Abstract
Purpose of Review
The purposes of this review are to discuss the management of shoulder and elbow fractures in athletes to optimize the return to sport and to highlight treatment impact on the return to play.
Recent findings
Fractures of the shoulder and elbow can have profound implications in an athlete career. Recent technique of fractures management trended toward to preserve soft tissue which is critical for an early recovery in athletic population. Arthroscopy presents a strong interest for the treatment of intra-articular fracture, and minimally invasive approach as developed in humeral shaft fracture can be considered to avoid soft tissue damage.
Summary
Non-articular, stable, and minimally displaced fractures are mainly treated conservatively. However, we encourage a more aggressive approach in shoulder and elbow injuries in the athletes including minimally invasive and stable fixation to preserve vascularity and muscle environment.
Keywords: Athlete fracture, Clavicle fracture, Glenoid fracture, Mid-shaft humeral fracture, Scapula fracture
Introduction
Upper extremity injuries are common among professional athletes, occurring in up to 50% of NFL games [1] and representing 50% of the injuries reported in Major League Baseball [2••]. These injuries include both soft tissue injuries as well as fractures, the topic of this review article. While fracture morphology in athletes may be similar to the general population, there are multiple issues that need to be accounted for when safe return to sports as quickly as possible and with the best possible outcome are the driving principles of treatment. When treating fractures in athletes, safe and successful, and expedient return to play is emphasized. In addition, expectations in terms of functional outcomes are dramatically higher in the athletic compared to the general population. The overarching principle when treating fractures in athletes is to select a treatment strategy that results in a rapid union of the fracture, with a short recovery time, and results in optimal time to return to sports at a high level.
In general terms, early habitation aimed to quick restoration of a complete arc of motion as well as institution of strengthening exercises as soon as possible are the mainstay of treatment in the athlete. While nonoperative treatment may be the treatment of choice for many extra-articular fractures in the general population, the potential for lengthy immobilization may make conservative treatment less desirable for athletes. On the other hand, although open reduction and internal fixation (ORIF) can provide the basis for immediate unprotected rehabilitation, when extensive dissection is required, soft tissue contractures might result in long-term functional limitations that would be detrimental to the athlete.
This article provides a review of common upper extremity fracture patterns in sport-related injuries and discusses treatment options that provide an early and safe return to sports with special considerations to less invasive techniques.
Clavicle
Epidemiology
In the general population, clavicular fractures have been reported to represent 2.6% to 10% of all adult fractures [3, 4]. In the athlete population, fractures of the mid-shaft (70%) and lateral shaft of the clavicle (25%) are the most common [5]. Around 45% of sport-related clavicle fractures are nondisplaced. Kaplan et al. 2005 [6] evaluated shoulder injuries in 226 elite collegiate football players and reported that clavicular fractures represented 4% of shoulder injuries.
In addition to collision sports—like football—cycling is related with a relatively high rate of clavicle fractures. Several studies have reported clavicle fractures as the most common bone injury in the cyclist population, accounting for 44% of all fractures collected between 2004 and 2008 in one particular study [7]. When looking at professional cyclists, collision between cyclists is a common cause of clavicle fracture (39%) followed by collision with obstacles as well as loss of bicycle control with resultant falling [8]. Among 140 amateur and professional cyclists, Nishimi et al. [9] correlated the prevalence of clavicular fractures with more intense weekly hour training.
Treatment
In the general population, clavicle fractures have traditionally been treated conservatively with reasonable functional results, even in the presence of mild to moderate displacement. However, residual symptoms of pain and loss of endurance (particularly when performing overhead activities), which are better tolerated in the general population, can have detrimental effects on an athlete’s performance. Robertson et al. [7] showed that of all sport-related fractures, clavicle fractures have the third longest time to return to sport, with as many as 20% of athletes failing to return to their sport.
Nonoperative treatment of a mid-shaft fracture of the clavicle in an athlete was the preferred treatment for decades. Recent studies, however, have suggested benefits of primary fixation of displaced mid-shaft clavicle fractures, resulting in an increase in the frequency of operative treatment for athletes to diminish functional deficits and early refractures [10].
Several studies have reported a relatively high rate of nonunion or symptomatic malunion in nonoperatively treated clavicular fractures [11, 12]. These findings were confirmed by a systematic review of the literature including a total of 412 patients; operative treatment provided a significantly lower rate of nonunion and symptomatic malunion compared to nonoperative treatment (p = .001 and p < .001 respectively) [13]. Moreover, this meta-analysis reported that primary surgical treatment of clavicle fractures was related to an earlier return to sports. In a prospective randomized trial on fractures of the mid-third of the clavicle, Witzel et al. [14] compared minimally invasive intramedullary pin osteosynthesis and conservative treatment in 68 patients. Patients treated surgically reported better postoperative mobility and earlier return to activity. Sixty days after injury or surgery, 80% of patients who received surgical treatment were able to return to a moderate activity, compared to only 55% of patients treated nonoperatively [14].
Rates of return to sports have been reported to be satisfactory after internal fixation of clavicle fractures in athletes. Considering 3 recent retrospective series [15–17], which included a total number of 122 athletes treated with open reduction and internal fixation (plate fixation) for a mid-shaft clavicle fracture, 99% of patients returned to sports and 97% of them returned at the same level. At a mean follow-up of 33.3 months, only 5% of patients experienced major complications, which included compression of the subclavian vein (1 shoulder), refracture (2 shoulders) and nonunion (3 shoulders). In a study of 54 athletes, Ranalletta et al. [16] reported that 16.6% of patients returned to sport within 6 weeks, and 74% of patients returned between 6 and 12 weeks.
For unstable lateral clavicle fractures, surgery is typically recommended. Minimally invasive techniques, including arthroscopic assisted techniques, require limited exposure, and no deltoid takedown. Ranalletta et al. 2017 [18] retrospectively reviewed 21 athletes with displaced lateral clavicle fractures and treated with closed reduction and minimally invasive endobutton fixation; at a mean follow-up of 41 months, 20 patients returned to sports at their preinjury level, 20% of patients returned within 6 weeks, and 70% returned between 6 and 12 weeks postoperatively. At most recent follow-up, the mean Constant and QD scores were 89.1 and 0.4, respectively. The only complication was one asymptomatic nonunion. Hardware removal was not performed in any of the shoulders.
Authors’ Preferred Method
Our preference is to treat nondisplaced fractures of the clavicle in the athlete nonoperatively. A brief period of immobilization is followed by early supine (to eliminate gravity as a deforming force) range of motion exercises (supine positioning eliminates gravity as a deforming force). If clinical and radiographic progression of healing are demonstrated 6 weeks after the injury, sport-related skills may be initiated. Collision sports, high impact, repetitive over shoulder height activities, and high-risk sports (cycling and others) are best avoided until 3 months after the injury.
