Abstract
Objective:
To identify the perspectives of patients with rheumatoid arthritis (RA) on electronic recording of between-visit disease activity and other patient-reported outcomes (PROs), and sharing this information with health care providers or peers.
Methods:
Patients with RA were recruited to participate in focus groups from December 2014 to April 2015. The topic guide and analysis were based on Andersen and Newman’s framework. Sessions were audio recorded, transcribed, independently coded, and analyzed for themes.
Results:
Thirty-one patients participated in seven focus groups. Their mean age was 51 (SD 13.1); 94% were female, 52% were African Americans, 11% were Hispanics, and 37% were Caucasians. Three themes emerged: 1) provider communication, 2) information seeking about RA, and 3) social and peer support. Participants expressed willingness to track disease activity data to share with health care providers electronically if providers would act on the information. Participants envisioned symptom tracking and information sharing as a mechanism to relay and obtain reliable information about RA. Participants were also interested in electronic communication between visits if it facilitated learning about symptom management and enhanced opportunities for social support among persons with RA.
Conclusion:
Patients with RA may be amenable to electronic collection and sharing of PRO-type data between clinical encounters if it facilitates communication with health care providers, and provides access to reliable information about RA. Providing patients with social support was important for enhancing PROs collection by helping them overcome barriers with using electronic devices and patients’ reservations about the value of this data.
Keywords: Patient Reported Outcomes, Rheumatoid Arthritis, qualitative research
Introduction
Evidence-based guidelines recommend that patients with rheumatoid arthritis (RA) be treated with the goal of attaining clinical remission or low disease activity as measured by validated patient- and/or rheumatologist-assessed disease activity measures.[1] Strong evidence has shown that many patient-reported outcomes (PROs), including health-related quality of life, pain, physical function, fatigue, sleep, work, and home productivity improve with use of RA disease-modifying anti-rheumatic drugs.[2–7] Indeed, some evidence suggests that patient self-assessments of RA are less subject to the placebo response than are some commonly accepted measures of inflammation, such as erythrocyte sedimentation rate and C-reactive protein level.[4]
A growing literature suggests that rheumatologists may not have placed enough emphasis on patient perspectives of RA symptoms and functioning, which may lead patients to decline treatment escalation recommended by their rheumatologists.[8, 9] Patients view disease activity based on criteria such as arthritis-related symptoms, functional impairment, and other disturbances to quality of life, some of which may have contributions from concurrent conditions such as fibromyalgia or depression. Perhaps in part for this reason, recent analyses have shown that >50% of patients do not undergo escalation of RA therapies despite not having achieved low disease activity.[10–13] RA disease activity likely influences several domains, including physical function, social and work-related duties, fatigue, and depression. Presenting information about their disease activity to patients can show the interplay of these domains and changes over time with RA treatment (i.e. changes in PRO scores). This, can deepen patients’ understanding of the way that RA treatment affects their lives as well as improve the shared decision-making process.
Collection of PROs typically occurs only every 2–3 months during follow-up visits, if at all, despite the importance of PRO data in clinical decision-making. During the interval between visits, patients may experience worsening joint pain, swelling, and flares that resolve and are not reported or documented at the subsequent encounter. Moreover, several studies have shown that PROs are inconsistently collected at the point-of-care due to time constraints, system-related errors, and communication lapses.[14, 15] Results from one investigation suggested that integrating self-reported patient data collected outside of clinical settings could allow for more comprehensive symptom reporting and could enhance fidelity and consistency of patient data.[14] These investigators proposed that by incorporating more frequent patient self-reporting, the patient-physician interaction could shift from symptom recall to addressing symptom severity and causality.[14] However, to date, a structured investigation of barriers and facilitators to communication and symptom reporting between provider visits has not been conducted among patients with RA. This is particularly important among patients with RA because they experience a variety of symptoms that inform treatment recommendations. Still, accurate assessment or measurement of each symptom may not occur in clinical encounters that happen only once every 2–3 months or even less frequently.
