Abstract
Purpose of Review
The purpose of this manuscript is to (1) examine the history, techniques, and methodology behind quantitative pivot shift investigations to date and (2) review the current status of pivot shift research for its clinical utility for management of anterior cruciate ligament (ACL) rupture with associated injuries including the anterolateral complex (ALC).
Recent Findings
The pivot shift is a useful physical exam maneuver for diagnosis of rotatory instability related to ACL tear. Recent evidence suggests that the pivot shift is multifactorial and can be seen in the presence of ACL tear with concomitant injury to secondary stabilizers or with predisposing anatomical factors.
Summary
The presence of a pivot shift post-operatively is associated with poorer outcomes after ACL reconstruction. Recent clinical and biomechanical investigations can help guide clinicians in utilizing pivot shift in diagnosis and surgical planning. Further research is needed to clarify optimal management of ALC in addition to ACL injury.
Keywords: Pivot shift, Anterior cruciate ligament tear, Anterior cruciate ligament reconstruction, Rotatory knee laxity, Anterolateral complex, Physical exam
Introduction
The optimal method of diagnosis and management of anterior cruciate ligament (ACL) ruptures continues to evolve with improved understanding of rotatory knee instability. Decision-making for treatment of ACL injuries depends on many factors, including level of activity or sport participation for the patient. Non-operative management of ACL tears can manifest as residual laxity or instability, especially during cutting, twisting, or pivoting motions. Consequently, it is crucial for clinicians to have an armamentarium of clinical tools, including accurate history taking, focused physical exam, and reliable diagnostic tests at their disposal.
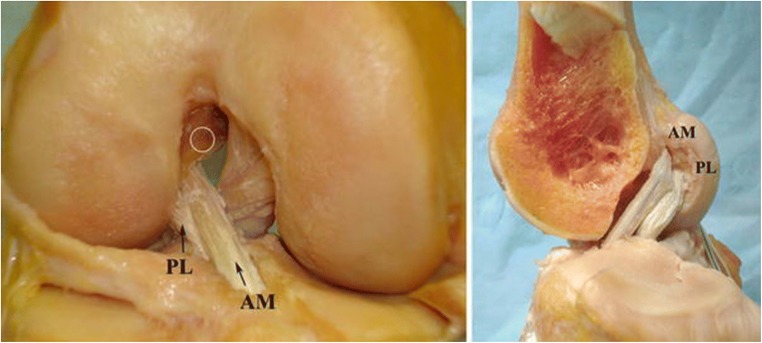
Understanding of the unique anatomy of the ACL is critical for accurately assessing laxity on physical exam. The ACL originates medially to the anterior intercondylar area of the tibia behind the anterior horn of the lateral meniscus. It travels posterolaterally through the knee joint to attach on the posteromedial aspect of the lateral femoral condyle [1]. Two separate bundles comprise the ACL with each performing a different biomechanical function (Fig. 1) [2]. The bundles function at different stages of knee motion with the anteromedial (AM) bundle taut at 90° of flexion and the posterolateral (PL) bundle tightening as the knee nears full extension. The AM bundle functions to restrain anterior tibial translation while the PL bundle is primarily responsible for controlling rotational stability.
Fig. 1.
Cadaveric representation of an anatomic double-bundle ACL reconstruction. The native relationship of the ACL to the PCL and intercondylar notch is reestablished. The circle marks the high AM position. (Reprinted with permission) [2]
Various diagnostic tests have been developed to evaluate for knee laxity secondary to ACL insufficiency [3]. Tests such as the anterior drawer and Lachman test for anterior tibial translation [4]. The Lachman test is a commonly performed technique as it has a high sensitivity for diagnosing ACL tear, as high as 94% to 98% in one study [5]. However, the Lachman test serves to only assess the AM bundle and fails to evaluate the ACL for objective rotational instability. Previous biomechanical evaluation of single-bundle ACL reconstruction using clinical maneuvers such as the anterior drawer and Lachman test demonstrated adequate function resisting anterior tibial loads, but they failed to restore the native kinematics of the ACL under rotatory testing [6–8]. The diagnosis of rotatory instability related to ACL tear is crucial as pivot shift correlated more closely than Lachman test with positive patient-reported outcomes post-operatively [9]. Additionally, the presence of a pivot shift post-operatively after ACL reconstruction is associated with persistent complaints of subjective instability from patients and can predict the development of early arthritis [10, 11]. Initially described by Galway et al., the pivot shift test was developed to test for lateral compartment rotatory laxity related to ACL insufficiency [12]. Current descriptions of the pivot shift test for dynamic ACL insufficiency by evaluating axial and sagittal stability of the knee as it is taken from extension to flexion with an external rotation and valgus stress on the proximal tibia.
The pivot shift is theoretically the ideal test to dynamically evaluate the ligamentous status of the knee, which is especially crucial in diagnosing ACL deficiency, evaluating reconstructive techniques, and constructing treatment algorithms for patients with ACL injury [13, 14]. Currently, the pivot shift test is the most specific clinical test to detect ACL injury [15]. The methodology for standardizing the pivot shift has been described and shown to have improved accuracy [16]. However, many studies utilize alternative methods for testing and quantifying the pivot shift. Accordingly, the pivot shift has been the subject of considerable research interest over the past few years. Investigations have shown that pivot shift phenomenon is multifactorial and that high-grade pivot shift is generally associated with a secondary injury in addition to the ACL. Incomplete understanding of the causes of pivot shift can cloud treatment approaches and may predispose surgeons towards supplementary reconstructive techniques, such as addressing the anterolateral complex (ALC), without identifying the true nature of the pathology. The purpose of this review is to discuss the current status of pivot shift methodology and clinical utility as it relates to ACL rupture and associated injuries.
