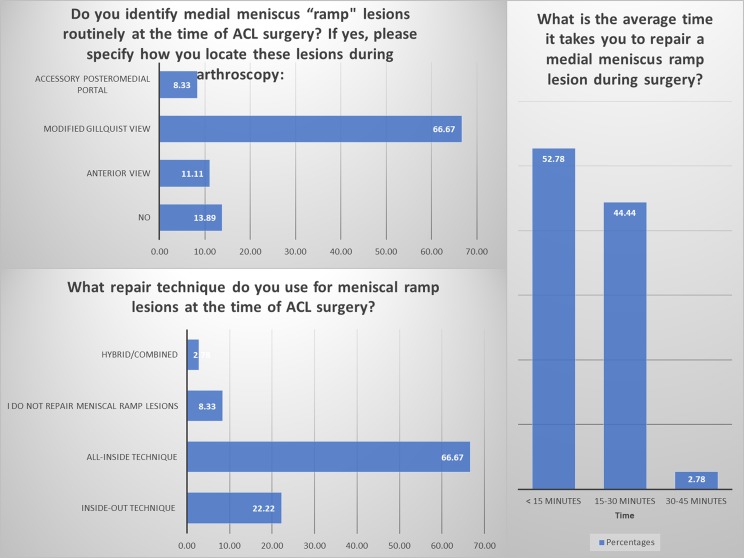
The most common meniscal ramp repair technique cited was all-inside (n = 24, 66.7%), followed by inside-out (n = 8, 22.2%). Three (8%) surgeons reported that they did not repair meniscal ramp lesions, and 1 (2.7%) surgeon cited a hybrid meniscal repair technique. Regarding surgical treatment (repair versus no treatment), the majority of surgeons reported using the extent of the tear (89%; partial versus full thickness) and the stability of tear upon probing (81%) as the main criteria for intraoperative decision making. Nine surgeons (25%) cited involvement of the meniscotibial ligament as a criterion for meniscal repair, and 21 (58.3%) surgeons indicated size of the tear (ie, >2.5 or <2.5 cm in length) as a decision-making criterion. A total of 19 (52.8%) surgeons reported requiring a mean time of <15 minutes for meniscal ramp repair, 16 surgeons (44.4%) needed 15 to 30 minutes, and 1 surgeon (2.8%) needed 30 to 45 minutes. No surgeon (0%) needed ≥60 minutes (Figure 1).
Figure 1.
Survey responses of the orthopaedic sports medicine fellowship directors in the United States (N = 36) regarding identification, treatment, and time of repair for medial meniscal ramp lesions. ACL, anterior cruciate ligament.
The majority of surgeons (n = 22, 61.1%) reported routine assessment of intraoperative knee stability (ie, Lachman testing) following ramp repair: 12 surgeons (33.3%) cited a subjective difference in knee stability prior to ACL reconstruction with a ramp repair, while 10 surgeons (27.8%) did not notice a subjective difference in knee stability. The most common prescribed weightbearing status following ACL reconstruction and meniscal ramp repair was weightbearing as tolerated with the use of crutches for 2 to 4 weeks (n = 23, 64%). The most common prescribed return-to-play timeline following primary ACL reconstruction and concomitant medial meniscal ramp repair was 7 to 8 months (n = 13, 36%) (Table 2).
TABLE 2.
Mean Return-to-Play Timeline Reported by Orthopaedic Sports Medicine Fellowship Directors in the United States (N = 36)a
| 5-6 mo | 6-7 mo | 7-8 mo | ≥9 mo | |
|---|---|---|---|---|
| “What is your prescribed return-to-play timeline following a primary ACL reconstruction and medial meniscal ramp repair?” | 2 (6) | 12 (33) | 13 (36) | 9 (25) |
aResults are reported as n (%). ACL, anterior cruciate ligament.
Discussion
This study reports the preferences and treatment strategies of the current US orthopaedic fellowship directors in the field of sports medicine. Specifically, the majority of surgeons surveyed reported that they routinely identify and repair meniscal ramp lesions at time of ACL surgery (86%), use an all-inside repair technique (67%), require <15 minutes for repair (53%), and allow their patients to return to full activities at postoperative 7 to 8 months (36%). These guidelines may be helpful for orthopaedic surgeons and may lead to established criteria for the treatment of ACL tears with concomitant medial meniscal ramp lesions.