We have a very low threshold to offer surgical management for displaced fractures in the athlete. Provided the fracture pattern allows, our preference is to perform anteroinferior plating of mid-shaft fractures to avoid plate prominence and decrease the need for hardware removal (Fig. 1). Active use of the shoulder is initiated in seven to 10 days, with earlier return to the practice of sport-related skills, but avoidance of collision or high-risk sports for 2 to 3 months.
Fig. 1.
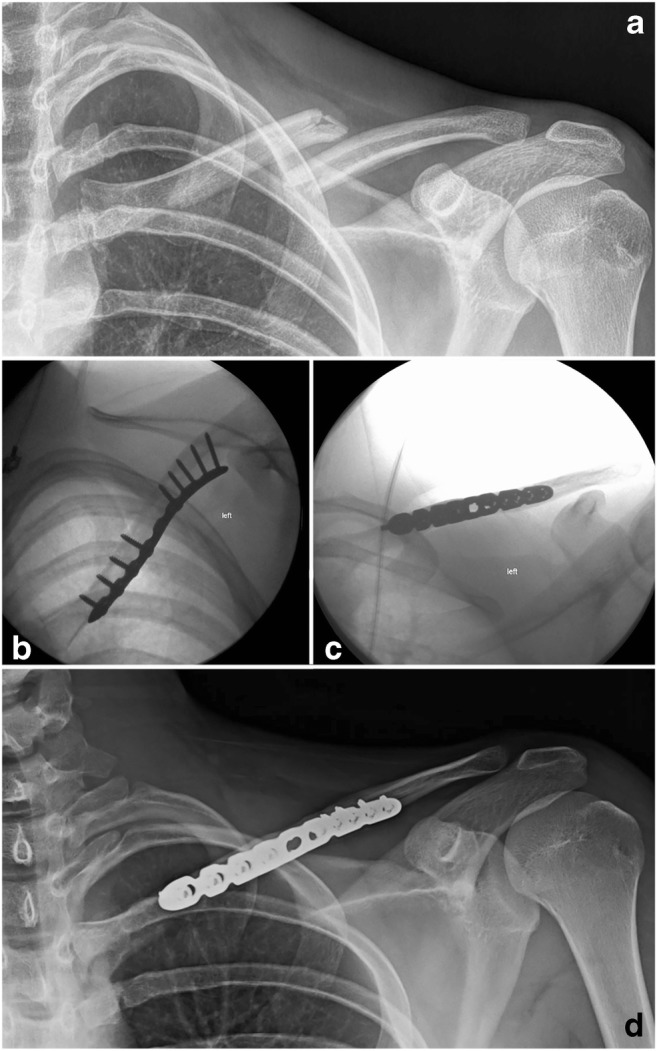
Open reduction and internal fixation of a displaced mid-shaft clavicle fracture using an anteroinferior plate
Unstable fractures of the lateral clavicle are typically treated surgically as well. We prefer coracoclavicular (CC) fixation with or without a distal clavicle plate. When the bone stock of the lateral fractured fragment allows, a lateral plate with CC fixation through the plate is favored. We typically use a superior plate, allowing CC fixation through the plate. In some fractures, arthroscopic assisted CC fixation alone is adequate. Although the principles of physical therapy are similar, we recommend up to 6 weeks of immobilization early on, as fixation is typically more tenuous in these fractures.
Humerus
Epidemiology
Humeral shaft fractures account for 6% of all long bone fractures [19]. The vast majority of humeral shaft fractures in the general population are related to direct trauma. However, in the athletic population, spiral fractures secondary to indirect injuries (throwing motion, arm wrestling) are more common than in the general population.
Treatment
The throwing motion is a complex movement involving the legs, core, shoulder, humerus elbow, wrist and hand in a linked kinetic chain. Among others parameters, Werner et al. found that velocity of the pitching motion was affected by maximum shoulder external rotation and peak elbow extension angular velocity [20]. As a consequence, if the treatment of a displaced humeral shaft fracture results in rotational malalignment, shoulder stiffness or elbow stiffness, overhead activities may be impaired and overhead athletes may not be able to return to their preinjury level of participation. This lowers the threshold for considering surgical management of displaced humeral shaft fractures in athletes. Furthermore, nonoperative management of humeral shaft fractures requires use of coaptation splints and functional bracing [26]. While early range of motion is encouraged with these techniques, many patients guard their shoulder and elbow, and range of motion on these two joints can be slow to return. Earlier return to ROM and function is advantageous when expectations are so high for function.
When surgical treatment is considered, open reduction and plate fixation is most commonly used. Compared to intramedullary nailing, plate fixation avoids access through the shoulder or elbow joints and provides the advantages of an anatomic reduction, stable fixation, and protection of the radial nerve. Recent literature has shown that plate fixation provides satisfactory outcomes, independent of the plate selection [21]. However, the morbidity of soft tissue dissection may significantly delay an athlete’s return to sport and affect their ability to pitch at the same level. To avoid an extensive dissection, minimally invasive percutaneous plate osteosynthesis (MIPPO) was developed and considered for patients predominantly involved in overhead activities [22]. Mahajan et al. [22] evaluated MIPPO for diaphysis humeral fractures in 48 patients who were predominantly involved in overhead activities, including athletes and manual laborers. Excellent clinical and functional results were reported, with no significant differences in function compared to the unaffected arm. Additionally, patients were able to return to original activities at a mean time of 64 days (36 to 182 days) postoperatively; the mean time to radiographic union was 45 days (34 to 180 days). The benefits of minimally invasive plate fixation were further supported by a meta-analysis comparing nail, ORIF, and MIPPO, which reported that the minimally invasive technique resulted in a significantly better outcome and lower complication rates. However, minimally invasive techniques fail to provide a direct visualization of the fracture line and neurovascular structures, and thus it can be difficult to ensure safe, anatomic reduction of the fracture.
Return to play/throwing can be initiated following healing of the fracture and restoration of shoulder and elbow motion. With dedicated physical therapy, a throwing program can be initiated around the 3-month mark. Contact activities can be initiated between 3 months and 5 months, depending on healing of the fracture.
Authors’ Preferences
Minimally and nondisplaced fractures are typically treated nonoperatively. Younger athletes form a stable soft callus quite rapidly, which allows return to sports earlier than in older, nonathlete patients. Displaced fractures in athletes are treated with minimally invasive plate fixation whenever possible; however, the benefits of less extensive soft tissue dissection must be balanced against the risk of neurovascular injury. Most fractures are approached through an anterolateral, brachialis splitting approach, but very low distal fractures are approached posteriorly by working on either or both sides of the triceps, trying to avoid a triceps split in athletes.