Pivot Shift Methodology
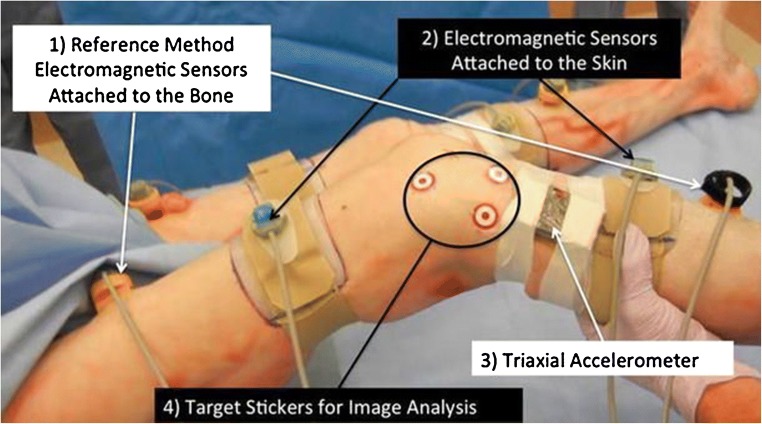
The historical criticism of the pivot shift mainly stems from the wide array of methods utilized for performing the maneuver [17]. The pivot shift can be inherently difficult to perform, and significant variability can exist between different examiners [18, 19]. The most commonly cited method of performing the pivot shift is: flexing the knee from 0° (full extension) to 90° of knee flexion while applying an external rotation stress to the tibia and a valgus stress to the knee [20]. A positive test is seen with a rapid anterior subluxation of the tibia at 20–30° of flexion as it reduces under the femoral condyles. Functionally, this is reproducing the event that occurs when the knee gives way due to ACL rupture. A slightly different technique in performing the procedure can affect the results; one recent study demonstrated significantly different pivot shift values with the tibia in internal versus external rotation when evaluating ACL-deficient knees [21]. Kuroda et al. described a most common variability in performing the maneuver with regard to flexion version extension type pivot shift and tibial rotation for the test, but they reported no significant differences between examiners for pivot shift acceleration or tibial translation [22]. Two major methods of teaching the pivot shift maneuver exist; either through real-time teaching from an instructor or passive learning through the use of instructional textbooks or videos. Comparing the two methods, the real-time teaching method demonstrated a higher success rate as this group was more effective at recreating the appropriate valgus and external rotation position [23]. The subject of a standardized pivot shift maneuver was discussed at the Panther Global Summit (Pittsburgh, PA, USA, August 2012) [24]. A subsequent study [25] testing 12 expert knee surgeons using their preferred method of pivot shift along with a standardized method (observed via video) was performed; the standardized test demonstrated good correlation between non-invasive (electromagnetic skin sensors, triaxial accelerometer, and image analysis) and direct (electromagnetic bone sensors) measurement parameters (Fig. 2).
Fig. 2.
Pivot shift quantification methods. (1) The electromagnetic tracking system attached to the bone (direct measurement), (2) electromagnetic tracking system attached to the skin (non-invasive measurement), (3) triaxial accelerometer (non-invasive measurement), and (4) image analysis system (non-invasive measurement). (Reprinted with permission) [25]
Subjectivity also exists in the grading systems described for quantifying the pivot shift. Various scoring systems have been proposed but none of these systems has been widely accepted due to the difficulty of assigning numerical values to factors that are not quantifiable [17]. In an ACL-deficient knee, the knee pivots from the medial tibial spine centrally to produce an anterior and medial subluxation. The lateral compartment then has exaggerated anterior tibial translation. The International Knee Documentation Committee (IKDC) classification defined a grading system for pathologic motion observed in a pivot shift test: grade 0 (normal), grade 1 (glide), grade 2 (clunk), or grade 3 (locked subluxation) [12]. A grade 3 pivot shift has been associated with poorer outcomes in clinical studies, including a possible earlier progression to knee osteoarthritis [11, 26].
