Abstract
Context:
Nurses play an inevitable role in providing compassionate care and support to dying patients and their families. However, it has been a bone of contention that whether the nursing curriculum is sufficiently set to achieve this goal.
Aims:
The primary objective of this study is to assess the attitude of nursing students attending a private nursing school in Central Travancore region toward the care of dying using the Frommelt Attitude Toward Care of the Dying Scale Form-B (FATCOD-B).
Methodology:
FATCOD-B was introduced among 146 participants and an arbitrary cutoff of 65% of the total score were chosen with those scoring more than that were assumed to have a positive attitude. A principal component analysis was done to identify the key constructs and mean score of the items within these identified constructs were calculated.
Results:
The positive attitude toward dying was shown by 39% of participants. Most of the students’ responses were averaging toward the option uncertain. A statistically significant increase in mean score by 3.15 (P = 0.02) was noticed among those who completed palliative care postings. The keys constructs identified included perception toward the end-of-life care, emotional engagement with the dying, and perceptions with respect to professional engagement with subgroup analysis showing an average mean score (standard deviation) of 4.36 (0.144), 2.25 (0.874), and 3.39 (0.85), respectively.
Conclusion:
The revision of the current curriculum incorporating more palliative care postings with specific attention toward handling emotional engagement with the dying may help in developing a positive attitude.
Keywords: Care of dying, Frommelt Attitude Toward Care of the Dying Scale Form-B, nursing curriculum, palliative care
INTRODUCTION
Nurses play a significant role in the delivery of palliative care services to those suffering from life-threatening illnesses by assessing their needs and providing services not just to the patients but also to the families McIntyre.[1] Although palliative care is a part of undergraduate curriculum, practical exposure to care of those with chronic debilitating conditions and care of dying are usually quite minimal. There is also dearth of literature in Indian context assessing the nursing students’ attitude toward palliative care and end-of-life care. The primary objective of the proposed study was to assess the attitude toward the care of dying by the nursing students using the Frommelt Attitude Toward Care of the Dying Scale Form-B (FATCOD-B).[2] FATCOD-B is a Likert-type questionnaire with 30 items, each scored from 1 to 5 in the increasing order of agreeability, 1 being strongly disagree and 5 being strongly agree. This is a commonly used tool to assess the influence of education in developing a positive attitude toward care of dying, among students belonging to a variety of specialties of the study.[2,3] The reliability of the tool was found to be adequate (Pearson's coefficient of 0.9269) with a high content validity; interrater agreement was 1.00 with good overall interclass correlation.[2,3,4]
METHODOLOGY
All the nursing students attending the Bachelor of Science in Nursing (BSc Nursing), a 4-year undergraduate program and Masters of Science in Nursing (MSc Nursing), a 2-year masters course, in a private Nursing School in the Central Travancore region of Kerala are recruited for the study. The 1st-year BSc nursing students were excluded from the study since they were completely new to the field of medicine, thus making the total number of students eligible for participating in the study as 166. Since the questionnaire only had serial numbers with nil option for writing names, anonymity of the participant was maintained. On a prefixed day, questionnaires were distributed to each batch of students in their respective classes along with a written informed consent. Each participant was given a time period of 30 min to complete the questionnaire. Participation was purely voluntary and those who did not return the questionnaire after half an hour were considered to be nonconsenters for the study. Due to time constraints, those who were absent on the day of the study were also not approached on a later date. Apart from FATCOD-B and basic information such as course attending and clinical exposure, the questionnaire also included the following additional questions:
Ever involved in preparing a deceased person body
Ever cared for a dying person
Ever cared for a dying person of your family or close friend
Whether completed clinical posting in the palliative care ward.
The data were entered using Epi Info version 7, a data entry software developed by the Center for Disease Control and Prevention in Atlanta, Georgia and were analyzed using SPSS statistics version 24 developed by IBM Corporation, Armonk, New York. The minimum and maximum scores that can be attained using FATCOD-B were 30 and 150, respectively. An arbitrary cut off of 65% and more of the total attainable score by each participant, which is 150, was taken to affirm that one has a positive attitude. Descriptive analysis was done and the following percentages were calculated:
Those attending different courses
Those involved in death care
Those completed the palliative care posting and
Those with positive attitude toward dying.
The mean FATCOD-B score with the 95% confidence interval was calculated. For each item in the FATCOD, mean was calculated following which the overall mean of the items means was calculated. A principal component analysis (PCA) with oblimin rotation and scree test was carried out for data reduction to find out the key constructs identified by selecting those items with pattern matrix value of more than 0.3. Within each identified constructs, overall mean of the item means within each construct were calculated.
RESULTS
A total of 146 students participated in the study of which 141 were BSc Nursing students and the rest 5 were doing their MSc Nursing degree. The rest of the students were either absent on the day of study or did not return the questionnaire. The general characteristics of the participants were summarized in Table 1.
