Abstract
Background/purpose
Various restoration materials have been used to restore as onlay materials to restore highly defected molar teeth. Different mechanical and physical properties of these materials may affect the success or survival of the restoration. The purpose of this study was to evaluate the restoration materials effects on stress distribution.
Materials and methods
Three dimensional finite element analysis (FEA) was used to evaluate the stress concentrations and distributions at the restoration and the tooth. Maxillar first molar tooth constructed to evaluate the stress distribution and concentration levels at the restorations and the tooth structure. Two kinds of restoration materials, bulkfill composite and conventional hybrid composite was evaluated for direct method, while full ceramic and indirect composite was used for indirect method. A load of 200 N was applied on the restorations and stress levels were calculated by von Mises stress values.
Results
Highest stress concentration was observed at the ceramic restoration (3.77 GPa). Stress levels were 2.90 GPa for bulkfill composite and 2.14 GPa for direct and indirect composite. At the tooth structure the stress levels were 3.33 GPa, 3.18 GPa and 2.48 GPa for bulkfill, direct and indirect composites respectively. The lowest stress values was observed with the porcelain restoration (1.69 GPa). Stress concentrations at the adhesive system were 2.10 MPa for bulkfill composite, 1.35 MPa for direct and indirect composites and 1.25 Mpa for porcelain restoration.
Conclusion
The restoration material affects the stress levels at the restoration and the tooth while the stress concentration areas remained nearly the same.
Keywords: Ceramics, Composites, Finite element analysis, Partial crown, Onlay
Introduction
It has been a continually controversial topic how to restore the large defects of a molar tooth. Using direct tooth filling or application of an inlay or onlay restorations instead of full crowns are more conservative treatment approaches. Besides, another controversial topic opens after selection of inlay or onlay restoration, direct restoration or indirect restoration. Esthetic, biomechanic, anatomic and financial criterias should be considered in order to decide which alternative should be used.1 However, molar tooth with a large defect possibly have an endedontic treatment. Teeth with endodontic treatment are not as strong as an intact tooth although they are reinforced with restorations.2, 3, 4
Inlay restorations restore a cavity in the centerline of a tooth while onlay restorations cover one or more tubercules of the tooth and provide a more favorable stress distribution and reduce fracture risk.2,3,5,6
With these advantages onlay restorations have been recommended to protect and restore endodontically treated teeth.4 However onlay preparation cause more reduction of tooth structure when compared with inlay preparation.
There are many material alternatives for inlay and onlay restorations such as metals, composites, ceramics and zirconia. One of the most primary properties of these materials should have is the strength and resistance to masticatory forces in the oral cavity.7 While the maximum occlusal force of a healthy man can reach to 847 N and a healthy woman can reach to 597 N, parafunctional habits such as bruxism may incrade the maximum occlusal force over 900 N.8 Besides, for the longevity of the restoration and for more uniform stress distribution, the elastic properties of the material should be similar to the tooth. However enamel and dentin have different elastic properties and one of them should be chosen as standard for the decision of the restorative material.7
For cast metal restorations, functional and non-functional tubercules should be reduced in order to achieve more favorable stress distribution.9 Further, as metal restorations usually cemented with conventional non-adhesive cements, it would be useful to cover to tubercules in order to increase the tooth structure resistance. However demand for non-metal restorations increased in recent years and many alternative restorative materials entered the dental market.
Non-metal restorations' such as composites and ceramics, primary advantages are more esthetic appearance, lack of allergic/toxic metal alloys.10 At the present time composite resins and ceramic and zirconia restorations became popular among patients and the clinicians. While composite resins' elasticity moduleses are similar to dentin, ceramics' elasticity moduleses are similar to enamel.11
Due to the polymerization depth, short functional lifetime and insufficient proximal contact areas of the direct composites techniques, indirect composite techniques were developed. Extraoral production of the restorations provides more effective polymerization with the use of heat, pressure and the light alone or in combination. Further indirect composites are stronger and more durable when compared with the hybrid composites, thus present more resistance to attrition, wear and fracture. Besides the high filler load of small sized fillers provide low polymerization shrinkage characteristic.7
The other alternatives for non-metal inlays and onlays are ceramics and zirconia. Dental ceramics have translucency, fluorescence, chemical stability, thus they are accepted as esthetical restoration material.9 Further, their biocompability, high compressive strength and thermal expansion coefficient is similar to natural tooth. However, beside these advantages ceramics are fragile under tensile strain.4 Many preparation alternatives were recommended for ceramic inlay or onlay restoration.1,12 However, the preparation of tooth for ceramic inlay or onlay restoration are based on conventional cast metal restorations with more occlusal reduction in order to provide more thickness to ceramic.13
Restoration or tooth fractures are the main reasons of inlay or onlay restorations failures. The other reasons are marginal adaptation loss, marginal deficiencies.2 The aim of this study was to evaluate and distinguish the material effects to stress distribution of an onlay restoration. Besides, it was also aimed to observe the stress concentrations and localizations, then assess if the stress concentrations were higher or lower than the adhesives strength.