The collection of patient-reported measures of disease activity between scheduled physician encounters (recorded at home by the patient) can provide a more frequent, accurate, and quantifiable representation of RA disease activity that can be incorporated into treatment decisions as part of routine clinical care. However, it is not clear how willing patients are to collect such data or communicate between office encounters. A deeper understanding of RA patients’ motivations, interests, and expectations related to collecting PRO-type data between visits is needed to inform the design and utility of tools to engage them in PRO recording outside of the clinical setting. This study’s objectives were to elicit perspectives of patients with RA regarding perceived barriers and facilitators to collecting data electronically to monitor disease activity and to assess patients’ willingness to share data with others, including their health care providers (rheumatologist or primary care provider), staff (nurse, infusion nurse, pharmacist, or triage personnel), and other patients with RA. We wanted to examine if sharing information with other patients with RA will help overcome barriers to electronic data collection at home.
Patients and Methods
Study design and protocol
We collected data in focus groups using a topic guide based on a specific theoretical framework. This guide was reviewed for content in several iterations by a multidisciplinary team with expertise in rheumatology, preventive medicine, and health behavior, as well as by patients with RA participating in the Patient Centered Outcomes Research Institute (PCORI)-funded Patient Powered Research Network (PPRN) ArthritisPower. The guide was developed with an emphasis on addressing the three main domains of the Andersen and Newman framework that consist of predisposing, enabling, or illness-level factors that may affect utilization of RA clinical and ancillary services (Figure 1).[16] Supplement A contains a summary of the topic guide for this project. In brief, we asked participants to share their perspectives about their health, finding health information, and seeking support from family, friends, peers, non-physician medical professionals, or their current physician (Predisposing factors). Other points of discussion were access to RA providers, treatment, and access to communication tools (Enabling factors) and access to tracking mechanisms for RA symptoms (Illness-level factors). Finally, we inquired about RA symptom management, tracking, and reporting, including how symptoms inform decisions regarding follow-up and sharing of health information with providers, family, and other patients with RA. We also elicited factors that influenced willingness to track and share individual-level symptom information over time in face-to-face or online formats (e.g. online forums, journaling or blogs, or using apps to track symptoms) with their health care team and others (e.g. relatives, friends, and other patients with RA).
Figure 1.
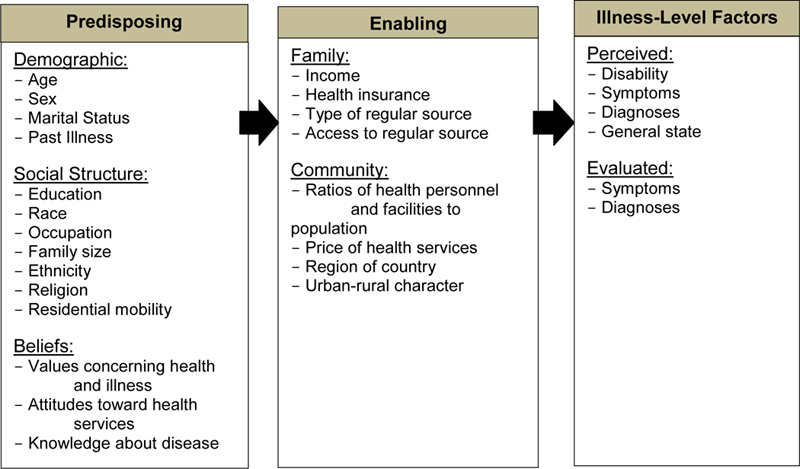
Individual Determination of Health Service Utilization (The Andersen and Newman framework)
To describe the sample, we gathered demographic information as well as each participant’s experience with RA, recent medication adherence (last 30 days), and comfort level with and likelihood of sharing RA and overall health data with a health care team as well as with family, friends and other patients with RA (Supplement B). We obtained written informed consent from participants prior to each session. The University of Alabama at Birmingham (UAB) Institutional Review Board approved study procedures.
Participant recruitment and eligibility
Participants were adult volunteers with RA (aged ≥19 years) recruited from the UAB Rheumatology Clinic from December 2014 to April 2015. Recruitment relied on provider-initiated referrals during regularly scheduled Rheumatology Clinic visits and study flyers posted in the Rheumatology Clinic. We aimed to recruit participants who reflected the demographics and disease duration observed in the clinic’s RA population. Eligibility criteria included a diagnosis of RA and willingness to participate in an audio-recorded focus group session.