Quantitative Assessment of the Pivot Shift
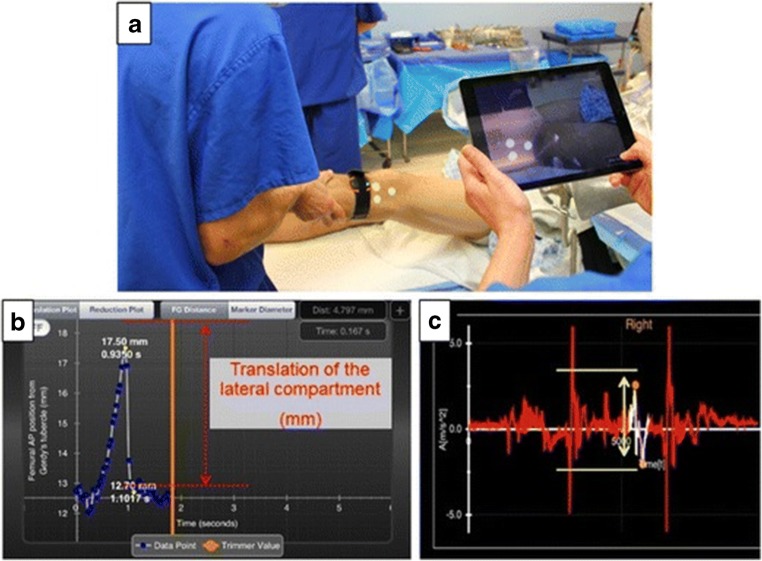
The methods for measuring pivot shift have shifted over the last decade. Previously, testing was performed predominately with computer navigation systems and electromagnetic sensor systems [13, 27, 28]. Other methods included biomechanical testing using cadaveric sectioning, serial radiographs, cable linear displacement transducers, and electro-goniometers with load cells [3]. More recent advancements have introduced inertial sensors and image analysis systems. One study found that 2D simple image analysis method and the 3D bony motion of the knee during the pivot shift test had similar outcomes [15]. This study concluded that the 2D simple image analysis is a non-invasive and repeatable tool to quantify the motion of the lateral knee compartment during the pivot shift test. The primary outcomes of interest for inertial sensors are lateral compartment translation and acceleration. It has been suggested that measurement of acceleration of the tibial reduction during the pivot shift can be performed in the office setting using just a single accelerometer [29]. Inertial sensors have also been used to quantify differences in lateral compartment motion between “high-grade” and “low-grade” laxity knees as tested by the IKDC machine [30]. Computer programs such as the KiRA acquisition system (KiRA, Orthokey LLC, Lewes, DE, USA) have been evaluated for as a potential method of standardized objective recording [31]. An iPad (iPad, Apple Inc., Cupertino, CA, USA) application has also been developed with encouraging initial results [24] (Fig. 3) [32]. Despite several studies on navigation systems, electromagnetic sensors, and other devices, issues with inconsistent methodology and technique have limited objective measurements to the research realm [29].
Fig. 3.
a The PIVOT iPad application software and KiRA accelerometer in clinical use. b The anterior translation of the lateral knee compartment in the PIVOT software interface. c The measured acceleration curve per unit time is plotted by the KiRA software. (Reprinted with permission) [32]
Permutations of Technique
No standardized validated system or technique is widely used. Study methodology varies frequently in outcome measure, manual versus mechanized testing, awake versus anesthetized testing, gravity-assisted pivot shift testing, or other subtle nuances in leg positioning while achieving the pivot shift. A number of in vitro cadaveric studies have been performed to simulate the pivot shift using a variety of different outcome measures including internal rotation torque, valgus torque, and iliotibial tract tension [20]. The outcomes most frequently reported are lateral compartment translation and tibial internal rotation. Musahl et al. examined the differences between manual and mechanized pivot shift testing. They found that in the ACL-deficient knee, manual pivot shift testing was associated with significantly higher tibial translation and rotation, suggesting that mechanized pivot shift measurement may be a more reliable and consistent grading method [33]. One of the main difficulties is that muscular resistance can suppress the pivot shift phenomenon and therefore many studies have performed the testing under anesthesia rather than with patients awake [34, 35]. The pivot shift has been reported to have higher sensitivity when performed under anesthesia than with awake patients [5]. The gravity-assisted pivot shift has been described and utilized in previous studies [36, 37]. Gravity-assisted pivot shift is performed with awake patients and is regarded as positive with lower leg internal rotation suddenly with the knee subluxating at an angle of approximately 20° of flexion, followed by the reduction with knee flexion. Testing with gravity assistance has been suggested as a more reliable test for predicting patients who may have worse post-operative function after ACL reconstruction [36].
Recent Pivot Shift Investigations
The pivot shift is a complex maneuver combining both translation and rotation of the tibia relative to the femur. The cause of the pivot shift is theorized to involve ACL injury as well as secondary stabilizers of the knee such as the menisci, meniscal roots, meniscotibial ligaments, collateral ligaments, capsule, ALC, and bony morphology of the femoral condyles and tibial plateau [10, 26, 38–41]. Accordingly, investigations into the individual and combined contributions of various anatomic structures towards rotatory knee instability have been performed in the last few years. The pivot shift has been utilized extensively in these recent investigations.
Meniscal Injury
Concomitant meniscal injury occurs commonly with ACL tear. Failure to recognize these injuries may lead to poorer outcomes after ACL reconstruction [42]. Disruption of the circumferential meniscal fibers seen in the meniscal body and root tears leads to compromised biomechanical function and functional loss of secondary restraint. MRI evidence of a concomitant injury to both the medial and lateral menisci is associated with increased knee rotatory instability in patients with an ACL injury [43]. A recent study evaluated the correlation between the pivot shift and lateral compartment acceleration in patients undergoing primary single-bundle ACL reconstruction [40]. It was shown that knees with combined ACL and lateral meniscus injury demonstrated increased lateral compartment acceleration and translation compared to ACL injury alone. Song et al. also reported pivoting sport involvement at time of injury and combined lateral meniscal injuries as additional risk factors associated with a high-grade pivot shift after ACL injury [44•]. Shybut et al. examined lateral meniscal root injuries in ACL-deficient knees in human cadaveric robotic testing [45]. It was shown that combined injury with lateral meniscal root demonstrated significantly higher anterior tibial translation but no significant difference with Lachman testing.