Scapula
Traumatic injuries of the scapula in athletes have received little attention in the literature because they are very uncommon. In a total of 7920 player participation hours recorded for 306 players, the reported rate of fractures of the scapula was 0.3 (range, 0.1 to 1.0) per 1000 h [23]. The relatively-deep location of the scapula behind the thorax explains why fractures of the scapula are relatively uncommon, representing only 1% of all fractures and 3% to 5% of upper extremity fractures [24, 25]. In the non-athlete population, fractures of the body of the scapula often result from high-energy trauma and are observed mostly in polytraumatized patients with substantial chest injuries (5% to 10% of polytraumatized patients present fractures in his region) [26]. On the contrary, glenoid rim fractures are often seen as a consequence of glenohumeral dislocation.
Most of the classifications for fracture of the scapula pay special attention to the glenoid, as it is the most critical structure of this bone, which can result in an intra-articular glenohumeral fracture [24, 27]. Established criteria for classifying scapular fractures based on size and displacement values are lacking [28–30]. The international scapula fracture classification represents a good starting point in understanding the potential complexity of these fractures [31, 32]. This system divides the scapula into 4 areas: glenoid fossa, coracoid, acromion and body. The glenoid fossa is defined as the portion of the scapula lateral to the plane parallel to the glenoid face through the suprascapular notch, not extending proximal to the superior articular rim. Although this classification system is shown to have better agreement than others [31, 32], it does not fully serve the purpose of orienting toward nonoperative or operative treatment.
Important prognostic factors of scapula fractures include the location, displacement, and presence of comminution [33]. Whereas for others fractures of the upper extremity, surgery is more often considered in the athlete population to achieve an earlier return to sport, fractures of the body of the scapula in athletes are almost always treated nonoperatively, since the robust surrounding musculature and vascularity allow for rapid restoration of ROM and function. In fact, exposure of fractures of the scapular body for surgical management may require a fair amount of muscle detachment, resulting in a longer recovery.
For these reasons, while no absolute consensus exists for the criteria for operative treatment of scapula fractures, [25] nonoperative treatment is preferred for the vast majority of fractures, and results in satisfactory healing and return to activity [24, 34]. Jones et al. [35] observed no significant difference in rates of union, range of motion, or ability to return to work between 2 groups of 31 patients treated either operatively or nonoperatively. When the two groups were matched by age, gender and occupation, the preoperative mean displacement, shortening and angulation were significantly greater in the operative group.
However, surgical treatments are still relevant for two specific conditions: a fracture of the neck of the scapula associated with a fracture of the clavicle creating an unstable floating shoulder, and a displaced fracture of the glenoid. As with other intra-articular fractures, fractures of the glenoid should be treated with anatomic internal fixation if they are displaced or associated with instability. Fracture of an anterior fragment of the glenoid rim involving more than 15–20% of the glenoid width is reported to be associated with recurrent anterior shoulder instability [36]. To avoid chronic joint dislocation, anatomic reduction and internal fixation are recommended [37]. Considering fixation of intra-articular fractures, arthroscopic assistance or all-arthroscopic procedures are being used more commonly for both upper and lower extremity joint fractures [38, 39]. Similar to fixation of tibial plateau or distal radius fracture, glenoid fractures are being increasingly treated with arthroscopic assistance [40–42] with different methods of fixation (suture anchors, screws, and others).
When evaluating fractures of the anterior glenoid rim in athletes, it is important to remember that the athletic population is particularly at risk for recurrent instability due to their participation in contact and non-contact sports. Not surprisingly, best outcomes seem to be achieved with internal fixation Glenoid rim fracture fixation using arthroscopic techniques provides an anatomic reduction with stable fixation and preserves soft tissues and vascularization. This technique is the most reliable to provide early rehabilitation and early return to sports without the risk of recurrent instability.
Regarding the floating shoulder, the concept of superior shoulder suspensory complex was coined to emphasize that the glenoid, coracoid, clavicle, and acromion form a ring-like structure along with the connecting ligaments and other soft tissues between these structures [43]. Disruption of two or more structures in this ring results in a complete interruption of the suspension between the upper extremity and the trunk. This represents an indication for a surgical fixation of the structures involved, including the scapula fracture.
Authors’ Preferences
We recommend nonoperative management for the vast majority of fractures of the scapular body. Uncommonly, fracture displacement with either severe glenoid medialization or marked body angulation is treated surgically with plate fixation. Exposure through separate incisions and interval may be particular beneficial in athletes to avoid extensive muscle dissection. When a fracture of the scapular body needs to be addressed surgically in the presence of a displaced fracture of the clavicle, the clavicle is typically fixed first. Regarding fractures of the glenoid rim, we have a low threshold to offer arthroscopically assisted internal fixation to decrease the risk of recurrent instability in the athletic population (Fig. 2).
Fig. 2.
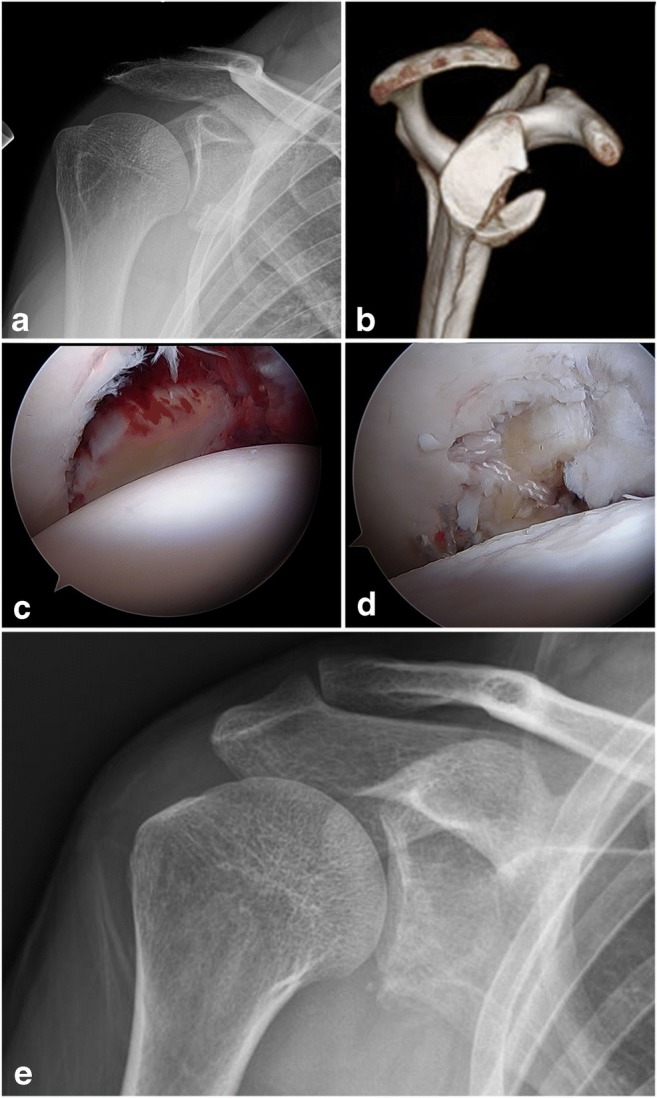
Arthroscopically assisted internal fixation of a displaced fracture of the anterior glenoid rim
Radial Head
Epidemiology
Radial head (RH) fractures account for 1.5% of long bone fractures in the adult population [54]. Miller et al. determined that most RH fractures occur from impact to the forearm with the elbow in ≤ 80 degrees of flexion [44]. In a study on 285 radial head or neck fractures, Ruchelsman et al. [45] identified that high-energy injuries, sports injuries and, falls from a height resulting in a RH fracture were significantly more common in male patients. They reported that Mason I type fractures were the most common fracture type. Direct blows or falls from height are often associated with Mason type I or II injuries [45].