Data collection
Trained research staff co-facilitated each focus group using the structured moderator guide. Groups met one time for 90 minutes each and were conducted in a private meeting space in the medical center. Sessions were audio recorded. After each session, each participant individually completed a brief paper questionnaire. The first three focus groups had a high no-show rate (two to three participants per group); hence, we conducted additional groups with five to eight participants in each subsequent group for a total of seven focus groups before reaching thematic saturation. Digital audio recordings from each session were securely uploaded into our server at UAB and transcribed verbatim by a medical transcription service. Transcriptions were uploaded into NVivo software version 10 (QSR International) software for analysis.
Analysis
Transcripts were reviewed and coded by two independent trained staff members for comparison prior to analysis (AZ and SS), with an initial coding outline structured according to the predisposing, enabling, and illness-level domains described in the Andersen-Newman framework, as related to RA management, information seeking, symptom tracking, and utilization of RA services. We generated the initial set of codes, which were then grouped into subthemes and subsequently themes. We deduced novel domains and associated themes during initial coding and generation of thematic summaries, and these domains and themes were combined with framework domains to produce an initial codebook. The panel of rheumatology providers who assisted with the development of the topic guide was consulted for coding discrepancies. Post-focus group questionnaire responses were analyzed using descriptive statistics to characterize the focus group cohort.
Results
A total of 31 patients with RA participated in the focus groups. Mean age (SD) of participants was 51 (13.1) years (range 25–84 years); 94% of participants were female; 52% were African Americans and 37% were Caucasian with 11% identifying as Hispanic ethnicity; and the mean (SD) disease duration was 10 (9.4) years. Among this group of patients, 18 (58%) of participants were “very” or “extremely” likely to use electronic/online tools for keeping track of their RA (Supplement B).
Themes/meaning units
Figure 2 includes a summary of several points that emerged during these focus groups that correspond to the main 3 domains of the Andersen-Newman framework. The three major themes and supporting quotes are summarized in Table 1.
Figure 2:
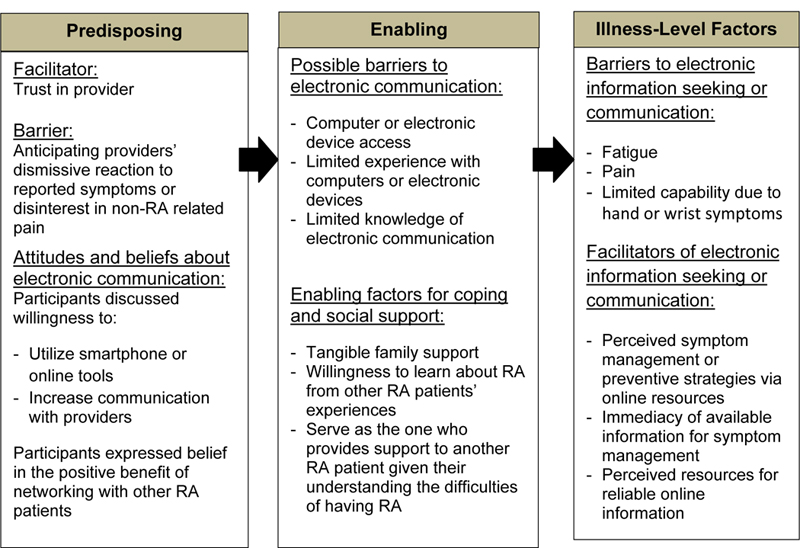
Summary of Barriers and Facilitators for Electronic Data Collection among Patients with Rheumatoid Arthritis
Table 1:
Themes with respective quotes that emerged as part of the focus groups conducted to interpret patients’ perspectives about tracking symptoms electronically at home.
