Abstract
Background:
Recent studies have described surgical techniques to increase the hamstring graft diameter for anterior cruciate ligament reconstruction (ACLR), particularly for 5-strand hamstring (5HS) autografts.
Purpose:
To review the literature examining the biomechanical and clinical outcomes of 5HS autografts for ACLR.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A systematic review using PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines was performed by searching PubMed, Embase, and the Cochrane Library for studies reporting the biomechanical and clinical outcomes of 5HS autografts. All English-language literature published from 2012 to 2018 that reported the biomechanical properties of 5HS grafts and/or clinical outcomes after ACLR with 5HS autografts with a minimum 1-year follow-up was reviewed by 2 independent reviewers. Graft diameter, stiffness, displacement, strength, failure rates, anteroposterior knee laxity, and patient-reported outcome scores were collected. The study methodology was evaluated using the modified Coleman Methodology Score.
Results:
Two biomechanical and 3 clinical studies (1 with level 2 evidence, 2 with level 3 evidence) were included. The biomechanical studies compared the results of fourteen 4-strand hamstring (4HS) and fourteen 5HS graft specimens for ACLR (ovine grafts, n = 12; cadaveric grafts, n = 16) and found no significant differences in ultimate load, stiffness, displacement, and stress relaxation (P > .05), likely attributed to insufficient incorporation of the fifth strand. The mean 5HS cadaveric graft diameter (8.2 mm) was significantly greater than that of 4HS grafts (6.8 mm) (P = .002), whereas the mean ovine graft diameters were not significantly different (4HS, 5.2 mm; 5HS, 5.3 mm) (P > .05). Two clinical studies compared the outcomes after ACLR of 53 patients with a 4HS autograft versus 62 patients with a 5HS autograft, while 1 clinical study reported the outcomes of 25 patients after ACLR with a 5HS autograft (mean age, 28.7 years; mean follow-up, 24.8 months). The overall mean diameter for 4HS and 5HS autografts was 8.4 and 9.1 mm, respectively. There was no significant difference in failure rates between 4HS and 5HS autografts (P = .82). None of the comparative studies reported significant differences in any clinical outcomes (P > .05 for all).
Conclusion:
The available literature on traditional 4HS and 5HS autografts for ACLR is limited. Of the available data, clinical and biomechanical studies suggest no difference in outcomes after ACLR with either graft construct. Additional research is needed to determine whether creating a 5HS graft is beneficial.
Keywords: anterior cruciate ligament, 5-strand hamstring autograft, graft diameter
Anterior cruciate ligament (ACL) ruptures are becoming increasingly more common, and the ACL is the most frequently reconstructed ligament of the knee.21 Current ACL reconstruction (ACLR) techniques vary in the graft used to reconstruct the native ACL, including bone–patellar tendon–bone (BTB) autografts, hamstring autografts, allografts, and hybrid autografts-allografts. Of the 2 most predominantly used grafts (BTB autograft and hamstring autograft), multiple authors have indicated decreased complications using hamstring autografts for ACLR, as they may decrease the risk of anterior knee donor site morbidity that is more prevalent with the use of BTB autografts.10–12,15,23,26,28,29 However, the variability in the cross-sectional diameter of these grafts has been a topic of concern. Increasing the cross-sectional area of an ACL graft has recently been linked to decreased rates of revision as well as improved patient-reported outcome (PRO) scores.1,2,21,22,24,25 Recent studies have determined that the likelihood of revision is drastically reduced if the graft is greater than 8 mm in diameter,2,9,21,22,31 although the quality of these studies is limited, particularly in determining the magnitude to which the graft diameter affects outcomes.
The graft diameter of a standard 4-strand hamstring (4HS) autograft has been reported to vary between 6 and 9 mm.2 Attempts to increase the diameter of grafts that are intrinsically smaller than 8 mm have led to the development of a 5-strand hamstring (5HS) autograft technique. The purpose of this study was to systematically review the literature to determine the biomechanical advantages and clinical outcomes after ACLR using 5HS autografts.
Methods
This systematic review was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using a PRISMA checklist. Two independent reviewers (J.-R.H.S., D.A.H.) searched PubMed, Embase, and the Cochrane Library up to August 6, 2018. The following search phrases were used: “five-strand hamstring graft” and “5-strand hamstring graft.” After the removal of duplicates, a total of 37 studies were reviewed by title and/or abstract to determine eligibility based on the inclusion criteria. Studies selected met the following inclusion criteria: they were published in the English language, they reported the biomechanical strength and properties of 5HS autografts and/or clinical outcomes after primary ACLR using 5HS autografts, and they had a minimum 1-year follow-up. Exclusion criteria included the following: studies not reporting clinical or biomechanical outcomes, use of BTB grafts or hybrid autografts-allografts, systematic reviews, scientific abstracts, and studies reporting techniques. Disparities in eligible studies were resolved by discussion between the 2 reviewers.