In the case of radial head fractures, displacement does not always imply instability or need for surgery. Broberg et al. observed that many partial RH fractures with a displacement of ≥2 mm were inherently stable [46]. However, the elbow is particularly prone to stiffness after trauma, especially when immobilization is prolonged. Long-term clinical outcome studies support nonoperative treatment for nondisplaced, stable, and minimally displaced partial articular fractures of the RH [47, 48]. Guzzini et al. [49] reported on nonsurgical treatment of Mason type II radial head fractures in 52 athletes with mean age of 28.1 years (13 to 48 years). Patients were involved in various sports, including cycling, baseball, boxing, basket, rugby, tennis, and football. The treatment consisted of long arm cast immobilization in 90° of flexion for 2 weeks, followed by rehabilitation with active and passive range of motion exercises. At a mean follow-up of 36 months, the mean DASH score was excellent in 48 patients (92%); however, range of motion was slightly impaired compared to the opposite side. All patients returned to their previous activity at a mean time of 48.4 days after removing the cast (62.4 days after the injury).
Management of displaced and unstable radial head fractures is less controversial, as surgical treatment is often required. As long as the radial head can be preserved, internal fixation is usually preferred, especially for younger patients. During the last two decades, the design of radial head plates has been improved with the introduction of low-profile plates and mini plates in order to avoid hardware impingement or irritation. However, in 2011, Burkhart et al. investigated six RH plates in a cadaveric study [50] and reported no RH plate provided a perfect fit on the complex radial head anatomy and encouraged plate modifications, such as bending, to minimize interference of this hardware with the surrounding soft tissue. Morrey and Steinman [51] described a “low-profile fixation” of the RH and recommended obliquely oriented screws from the radial head into the shaft to avoid distal dissection of the soft tissues and placement of hardware in an already-constrained area adjacent to annular ligament and adjacent structures. A minimum of two screws in opposing planes is recommended to prevent rotational displacement.
Ring et al. [52] reported a high rate of fixation failure after ORIF involving more than three fragments of the RH or associated with dislocation of the elbow. For complex and potentially nonrepairable articular fractures, radial head arthroplasty is another viable surgical option. Currently, there is limited information regarding rates of implant loosening or capitellar wear in patients that continue to perform elbow-related sports activities after metallic radial head replacement. Dunn et al. [53] studied a group of 19 US military service members treated with a radial head replacement for isolated radial head fractures or associated with elbow dislocation. Although patients reported excellent subjective outcome scores, they observed a considerably higher rate of adverse outcomes (47%) in this very physically active group of patients compared to the general population (20%) [54]. This difference may be secondary to the high preinjury physical expectations in the military and athlete population. Adverse effects included loosening (1), heterotopic classification (5), and neurological sequelae (4). There were three reoperations at an average of 13 months postoperatively for heterotopic ossification or loosening. In an athletic population, especially with a high functional demand on the upper extremity, RH arthroplasty should be reserved for cases where the fractured radial head cannot be salvaged.
Radial head excision is another alternative for the treatment of comminuted and displaced RH fractures that cannot be fixed reliably. Despite satisfactory clinical results, there are concerning biomechanical consequences. Beingessner et al. [55] showed that radial head excision, even in elbows with intact ligaments, altered elbow kinematics. Patients considered for radial head resection must be counseled regarding the potential for subjective instability when playing sports as well as the high rate of reported radiographic osteoarthritis at long-term follow-up.
Authors’ Preferred Technique
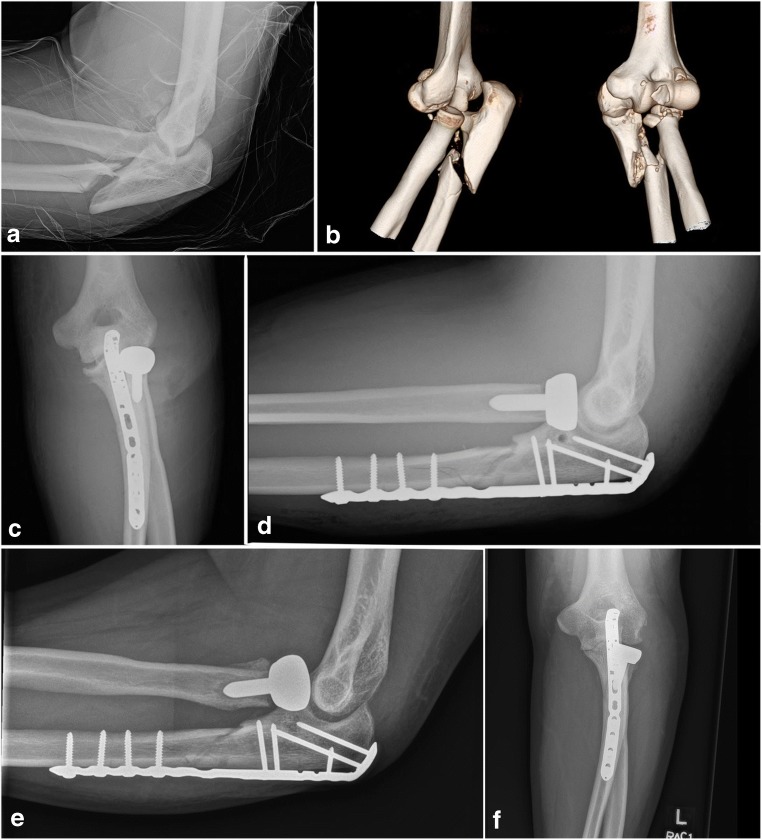
Our recommendations for RH fracture management in the athlete population mirror treatment recommendations in the non-athlete population. For minimally or nondisplaced fractures that are not associated with elbow instability, nonoperative management, with early restoration of ROM is recommended. In displaced fractures, particularly those associated with elbow instability, surgical management is recommended. For fixable fractures, headless compression screws are preferred (Fig. 3). Plates may lead to decreased forearm rotation and should be avoided when possible. In fracture-dislocations, with fragmentation of the radial head, arthroplasty and ligament repair are frequently required for stability. Patients should be informed about the lack of data regarding the long-term effects of a radial head replacement on the capitelum in patients actively involved in sports.