Meniscotibial Ligaments
“Ramp lesions” or tears at the peripheral attachment of the posterior horn of the medial meniscus at the meniscocapsular junction have been suspected to play a role in rotatory instability. DePhillipo et al. examined the biomechanical contributions of the meniscocapsular and meniscotibial attachments of the posterior medial meniscus by performing robotic human cadaveric testing. It was reported that injury to meniscocapsular and meniscotibial lesions of the posterior horn of the medial meniscus increased pivot shift in ACL-deficient knees, and the pivot shift was not restored after isolated ACL reconstruction [46]. A recent study by Pfeiffer et al. looking at the biomechanical profile of ramp lesions before and after repair with simulated ACL reconstruction found that ramp lesion repair with all-inside technique at 10° of knee flexion resulted in decreased anterior translation, increased valgus rotation, and increased bony contact forces in the lateral compartment suggesting potential over-constraint with repair [47].
Bony Morphology
Previous investigations have described the association between a smaller medial-to-lateral tibial plateau diameter and a high-grade pivot shift [39]. One recent study [48] examined the correlation between lateral femoral notch depth and rotatory knee instability. No correlation between rotatory instability using quantitative pivot shift of ACL-injured patients and lateral femoral notch depth was shown; however, they did note a significantly higher rate of associated lateral meniscus injury. Lateral tibial plateau slope has also been shown to have greater correlation with high-grade rotatory laxity with pivot shift testing; compared with the low-grade rotatory laxity group, high grade had a larger slope (9.3 ± 3.4° versus 6.1 ± 3.7°) [49]. Interestingly, another study reported that having a slope less than 5.5% had an association with high anteroposterior laxity at 30° and 90° of flexion [50]. Branch et al. examined a group of patients who had undergone ACL reconstruction and evaluated their bony morphology radiographically. A significantly higher rate of post-operative pivot shift was observed when patients had a higher femur-tibia size ratio (FRSR), when the femur was larger relative to the tibia, or a smaller tibia to posterior femoral condyle ratio (TPFCR), and when there was smaller tibial depth relative to the depth of the lateral posterior condyle [51].
Hypermobility
Joint hypermobility and ligamentous laxity are important factors to assess when evaluating a patient with ACL injury. Ligamentous laxity can be tested using the Beighton criteria, which is a measure of five joint movements and is interpreted based on a maximum score of 9, with scores greater than or equal to 4 being classified as hypermobile [52]. For patients with generalized hypermobility, a recent study showed greater laxity with pivot shift testing in the contralateral uninjured knee in patients with high Beighton hypermobility scores compared to those without hypermobility [53]. Interestingly, a high Beighton score did not correlate with any difference in pivot shift testing for the ACL-injured side. Pfeiffer et al. also examined generalized ligamentous laxity and knee hyperextension as measured in collegiate athletes without a history of knee injury [54]. Significantly higher anterior translation of the lateral compartment was observed during pivot shift in females, but no correlation with knee hyperextension or Beighton criteria was found.
High-grade Laxity
Several studies have investigated what factors play a role in a high-grade pivot shift. Magnussen et al. [55] reported chronic ACL injury, age greater than 20, and female gender to be factors associated with high-grade pivot shift. High-grade pre-operative pivot shift testing and knee hyperextension were found to be associated with higher risk of post-operative pivot shift after ACL reconstruction [56]. Song et al. reported on a comparison between low-grade and high-grade pivot shift patients with acute ACL injuries [41]. It was shown that the high-grade pivot shift group had a significantly higher prevalence of concomitant ALC injury on MRI. In knees designated as “high-grade laxity” with IKDC testing, both lateral compartment motion measured with image analysis and tibial acceleration measured with the inertial sensor were significantly higher compared to the “low-grade” group [30].
Remnant ACL
Kitamura et al. examined the effects of remnant ACL tissue preservation in improving long-term rotational laxity as measured by pivot shift [57]. They reported significantly improved anterior tibial translation and acceleration of posterior translation with pivot shift at 12 months compared to immediately post-operatively. It was suggested that the remnant tissue aided with healing and reported a significant association with the amount of tissue available to cover the graft at index surgery.
Contributions of the ALC
A recent consensus article discussed the anatomy, function, and current body of literature for the ALC [58•]. While some biomechanical studies have demonstrated that the ALC contributes to stability at the time of ACL reconstruction, some concerns remain about the possibility for over-constraining the lateral compartment. Optimal strategies for lateral extra-articular augmentation procedures are not clear as clinical evidence is currently lacking for specific indications. Debate exists as to the importance of the ALC when compared with the ACL and the iliotibial band (ITB) [58•].
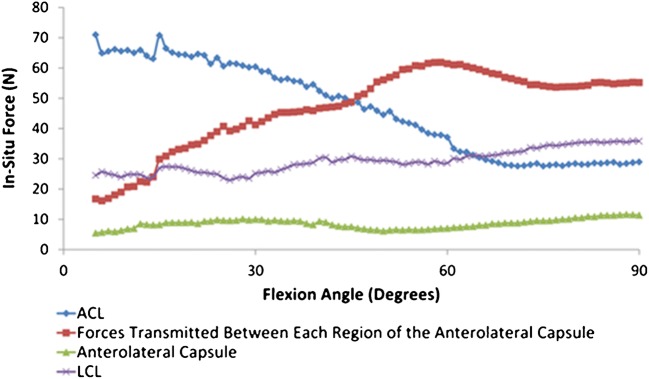
The ALC has been investigated extensively over the last several years in relation to ACL injuries and its contributions to rotatory instability. Cadaveric testing has been performed to evaluate the effect of the ALC; one study reported that ACL- and ALC-injured knees had significantly increased internal tibial rotation compared to the intact knee, but isolated ACL injury did not [59]. Noyes et al. performed cadaveric robotic testing and found that sectioning of the ALC after ACL reconstruction resulted in a small increase in internal rotation torque at high flexion and modestly reduced the forces seen by the ACL graft but did not change lateral compartment translation [60]. It was observed that pivot shift was increased at 20–30° of knee flexion. Bell et al. found that the ALC played a significant role as a secondary stabilizer at flexion angles greater than 60°. In this study, the dissected anterolateral ligament had a negligible contribution to rotatory knee instability (Fig. 4) [61•].