| Theme | Quote |
|---|---|
| Theme 1: Provider communication |
“This app would give me a reminder time when to take my medications, it would give me a way to communicate with my doctor via email, it would be a tool that if I am going through something I can talk into the phone and store this information and go back at a later date and review it.” “I want to be able to communicate with him but not just drive him crazy … I am going to tell him the most important things and give him time to make the arrangements to try and help me because I’m not the only patient.” “I guess a lot of it is whatever is affecting me that day. And I might not even think about what to ask, but I need to be proactive and writing down things because of this. Even three months, you know even four, even month-to-month even you might think of something. If I don’t write it down I’m going to forget. If it doesn’t affect me between then and when I go back, it’s gone.” “I had an app that you have to keep up with when you’re trying to get pregnant. You could also go to a chat room from the app, and you could track your symptoms and stuff like that. It was really nice to have. I’m sure they’re out there for rheumatoid arthritis, but I haven’t even bothered to look yet.” |
| Theme 2: Information seeking: strategies for symptom management |
“A place where questions could be asked about that to a doctor that, you know, is well read that can get that information back to us. Because, you know, the media is killing us.” “I try to avoid the internet for any questions. I just prefer to just go ahead – to go to the sources and just go to my medical doctor and be like, “Look, I have this question, I’m having these symptoms, I feel like this. What should I do?” “The internet… You know, you can ask the internet anything. Now just because it’s on there doesn’t mean it’s true…. I look to sources like, WebMD, MD Anderson or Johns Hopkins.” |
| Theme 3: Social and peer support: |
“If we had, like, a central, you know, where people from Birmingham could talk about rheumatoid arthritis, and people from the Southeast could talk about rheumatoid arthritis, you could have, like, some sort of a website where you list all of your symptoms and keep an eye on them for yourself. And you can send that to your provider, or you could talk to somebody about a certain joint disease all in one webpage or app, for those of us who like our iPhones a lot.” “We show you, you know, how to access it through your email,” or we take your phone and say, “This is how you find this app. This is how you do it.” Have someone, whether it’s a receptionist, or a nurse, or somebody from the IT department, say, “Okay, this is the person who’s going to help the people who aren’t tech savvy access this stuff.” “I have family support” “I’m all about apps and stuff like that. But for people who aren’t, have someone in the office to show them, walk them through it step by step and make sure that they’re okay with it before they leave.” “Well I have adult children and they taught me the art of communication through text messaging, “If you want to ask me a question text me,” and I did.” “I think it’s great because you get to see other people and – and talk to them and hear how they dealt with theirs and let for instance me a year and a half I’ve had it and known about it. And I don’t really have anybody to talk to. So I don’t know what they’re doing and what they have done. I know of a few people that – that have it and when I first was diagnosed I did call one girl that I know, but I don’t see her regularly and interact with her.” |
Theme 1: Provider communication:
Participants expressed a great deal of interest in augmented communication with RA health care providers in real time or soon after symptoms arise. Most participants preferred phone or email communication, with few reporting use of a patient portal or electronic medical record (EMR) messaging. Common reasons for reaching out to providers were flare symptoms, medication refills, questions about medication, or requesting an appointment sooner. Participants expressed that their provider was a crucial source of support and trust for information, recommendations, and treatment decisions. However, participants were less interested in communicating with their physicians between visits if they perceived that they were doing well. Groups listed common perceived barriers and facilitators to electronic communication with providers as well as to completing questionnaires electronically (Figure 2).
Barriers to electronic data collection at home:
Barriers were illness-level factors, attitudes about care, and low awareness of a platform for collecting PRO. Many participants expressed their inability to type on a computer keyboard or phone keypad during symptoms of fatigue or hand pain. Other barriers were not having access to a computer or unfamiliarity with this technology. Participants were interested in providing data to physicians, but they also expressed discouragement when physicians did not attend to the information they provided at the point of care. Participants emphasized that if they shared information with the provider, whether at home or at the point of care, they wanted physicians to act on this information. If physicians did not incorporate the provided data, patients were far less interested in completing questionnaires at home.
Facilitators to electronic data collection at home:
Facilitators were largely enabling factors, including access to a computer, internet service, and familiarity with computers or smartphones. Those who expressed difficulty with technology indicated that having formal instruction or someone to assist or engage them in the electronic communication could empower them to consider this avenue. Some participants were already journaling or recording symptoms at home, and many indicated willingness to share additional data if their treating rheumatologist requested it. At the same time, they expressed motivation to collect data if they were used to manage symptoms or obtain support from their physician (See Themes 1, 2, 3 and Figure 2). They also expressed interest in the data collection platform allowing them to learn about RA and RA medications including side effects (see Themes 2 and 3), and learn about nonmedical (i.e. self-management) options for treating RA.