Materials and methods
Three dimensional finite element analysis (FEA) model of a maxillar first molar tooth constructed to evaluate the stress distribution and concentration levels at the restorations and the tooth structure. Graphic processing programs (Rhinoceros 4.0, McNeel, Seattle and Ansys 11.0, Ansys Inc. Pennsylvania) were used to construct the mathematical models that are consisting of tooth structure, onlay restorations and adhesives. The model simulated an endodontically restored tooth with loss of both functional cusps. The surrounding bone was ignored as it was aimed to investigate the stress concentrations at the restorations and the crown of the tooth. Each mathematical model included approximately 14200 nodes. The calculation of the displacement of each of the nodes was used verify the stress throughout the structure. A finer mesh was produced at the interfaces to ensure accuracy of force transfer.
Two different materials for two different techniques were evaluated; conventional composite and bulkfill composite was used for direct method and full ceramic and indirect composite was used for indirect method.
The onlay restorations were prepared with dimensions of 2.7 mm cavity depth, 2.3 mm isthmus width, and 1.2 mm gingival wall width.
As it is impossible to obtain precise organic material properties, all materials were considered as isotropic, homogenous and linearly elastic. The elastic properties (Young's modulus (E) and Poisson's ratio (μ)) were used in the models were taken from the literature (Table 1).
Table 1.
Elasticity modulus and Poisson's ratio of the materials.
| Modulu of elasticity (MPa) | Poisson's ratio | |
|---|---|---|
| Enamel (mine) | 84,000 | 0.20 |
| Dentin | 18,600 | 0.31 |
| Ceramic | 65,000 | 0.19 |
| Resin cement | 8,300 | 0.35 |