Fig. 4.
The in situ force in the ACL and the anterolateral structures throughout the range of flexion for the intact knee (newtons, mean). (Reprinted with permission) [61•]
Lateral Extra-articular Tenodesis
Cadaver testing of lateral extra-articular tenodesis (LET) in ACL-deficient and reconstructed knees was performed by Herbst et al. [62]. It was shown that ACL reconstruction in combination with LET reduced anterior tibial translation and internal tibial rotation with pivot shift testing in the setting of a knee with pre-existing ACL and ALC injury; for those patients with isolated ACL injury treated with reconstruction and LET, the end result was over-constraining of the knee. Monaco et al. reported that the addition of LET to ACL reconstruction resulted in little change to measured anterior displacement of the tibia at 30° of flexion, but it was more effective than isolated ACL reconstruction at reducing tibial rotation [63].
A clinical study examining chronic ACL injuries and resultant treatment with ACL with or without LET found that the addition of the LET was associated with significantly improved IKDC, Lysholm scores, and KT-1000 scores [64]. A lower rate of post-operative pivot shift with ALC capsular procedure was observed; however, they did not quantify this result.
ITB and Association with ALC
A number of studies have investigated the role of the ITB in its role relating to the ALC. Kittl et al. performed a biomechanical sectioning study; it was reported that the ITB made a greater contribution than the ALC to internal rotation control at larger flexion angles, with the ACL having its greatest contribution closer to extension [65]. Huser et al. also performed cadaveric robotic testing in cadaveric specimens with intact ACL to determine the contributions of the ALC and ITB to potential for pivot shift [66]. It was found that sectioning the ALC alone had no effect on lateral compartment translation or internal rotation under any loading condition, while ITB sectioning resulted in small increases in IR at 60 and 90° of flexion. A combined injury to ALC and ITB (with intact ACL) resulted in clinically undetectable but small increases in pivot shift internal rotation and lateral compartment translation. Similarly, Geeslin et al. examined the roles of the ALC with the Kaplan fibers of the distal ITB in ACL-deficient knees using robotic testing of human cadaveric specimens [67]. Sectioning the Kaplan fibers was found to lead to greater tibial internal rotation at high flexion angles (60–90°) as compared with sectioning of the ALC. Another biomechanical study examining ACL with combined simulated ALC injury compared LET using a Lemaire procedure with an ALC reconstruction; it was concluded that the LET restored normal laxities at all angles of flexion for graft fixation (0°, 30°, or 60°), with the ALC reconstruction only restored intact knee kinematics when tensioned in full extension [68]. In a clinical study, Porter et al. examined a group of patients who had residual pivot shift intraoperatively after revision ACL reconstruction who then underwent ITB tenodesis as a supplementary procedure [69]. ITB tenodesis resulted in a significant decrease in anterior tibial translation and in internal tibial rotation. No significant differences were noted in Tegner activity scores post-operatively.
Conclusions
The pivot shift phenomenon is multifactorial. With growing evidence that meniscal, meniscocapsular, and ALC injury may play a role in rotatory knee instability, it is important for the clinician to be aware of concomitant soft tissue injuries with planned ACL reconstruction procedures. Additional patient anatomic factors such as bony morphology or ligamentous laxity should also be considered. While lateral extra-articular tenodesis procedures are regaining popularity, further research is needed to clarify individual contributions of ligamentous structures and to solidify a standardized testing and grading methodology of the pivot shift.
Conflict of Interest
Nicholas J. Vaudreuil, Benjamin B. Rothrauff, and Darren de Sa declare no conflict of interest.