Fig. 3.

Internal fixation of a fractured radial head with elbow instability
Olecranon Fractures
Epidemiology
Fractures of the olecranon represent approximatively 10% of all upper extremity fractures, 20% of all proximal forearm fractures, [56] and 82% of proximal ulna fractures [57]. They range from simple nondisplaced fractures to complex transolecranon fracture-dislocations of the elbow.
Proximal ulna fractures commonly occur from a direct or indirect blow to the elbow following a fall from standing height [56, 58, 59]. Olecranon fractures are very rare in athletes, and few cases are reported in the literature. The most common olecranon injuries reported specifically in athletes are stress fractures of the olecranon.
Several treatment options are considered for the management of olecranon fracture, from nonoperative treatment to internal fixation using various techniques, including tension band wiring (TBW), intramedullary screws, and plate fixation. Plate fixation is preferred in the setting of articular comminution (not amenable to tension band construct). By definition, olecranon fractures are intra-articular injuries which require anatomical reduction or at least a normal surface reduction to avoid impingement of the trochlear notch. In addition, a stable fixation allowing early mobilization is required to avoid stiffness of the elbow. It has been established that stable fixation allowing early-term rehabilitation has a positive impact on elbow range of motion and improves clinical outcomes [60, 61]. This is even more critical for the management of young athletes to obtain an earlier return to sport at the same level.
The TBW, also called the AO technique, is still the most common fixation for displaced transverse fracture of the olecranon. The tension band, which is used to convert the distracting forces generated by the triceps into compressive forces, provides sufficiently strong fracture fixation to maintain a low rate of nonunion. However, the TBW is associated with other complications. Hardware prominence through the thin tissue covering the extensor surface of the elbow is frequently observed, and hardware removal seems to be more common than with the use of compression plate [62, 63].
Fractures due to direct trauma are usually more comminuted [64]. The goals remain identical to non-comminuted transverse fracture, but because of the specific pattern due to the comminution, plate fixation is recommended. In cases of comminuted fractures with bone loss, early motion initiated after TBW may be related to failures [65]. In a biomechanical model study, Gordon et al. showed that posterior plate fixation with an intramedullary screw was a more stable method of fixation for comminuted olecranon fractures when compared to dual plating or a single posterior plate without intramedullary screw [66].
Olecranon stress fractures (OSF) remain rare even in the athlete population. Athletes at risk include gymnasts and athletes who engage in overhead activities, like baseball players, javelin throwers, and weight lifters [67]. Characteristics of olecranon stress fractures are largely dependent on the age of patients and, even more so, the status of the physis. The olecranon physis usually fuses between the ages of 15 and 17, but it can be delayed until 19 years [68]. Furushima et al. [69] developed a classification system of olecranon stress fractures in baseball players, which consists of four stages based on the origin and direction of the fracture plane. They diagnosed associated UCL injuries in 71% to 95% of OSF. Ulnar stress fractures are usually caused by repetitive forces in adult overhead athletes secondary to repetitive micro trauma against the olecranon fossa or excessive tensile stress [70]. Posteromedial olecranon contact pressures can be significantly increased and the contact area decreased because of a medial UCL insufficiency [71].
Because of its atypical clinical presentation with unusual posterior elbow pain and no significant radiographic findings, the diagnosis of OSF is sometimes difficult [67]. Specific examination maneuvers such as the snapping extension test and the arm bar test may be useful to support the diagnosis. Additionally, specific imaging, such as computed tomographic (CT) scan or magnetic resonance imaging (MRI), is helpful. Although there are reports of success with nonoperative management [72], stable fixation that allows early active mobilization is often preferred for the high-demand overhead athlete population [73]. Internal fixation of OSF can be performed using several techniques, including a cannulated screw or plate osteosynthesis. Titanium implants are preferred in case postoperative MRI is considered. Paci et al. [67] reported particularly good outcomes and a high rate of success using screw fixation for refractory olecranon stress fractures in a series of 18 baseball athletes. Players were able to return to sport and perform at or above their former level of activity. In addition, repair or reconstruction of the medial UCL may be required in patients with underlying MCL incompetence in order to decrease pressure on the olecranon and reduce the risk of recurrence [70, 71].
Rehabilitation following an elbow injury or surgery is vital for restoration of normal function and rapid return to sport. To enhance restoration of full motion, muscular strength, and neuromuscular control, Wilk et al. [74] proposed a sequential and progressive multiphase approach. The rehabilitation protocol proceeds in four phases, beginning with immediate motion, an intermediate phase, followed by an advanced strengthening phase, and finally a return to activity to allow the athlete to progressively return to competition.
Authors’ Preferred Treatment
Our preference is to treat most displaced olecranon fractures in the athletes with plate fixation, which allows rigid fixation and potentially an earlier return to the practice of sports (Fig. 4). Plate removal is considered only for those athletes complaining of hardware discomfort, and delayed a minimum of 6 months after fixation. Olecranon stress fractures may be difficult to diagnose without advanced imaging studies. Internal fixation with titanium implants (typically screws, occasionally plates) provides good outcomes; not uncommonly, associated pathology (MCL insufficiency or posteromedial impingement) needs to be addressed as well as to optimize return to sports and decrease stress fracture recurrence.
Fig. 4.
Plate fixation and radial head arthroplasty of a complex olecranon fracture associated with radial head fracture
Medial Epicondyle Fracture
Epidemiology
The late timeline of skeletal maturity (15–16 years) confers weakness to epiphyseal plates, thus, the medial epicondyle remains more fragile in adolescents [75]. Being the last ossification center of the elbow makes the medial epicondyle of particular importance to the overhead throwing athletes [76, 77]. Medial epicondyle fractures account for approximatively 12% of all elbow fractures in adolescents [78].
The powerful muscles of the flexor pronator group, which originate from the medial epicondyle, and stabilize the medial elbow to valgus stress, likely contribute to this fracture type [79, 80]. The repetitive muscle activation regularly stresses the medial apophysis causing an inflammation. During overhead throwing motion, the maximum valgus stress is reported at 87° during the late cocking phase with a maximum valgus torque of 18–28 Nm [81]. Such high forces, across an already weak epiphyseal plate can explain apophysitis, stress fracture, or acute displaced fracture of the medial epicondyle in young athletes.