Reporting Outcomes
Outcomes assessed included failure rates, anteroposterior (AP) laxity, biomechanical properties, and PRO scores. The biomechanical properties assessed included load to failure, stress relaxation, stiffness, and displacement. PRO measures included the Lysholm Knee Scoring Scale,20 the Knee injury and Osteoarthritis Outcome Score (KOOS),27 the Physical Component Summary (PCS) and Mental Component Summary (MCS) of the 36-Item Short Form Health Survey (SF-36),34 and the subjective International Knee Documentation Committee (IKDC) form.14
Study Methodology Assessment
The quality of study methodology was evaluated using the modified Coleman Methodology Score (MCMS), based on a scaled potential score ranging from 0 to 100.8 Scores ranging from 85-100 are excellent, 70-84 are good, 55-69 are fair, and <55 are poor.
Statistical Analysis
An overall weighted mean was calculated for numerical demographic data (age and follow-up) and PRO scores. A chi-square test was performed for categorical variables, where P < .05 indicated statistical significance.
Results
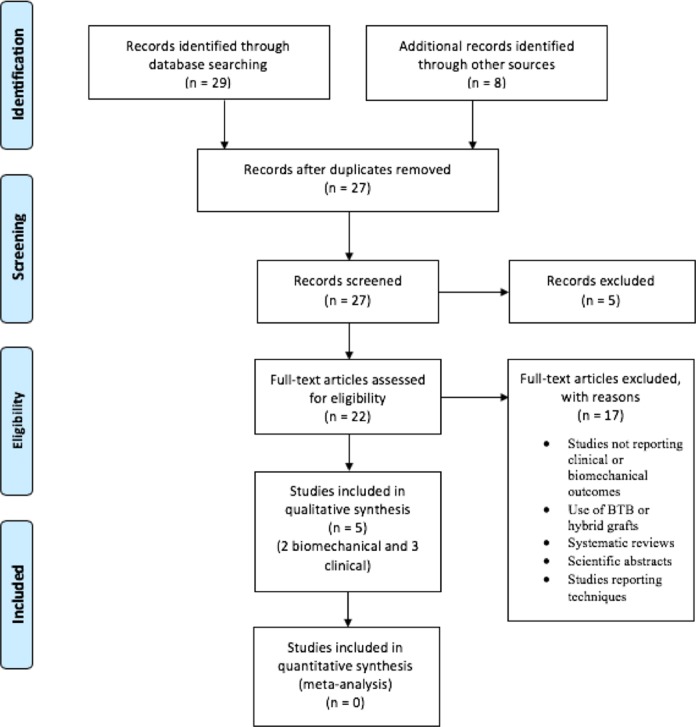
Five studies,3,6,18,19,33 including 2 biomechanical studies3,33 and 3 clinical studies6,18,19 (1 with evidence level 2, 2 with evidence level 3), met inclusion and exclusion criteria (Figure 1). Two studies6,19 compared the clinical outcomes of 4HS and 5HS autografts for ACLR, while 1 study18 reported the clinical outcomes of 5HS autografts. In one of the comparative clinical studies,19 the 5HS cohort was duplicated from the authors’ previous study.18 The 2 biomechanical studies3,33 compared the biomechanical results of 4HS grafts with 5HS grafts.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Patient Demographics
A total of 115 patients were included in this systematic review, including 53 patients undergoing ACLR with a 4HS autograft and 62 patients undergoing ACLR with a 5HS autograft. The overall mean patient age at the time of surgery was 28.7 years (4HS, 29.5 years; 5HS, 27.6 years). Additionally, a total of 28 hamstring graft specimens (4-strand, n = 14; 5-strand, n = 14) subjected to biomechanical analysis were included (Table 1).
TABLE 1.