Volker Musahl has done consulting work for Smith & Nephew.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N. The anatomy of the ACL and its importance in ACL reconstruction. Eur J Orthop Surg Traumatol. 2013;23(7):747–752. doi: 10.1007/s00590-012-1079-8. [DOI] [PubMed] [Google Scholar]
- 2.Colvin AC, Shen W, Musahl V, Fu FH. Avoiding pitfalls in anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):956–963. doi: 10.1007/s00167-009-0804-2. [DOI] [PubMed] [Google Scholar]
- 3.Lane CG, Warren R, Pearle AD. The pivot shift. J Am Acad Orthop Surg. 2008;16(12):679–688. doi: 10.5435/00124635-200812000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4(2):84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 5.Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36(5):267–288. doi: 10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 6.Woo SL, Kanamori A, Zeminski J, et al. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84-A(6):907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SLY. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(5):660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 8.Woo SL, Wu C, Dede O, Vercillo F, Noorani S. Biomechanics and anterior cruciate ligament reconstruction. J Orthop Surg Res. 2006;1:2. doi: 10.1186/1749-799X-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaplan N, Wickiewicz TL, Warren RF. Primary surgical treatment of anterior cruciate ligament ruptures. A long-term follow-up study. Am J Sports Med. 1990;18(4):354–358. doi: 10.1177/036354659001800404. [DOI] [PubMed] [Google Scholar]
- 10.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 11.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75(5):594–599. doi: 10.1080/00016470410001484. [DOI] [PubMed] [Google Scholar]
- 12.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980;147:45–50. [PubMed] [Google Scholar]
- 13.Sundemo D, Alentorn-Geli E, Hoshino Y, Musahl V, Karlsson J, Samuelsson K. Objective measures on knee instability: dynamic tests: a review of devices for assessment of dynamic knee laxity through utilization of the pivot shift test. Curr Rev Musculoskelet Med. 2016;9(2):148–159. doi: 10.1007/s12178-016-9338-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsumoto H. Mechanism of the pivot shift. J Bone Joint Surg Br. 1990;72(5):816–821. doi: 10.1302/0301-620X.72B5.2211763. [DOI] [PubMed] [Google Scholar]
- 15.Arilla FV, Rahnemai-Azar AA, Yacuzzi C, Guenther D, Engel BS, Fu FH, Musahl V, Debski RE. Correlation between a 2D simple image analysis method and 3D bony motion during the pivot shift test. Knee. 2016;23(6):1059–1063. doi: 10.1016/j.knee.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S, Karlsson J, Fu FH, Musahl V. Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):732–736. doi: 10.1007/s00167-011-1850-0. [DOI] [PubMed] [Google Scholar]
- 17.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 18.Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, Karlsson J, Fu FH. The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):724–731. doi: 10.1007/s00167-011-1859-4. [DOI] [PubMed] [Google Scholar]
- 19.Noyes FR, Grood ES, Cummings JF, Wroble RR. An analysis of the pivot shift phenomenon. The knee motions and subluxations induced by different examiners. Am J Sports Med. 1991;19(2):148–155. doi: 10.1177/036354659101900210. [DOI] [PubMed] [Google Scholar]
- 20.Arilla FV, Yeung M, Bell K, Rahnemai-Azar AA, Rothrauff BB, Fu FH, Debski RE, Ayeni OR, Musahl V. Experimental execution of the simulated pivot-shift test: a systematic review of techniques. Arthroscopy. 2015;31(12):2445–2454. doi: 10.1016/j.arthro.2015.06.027. [DOI] [PubMed] [Google Scholar]
- 21.Kopf S, Musahl V, Perka C, Kauert R, Hoburg A, Becker R. The influence of applied internal and external rotation on the pivot shift phenomenon. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1106–1110. doi: 10.1007/s00167-017-4429-6. [DOI] [PubMed] [Google Scholar]
- 22.Kuroda R, Hoshino Y, Kubo S, Araki D, Oka S, Nagamune K, Kurosaka M. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency: a global survey and kinematics assessment. Am J Sports Med. 2012;40(1):91–99. doi: 10.1177/0363546511423634. [DOI] [PubMed] [Google Scholar]
- 23.Patel NK, Murphy CI, Nagai K, et al. Passive teaching is not as effective as active teaching for learning the standard technique of pivot shift test. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine 2018.
- 24.Hoshino Y, Araujo P, Ahlden M, et al. Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):975–980. doi: 10.1007/s00167-013-2396-0. [DOI] [PubMed] [Google Scholar]
- 25.Araujo PH, Ahlden M, Hoshino Y, Muller B, Moloney G, Fu FH, Musahl V. Comparison of three non-invasive quantitative measurement systems for the pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):692–697. doi: 10.1007/s00167-011-1862-9. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka M, Vyas D, Moloney G, Bedi A, Pearle AD, Musahl V. What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc. 2012;20(4):737–742. doi: 10.1007/s00167-011-1866-5. [DOI] [PubMed] [Google Scholar]
- 27.Colombet P, Robinson J, Christel P, Franceschi JP, Djian P. Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res. 2007;454:59–65. doi: 10.1097/BLO.0b013e31802baf56. [DOI] [PubMed] [Google Scholar]
- 28.Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD. In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):487–492. doi: 10.1007/s00167-008-0504-3. [DOI] [PubMed] [Google Scholar]