Theme 2: Information seeking: strategies for symptom management:
Nearly all participants expressed the belief that their health care provider was their most trusted source of health information and treatment recommendations (See Theme 1), and they preferred to learn about RA from their provider. Few were certain about the trustworthiness of electronic resources. Many described frustrations with illness-level factors, including pain, effects of RA on the body, and interference with daily activity, particularly near the time of diagnosis. They expressed interest in accessing educational resources for medical and nonmedical symptom management. Several participants were interested in learning from others with RA about available online resources, how to better use electronic or online resources available for patients with RA, and the best ways to communicate with their doctors. However, very few participants were aware of existing platforms for PRO-type data collection that they can use to track their symptoms and share the information with their provider or even another patient with RA.
Barriers to obtaining information about symptom management:
Several participants identified a need for resources for accurate and tailored medication information, provided in lay terms, that includes evidence of long-term effects of RA medication and potential drug interactions (e.g. thyroid medication and antibiotics). Many were unsure of how to retrieve dependable information online or in real time. For some participants, actual and anticipated side effects were barriers to therapeutic management of symptoms, and persons who reported using electronic or online resources expressed concerns regarding understandability and credibility of online sources.
Facilitators to obtaining information about symptom management:
Participants expressed interest in learning about symptom and medication management through platforms similar to those with which they communicated data to their providers. They expressed that having this information would be a motivator for them to enter responses to electronic questionnaires through platforms, more so if their provider also requested that they complete the questionnaires. Still, as mentioned in Theme 1, participants emphasized that providers should use this information in order to keep the patient motivated to continue tracking their symptoms (via PROs).
Theme 3: Social and peer support:
Participants agreed that having some form of social support was vital to wellness and coping. This included supportive communication, electronic or in person, with their health care team; receiving support from partners and family members; and supportive communication (giving or receiving) with other patients with RA.
Barriers to social and peer support:
Few participants had made social connections with other patients with RA. Most received a significant amount of support from local family members for coping and health management. However, many expressed feelings of isolation at time of diagnosis and were unsure of how to establish supportive connections with peers with RA, online or in person.
Facilitators to social and peer support:
Participants expressed eagerness to communicate with other patients with RA to establish expectations of treatment and obtain information about flares and symptom management. They expressed interest in a platform for connecting with others with RA as a way of learning about RA and coping, particularly for reducing isolation. They wanted to learn what to expect from their treating rheumatologist, how best to communicate with providers, and what to expect from RA and the medications used to treat it. Participants expressed that these resources can help them overcome their feelings of isolation, which at the same time could serve as a motivation for them to engage in electronic data collection as well. They expressed that working with another patient with RA could help overcome their lack of familiarity with computers and electronic devices and assist in completing questionnaires about disease activity online (Barriers Theme 1; Enabling domain Figure 2).
Participants expressed the desire to have an initial interaction in a structured, facilitated meeting or face-to-face group to establish trust before engaging in online communication with peers. Participants further expressed that initiating social connections in person could help overcome reservations for sharing RA data electronically, the process of sharing symptoms and entering disease activity data in a PRO or electronic format.
Discussion
The results of this study demonstrate that these patients with RA were interested in frequent, positive communication with a trusted provider; reliable, tailored information for symptom management in therapeutic and non-medical approaches (i.e. self-management); and supportive connections, including those with other patients with RA. Many participants expressed willingness to find and share data regarding RA disease activity for improved symptom management and social support, but most were unfamiliar with electronic or PRO platforms. Focus group participants expressed interest in tracking and sharing symptoms between visits, which may include PROs, as part of their clinical care, if their treating rheumatologist would utilize the information to treat their disease. Other aspects of great importance as motivators to electronic data collection were a desire to learn about expectations for short- and long-term disease management, information on symptoms and medication side effects, and seeking support from physicians, family, and other patients with RA. However, our findings indicated that asking patients to collect and share data electronically is not enough to engage them. Disease monitoring through electronic tracking of symptoms or PRO platform use should be aligned with social and/or provider support, adequate instruction on electronic device use (e.g. smartphones and computers), tailored information on managing symptoms and side effects, and lifestyle programs for patients with RA. Meeting these needs may provide necessary motivation among patients with RA to electronically track and report data between doctor visits, especially if the purpose of the data collection is clearly explained.