There is no consensus about an optimal treatment of medial epicondyle fractures. In the absence of obvious surgical indication including elbow instability, incarcerated fragment in the joint, open fracture or nerve injury, the main criteria involved in the therapeutic decision is the amount of displacement. Historically, displacement of less than 5 mm has been treated nonoperatively with acceptable results. However, some authors reduced the threshold to 2 mm for adolescent athletes (Redler, 2015 #443) [82]. Indeed, the importance of medial epicondyle in resisting valgus stress convinced several authors to consider fracture fixation, even in the setting of minimal displacement (Cain, 2003 #237) [73]. However, Lawrence et al. reported satisfactory functional outcomes and return to sports in 6 patients treated nonoperatively after medial epicondyle fracture with a mean displacement of 5.3 ± 2.0 mm [83].
Screw fixation is preferred to k-wire fixation to provide more stability and early motion. A medial approach is performed and the ulnar nerve protected before identification, reduction and fixation of the medial epicondyle. In a cohort of 14 adolescent athletes with displaced medial epicondyle fracture, Lawrence et al. achieved reduction with one screw and a washer. Passive range of motion was initiated after 3 weeks and physical therapy after 6 to 8 weeks if full range of motion had not been achieved. Including 8 overhead athletes, they reported excellent DASH scores with no limitation of performance and all patients returned to sport to the next appropriate higher level given their age [83].
Authors’ preferred treatment
Minimally and nondisplaced medial epicondyle fractures in young athletes are preferentially treated nonoperatively. We tolerate a displacement of up to 5 mm in the athlete population. This threshold exceeded, we prefer an open reduction through a medial approach and internal fixation with one screw. The addition of an offloading locking suture through the flexor pronator group and tied to the more proximal medial humerus can protect the screw repair. Early mobilization is initiated after 1 week of immobilization.
Conclusions
While fractures of the shoulder and elbow are not particularly common in upper extremity athletes, they can have profound implications. We favor a more aggressive surgical approach for many of these injuries in the athletic population, in particular with clavicle and humeral shaft fractures. Optimizing surgical technique to avoid soft tissue damage is critical. Radial head fractures and elbow instability must be carefully assessed, as elbow instability can preclude throwing and other overhead activities. Olecranon stress fractures must be ruled out when evaluating olecranon fractures, in particular in pitchers and overhead athletes.
Conflict of Interest
Marion Burnier and Jon D. Barlow declare no conflict of interest.
Joaquin Sanchez-Sotelo is a consultant for Stryker.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012–2014. Orthop J Sports Med. 2015;3(5):2325967115583653. doi: 10.1177/2325967115583653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conte S, Camp CL, Dines JS. Injury trends in major league baseball over 18 seasons: 1998–2015. Am J Orthop (Belle Mead NJ) 2016;45(3):116–123. [PubMed] [Google Scholar]
- 3.Robinson CM. Fractures of the clavicle in the adult: epidemiology and classification. J Bone Joint Surg Br Vol. 1998;80(3):476–484. doi: 10.1302/0301-620X.80B3.8079. [DOI] [PubMed] [Google Scholar]
- 4.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elb Surg. 2002;11(5):452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 5.Aitken SA, Hutchison JD, McQueen MM, Court-Brown CM. The importance of epidemiological fracture data: injury epidemiology for the non-epidemiologist. Bone Joint J. 2014;96–b(7):863–867. doi: 10.1302/0301-620X.96B7.34023. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33(8):1142–1146. doi: 10.1177/0363546505274718. [DOI] [PubMed] [Google Scholar]
- 7.Robertson GA, Wood AM, Bakker-Dyos J, Aitken SA, Keenan AC, Court-Brown CM. The epidemiology, morbidity, and outcome of soccer-related fractures in a standard population. Am J Sports Med. 2012;40(8):1851–1857. doi: 10.1177/0363546512448318. [DOI] [PubMed] [Google Scholar]
- 8.Bagherian S, Rahnama N. Epidemiology of injury in professional cyclists. Br J Sports Med. 2010;44(Suppl 1):i4–ii. doi: 10.1136/bjsm.2010.078725.11. [DOI] [Google Scholar]
- 9.Nishimi AY, Belangero PS, Mesquita RS, Andreoli CV, Pochini AC, Ejnisman B. Frequency and risk factors of clavicle fractures in professional cyclists. Acta Ortop Bras. 2016;24(5):240–242. doi: 10.1590/1413-785220162405157391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furey MJ, Zdero R, McKee MD. Clavicular refracture at the site of angular malunion in young athletes. J Orthop Trauma. 2017;31(4):e130–e1e2. doi: 10.1097/BOT.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 11.De Giorgi S, Notarnicola A, Tafuri S, Solarino G, Moretti L, Moretti B. Conservative treatment of fractures of the clavicle. BMC Res Notes. 2011;4:333. doi: 10.1186/1756-0500-4-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elb Surg. 2006;15(2):191–194. doi: 10.1016/j.jse.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 13.McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. JBJS. 2012;94(8):675–684. doi: 10.2106/JBJS.J.01364. [DOI] [PubMed] [Google Scholar]
- 14.Witzel K. Intramedullary osteosynthesis in fractures of the mid-third of the clavicle in sports traumatology. Z Orthop Unfall. 2007;145(5):639–642. doi: 10.1055/s-2007-965616. [DOI] [PubMed] [Google Scholar]
- 15.Meisterling SW, Cain EL, Fleisig GS, Hartzell JL, Dugas JR. Return to athletic activity after plate fixation of displaced midshaft clavicle fractures. Am J Sports Med. 2013;41(11):2632–2636. doi: 10.1177/0363546513501494. [DOI] [PubMed] [Google Scholar]
- 16.Ranalletta M, Rossi LA, Piuzzi NS, Bertona A, Bongiovanni SL, Maignon G. Return to sports after plate fixation of displaced midshaft clavicular fractures in athletes. Am J Sports Med. 2015;43(3):565–569. doi: 10.1177/0363546514559913. [DOI] [PubMed] [Google Scholar]
- 17.Verborgt O, Pittoors K, Van Glabbeek F, Declercq G, Nuyts R, Somville J. Plate fixation of middle-third fractures of the clavicle in the semi-professional athlete. Acta Orthop Belg. 2005;71(1):17–21. [PubMed] [Google Scholar]