In the current survey, the modified Gillquist view (transnotch, advancing the arthroscope medial to the posterior cruciate ligament) was the most common utilized approach to identify a potential ramp lesion. However, previous authors have advocated for the use of an accessory posteromedial portal to both visualize and repair ramp lesions.12,14,16 In a study evaluating the diagnostic accuracy of adding a posteromedial portal for evaluation of ramp lesions, Sonnery-Cottet et al14 documented a high rate (17%) of missed meniscocapsular tears before adding a posteromedial portal. However, in the current survey, only 8% of surgeons indicated the use of an accessory posteromedial portal during evaluation of a ramp lesion. Thus, the reported necessity of this accessory portal was not common in clinical practice by the orthopaedic sports medicine fellowship directors in the United States. Consequently, an accessory posteromedial portal may not be necessary for visualization with the previously established modified Gillquist view.7
The most common meniscal ramp repair technique reported in this survey was all-inside (67%), followed by inside-out (22%). Previous literature has described various meniscal ramp repair techniques; however, clinical outcomes have been published only for all-inside ramp repair techniques.8,16,17 Thaunat et al16 documented good outcomes following combined ACL reconstruction and all-inside meniscal ramp repair, with a 9% clinical failure rate. Liu et al10 evaluated outcomes comparing all-inside versus no repair (trephination only) among patients who underwent ACL reconstruction with stable meniscal ramp lesions. These authors cited no significant differences between the repair and no-repair groups and no significant differences in meniscal healing rates. These reports support the potential for stable meniscal ramp lesions to heal without surgical repair; however, only 8% of our survey respondents indicated that they do not repair meniscal ramp lesions. Thus, the current trend (92%) by US orthopaedic sports medicine fellowship directors supports medial meniscal ramp repair.
The most commonly prescribed postoperative rehabilitation protocols after ACL reconstruction and meniscal ramp repair were weightbearing as tolerated with the use of crutches for 2 to 4 weeks (64%) and allowing patients to return to full activity at postoperative 7 to 8 months (36%). Thaunat et al16 reported full weightbearing by week 3 and return to full activities by 9 months following combined ACL reconstruction and meniscal ramp repair. Thus, the cited rehabilitation programs by the orthopaedic sports medicine fellowship directors in the United States are consistent with previous literature.
This study has limitations inherent to those of a survey questionnaire. As such, the subjective reports and common trends of the survey respondents cannot be validated with evidence-based recommendations, although these practices may be adopted into future research studies for validation. In addition, there was a relatively low response rate for the orthopaedic sports medicine fellowship directors. This may have introduced bias into the results, which should thus be interpreted with caution.
Conclusion
This survey provides insight regarding meniscal ramp tear identification, treatment, and repair strategies from the fellowship directors of sports medicine orthopaedic surgery in the United States. This information may be useful for current orthopaedic surgeons to advance their practice according to the current trends surrounding ACL reconstruction and medial meniscal ramp repair.
Footnotes
One or more of the authors has declared the following potential conflict of interest and source of funding: L.E. receives research support from Arthrex, Biomet, Smith & Nephew, and Health Southeast Norway and royalties from Arthrex and Smith & Nephew. R.F.L. receives educational support from Arthrex; is a consultant for Arthrex, Ossur, and Smith & Nephew; receives royalties from Arthrex, Ossur, and Smith & Nephew; is a paid speaker/presenter for Arthrex and Smith & Nephew; and has received hospitality payments from Arthrex and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Vail Valley Medical Center Institutional Review Board (protocol No. 2017-42).
References
- 1. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90–95. [DOI] [PubMed] [Google Scholar]
- 2. Barber-Westin SD, Noyes FR. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30(1):134–146. [DOI] [PubMed] [Google Scholar]
- 3. DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 4. DePhillipo NN, Cinque ME, Kennedy NI, et al. Inside-out repair of meniscal ramp lesions. Arthrosc Tech. 2017;6(4):e1315–e1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46(10):2422–2431. [DOI] [PubMed] [Google Scholar]
- 6. Duchman KR, Westermann RW, Spindler KP, et al. The fate of meniscus tears left in situ at the time of anterior cruciate ligament reconstruction: a 6-year follow-up study from the MOON Cohort. Am J Sports Med. 2015;43(11):2688–2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gillquist J, Hagberg G, Oretorp N. Arthroscopic visualization of the posteromedial compartment of the knee joint. Orthop Clin North Am. 1979;10(3):545–547. [PubMed] [Google Scholar]
- 8. Li WP, Chen Z, Song B, Yang R, Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27(1):56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. [DOI] [PubMed] [Google Scholar]
- 10. Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45(5):1004–1011. [DOI] [PubMed] [Google Scholar]
- 11. Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. [DOI] [PubMed] [Google Scholar]
- 12. Peltier A, Lording TD, Lustig S, Servien E, Maubisson L, Neyret P. Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy. 2015;31(4):691–698. [DOI] [PubMed] [Google Scholar]
- 13. Seil R, Mouton C, Coquay J, et al. Ramp lesions associated with ACL injuries are more likely to be present in contact injuries and complete ACL tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1080–1085. [DOI] [PubMed] [Google Scholar]
- 14. Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42(4):921–926. [DOI] [PubMed] [Google Scholar]
- 15. Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–408. [DOI] [PubMed] [Google Scholar]
- 16. Thaunat M, Jan N, Fayard JM, et al. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32(11):2269–2277. [DOI] [PubMed] [Google Scholar]
- 17. Tiftikci U, Serbest S. Does the location of placement of meniscal sutures have a clinical effect in the all-inside repair of meniscocapsular tears? J Orthop Surg Res. 2017;12(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]