Table 1.
General characteristics of the study participants
| Characteristics | n (%) |
|---|---|
| Course attending | |
| BSc | 141 (96.6) |
| MSc | 5 (3.4) |
| Clinical exposure (years) | |
| ≤3 | 109 (74.7) |
| >3 | 37 (25.3) |
| Completed posting in palliative care unit | |
| Yes | 50 (34.2) |
| No | 96 (65.8) |
| Ever involved in the preparation of deceased person’s body | |
| Yes | 117 (80.1) |
| No | 29 (19.9) |
| Ever cared for a dying person | |
| Yes | 132 (90.4) |
| No | 14 (9.6) |
| Ever cared for a dying member of your family or close friend | |
| Yes | 45 (30.8) |
| No | 101 (69.2) |
The mean FATCOD score (confidence interval) obtained in the study was 95.81 (94.48–97.14), with scores ranging between 73 and 126. Total scores obtained by the participants followed a normal distribution curve, allowing the application of parametric tests. The mean score attained by BSc students was 95.75, whereas the 5 MSc participants obtained a mean score of 97.4. In Figure 1, the difference in mean FATCOD score obtained by those ever cared for dying patients in comparison to those who have not is given.
Figure 1.
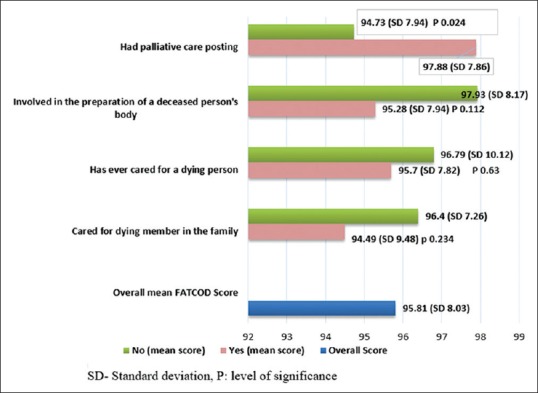
Mean Frommelt Attitude Toward Care of the Dying Scale Form score difference between those ever cared for dying and those who have not.
It was found that 39% (95% confidence interval: 31%–47%) of the participants had a positive attitude toward dying. The overall mean of the items averaged between 3.15 and 3.23. Through the principal component analysis, three components were decided upon after analyzing the scree plot. The Kaiser–Meyer–Olkin measure of sampling adequacy score was 0.708 with a significant Bartlett's Test of Sphericity (<0.001). Together these three identified components explained 45% of the total variance. After analyzing, the pattern matrix values and the respective items in the FATCOD the three components were deduced as perception toward end-of-life care, emotional engagement with the dying, and perceptions with respect to the professional engagement. The various items in the questionnaire which showed a pattern matrix value of more than 0.3 for each of the aforementioned components, with their respective FATCOD item mean were shown in Table 2.
Table 2.
Principal component analysis with average mean values of each item
| Items | Mean±SD | Perception toward end-of-life care | Emotional engagement with the dying | Perceptions with respect to professional engagement |
|---|---|---|---|---|
| Families need emotional support to accept the behavioral changes of the dying person | 4.49±0.816 | 0.724 | ||
| Families should be concerned about helping their dying member make the best of his/her remaining life | 4.42±0.759 | 0.688 | ||
| It is beneficial for the dying person to verbalize his/her feelings | 4.46±0.789 | 0.652 | ||
| It is possible for nurses to help patients prepare for death | 4.14±0.884 | 0.622 | ||
| Families should maintain as normal an environment as possible for their dying member | 4.30±0.890 | 0.531 | ||
| I would not want to be assigned to care for a dying person | 1.39±0.689 | 0.402 | ||
| I would be upset when the dying person I was caring for gave up hope of getting better | 3.17±1.376 | 0.672 | ||
| The length of time required to give nursing care to a dying person would frustrate me | 2.14±1.076 | 0.662 | ||
| I am afraid to become friends with the dying person | 1.72±0.828 | 0.458 | ||
| As a patient nears death, the nurse should withdraw from his/her involvement with the person | 1.58±0.901 | 0.449 | ||
| There are times when death is welcomed by the dying person | 3.47±0.998 | 0.428 | ||
| The nurse should not be the one to talk about death with the dying person | 2.95±1.408 | −0.463 | ||
| Family members who stay close to a dying person often interfere with the professional’s job with the patient | 2.88±1.092 | −0.675 | ||
| Nursing care should extend to the family of the dying person | 4.36±0.892 | −0.602 | ||
| I would be uncomfortable talking about impending death with the dying person | 2.53±1.282 | −0.569 | ||
| Nursing care for the patients family should continue throughout the period of grief and bereavement | 4.26±0.933 | −0.568 | ||
| Mean±SD | 4.36±0.144 | 2.25±0.874 | 3.39±0.85 |
SD: Standard deviation
DISCUSSION
This is a study conducted among the nursing students, both bachelors and masters, attending a private nursing school in Kerala to understand their attitude regarding care of those who are dying. The results show that only 39% ± 8% showed a positive attitude toward the care of dying with a mean score of 95.81. Although much data are not available in this regard from the Indian context, figures from Western studies give us a mixed picture. Grubb and Arthur in their study conducted in the United Kingdom found that nearly 92% of their participant had a positive attitude[5] probably because of the lower cutoff score used for the FATCOD. Meanwhile, Jafari et al. in their study conducted in Iran had found a negative to neutral attitude toward the care of dying.[6] Similarly, another study from Palestine also showed a low attitude with a mean FATCOD score similar to the current study, 96.96 ± 8.30.[7]