Included Studiesa
| Clinical Outcomes | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Follow-up, n/N (%) | Male/Female, n | Mean Age, y | Mean Follow-up, mo | Mean Graft Diameter, mm | ||||||||||
| 4HS | 5HS | 4HS | 5HS | 4HS | 5HS | 4HS | 5HS | 4HS | 5HS | ||||||
| Calvo et al6 (2017) | 33/33 (100.0) | 37/37 (100.0) | NR | NR | 29.7 | 30.2 | 32.2 | 30.4 | 8.50 | 9.20 | |||||
| Krishna et al18 (2018) | — | 25/30 (80.3) | — | 19/6 | — | 25.6 | — | 17.8 | — | 9.06 | |||||
| Krishna et al19 (2018) | 20/21 (95.2) | 25/27 (92.6) | 19/1 | 19/6 | 29.2 | 25.6 | 16.8 | 17.8 | 8.13 | 9.06 | |||||
| Total | 53/54 (98.1) | 87/96 (90.1) | 19/1 | 57/13 | 29.5 | 27.6 | 26.4 | 23.2 | 8.36 | 9.12 | |||||
| Biomechanical Results | |||||||||||||||
| Study | Graft Material | No. of Specimens | Graft Testing Method | Suture Method | |||||||||||
| 4HS | 5HS | ||||||||||||||
| Broadhead et al3 (2017) | Ovine flexor tendon | 6 | 6 | Uniaxial electromechanical load system | Suspensory fixation | ||||||||||
| Vaillant et al33 (2017) | Cadaveric gracilis and semitendinosus tendon | 8 | 8 | DVRT | Krackow interlocking | ||||||||||
| Total | — | 14 | 14 | — | — | ||||||||||
Associated Injuries
Two clinical studies18,19 included patients treated with concomitant injuries, including medial and lateral meniscal tears and chondral injuries. Calvo et al6 excluded patients with any concomitant injuries, and all 3 clinical studies6,18,19 excluded patients with multiligament knee injuries.
Surgical Technique
All 3 clinical studies6,18,19 created standard anteromedial and anterolateral arthroscopic portals adjacent to the patellar tendon, and diagnostic arthroscopic surgery was performed to assess the ACL tear and other concurrent injuries. The semitendinosus and gracilis tendons were harvested using a closed tendon stripper.6,18,19 After debridement of residual muscle tissue, all 3 studies measured the tendon diameters using a sizing block. Graft diameter was defined as the smallest diameter lumen that the entire graft could pass through smoothly.18,19 Preliminary sizing of the 4HS graft was performed to determine if the graft was sufficient in diameter. If the graft was less than 8 mm in diameter, a 5HS graft was prepared. Two of the studies18,19 indicated a minimum length of 24 cm and 16 cm for the semitendinosus and gracilis tendons, respectively, to prepare the 5HS graft. The remaining study6 indicated a minimum length of 21 cm for the semitendinosus tendon. When minimum lengths were not achieved, the standard 4HS graft was prepared.6,18,19
One study6 prepared the 5HS graft by preparing both ends of the semitendinosus graft with FiberWire (Arthrex). Then, the semitendinosus tendon was tripled, creating 3 strands of equal length, and sutured with FiberWire under tension from pulling the 2 previous sutures. Next, 5 mm of the thinner end of the semitendinosus graft was passed over the tripled graft, and the gracilis graft was doubled over the semitendinosus and sutured in the apex of the graft with an absorbable suture. The remaining studies18,19 prepared the 5HS graft by placing a whipstitch at the end of the gracilis tendon with nonabsorbable sutures. A whipstitch was also placed at the distal free end of the semitendinosus tendon. The semitendinosus tendon was then measured and marked to identify 3 equal segments, and the graft was folded such that the proximal free end reached the junction between the proximal two-thirds and distal one-third of the tendon. This end was whipstitched to the body of the tendon, while the free ends of the nonabsorbable suture were tied over the looped end of the graft. A second nonabsorbable suture was then passed around the free looped segment of the semitendinosus graft. A nonabsorbable suture was next placed around the doubled gracilis tendon graft and around the sutured segment of the semitendinosus graft, and a second nonabsorbable suture was then passed around the free looped segment of the semitendinosus graft to form the 5HS graft. All studies6,18,19 prepared the tibial and femoral tunnels with a cannulated drill. The size of the femoral and tibial tunnels corresponded to the diameter of the grafts. In all 3 studies,6,18,19 the graft was fixed at the femoral and tibial tunnels via interference screw fixation.