- 29.Zaffagnini S, Lopomo N, Signorelli C, Marcheggiani Muccioli GM, Bonanzinga T, Grassi A, Visani A, Marcacci M. Innovative technology for knee laxity evaluation: clinical applicability and reliability of inertial sensors for quantitative analysis of the pivot-shift test. Clin Sports Med. 2013;32(1):61–70. doi: 10.1016/j.csm.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 30.Musahl V, Griffith C, Irrgang JJ, Hoshino Y, Kuroda R, Lopomo N, Zaffagnini S, Samuelsson K, Karlsson J, PIVOT Study Group. Oostdyk A, Rahnemai-Azar AA, Arilla FV, Guenther D, Zlotnicki J, Ohashi B, Araujo P, Kurosaka M, Nagamune K, Marcheggiani Muccioli GM, Signorelli C, Bjoernsson H, Ahlden M, Desai N, Fu FH. Validation of quantitative measures of rotatory knee laxity. Am J Sports Med. 2016;44(9):2393–2398. doi: 10.1177/0363546516650667. [DOI] [PubMed] [Google Scholar]
- 31.Lopomo N, Zaffagnini S, Signorelli C, Bignozzi S, Giordano G, Marcheggiani Muccioli GM, Visani A. An original clinical methodology for non-invasive assessment of pivot-shift test. Comput Methods Biomech Biomed Engin. 2012;15(12):1323–1328. doi: 10.1080/10255842.2011.591788. [DOI] [PubMed] [Google Scholar]
- 32.Zlotnicki JP, Naendrup JH, Ferrer GA, Debski RE. Basic biomechanic principles of knee instability. Curr Rev Musculoskelet Med. 2016;9(2):114–122. doi: 10.1007/s12178-016-9329-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Musahl V, Voos J, O’Loughlin PF, et al. Mechanized pivot shift test achieves greater accuracy than manual pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1208–1213. doi: 10.1007/s00167-009-1004-9. [DOI] [PubMed] [Google Scholar]
- 34.Kuroda R, Hoshino Y, Araki D, Nishizawa Y, Nagamune K, Matsumoto T, Kubo S, Matsushita T, Kurosaka M. Quantitative measurement of the pivot shift, reliability, and clinical applications. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):686–691. doi: 10.1007/s00167-011-1849-6. [DOI] [PubMed] [Google Scholar]
- 35.Matsushita T, Oka S, Nagamune K, et al. Differences in knee kinematics between awake and anesthetized patients during the Lachman and pivot-shift tests for anterior cruciate ligament deficiency. Orthop J Sports Med. 2013;1(1):2325967113487855. doi: 10.1177/2325967113487855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sakai H, Hiraoka H, Yashiki M. Gravity-assisted pivot-shift test can predict the function of the reconstructed anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):572–578. doi: 10.1007/s00167-010-1279-x. [DOI] [PubMed] [Google Scholar]
- 37.Sakai H, Yajima H, Kobayashi N, Kanda T, Hiraoka H, Tamai K, Saotome K. Gravity-assisted pivot-shift test for anterior cruciate ligament injury: a new procedure to detect anterolateral rotatory instability of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):2–6. doi: 10.1007/s00167-005-0630-0. [DOI] [PubMed] [Google Scholar]
- 38.Fetto JF, Marshall JL. Injury to the anterior cruciate ligament producing the pivot-shift sign. J Bone Joint Surg Am. 1979;61(5):710–714. doi: 10.2106/00004623-197961050-00010. [DOI] [PubMed] [Google Scholar]
- 39.Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL. The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1232–1238. doi: 10.1007/s00167-010-1129-x. [DOI] [PubMed] [Google Scholar]
- 40.Musahl V, Burnham J, Lian J, et al. High-grade rotatory knee laxity may be predictable in ACL injuries. Knee Surg Sports Traumatol Arthrosc 2018. [DOI] [PubMed]
- 41.Song GY, Zhang H, Wu G, Zhang J, Liu X, Xue Z, Qian Y, Feng H. Patients with high-grade pivot-shift phenomenon are associated with higher prevalence of anterolateral ligament injury after acute anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1111–1116. doi: 10.1007/s00167-017-4492-z. [DOI] [PubMed] [Google Scholar]
- 42.Shaver JC, Johnson DL. Unlocking the ‘pivot shift’ in ACL surgery: medial meniscus evaluation and treatment. Orthopedics 2008;31(12). [DOI] [PubMed]
- 43.Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, Lopomo N, Samuelsson K, Irrgang JJ. The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. 2016;44(12):3126–3131. doi: 10.1177/0363546516659649. [DOI] [PubMed] [Google Scholar]
- 44.Song GY, Zhang H, Wang QQ, et al. Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med. 2016;44(2):362–369. doi: 10.1177/0363546515613069. [DOI] [PubMed] [Google Scholar]
- 45.Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC, Lowe WR. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. doi: 10.1177/0363546514563910. [DOI] [PubMed] [Google Scholar]
- 46.DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med 2018:363546518774315. [DOI] [PubMed]
- 47.Pfeiffer TR, Naendrup JH, Chan C, et al. Effect of meniscal ramp repair on knee kinematics, ACL in situ force and bony contact forces - a biomechanical study. Orthop J Sports Med. 2018;6(7_suppl4):2325967118S00157. [Google Scholar]
- 48.Kanakamedala AC, Burnham JM, Pfeiffer TR, Herbst E, Kowalczuk M, Popchak A, Irrgang J, Fu FH, Musahl V. Lateral femoral notch depth is not associated with increased rotatory instability in ACL-injured knees: a quantitative pivot shift analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1399–1405. doi: 10.1007/s00167-017-4770-9. [DOI] [PubMed] [Google Scholar]
- 49.Rahnemai-Azar AA, Abebe ES, Johnson P, Labrum J, Fu FH, Irrgang JJ, Samuelsson K, Musahl V. Increased lateral tibial slope predicts high-grade rotatory knee laxity pre-operatively in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1170–1176. doi: 10.1007/s00167-016-4157-3. [DOI] [PubMed] [Google Scholar]