- 18.Ranalletta M, Rossi LA, Barros H, Nally F, Tanoira I, Bongiovanni SL, Maignon GD. Minimally invasive double-button fixation of displaced lateral clavicular fractures in athletes. Am J Sports Med. 2017;45(2):462–467. doi: 10.1177/0363546516666816. [DOI] [PubMed] [Google Scholar]
- 19.Ekholm R, Adami J, Tidermark J, Hansson K, Tornkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br Vol. 2006;88(11):1469–1473. doi: 10.1302/0301-620X.88B11.17634. [DOI] [PubMed] [Google Scholar]
- 20.Werner SL, Suri M, Guido JA, Jr, Meister K, Jones DG. Relationships between ball velocity and throwing mechanics in collegiate baseball pitchers. J Shoulder Elb Surg. 2008;17(6):905–908. doi: 10.1016/j.jse.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Singh AK, Narsaria N, Seth RR, Garg S. Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates. J Orthop Traumatol. 2014;15(2):117–122. doi: 10.1007/s10195-014-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahajan AS, Kim YG, Kim JH, D'sa P, Lakhani A, Ok HS. Is anterior bridge plating for mid-shaft humeral fractures a suitable option for patients predominantly involved in overhead activities? A functional outcome study in athletes and manual laborers. Clin Orthop Surg. 2016;8(4):358–366. doi: 10.4055/cios.2016.8.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Usman J, McIntosh AS, Quarrie K, Targett S. Shoulder injuries in elite rugby union football matches: epidemiology and mechanisms. J Sci Med Sport. 2015;18(5):529–533. doi: 10.1016/j.jsams.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Goss TP. Scapular fractures and dislocations: diagnosis and treatment. J Am Acad Orthop Surg. 1995;3(1):22–33. doi: 10.5435/00124635-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br Vol. 1984;66(5):725–731. doi: 10.1302/0301-620X.66B5.6501369. [DOI] [PubMed] [Google Scholar]
- 26.Thompson DA, Flynn TC, Miller PW, Fischer RP. The significance of scapular fractures. J Trauma. 1985;25(10):974–977. doi: 10.1097/00005373-198510000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures. Incidence and classification of 338 fractures. Acta Orthop Scand. 1995;66(5):395–397. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 28.Cole PA, Gauger EM, Schroder LK. Management of scapular fractures. J Am Acad Orthop Surg. 2012;20(3):130–141. doi: 10.5435/JAAOS-20-03-130. [DOI] [PubMed] [Google Scholar]
- 29.Schandelmaier P, Blauth M, Schneider C, Krettek C. Fractures of the glenoid treated by operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg Br Vol. 2002;84(2):173–177. doi: 10.1302/0301-620X.84B2.12357. [DOI] [PubMed] [Google Scholar]
- 30.Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surg Am. 1993;75(4):479–484. doi: 10.2106/00004623-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Harvey E, Audige L, Herscovici D, Jr, Agel J, Madsen JE, Babst R, et al. Development and validation of the new international classification for scapula fractures. J Orthop Trauma. 2012;26(6):364–369. doi: 10.1097/BOT.0b013e3182382625. [DOI] [PubMed] [Google Scholar]
- 32.Neuhaus V, Bot AG, Guitton TG, Ring DC, Abdel-Ghany MI, Abrams J, et al. Scapula fractures: interobserver reliability of classification and treatment. J Orthop Trauma. 2014;28(3):124–129. doi: 10.1097/BOT.0b013e31829673e2. [DOI] [PubMed] [Google Scholar]
- 33.Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res. 1991(269):174–80. [PubMed]
- 34.DePalma A. Fractures of the scapula. Surgery of the shoulder. Philadelphia: Lippincott; 1983. [Google Scholar]
- 35.Jones CB, Sietsema DL. Analysis of operative versus nonoperative treatment of displaced scapular fractures. Clin Orthop Relat Res. 2011;469(12):3379–3389. doi: 10.1007/s11999-011-2016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82(1):35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Rockwood CAMF. The scapula. The shoulder. Philadelphia: WB Saunders; 1990. [Google Scholar]
- 38.Chan YS, Chiu CH, Lo YP, Chen AC, Hsu KY, Wang CJ, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24(7):760–768. doi: 10.1016/j.arthro.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 39.Varitimidis SE, Basdekis GK, Dailiana ZH, Hantes ME, Bargiotas K, Malizos K. Treatment of intra-articular fractures of the distal radius: fluoroscopic or arthroscopic reduction? J Bone Joint Surg Br Vol. 2008;90(6):778–785. doi: 10.1302/0301-620X.90B6.19809. [DOI] [PubMed] [Google Scholar]
- 40.Bauer T, Abadie O, Hardy P. Arthroscopic treatment of glenoid fractures. Arthroscopy. 2006;22(5):569.e1–569.e6. doi: 10.1016/j.arthro.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Carro LP, Nunez MP, Llata JI. Arthroscopic-assisted reduction and percutaneous external fixation of a displaced intra-articular glenoid fracture. Arthroscopy. 1999;15(2):211–214. doi: 10.1053/ar.1999.v15.015021. [DOI] [PubMed] [Google Scholar]
- 42.Taverna E, Guarrella V, Freehill MT, Garavaglia G. Arthroscopic reduction with endobutton fixation for glenoid fracture. Joints. 2017;5(2):127–130. doi: 10.1055/s-0037-1603675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7(2):99–106. doi: 10.1097/00005131-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Amis AA, Miller JH. The mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury. 1995;26(3):163–168. doi: 10.1016/0020-1383(95)93494-3. [DOI] [PubMed] [Google Scholar]
- 45.Ruchelsman DE, Christoforou D, Jupiter JB. Fractures of the radial head and neck. J Bone Joint Surg Am. 2013;95(5):469–478. doi: 10.2106/JBJS.J.01989. [DOI] [PubMed] [Google Scholar]
- 46.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669–674. doi: 10.2106/00004623-198668050-00005. [DOI] [PubMed] [Google Scholar]
- 47.Akesson T, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg Am. 2006;88(9):1909–1914. doi: 10.2106/JBJS.E.01052. [DOI] [PubMed] [Google Scholar]
- 48.Herbertsson P, Josefsson PO, Hasserius R, Karlsson C, Besjakov J, Karlsson M. Uncomplicated mason type-II and III fractures of the radial head and neck in adults. A long-term follow-up study. J Bone Joint Surg Am Vol. 2004;86-a(3):569–574. doi: 10.2106/00004623-200403000-00016. [DOI] [PubMed] [Google Scholar]
- 49.Guzzini M, Vadala A, Agro A, Di Sanzo V, Pironi D, Redler A, et al. Nonsurgical treatment of Mason type II radial head fractures in athletes. A retrospective study. G Chir. 2017;37(5):200–205. doi: 10.11138/gchir/2016.37.5.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burkhart KJ, Nowak TE, Kim YJ, Rommens PM, Muller LP. Anatomic fit of six different radial head plates: comparison of precontoured low-profile radial head plates. J Hand Surg. 2011;36(4):617–624. doi: 10.1016/j.jhsa.2010.12.028. [DOI] [PubMed] [Google Scholar]