Biomechanical Specimen Testing
One biomechanical study3 used ovine flexor tendon split grafts to create 5-strand and 4-strand graft constructs. A longitudinal incision was made along the posterior aspect of the sheep’s hindlimb, and the skin and fat were removed to display the flexor digitorum superficialis and gastrocnemius tendons. The fascia was then dissected from the tendons, and any tendons presenting defects were discarded. The tendons were fixed at both ends with clamps and split along the center of the tendon at 1-cm intervals, producing 2 parts for use per tendon. The flexor tendon split grafts were marked at 3 cm from each end, and whipstitches were placed 0.5 cm apart. Excess tendon was removed from the ends of the graft. The 5-strand construct was made by folding the flexor digitorum superficialis tendon grafts 3 times while folding the gastrocnemius tendon in half. The 4-strand construct was made by folding both the superficial flexor and the gastrocnemius tendons in half. Suspensory fixation was used to test both constructs.3
The other biomechanical study33 used cadaveric lower extremities to create 4HS and 5HS grafts. Semitendinosus and gracilis tendons were harvested with a closed tendon stripper, producing grafts of 180 mm in length, and the surrounding muscle tissues were removed. The remaining length of the semitendinosus was used as the fifth strand in the 5HS graft. Locking sutures were placed at both ends of the graft. Preparation of the 4HS graft was conducted in a standard fashion by passing the 4 strands through the cortical button loop. For the 5HS graft, one end of the fifth strand was secured to the loop with suture and reinforced with a 2-loop Krackow stitch. The remaining strands were placed through the cortical button loop in a standard fashion, creating a 5HS graft. All sutures were Krackow interlocking sutures.
Study Methodology Assessment
Table 2 shows the MCMS scores from the 3 included clinical studies, all of which achieved fair scores.6,18,19
TABLE 2.
Modified Coleman Methodology Score in Clinical Studies
| Study | Scorea |
|---|---|
| Calvo et al6 (2017) | 64 |
| Krishna et al18 (2018) | 58 |
| Krishna et al19 (2018) | 61 |
| Mean ± SD | 61 ± 3 |
a85-100 = excellent, 70-84 = good, 55-69 = fair, <55 = poor.
Clinical Outcomes
Failure
One study6 defined clinical failure as magnetic resonance imaging–diagnosed ACL reruptures. The remaining 2 studies18,19 did not clearly define clinical failure. Two studies6,19 indicated that a total of 7.0% of patients experienced reruptures of the ACL (4HS, 7.5%; 5HS, 6.5%) (Table 3). There was no significant difference in failure rates between 4HS and 5HS grafts (P = .82).
TABLE 3.
Failures in Clinical Studiesa
| Study | Graft Failure | |
|---|---|---|
| 4HS | 5HS | |
| Calvo et al6 (2017) | 3/33 (9.1) | 2/37 (5.4) |
| Krishna et al18 (2018) | — | NR |
| Krishna et al19 (2018) | 1/20 (5.0) | 2/25 (8.0) |
| Total | 4/53 (7.5) | 4/62 (6.5) |
aData are reported as No. of failures/total No. of patients in group (%). 4HS, 4-strand hamstring; 5HS, 5-strand hamstring; NR, not reported.
AP Knee Laxity
One study6 measured the mean postoperative AP knee laxity using a KT-1000 arthrometer. This study found no significant difference in postoperative AP knee laxity between 4HS (1.45 mm) and 5HS autografts (2.10 mm) (P = .20).
PRO Scores
One study6 reported mean postoperative subjective IKDC scores preoperatively and postoperatively (Table 4). All 3 studies6,18,19 reported preoperative and postoperative Lysholm scores (Table 4). Two studies18,19 also reported KOOS subscores (Table 5) and PCS and MCS scores of the SF-36 (Table 4) both preoperatively and postoperatively. One study19 noted that there was a significant improvement from baseline scores in both the 5HS and the 4HS graft groups on the Lysholm scale (P < .001 for both), KOOS Symptoms (P = .042 and P = .001, respectively), KOOS Pain (P = .035 and P < .001, respectively), KOOS Activities of Daily Living (P = .003 for both), KOOS Sports (P < .001 for both), KOOS Quality of Life (P = .001 for both), and SF-36 PCS (P = .001 and P < .001, respectively).
TABLE 4.
Patient-Reported Outcome Scoresa
| Study | IKDC | Lysholm | SF-36 PCS | SF-36 MCS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4HS | 5HS | P | 4HS | 5HS | P | 4HS | 5HS | P | 4HS | 5HS | P | |
| Preoperative | ||||||||||||
| Calvo et al6 (2017) | 63.1 | 61.0 | .62 | 61.8 | 59.1 | .75 | NR | NR | — | NR | NR | — |
| Krishna et al18 (2018) | — | NR | — | — | 74.0 | — | — | 48.8 | — | — | 51.3 | — |
| Krishna et al19 (2018) | NR | NR | — | 70.5 ± 14.5 | 72.6 ± 16.4 | .48 | 44.4 ± 6.3 | 47.4 ± 7.3 | .14 | 53.9 ± 5.3 | 50.3 ± 9.5 | .24 |
| Total | 63.1 | 61.0 | .62 | 70.5 | 73.3 | .62 | 44.4 | 96.2 | .14 | 53.9 | 50.8 | .24 |
| Postoperative | ||||||||||||
| Calvo et al6 (2017) | 91.0 | 96.8 | .18 | 93.3 | 97.1 | .79 | NR | NR | — | NR | NR | — |
| Krishna et al18 (2018) | — | NR | — | — | 95.0 | — | — | 53.9 | — | — | 55.8 | — |
| Krishna et al19 (2018) | NR | NR | — | 88.5 ± 10.5 | 90.4 ± 8.1 | .58 | 53.9 ± 3.8 | 52.7 ± 4.8 | .59 | 56.3 ± 5.9 | 52.0 ± 10.6 | .21 |
| Total | 91.0 | 96.8 | .18 | 91.5 | 94.6 | .69 | 53.9 | 53.3 | .59 | 56.3 | 53.9 | .21 |
aData are reported as mean ± SD (when available), with “total” as the weighted mean. 4HS, 4-strand hamstring; 5HS, 5-strand hamstring; IKDC, International Knee Documentation Committee; MCS, Mental Component Summary; NR, not reported; PCS, Physical Component Summary; SF-36, 36-Item Short Form Health Survey.