When looked into the various randomly chosen factors that could help in developing a positive attitude such as involvement in care of dying, either a patient or a family member, involvement in the preparation of the body of a deceased person, and posting in a palliative care setting; it has been found that only the factor posting in a palliative care setting had caused a statistically significant increase in the mean value of the participants. The mean value of the FATCOD score of those having the palliative posting was higher by 3.15 (P = 0.024) when compared those did not have the posting. These findings are congruent with the findings from other studies which showed a positive association between knowledge in palliative care and better care of the dying patient.[8,9] A systematic review done to understand the effect of training nurses in palliative care through conventional methods of teaching, such as didactic sessions, workshops, and scenario-based learning, found that these methods were unlikely to promote better patient outcomes.[10] Even in our study, the mean score of those who were doing their masters, who are expected to have better knowledge about palliative care, were more by 1.65 than those who were doing their bachelors and this difference was not statistically significant. This invariably suggests that it is not sufficient that palliative care is incorporated in the curriculum and it is equally important that the students have practical, hands-on, compulsory postings in a palliative care setting to develop a positive attitude toward the care of dying.
Through PCA, the study identified three main components which will help in understanding the attitude of the students in a better way, thereby providing an insight toward the area that requires more focus. With respect to their perspectives regarding end-of-life care, the students appeared to have positive attitude with respect to the involvement of family members in improving the quality of remaining days of the patient and in providing a normal environment as much as possible. They also seemed to have identified the role of nurses in helping the patients in verbalizing their thoughts and also to help them to prepare for their death. The mean of the individual items that contribute to this component average toward 4.36 revealing the positive attitude of the students. These perceptions by the students were consistent with the responsibilities identified by professional bodies like Royal College of Nursing as the role of nurses in end-of-life care.[11]
When analyzed the items within the second component, emotional engagement with the dying patients, the attitude was clearly negative. The average mean score obtained in the items within the component was 2.25. They were more in favor of not having a dying patient being assigned for caregiving probably because death often upset the caregivers. With respect to the third component, perception with respect to the professional engagement, the average mean score of the items were 3.39 suggesting a “neutral” or “do not know” attitude. The item scores suggest that the student nurses were unsure of the nurses’ expected roles in end-of-life care and bereavement support. Death is an inevitable process and the act of dealing with it is a personal experience and not all are adequately prepared for it. Studies have shown that exposure to death would evoke overwhelming emotional and psychological distress among nurses.[12,13,14] It is important that core education strategies related to the care of dying should be incorporated into the training of health-care workers. This is particularly relevant in the context of Kerala where palliative care activities have taken an altruistic turn with people irrespective of their professional background have gotten involved in the establishing and spearheading its activities. When there is a baseline coverage of such services exist in society, those in the health profession should definitely be trained in palliative and end-of-life care to match up with the public perceptions and also to remove misconceptions that prevail within the health field.
Kerala government through its “Palliative Care Project” initiative is targeting a complete palliative care coverage of the state.[15,16] It is the only state in India having a palliative care policy.[16] The service delivery is expected to be under the leadership of the government primary health centers and local self-government.[16] However, the majority of the nursing training and education has been provided by the private sector.[17] Although many community-based organizations are actively involved in palliative care delivery, data regarding the involvement and the expertise of the private sector hospitals providing nursing education in palliative care is not available. If a particular private nursing school does not have the adequate expertise, the students can complete their posting from another center which provides such services. However, the government must come up with guidelines for choosing such centers so that the quality in nursing education with respect to palliative care and bereavement support would not get compromised.
Limitations
Since the study included students from a single nursing school, the generalizability of the findings may not be feasible. The nursing school was part of the hospital which had established palliative care settings with inpatient care, outpatient care, and home care facilities. Likewise, all the students had regular postings in this palliative care ward. This might have an influence on the participants in developing a positive attitude toward the care of dying. A study result from another school which does not have a palliative care facility may show a lower percentage having positive attitude.