| Composite resin | 21,000 | 0.24 |
| Indirect composite resin | 25,000 | 0.24 |
| Bull-fill composite | 5,500 | 0.24 |
| Fiber post | 40,000 | 0.26 |
The load applied on the restorations was 200 N. The stress levels were calculated using von Mises stress values which are commonly reported in other finite element analyses studies as Von Mises stress values are used to compare the stress distribution in ductile materials. Especially the maximum value was used as reference. A color scale was used to provide comprehensible view of the stress concentrations.
Results
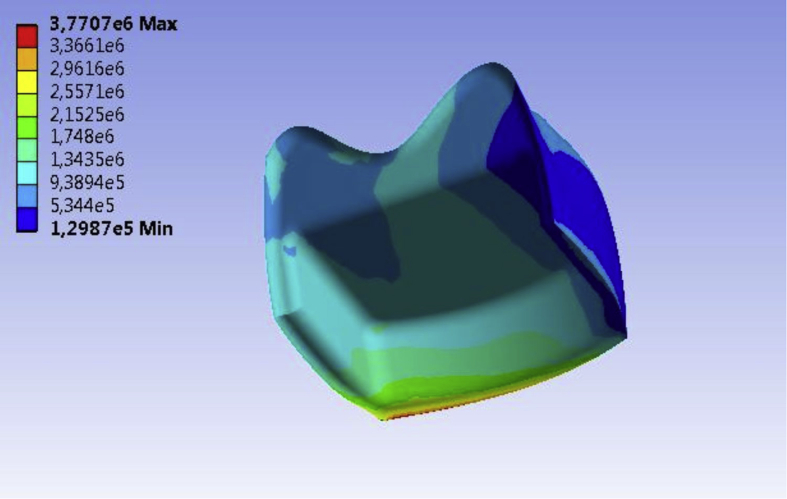
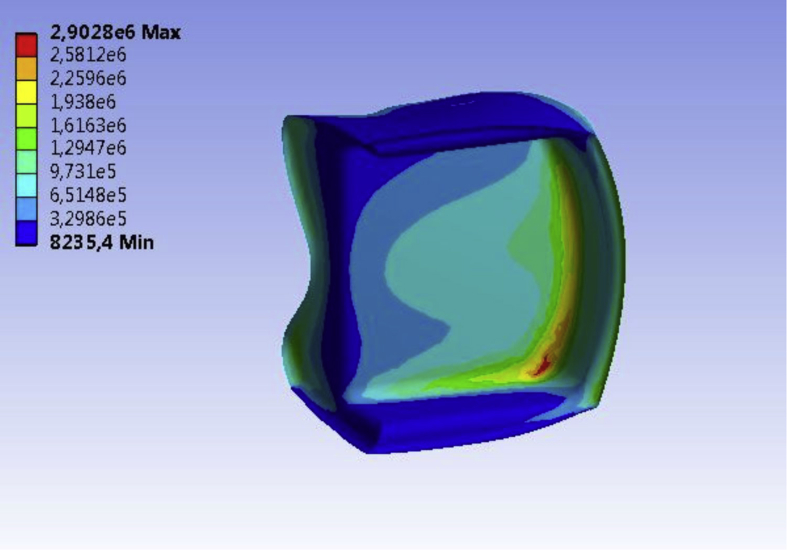
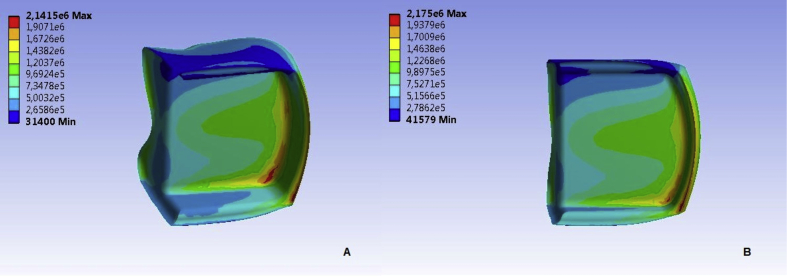
Among the superstructure materials the highest stress concentrations was observed at the ceramic restoration (3.77 GPa) (Fig. 1). The composite materials showed lower stress values than the ceramic and the second highest stress concentration was observed within bulkfill composite material (2.90 GPa) (Fig. 2). The stress concentrations at the direct and indirect composite materials were similar (2.14 GPa) (Fig. 3).
Figure 1.
Highest stress concentration was observed at the lower border of the ceramc restoration.
Figure 2.
The bulkfill composite exhibited the second highest stress level. The stresses concentrated at the cuspal area.
Figure 3.
Stress concentrations of the direct (A) and indirect (B) composites were similar.
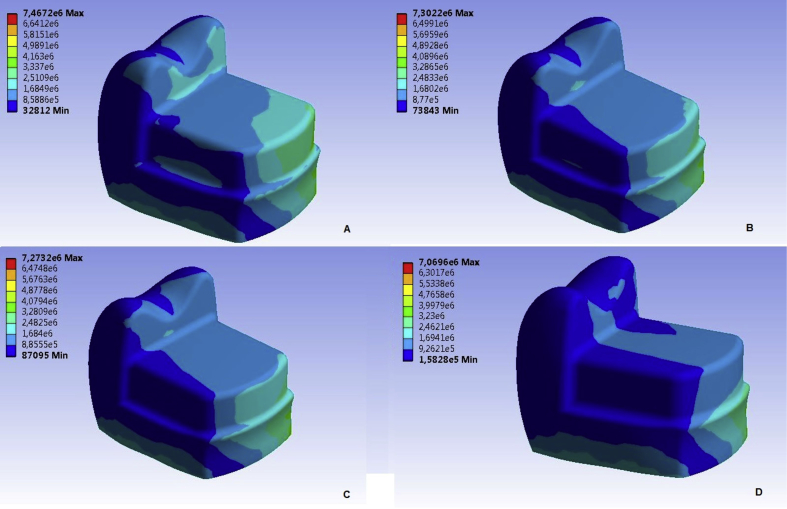
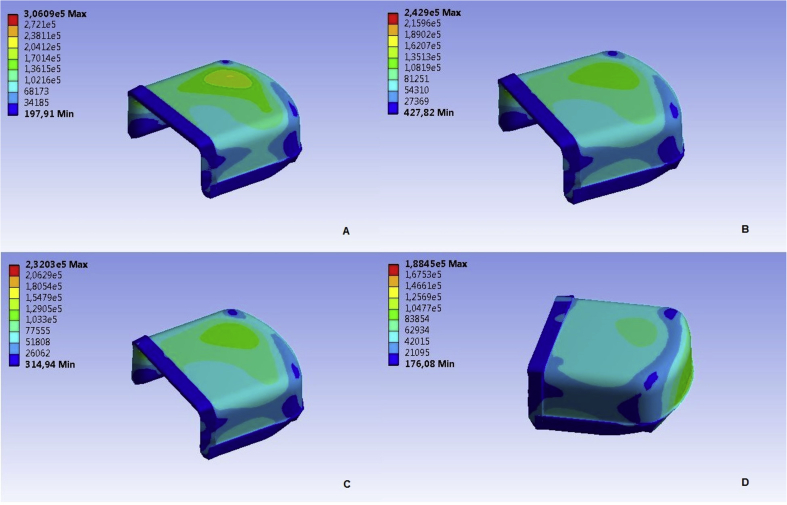
The stress concentrations at the tooth structure were 3.33 GPa, 3.18 GPa and 2.48 GPa for bulkfill, direct and indirect composites respectively. The lowest stress values was observed with the ceramic restoration (1.69 GPa) (Fig. 4).
Figure 4.
Stress distributions at the tooth. (A) Bulkfill Composite, (B) Direct Composite, (C) Indirect Composite, (D) Ceramic.