As many participants were unfamiliar with electronic PRO platforms, they did not mention how information provided through PROs is helpful to them personally, how it could reflect the status of their disease, and how it could allow comparison of their disease status with other patients with RA. A possible explanation is that they did not understand that PROs can provide individual and population-based information about RA longitudinally. Giving patients a general understanding about PROs and their clinical utility could serve as another motivation for patients to collect these data. Since patients indicated difficulty typing on electronic devices due to disease activity, another technology for consideration is passive data collection (e.g. body sensors of gait, texting speed, or pedometers).
Participants valued positive communication with trusted providers and information about what to expect of medications. These findings suggest that coupling PRO collection at home with education on medications and side effects may be a reasonable strategy for collecting this information between visits. These findings are consistent with published benefits of PRO use in clinical practice, including improvement in patient-physician communication, self-efficacy, and treatment plan adherence, as well as greater satisfaction with care and more efficient use of resources.[17] Additionally, compared with simply asking patients to complete PRO questionnaires, collection of PRO data paired with a learning experience for the patient was shown to be more successful in engaging patients to use self-tracking technologies.[18]
It was important to patients that their providers utilize the disease information they shared. Compared with standard paper forms or unstructured self-report at the visit, an electronic tool may allow easier data entry for patients and simpler interpretation for providers. As a recent study showed that young patients with RA prioritize function while older patients with RA want to avoid fatigue.[19] Therefore, systematic symptom and disease activity data collection by patients may enhance interpretability so physicians can better address patient priorities.
Importantly, participants showed great interest in obtaining information for RA management. Providing patients with appropriate guidance and encouraging them to utilize a PRO platform may enable useful insights into the significance and trends of their individual data and how these measures can be used to improve RA care and support. These data can also facilitate discussion with providers at or between visits about aspects of health that matter most to patients. This study serves as a foundation for follow-up studies to evaluate the use of PROs for improved patient satisfaction and outcomes in RA.
Our study has several strengths. It is a qualitative investigation guided by a conceptual framework of factors influencing health care utilization, which provided a consistent structure from conception (research question and topic guide) through analysis (coding and theme structure). The topic guide used for the focus groups was extensively vetted by patients and investigators with different backgrounds and expertise, resulting the incorporation of a variety of perspectives. This study achieved theme saturation and engaged a relatively large sample size for a qualitative study. Additionally, the final sample included a large number of women and African American participants, groups traditionally underrepresented in RA research.
There were also several limitations to our study worth considering. The participants were from a single center, and not all scheduled participants participated. However, the sample allowed us to recognize patients’ perspectives, attitudes, and opinions and met the goal of hypothesis generation. We also obtained the patient perspective only, and subsequent investigation into rheumatologists’ perspectives on the use of PROs to inform RA treatment is warranted.
In conclusion, patients may be willing to use questionnaires to collect PROs between office visits, and many are amenable to electronic data capture. An electronic data capture tool may be useful in providing quantifiable information to RA health care providers to complement signs and symptoms described during office encounters, and patients may be more willing to engage with such a tool if it also provides reliable educational information about RA and its treatments for patients, preferably delivered or at least recommended by their doctor. These patients valued the receipt of information regarding symptom management and support, as well as communication with trusted providers, at and between scheduled clinic visits. Electronic tracking of PRO data may be an important communication mechanism for persons with RA and their health care team. Self-tracking technologies may be more attractive to patients with RA if coupled with opportunities to learn about RA-specific issues, including symptom management, medications and side effects; and opportunities to obtain social support.
Supplementary Material
Key Points:
The major motivation for patients with RA to complete questionnaires at home was that their treating rheumatologists would pay attention to and act upon this information.
Participants were eager to have a platform, preferably endorsed by their treating rheumatologist, with reliable information about RA, side effects of RA medications, diet, and exercise. Combining a learning experience about these aspects with completion of questionnaires at home would motivate them because they would not only provide but also obtain information.
Providing patients with social support by peers appeared to be a reasonable approach to enhance the collection of PROs by helping them overcome barriers with the use of electronic devices and patients’ reservations about the value of collecting this data for their provider.
Acknowledgments
Acknowledgements:
Anna Cornelius-Schecter and Erin Thacker for editing this manuscript. We would like to thank the patients that participated in these focus groups.