- 50.Grassi A, Signorelli C, Urrizola F, Raggi F, Macchiarola L, Bonanzinga T, Zaffagnini S. Anatomical features of tibia and femur: influence on laxity in the anterior cruciate ligament deficient knee. Knee. 2018;25(4):577–587. doi: 10.1016/j.knee.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 51.Branch T, Stinton S, Sharma A, Lavoie F, Guier C, Neyret P. The impact of bone morphology on the outcome of the pivot shift test: a cohort study. BMC Musculoskelet Disord. 2017;18(1):463. doi: 10.1186/s12891-017-1798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sundemo D, Blom A, Hoshino Y, et al. Correlation between quantitative pivot shift and generalized joint laxity: a prospective multicenter study of ACL ruptures. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2362–2370. doi: 10.1007/s00167-017-4785-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pfeiffer TR, Kanakamedala AC, Herbst E, Nagai K, Murphy C, Burnham JM, Popchak A, Debski RE, Musahl V. Female sex is associated with greater rotatory knee laxity in collegiate athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1319–1325. doi: 10.1007/s00167-017-4684-6. [DOI] [PubMed] [Google Scholar]
- 55.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP, Andrish JT, Jones MH, Parker RD, McCarty EC, Vidal AF, Wolcott ML, Marx RG, Amendola A, Wolf BR, Flanigan DC, Kaeding CC, Brophy RH, Matava MJ, Wright RW, Dunn WR. Factors associated with high-grade Lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(6):1080–1085. doi: 10.1016/j.arthro.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ueki H, Nakagawa Y, Ohara T, Watanabe T, Horie M, Katagiri H, Otabe K, Katagiri K, Hiyama K, Katakura M, Hoshino T, Inomata K, Araya N, Sekiya I, Muneta T, Koga H. Risk factors for residual pivot shift after anterior cruciate ligament reconstruction: data from the MAKS group. Knee Surg Sports Traumatol Arthrosc. 2018;26:3724–3730. doi: 10.1007/s00167-018-5005-4. [DOI] [PubMed] [Google Scholar]
- 57.Kitamura N, Yasuda K, Yokota M, Goto K, Wada S, Onodera J, Kondo E. The effect of intraoperative graft coverage with preserved remnant tissue on the results of the pivot-shift test after anatomic double-bundle anterior cruciate ligament reconstruction: quantitative evaluations with an electromagnetic sensor system. Am J Sports Med. 2017;45(10):2217–2225. doi: 10.1177/0363546517706702. [DOI] [PubMed] [Google Scholar]
- 58.• Getgood A, Brown C, Lording T, et al. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg sports Traumatol Arthrosc 2018. This is a detailed review of current data regarding anterolateral complex of knee including current treatment recommendations. [DOI] [PubMed]
- 59.Monaco E, Fabbri M, Mazza D, Daggett M, Redler A, Lanzetti RM, de Carli A, Ferretti A. The effect of sequential tearing of the anterior cruciate and anterolateral ligament on anterior translation and the pivot-shift phenomenon: a cadaveric study using navigation. Arthroscopy. 2018;34(4):1009–1014. doi: 10.1016/j.arthro.2017.09.042. [DOI] [PubMed] [Google Scholar]
- 60.Noyes FR, Huser LE, Jurgensmeier D, Walsh J, Levy MS. Is an anterolateral ligament reconstruction required in ACL-reconstructed knees with associated injury to the anterolateral structures? A robotic analysis of rotational knee stability. Am J Sports Med. 2017;45(5):1018–1027. doi: 10.1177/0363546516682233. [DOI] [PubMed] [Google Scholar]
- 61.Bell KM, Rahnemai-Azar AA, Irarrazaval S, et al. In situ force in the anterior cruciate ligament, the lateral collateral ligament, and the anterolateral capsule complex during a simulated pivot shift test. J Orthop Res. 2018;36(3):847–853. doi: 10.1002/jor.23676. [DOI] [PubMed] [Google Scholar]
- 62.Herbst E, Arilla FV, Guenther D, Yacuzzi C, Rahnemai-Azar AA, Fu FH, Debski RE, Musahl V. Lateral extra-articular tenodesis has no effect in knees with isolated anterior cruciate ligament injury. Arthroscopy. 2018;34(1):251–260. doi: 10.1016/j.arthro.2017.08.258. [DOI] [PubMed] [Google Scholar]
- 63.Monaco E, Maestri B, Conteduca F, Mazza D, Iorio C, Ferretti A. Extra-articular ACL reconstruction and pivot shift: in vivo dynamic evaluation with navigation. Am J Sports Med. 2014;42(7):1669–1674. doi: 10.1177/0363546514532336. [DOI] [PubMed] [Google Scholar]
- 64.Helito CP, Camargo DB, Sobrado MF, et al. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2018. [DOI] [PubMed]
- 65.Kittl C, El-Daou H, Athwal KK, et al. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee: response. Am J Sports Med. 2016;44(4):NP15–NP18. doi: 10.1177/0363546516638070. [DOI] [PubMed] [Google Scholar]
- 66.Huser LE, Noyes FR, Jurgensmeier D, Levy MS. Anterolateral ligament and iliotibial band control of rotational stability in the anterior cruciate ligament-intact knee: defined by tibiofemoral compartment translations and rotations. Arthroscopy. 2017;33(3):595–604. doi: 10.1016/j.arthro.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 67.Geeslin AG, Chahla J, Moatshe G, Muckenhirn KJ, Kruckeberg BM, Brady AW, Coggins A, Dornan GJ, Getgood AM, Godin JA, LaPrade RF. Anterolateral knee extra-articular stabilizers: a robotic sectioning study of the anterolateral ligament and distal iliotibial band Kaplan fibers. Am J Sports Med. 2018;46(6):1352–1361. doi: 10.1177/0363546518759053. [DOI] [PubMed] [Google Scholar]
- 68.Inderhaug E, Stephen JM, Williams A, Amis AA. Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45(13):3089–3097. doi: 10.1177/0363546517724422. [DOI] [PubMed] [Google Scholar]
- 69.Porter MD, Shadbolt B, Pomroy S. The augmentation of revision anterior cruciate ligament reconstruction with modified iliotibial band tenodesis to correct the pivot shift: a computer navigation study. Am J Sports Med. 2018;46(4):839–845. doi: 10.1177/0363546517750123. [DOI] [PubMed] [Google Scholar]