TABLE 5.
KOOS Subscoresa
| Study | KOOS Symptoms | KOOS Pain | KOOS Activities of Daily Living | KOOS Sports | KOOS Quality of Life | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4HS | 5HS | P | 4HS | 5HS | P | 4HS | 5HS | P | 4HS | 5HS | P | 4HS | 5HS | P | |
| Preoperative | |||||||||||||||
| Calvo et al6 (2017) | NR | NR | — | NR | NR | — | NR | NR | — | NR | NR | — | NR | NR | — |
| Krishna et al18 (2018) | — | 89.3 | — | — | 88.9 | — | — | 92.7 | — | — | 45.0 | — | — | 43.7 | — |
| Krishna et al19 (2018) | 76.1 ± 13.3 | 79.7 ± 17.7 | .38 | 79.2 ± 14.4 | 86.7 ± 14.0 | .07 | 87.4 ± 9.9 | 88.1 ± 11.6 | .54 | 33.3 ± 28.7 | 45.2 ± 28.1 | .13 | 49.7 ± 16.4 | 47.5 ± 19.8 | .31 |
| Total | 76.1 | 84.5 | .38 | 70.2 | 87.8 | .07 | 87.4 | 90.4 | .54 | 33.3 | 45.1 | .13 | 49.7 | 45.6 | .31 |
| Postoperative | |||||||||||||||
| Calvo et al6 (2017) | NR | NR | — | NR | NR | — | NR | NR | — | NR | NR | — | NR | NR | — |
| Krishna et al18 (2018) | — | 92.9 | — | — | 97.2 | — | — | 98.5 | — | — | 85.0 | — | — | 68.8 | — |
| Krishna et al19 (2018) | 89.1 ± 10.7 | 88.1 ± 11.9 | .83 | 93.6 ± 6.5 | 93.6 ± 9.3 | .46 | 96.0 ± 5.4 | 96.5 ± 8.7 | .52 | 83.5 ± 17.1 | 85.4 ± 14.3 | .69 | 69.1 ± 13.2 | 66.8 ± 21.6 | .99 |
| Total | 89.1 | 90.5 | .83 | 93.6 | 95.4 | .46 | 96.0 | 97.5 | .52 | 83.5 | 85.2 | .69 | 69.1 | 67.8 | .99 |
aData are reported as mean ± SD (when available), with “total” as the weighted mean. 4HS, 4-strand hamstring; 5HS, 5-strand hamstring; KOOS, Knee injury and Osteoarthritis Outcome Score; NR, not reported.
Biomechanical Results
One biomechanical study3 compared the mean failure load and mean stress relaxation between the 4-strand and 5-strand constructs. Failure included graft ruptures as well as failure at the EndoButton fixation site. Mean failure was measured using the uniaxial electromechanical load system (MTS). Stress relaxation was defined as the observed decrease in stress while the graft was held at constant strain. Broadhead et al3 indicated no statistical differences in the mean failure load or the mean stress relaxation (P = .46 and P = .59, respectively). The second biomechanical study33 compared graft displacement between 4-strand and 5-strand grafts (6.8 and 7.7 mm, respectively) and noted no significant differences between grafts (P = .29). Displacement was defined as the distance from the initial to final position at failure of the graft. It is important to note that this may be because of the lack of incorporation of the fifth strand.