Funding:
Rheumatology Research Foundation Innovative Research Grant and Pfizer supported this work. INM was funded by the Innovative Research Award from the Rheumatology Research Foundation and K23AR068449 National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health. Research reported in this publication was also supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231 (Fraenkel). HY receives research support from BMS and Pfizer for unrelated work.
Footnotes
Disclosures:
INM, AZ, SS, BJ, MID, JW, HY, MMS, JRC, LF have nothing to disclose.
References
- 1.Singh JA, et al. , 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken), 2016. 68(1): p. 1–25. [DOI] [PubMed] [Google Scholar]
- 2.Hazes JM, et al. , Physical function improvements and relief from fatigue and pain are associated with increased productivity at work and at home in rheumatoid arthritis patients treated with certolizumab pegol. Rheumatology (Oxford), 2010. 49(10): p. 1900–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strand V, et al. , Improvements in health-related quality of life after treatment with tocilizumab in patients with rheumatoid arthritis refractory to tumour necrosis factor inhibitors: results from the 24-week randomized controlled RADIATE study. Rheumatology (Oxford), 2012. 51(10): p. 1860–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strand V, et al. , Patient-reported outcomes better discriminate active treatment from placebo in randomized controlled trials in rheumatoid arthritis. Rheumatology (Oxford), 2004. 43(5): p. 640–7. [DOI] [PubMed] [Google Scholar]
- 5.Strand V, et al. , Use of “spydergrams” to present and interpret SF-36 health-related quality of life data across rheumatic diseases. Ann Rheum Dis, 2009. 68(12): p. 1800–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strand V, et al. , Rapid and sustained improvements in health-related quality of life, fatigue, and other patient-reported outcomes in rheumatoid arthritis patients treated with certolizumab pegol plus methotrexate over 1 year: results from the RAPID 1 randomized controlled trial. Arthritis Res Ther, 2009. 11(6): p. R170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strand V, et al. , Health-related quality of life outcomes of adalimumab for patients with early rheumatoid arthritis: results from a randomized multicenter study. J Rheumatol, 2012. 39(1): p. 63–72. [DOI] [PubMed] [Google Scholar]
- 8.Dougados M, et al. , Relative importance of doctor-reported outcomes vs patient-reported outcomes in DMARD intensification for rheumatoid arthritis: the DUO study. Rheumatology (Oxford), 2013. 52(2): p. 391–9. [DOI] [PubMed] [Google Scholar]
- 9.Khan NA, et al. , Determinants of discordance in patients’ and physicians’ rating of rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken), 2012. 64(2): p. 206–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh JA, et al. , 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken), 2012. 64(5): p. 625–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smolen JS, et al. , Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis, 2010. 69(4): p. 631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang J, et al. , Thresholds in disease activity for switching biologics in rheumatoid arthritis patients: experience from a large U.S. cohort. Arthritis Care Res (Hoboken), 2011. 63(12): p. 1672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fraenkel L and Cunningham M, High disease activity may not be sufficient to escalate care. Arthritis Care Res (Hoboken), 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valikodath NG, et al. , Agreement of Ocular Symptom Reporting Between Patient-Reported Outcomes and Medical Records. JAMA Ophthalmol, 2017. 135(3): p. 225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Margalit RS, et al. , Electronic medical record use and physician-patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns, 2006. 61(1): p. 134–41. [DOI] [PubMed] [Google Scholar]
- 16.Andersen R and Newman JF, Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc, 1973. 51(1): p. 95–124. [PubMed] [Google Scholar]
- 17.Donaldson MS, Taking PROs and patient-centered care seriously: incremental and disruptive ideas for incorporating PROs in oncology practice. Qual Life Res, 2008. 17(10): p. 1323–30. [DOI] [PubMed] [Google Scholar]
- 18.Fors V and Pink S, Pedagogy as Possibility: Health Interventions as Digital Openness. Social Sciences, 2017. 6(2): p. 59. [Google Scholar]
- 19.Bacalao EJ, et al. , Standardizing and personalizing the treat to target (T2T) approach for rheumatoid arthritis using the Patient-Reported Outcomes Measurement Information System (PROMIS): baseline findings on patient-centered treatment priorities. Clin Rheumatol, 2017. 36(8): p. 1729–1736. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