The adhesive was the least affected component of the onlay system. The stress values were 2.10 MPa for bulkfill composite, 1.35 MPa for direct and indirect composites and 1.25 Mpa for ceramic restoration (Fig. 5).
Figure 5.
Stress distributions at the adhesive resin. (A) Bulkfill Composite, (B) Direct Composite, (C) Indirect Composite, (D) Ceramic. The stress patterns are similar.
Table 2 shows the comparison of the stress concentrations at the superstructures, adhesive and the tooth.
Table 2.
Comparison of stress concentrations at the superstructure materials, adhesive and tooth structure and loading.
| Within the restoration | Tooth structure | Adhesive | |
|---|---|---|---|
| Ceramic | 3.77 GPa | 1.69 GPa | 1.25 Mpa |
| Bulkfill composite | 2.90 GPa | 3.33 GPa | 2.10 MPa |
| Direct composite | 2.14 GPa | 3.18 GPa | 1.35 MPa |
| Indirect composite | 2.14 GPa | 2.48 GPa | 1.35 MPa |
Discussion
The results from the previous studies that evaluated the effects of restorative materials on stress distribution in tooth structures are contradicting.7 Further, previous studies have investigated stress distributions or adhesive strength of cements and bonding agents. These studies did not combine the stress distributions and concentrations with the response of adhesives or restoration materials under loading. For a better view of this issue, a 3D finite element analysis of different restoration materials was performed. Due to costs, risks and ethical problems of in vivo studies in vitro studies and mathematical models and analysis are much popular among investigators.8 However depending only on the results of in vitro experiments or finite element analysis may be misleading.14 Thus in vivo studies should be performed following the in vitro tests.