Both biomechanical studies3,33 reported the mean stiffness of both graft constructs and indicated no significant differences between 4-strand and 5-strand grafts. One of the studies3 measured stiffness as the slope of the stress-strain curve, with a steeper slope indicating a stiffer construct and indicated no significant difference between constructs. This study also included a bimodal measurement of stiffness, initial and secondary, and indicated no significant difference in either outcome between constructs (P = .30 and P = .80, respectively). The other study33 measured stiffness as the slope of the load versus displacement curve, with a steeper slope indicating a stiffer construct. Similarly, there were no statistically significant differences in stiffness between 4-strand and 5-strand constructs (160.5 and 162.5 N/mm, respectively; P = .82).
Discussion
The results of this systematic review suggest that, at a mean follow-up of 30.2 months, patients undergoing primary ACLR using 5HS autografts do not demonstrate significantly different rates of clinical success and PRO scores when compared with patients undergoing ACLR using 4HS autografts greater than 8 mm in diameter.6,18,19 Additionally, no significant difference in failure rates between patients undergoing ACLR using 5HS autografts and patients undergoing ACLR using 4HS autografts greater than 8 mm in diameter were observed. Moreover, failure rates for ACLR using 5HS autografts were similar to those using 4HS autografts between 7.5 and 8 mm in diameter, as indicated by Magnussen et al,21 in which revision ACLR was necessary in 6.5% of these cases. However, the 5HS autografts demonstrated lower failure rates in comparison with the results of ACLR using 4HS autografts less than 7.5 mm in diameter, for which revision was necessary in 13.6% of these cases.21 Additionally, 1 biomechanical study3 indicated no significant difference in the mean failure load, mean stress relaxation, or mean stiffness between 4HS and 5HS constructs. Similarly, Vaillant et al33 indicated no significant difference in graft displacement and mean stiffness between 4HS and 5HS constructs. These results suggest that 5HS grafts do not significantly differ in their biomechanical properties when compared with 4HS grafts.3,33
Previous biomechanical studies2,13 have indicated a relationship between increased load to failure with increasing graft size. Additionally, clinical studies9,21,22,30 have demonstrated a reduced revision risk, as well as improved PRO scores, with an increased graft diameter. From a sample of 256 patients, Magnussen et al21 indicated that revision was required for 1.7% of grafts greater than 8 mm, 6.5% of grafts between 7.5 and 8 mm, and 13.6% of grafts smaller than 7 mm in diameter. Furthermore, Boniello et al2 indicated a similar increase in strength as the graft diameter increased. They demonstrated that, with 1 mm–diameter increments, the greatest strength gain was seen with the 6- to 7-mm increment (38% increase in strength); however, the lowest strength gain was seen with the 8- to 9-mm increment (12% increase in strength). The methodologies used in the present study differ from those used by Boniello et al,2 as they did not solely use 5HS grafts to increase the graft diameter but rather used 2-strand to 6-strand hamstring grafts to create a sample of constructs 6, 7, 8, or 9 mm in diameter. However, their results do suggest a gradual decrease in the effect of graft diameter on graft strength as the diameter increases. This suggests that the most drastic improvements in biomechanical strength of a hamstring autograft occur before the graft’s diameter surpasses the 8-mm mark, with less substantial improvement occurring thereafter. Similarly, Magnussen et al21 indicated that once a hamstring autograft surpasses 8 mm in diameter, there is a significant decrease in the risk of revision.
Because of the variability of standard 4HS grafts, the 5HS graft technique has been implemented to achieve grafts greater than 8 mm in diameter, and Krishna et al17 indicated that the 5HS technique is successful in providing a graft exceeding 8 mm in diameter to patients who would otherwise fail to reach this minimum. While the use of a hybrid autograft-allograft is an option for increasing the graft diameter,16 the use of a 5HS autograft eliminates the need for allograft augmentation. Further, Burrus et al5 indicated that hybrid autografts-allografts fail or become structurally compromised at a higher rate compared with complete hamstring autografts greater than 7.5 mm in diameter.