CONCLUSION
In an aging society like Kerala, which has experienced an epidemiological shift toward chronic diseases palliative care is an inevitable part of medical care. Nurses play a vital role in the effective implementation of palliative care services. It is important to analyze whether the nursing curriculum is adequately modified to face this challenge. The current study which looked into the attitude of the nursing students toward the care of dying is one such attempt. Although the generalizability of the study is questionable since it is a single-center study, the findings it put forward is worth considering and could lead to further research in this field.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lugton J, McIntyre R. Palliative Care: The Nursing Role. 2nd ed. London: Elsevier Health Sciences; 2005. p. 434. [Google Scholar]
- 2.Frommelt KH. Attitudes toward care of the terminally ill: An educational intervention. Am J Hosp Palliat Care. 2003;20:13–22. doi: 10.1177/104990910302000108. [DOI] [PubMed] [Google Scholar]
- 3.Mastroianni C, Piredda M, Taboga C, Mirabella F, Marfoli E, Casale G, et al. Frommelt attitudes toward care of the dying scale form B: Psychometric testing of the Italian version for students. Omega (Westport) 2015;70:227–50. doi: 10.1177/0030222815568944. [DOI] [PubMed] [Google Scholar]
- 4.Wang LP, Li YJ, Yan WZ, Li GM. Development and psychometric testing Chinese version of the frommelt attitude toward care of the dying scale, form B in nurses and nursing students. J Cancer Educ. 2016;31:123–30. doi: 10.1007/s13187-015-0810-7. [DOI] [PubMed] [Google Scholar]
- 5.Grubb C, Arthur A. Student nurses’ experience of and attitudes towards care of the dying: A cross-sectional study. Palliat Med. 2016;30:83–8. doi: 10.1177/0269216315616762. [DOI] [PubMed] [Google Scholar]
- 6.Jafari M, Rafiei H, Nassehi A, Soleimani F, Arab M, Noormohammadi MR, et al. Caring for dying patients: Attitude of nursing students and effects of education. Indian J Palliat Care. 2015;21:192–7. doi: 10.4103/0973-1075.156497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abu-El-Noor NI, Abu-El-Noor MK. Attitude of Palestinian nursing students toward caring for dying patients: A call for change in health education policy. J Holist Nurs. 2016;34:193–9. doi: 10.1177/0898010115596492. [DOI] [PubMed] [Google Scholar]
- 8.Ayed A, Sayej S, Harazneh L, Fashafsheh I, Eqtait F. The nurses’ knowledge and attitudes towards the palliative care. J Educ Pract. 2015;6:91–9. [Google Scholar]
- 9.Wilson O, Avalos G, Dowling M. Knowledge of palliative care and attitudes towards nursing the dying patient. Br J Nurs. 2016;25:600–5. doi: 10.12968/bjon.2016.25.11.600. [DOI] [PubMed] [Google Scholar]
- 10.Anstey S, Powell T, Coles B, Hale R, Gould D. Education and training to enhance end-of-life care for nursing home staff: A systematic literature review. BMJ Support Palliat Care. 2016;6:353–61. doi: 10.1136/bmjspcare-2015-000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Royal College of Nursing. Roles and Responsibilities [Internet]. Get. It Right Everytime Fundam. Nurs Care End Life. 2015. [Cited 2018 Jun 29]. Available from: http://www.rcnendoflife.org.uk/my-role .
- 12.Cevik B, Kav S. Attitudes and experiences of nurses toward death and caring for dying patients in Turkey. Cancer Nurs. 2013;36:E58–65. doi: 10.1097/NCC.0b013e318276924c. [DOI] [PubMed] [Google Scholar]
- 13.Hopkinson JB, Hallett CE, Luker KA. Caring for dying people in hospital. J Adv Nurs. 2003;44:525–33. doi: 10.1046/j.0309-2402.2003.02836.x. [DOI] [PubMed] [Google Scholar]
- 14.Zambrano SC, Chur-Hansen A, Crawford GB. The experiences, coping mechanisms, and impact of death and dying on palliative medicine specialists. Palliat Support Care. 2014;12:309–16. doi: 10.1017/S1478951513000138. [DOI] [PubMed] [Google Scholar]
- 15.Government of Kerala. Palliative Care. 2018. [Cited 2018 Jun 28]. Available from: https:// 13 www.kerala.gov.in/palliative-care .
- 16.National Health Mission. Palliative Care Project. National Health Mission 14 Arogyakeralam. 2018. [Cited 2018 Jun 28]. Available from: http://www.arogyakeralam.gov. 15 in/index.php/special-initiaves/palliative-careproject .
- 17.Evans C, Razia R, Cook E. Building nurse education capacity in India: Insights from a faculty development programme in Andhra Pradesh. BMC Nurs. 2013;12:8. doi: 10.1186/1472-6955-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