The common opinion of the previous studies is oblique loads generate more stress than vertical loads.7 However previous studies have mentioned that occlusal force is insufficient to cause restoration failure as the fracture resistance of teeth restored by inlays/onlays is beyond the maximum occlusal force of the average man or woman.15 Thus, it was aimed to evaluate the maximum von Mises values and stress distribution in teeth and the restorations and observe the failure mechanism with various restorative materials. Stress concentrations indicate the location and the probable failure initiation and fracture of the tooth.2
It has been reported that elastic modulus of the restoration material is more effective on stress concentrations than the thickness of the material.3,16 High elastic modulus materials tend to accumulate stresses and low elastic modulus materials absorb stresses.3,17,18 However in our study, a high elastic moduli material, porcelain, showed higher stress values inside the material but did not transfer the stress to the tooth structure. The higher amount of stress transferred to the tooth structure may have detrimental effects such as crown or root fractures. The materials that absorb the stresses may show higher failure rates, however it may also preserve the tooth structure as well. Further, stress concentrations are dependent on other factors such as geometry of the material, loading conditions, and presence of intrinsic or extrinsic flaws.8,9,19 However, it has been reported that adhesively cemented indirect composite resin restorations are reported to absorb the stresses initially, but instantly transfer it to the tooth. The restoration and the tooth complex accumulate energy until failure.3,20 Neverthless, with respect to wall-to wall adaptation adhesively cemented indirect composites are slightly better than direct composite restorations.2 Also, finite element analysis of previous studies indicated composite resin yielded lower risks of root fracture.8 In our study only the coronal part of the tooth was observed. However the restoration materials also have effects on the root and root fractures. The materials with higher elasticity modulus tend to transfer stresses to the deeper part of the root.8
Some researchers reported that ceramic inlays reduced tension at the dentin-adhesive interface, thus able to provide better resistance against debonding when compared with composite resins.2,18,21 In the current study, similar results were obtained. The ceramic restoration reduced the tension at the dentin-adhesive interface. However, contradictory reports also exist such as Ausiello et al. who reported that ceramic restorations created higher stress levels at the internal surfaces of the preparations.22, 23 Besides Jiang et al. stated that composite resin inlays show similar biomechanical properties with tooth and redistribute stresses.5
The effect of the resin luting agents used with the indirect techniques may reduce the stress concentrations, however it is insufficient to absorb the stresses.23 Our study's outcomes also approved this and the luting agent showed the least stress concentration levels.
The preparation design may influence the stress distribution and concentrations as well. Knife-edge preparations should be avoided in places that were exposed to significant loads.4 Soares et al. reported that cuspal coverage did not have effect on fracture resistance of posterior ceramic restorations.9,19
There were several limitations in the study. FEA is only a simulation and it is not possible to include all of the factors. Also a single type of loading was applied on the restorations. The materials and the tissues are unisotropic but they were assumed isotropic. However the results of the study may assist the clinicians to choose the material to restore for a highly damaged tooth. Furthermore, the adhesive failure of the restorations should be studied with mechanical tests.
In conclusion, the results of this study indicate the ceramic as a more favorable restoration material for onlay restorations. The indirect composite may also be an alternative restoration material for onlays. Besides, with the preferable stress distribution and concentration characteristics, the opportunity to fabricate restorations with better contact areas, favorable esthetics and durability, indirect restorations may be the superior alternative for onlay restorations.
Funding
This study was supported by Afyon Kocatepe University Scientific Researchs Committee with Grant Number 15.HIZ.DES.88.
Conflicts of interest
The author has no conflicts of interest relevant to this article.
References
- 1.Garber DA, Goldstein RE. Porcelain and Composite Inlays and Onlays. Esthetic Posterior Restorations. 1st ed. Chicago: Quintessence; 1994. p.38.
- 2.Jiang W., Bo H., Yongchun G., LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent. 2010;103:6–12. doi: 10.1016/S0022-3913(09)60206-7. [DOI] [PubMed] [Google Scholar]
- 3.Fonseca R.B., Fernandes-Neto A.J., Correr-Sobrinho L., Soares C.J. The influence of cavity preparation design on fracture strength and mode of fracture of laboratory-processed composite resin restorations. J Prosthet Dent. 2007;98:277–284. doi: 10.1016/S0022-3913(07)60101-2. [DOI] [PubMed] [Google Scholar]
- 4.Dejak B., Mlotkowski A., Romanowicz M. Strength estimation of different designs of ceramic inlays and onlays in molars based on the Tsai-Wu failure criterion. J Prosthet Dent. 2007;98:89–100. doi: 10.1016/S0022-3913(07)60042-0. [DOI] [PubMed] [Google Scholar]
- 5.Shillingburg HT. Fundamentals of Fixed Prosthodontics. 3rd ed. Chicago: Quintessence; 1997. p.171–9.