Although previous biomechanical studies2,13 indicated greater strength with increasing graft diameter, the 2 biomechanical studies included in this systematic review3,33 demonstrated no significant differences in load to failure, stress relaxation, displacement, or stiffness when compared with the 4HS grafts of a smaller diameter. However, it is noted33 that the possible reason behind this discrepancy is the ineffective incorporation of the additional strand into the graft construct because of the fixation technique employed. It has been suggested that the use of suspensory fixation techniques, rather than interference fixation techniques, is less successful in incorporating the fifth strand in a 5HS graft construct.18,33
The clinical studies included in this systematic review were limited to procedures that exclusively used interference fixation techniques.6,18,19 It has been noted that the 5HS graft technique does increase the graft diameter and therefore has the potential to increase the overall success in grafts that would otherwise be less than 8 mm in diameter. Tutkus et al32 suggested that 5HS grafts have a diameter that is significantly larger than 8 mm in 98.4% of cases. The remaining 1.6% of 5HS grafts less than 8 mm in diameter all occurred within female cases.32 However, results of the current systematic review indicate no significant differences in clinical outcomes between 5HS autografts and 4HS autografts that are already greater than 8 mm in diameter. Calvo et al6 reported that there was no statistically significant difference in rerupture rates between 4HS grafts greater than 8 mm in diameter and 5HS grafts. Additionally, all included clinical studies indicated no statistically significant differences among PRO scores between 4HS grafts greater than 8 mm in diameter and 5HS grafts.6,18,19
Limitations
The strengths of this study include a comprehensive systematic review performed by 2 independent reviewers. Additionally, there was an overall high follow-up rate across all clinical studies. The limitations of this study should also be noted. First, the small number of clinical studies included limits the overall sample size. While this small sample size may limit the conclusion that no significant difference exists between 5HS autografts and 4HS autografts greater than 8 mm in diameter, sample size analyses to assess minimal differences in outcomes and obtain a statistical power of at least 80% were performed in 1 of the biomechanical studies33 and the 2 comparative clinical studies.6,19 Second, a patient cohort from 1 study18 was duplicated in a separate study19 by the same authors to represent the 5HS graft group. This again limits the overall sample size. Third, there were very few female cases included in the study groups. Female patients are most likely to have grafts that do not reach 8 mm in diameter, and these are cases in which the 5HS graft technique would be most useful.22 Fourth, the overall mean follow-up time was relatively short at 30.2 months, and 2 of the studies18,19 included a mean follow-up of 17.3 and 17.8 months.
Moreover, 1 clinical study6 did not report preoperative PRO scores. Additionally, no direct comparison between the 5HS autografts that were greater than 8 mm in diameter and smaller 4HS autografts that were less than 8 mm was available. Further, the surgical techniques in the included clinical studies6,18,19 are only applicable when using interference screw fixation; because cortical suspensory fixation devices are the most commonly used ACL femoral graft fixation technique, this would be inapplicable for the majority of hamstring ACLRs performed worldwide.4,7
With respect to the biomechanical studies, limitations included the use of different graft specimens between studies, with 1 study3 using nonhuman tendons, as well as the small sample size of both studies. Broadhead et al3 claimed that ovine flexor tendon split grafts have been validated in the in vivo setting for the evaluation of ACL endoligamentous and tunnel remodeling. However, more research is needed to validate ovine flexor tendon split grafts as an accurate simulation for the biomechanical performance of human tendons. Furthermore, the limitations in the current data regarding the relationship between graft diameter and outcomes should be addressed. Although indications have been shown that graft size appears to affect revision rates and PRO scores, the magnitude of the effect is still unclear.
Future research should be directed toward comparing 5HS autografts to hybrid autografts-allografts as well as a direct comparison of 5HS grafts with 4HS grafts that are less than 8 mm in diameter. Because 5HS grafts show minimal differences when compared with 4HS grafts larger than 8 mm, and previous studies2,9,21,22,31 have suggested significant improvements in failure rates when 4HS grafts are greater than 8 mm in diameter, 5HS grafts may also provide decreased failure rates in comparison with 4HS grafts less than 8 mm. A study directly comparing failure rates and clinical outcomes between 4HS grafts less than 8 mm in diameter with 5HS grafts may generate a more clinically significant result. Also, it will be interesting to see the results of future studies, especially those performing ACLR using femoral cortical suspensory devices, including more patients and longer term follow-up outcomes. Finally, future biomechanical studies implementing interference screw fixation would be helpful to determine if there is a biomechanical advantage to 5HS grafts.
Conclusion
The available literature on traditional 4HS and 5HS autografts for ACLR is limited. Given the small overall sample sizes and relatively low quality of the published studies available for this review, we were unable to confirm a statistically significant difference in outcomes between 4HS and 5HS autografts for ACLR with either graft construct. Additional research is needed to determine if creating a 5HS graft is beneficial, especially compared with cases in which the traditional 4HS graft is less than 8 mm in diameter.