- 51.Smith AM, Morrey BF, Steinmann SP. Low profile fixation of radial head and neck fractures: surgical technique and clinical experience. J Orthop Trauma. 2007;21(10):718–724. doi: 10.1097/BOT.0b013e31812e5168. [DOI] [PubMed] [Google Scholar]
- 52.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am Vol. 2002;84–a(10):1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Dunn JC, Kusnezov NA, Koehler LR, Eisenstein ED, Kilcoyne KG, Orr JD, et al. Radial head arthroplasty in the active duty military service member with minimum 2-year follow-up. J Hand Surg. 2017;42(8):660.e1–660.e7. doi: 10.1016/j.jhsa.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 54.Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5(1):1–10. doi: 10.5435/00124635-199701000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Beingessner DM, Dunning CE, Gordon KD, Johnson JA, King GJ. The effect of radial head excision and arthroplasty on elbow kinematics and stability. JBJS. 2004;86(8):1730–1739. doi: 10.2106/00004623-200408000-00018. [DOI] [PubMed] [Google Scholar]
- 56.Court-Brown CM, Aitken SA, Forward D, O’Toole RV. The epidemiology of adult fractures. Philadelphia: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 57.Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012;43(3):343–346. doi: 10.1016/j.injury.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 58.Karlsson MK, Hasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon: a 15- to 25-year follow up of 73 patients. Clin Orthop Relat Res. 2002;403:205–212. doi: 10.1097/00003086-200210000-00030. [DOI] [PubMed] [Google Scholar]
- 59.Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin N Am. 2008;39(2):229–236. doi: 10.1016/j.ocl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 60.Buijze GA, Blankevoort L, Tuijthof GJ, Sierevelt IN, Kloen P. Biomechanical evaluation of fixation of comminuted olecranon fractures: one-third tubular versus locking compression plating. Arch Orthop Trauma Surg. 2010;130(4):459–464. doi: 10.1007/s00402-009-0980-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cabanella ME, Morrey BF. Fractures of the proximal ulna and olecranon. The elbow and its disorders. Philadelphia: WB Saunders; 1993. [Google Scholar]
- 62.Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res. 1992;285:229–235. [PubMed] [Google Scholar]
- 63.Wolfgang G, Burke F, Bush D, Parenti J, Perry J, LaFollette B, et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res. 1987;224:192–204. [PubMed] [Google Scholar]
- 64.Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575–581. doi: 10.1016/j.injury.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 65.Anderson ML, Larson AN, Merten SM, Steinmann SP. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21(6):386–393. doi: 10.1097/BOT.0b013e3180ce831e. [DOI] [PubMed] [Google Scholar]
- 66.Gordon MJ, Budoff JE, Yeh ML, Luo ZP, Noble PC. Comminuted olecranon fractures: a comparison of plating methods. J Shoulder Elb Surg. 2006;15(1):94–99. doi: 10.1016/j.jse.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 67.Paci JM, Dugas JR, Guy JA, Cain EL, Jr, Fleisig GS, Hurst C, Wilk KE, Andrews JR. Cannulated screw fixation of refractory olecranon stress fractures with and without associated injuries allows a return to baseball. Am J Sports Med. 2013;41(2):306–312. doi: 10.1177/0363546512469089. [DOI] [PubMed] [Google Scholar]
- 68.Maffulli N, Chan D, Aldridge MJ. Overuse injuries of the olecranon in young gymnasts. J Bone Joint Surg Br Vol. 1992;74(2):305–308. doi: 10.1302/0301-620X.74B2.1544975. [DOI] [PubMed] [Google Scholar]
- 69.Furushima K, Itoh Y, Iwabu S, Yamamoto Y, Koga R, Shimizu M. Classification of olecranon stress fractures in baseball players. Am J Sports Med. 2014;42(6):1343–1351. doi: 10.1177/0363546514528099. [DOI] [PubMed] [Google Scholar]
- 70.Griggs SM, Weiss AP. Bony injuries of the wrist, forearm, and elbow. Clin Sports Med. 1996;15(2):373–400. [PubMed] [Google Scholar]
- 71.Ahmad CS, Park MC, Elattrache NS. Elbow medial ulnar collateral ligament insufficiency alters posteromedial olecranon contact. Am J Sports Med. 2004;32(7):1607–1612. doi: 10.1177/0363546503263149. [DOI] [PubMed] [Google Scholar]
- 72.Nuber GW, Diment MT. Olecranon stress fractures in throwers. A report of two cases and a review of the literature. Clin Orthop Relat Res. 1992;278:58–61. [PubMed] [Google Scholar]
- 73.Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 74.Wilk KE, Reinold MM, Andrews JR. Rehabilitation of the thrower’s elbow. Tech Hand Upper Extrem Surg. 2003;7(4):197–216. doi: 10.1097/00130911-200312000-00011. [DOI] [PubMed] [Google Scholar]
- 75.Gregory B, Nyland J. Medial elbow injury in young throwing athletes. Muscles Ligaments Tendons J. 2013;3(2):91–100. doi: 10.32098/mltj.02.2013.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen FS, Diaz VA, Loebenberg M, Rosen JE. Shoulder and elbow injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2005;13(3):172–185. doi: 10.5435/00124635-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 77.Sabick MB, Torry MR, Lawton RL, Hawkins RJ. Valgus torque in youth baseball pitchers: a biomechanical study. J Shoulder Elb Surg. 2004;13(3):349–355. doi: 10.1016/j.jse.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 78.Wilkins KE. Fractures involving the medial epicondylar apophysis. Fractures in children. Philadelphia: JB Lippincott; 1991. [Google Scholar]
- 79.Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9(2):99–113. doi: 10.5435/00124635-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 80.Miller CD, Savoie FH., 3rd Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg. 1994;2(5):261–269. doi: 10.5435/00124635-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 81.Sabick MB, Torry MR, Kim Y-K, Hawkins RJ. Humeral torque in professional baseball pitchers. Am J Sports Med. 2004;32(4):892–898. doi: 10.1177/0363546503259354. [DOI] [PubMed] [Google Scholar]
- 82.Redler LH, Dines JS. Elbow trauma in the athlete. Hand Clin. 2015;31(4):663–681. doi: 10.1016/j.hcl.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 83.Lawrence JT, Patel NM, Macknin J, Flynn JM, Cameron D, Wolfgruber HC, et al. Return to competitive sports after medial epicondyle fractures in adolescent athletes: results of operative and nonoperative treatment. Am J Sports Med. 2013;41(5):1152–1157. doi: 10.1177/0363546513480797. [DOI] [PubMed] [Google Scholar]