- 6.Magne P., Belser U.C. Porcelain versus composite inlays/onlays: effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodontics Restor Dent. 2003;23:543–555. [PubMed] [Google Scholar]
- 7.Yamanel K., Çaglar A., Gülsahi K., Özden U.A. Effects of different ceramic and composite materials on stress distribution in inlay and onlay cavities: 3-D finite element analysis. Dent Mater J. 2009;28:661–670. doi: 10.4012/dmj.28.661. [DOI] [PubMed] [Google Scholar]
- 8.Magne P. Virtual prototyping of adhesively restored, endodontically treated molars. J Prosthet Dent. 2010;103:343–351. doi: 10.1016/S0022-3913(10)60074-1. [DOI] [PubMed] [Google Scholar]
- 9.Soares C.J., Martins L.R.M., Fonseca R.B., Correr-Sobrinho L., Neto A.J.F. Influence of cavity preparation design on fracture resistance of posterior Leucite-reinforced ceramic restorations. J Prosthet Dent. 2006;95:421–429. doi: 10.1016/j.prosdent.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Sadowsky S.J. An overview of treatment considerations for esthetic restorations: a review of the literature. J Prosthet Dent. 2006;96:433–442. doi: 10.1016/j.prosdent.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Albakry M., Guazzato M., Swain M.V. Biaxial flexural strength, elastic moduli, and x-ray diffraction characterization of three pressable all-ceramic materials. J Prosthet Dent. 2003;89:374–380. doi: 10.1067/mpr.2003.42. [DOI] [PubMed] [Google Scholar]
- 12.Bremer B.D., Geurtsen W. Molar fracture resistance after adhesive restoration with ceramic inlays or resin-based composites. Am J Dent. 2001;14:216–220. [PubMed] [Google Scholar]
- 13.Etemadi S., Smales R.J., Drummond P.W., Goodhart J.R. Assessment of tooth preparation designs for posterior resin-bonded porcelain restorations. J Oral Rehabil. 1999;26:691–697. doi: 10.1046/j.1365-2842.1999.00440.x. [DOI] [PubMed] [Google Scholar]
- 14.Thompson M.C., Field C.J., Swain M.V. The all-ceramic, inlay supported fixed partial denture. Part 3. Experimental approach for validating the finite element analysis. Aust Dent J. 2012;57:23–30. doi: 10.1111/j.1834-7819.2011.01638.x. [DOI] [PubMed] [Google Scholar]
- 15.St-Georges A.J., Sturdevant J.R., Swift E.J., Jr., Thompson J.Y. Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent. 2003;89:551–557. doi: 10.1016/s0022-3913(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 16.Kelly J.R. Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent. 1999;81:652–661. doi: 10.1016/s0022-3913(99)70103-4. [DOI] [PubMed] [Google Scholar]
- 17.Dejak B., Mlotkowski A., Romanowicz M. Finite element analysis of stresses in molars during clenching and mastication. J Prosthet Dent. 2003;90:591–597. doi: 10.1016/j.prosdent.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Lin C.L., Chang Y.H., Liu P.R. Multi-factorial analysis of a cusp-replacing adhesive premolar restoration: a finite element study. J Dent. 2008;36:194–203. doi: 10.1016/j.jdent.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Schaefer O., Watts D.C., Sigusch B.W., Kuepper H., Guentsch A. Marginal and internal fit of pressed lithium disilicate partial crowns in vitro: a three-dimensional analysis of accuracy and reproducibility. Dent Mater. 2012;28:320–326. doi: 10.1016/j.dental.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Ortega V.L., Pegoraro L.F., Conti P.C., do Valle A.L., Bonfante G. Evaluation of fracture resistance of endodontically treated maxillary premolars, restored with ceromer or heat-pressed ceramic inlays and fixed with dual-resin cements. J Oral Rehabil. 2004;31:393–397. doi: 10.1046/j.1365-2842.2003.01239.x. [DOI] [PubMed] [Google Scholar]
- 21.Magne P., Perakis N., Belser U.C., Krejci I. Stress distribution of inlay-anchored adhesive fixed partial dentures: a finite element analysis of influence of restorative materials and abutment preparation design. J Prosthet Dent. 2002;87:516–527. doi: 10.1067/mpr.2002.124367. [DOI] [PubMed] [Google Scholar]
- 22.Ausiello P., Rengo S., Davidson C.L., Watts D.C. Stress distributions in adhesively cemented ceramic and resin-composite ClassII inlay restorations: a 3D-FEA study. Dent Mater. 2004;20:862–872. doi: 10.1016/j.dental.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Soares C.J., Martins L.R.M., Pfeifer J.M., Giannini M. Fracture resistance of teeth restored with indirect-composite and ceramic inlay systems. Quintessence Int. 2004;35:281–286. [PubMed] [Google Scholar]