Footnotes
One or more of the authors has declared the following potential conflicts of interest or source of funding: A.F.V. is a consultant for ArthroCare and Stryker, is a paid speaker/presenter for Arthrex and Ceterix, has received educational support from Smith & Nephew, and has received hospitality payments from Steris. R.M.F. has received educational support from Arthrex, Medwest, and Smith & Nephew and hospitality payments from Stryker. J.T.B. is a consultant for DJ Orthopedics, Encore Medical, Smith & Nephew, and Stryker; has received research support from Stryker; has received fellowship funding from Mitek; and receives royalties from Shukla Medical. E.C.M. is a consultant for Biomet and DePuy; has received research support from Biomet, Mitek, Smith & Nephew, and Stryker; and receives royalties from Biomet and Elsevier. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. [DOI] [PubMed] [Google Scholar]
- 2. Boniello MR, Schwingler PM, Bonner JM, Robinson SP, Cotter A, Bonner KF. Impact of hamstring graft diameter on tendon strength: a biomechanical study. Arthroscopy. 2015;31(6):1084–1090. [DOI] [PubMed] [Google Scholar]
- 3. Broadhead ML, Singla AA, Bertollo N, Broe D, Walsh WR. A biomechanical comparison of 4-strand and 5-strand anterior cruciate ligament graft constructs. Orthop Rev (Pavia). 2017;9(1):6989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brown CH., Jr Editorial commentary: how to increase hamstring tendon graft size for anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(9):2641–2646. [DOI] [PubMed] [Google Scholar]
- 5. Burrus MT, Werner BC, Crow AJ, et al. Increased failure rates after anterior cruciate ligament reconstruction with soft-tissue autograft-allograft hybrid grafts. Arthroscopy. 2015;31(12):2342–2351. [DOI] [PubMed] [Google Scholar]
- 6. Calvo R, Figueroa D, Figueroa F, et al. Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: clinical outcomes with a minimum 2-year follow-up. Arthroscopy. 2017;33(5):1007–1013. [DOI] [PubMed] [Google Scholar]
- 7. Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A. An international survey on anterior cruciate ligament reconstruction practices. Int Orthop. 2013;37(2):201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2–11. [DOI] [PubMed] [Google Scholar]
- 9. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 10. Cooley VJ, Deffner KT, Rosenberg TD. Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy. 2001;17(8):795–800. [DOI] [PubMed] [Google Scholar]
- 11. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. [DOI] [PubMed] [Google Scholar]
- 12. Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21(7):791–803. [DOI] [PubMed] [Google Scholar]
- 13. Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81(4):549–557. [DOI] [PubMed] [Google Scholar]
- 14. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 15. Jansson KA, Linko E, Sandelin J, Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(1):12–18. [DOI] [PubMed] [Google Scholar]
- 16. Kraeutler MJ, Kim SH, Brown CC, et al. Clinical outcomes following primary anterior cruciate ligament reconstruction with hamstring autograft versus planned hybrid graft. J Knee Surg. 2018;31(9):827–833. [DOI] [PubMed] [Google Scholar]
- 17. Krishna L, Panjwani T, Mok YR, Lin Wong FK, Singh A, Toh SJ. Use of the 5-strand hamstring autograft technique in increasing graft size in anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(9):2633–2640. [DOI] [PubMed] [Google Scholar]
- 18. Krishna L, Tan XY, Thangaraja A, Wong FKL. Five-strand hamstring autograft in primary anterior cruciate ligament reconstruction [published online April 4, 2018]. J Knee Surg. doi:10.1055/s-0038-1641175 [DOI] [PubMed] [Google Scholar]
- 19. Krishna L, Tan XY, Wong FKL, Toh SJ. A 5-strand hamstring autograft achieves outcomes comparable to those of a 4-strand hamstring autograft with a graft diameter of 8 mm or more in anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;6(3):23259 67118760815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 21. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 22. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29(12):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66(3):344–352. [PubMed] [Google Scholar]
- 25. Odensten M, Gillquist J. Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg Am. 1985;67(2):257–262. [PubMed] [Google Scholar]
- 26. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. [DOI] [PubMed] [Google Scholar]
- 27. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 28. Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34(12):1933–1940. [DOI] [PubMed] [Google Scholar]
- 29. Schuette HB, Kraeutler MJ, Houck DA, McCarty EC. Bone-patellar tendon-bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Orthop J Sports Med. 2017;5(11):23259 67117736484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Snaebjornsson T, Hamrin Senorski E, Ayeni OR, et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med. 2017;45(9):2092–2097. [DOI] [PubMed] [Google Scholar]
- 31. Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(11):1945–1949. [DOI] [PubMed] [Google Scholar]
- 32. Tutkus V, Kluonaitis K, Silove S, Tutkuviene J. ACL reconstruction using 5- or 6-strand hamstring autograft provides graft’s diameter bigger than 8 mm. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1349–1356. [DOI] [PubMed] [Google Scholar]
- 33. Vaillant ER, Parks BG, Camire LM, Hinton RY. Five-strand versus four-strand hamstring tendon graft technique for anterior cruciate ligament reconstruction: a biomechanical comparison. J Knee Surg. 2017;30(9):916–919. [DOI] [PubMed] [Google Scholar]
- 34. Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]