Abstract
Background/Purpose
Dental caries in primary dentition is a major public health problem in many countries, as well as Taiwan. The service of professional topical fluoride application for children under 5 years of age, performed twice a year by the BNHI in Taiwan through the “Preventive Dental Health Service for Children” plan, began in July 2004. The purpose of this study was to examine the effect and trend of professional topical fluoride application on dental utilization.
Materials and methods
The sample subjects were taken from the Normalized Million People File of 2010 in the National Health Insurance Research Database from 2000 to 2012, for the purpose of analyzing the status of the professional topical fluoride program. The main analysis included utilization of professional topical fluoride application, utilization of restorative treatment and utilization of endodontic therapy in children 1-to-5-years of age. The Cochran–Armitage trend test was used for statistical analysis.
Results
Professional topical fluoride utilization increased year upon year, particularly after 2012 (P < .001). There was a tendency to reduce the utilization of endodontic therapy (P < .001). The severity of dental caries (number of times receiving dental restoration or endodontic therapy) was decreased after professional topical fluoride application was performed (P < .001).
Conclusion
Because the dental caries rate for preschool children in Taiwan remains high, it is beneficial to receive professional topical fluoride application for dental care, as this reduces the severity of dental caries and endodontic therapy needs.
Keywords: Dental caries, Endodontic therapy, Preschool children, Professional topical fluoride, Restoration treatment
Introduction
Oral health is essential to an individual's general health and quality of life. The World Health Organization (WHO) established the goal of creating nationwide oral health care in 1979, with the theme of “Health for All”. The plan was to make a 2000 Oral Health Goal where 50% of 5-to-6 year-old children were caries-free. For the year 2010, this goal was increased to 90%.1 According to the WHO Global Oral Health Database, tooth decay affects an estimated 60–90% of schoolchildren and nearly 100% of adults worldwide.2 An oral status survey of Taiwanese children under the age of 6 found that the caries prevalence rate was 60% in 3-year-old children, 75% in 4-year-old children, and 89% in 5-year-old children.3 These data show that the prevalence of dental caries in preschool children is higher than the standards set by the WHO. While the prevalence of dental caries has been in decline for the general population over the past decades, dental caries in primary dentition remains a prevalent public health care problem in many countries, including Taiwan. Dental caries is an infectious, multifactorial disease that can occur in very young children and possesses the ability to progress rapidly.4,5
Widespread use of fluoride has been a major factor towards the decline in both the prevalence and severity of dental caries in economically developed countries. Community water fluoridation is the most feasible and cost-effective strategy for reaching entire communities. Water fluoridation has resulted in children experiencing 35% fewer decayed, missing and filled baby teeth, along with 26% fewer decayed, missing and filled permanent teeth. Fluoridation has also led to a 15% increase in the number of children having no decay in their baby teeth, while a 14% increase in children with no decay in their permanent teeth was also a result.6 Unfortunately, such an economical, safe and effective method to better monitor oral hygiene in Taiwan has not been put into use.
The Guideline on Fluoride Therapy, as revised by the American Academy of Pediatric Dentistry (AAPD), recommends professionally applied topical fluoride treatment as being efficacious in reducing caries in children who are at risk.7 Fluoride reduces the incidence of dental caries, while also slowing or reversing the progression of existing lesions. The role that fluoride containing products play in the prevention of dental caries has been reported in many studies, and has also been confirmed through systemic reviews and meta-analysis.8, 9, 10 Most studies have examined fluoride varnish efficacy in the permanent teeth of school-aged children, where the evidence exposing the benefits of applying fluoride varnish to permanent teeth is generally positive.11 A Cochrane collaboration meta-analysis report written by Marinho et al. (2002) estimated the pooled preventive fraction of fluoride varnishes in primary teeth to be 33% (95% CI:19–48%).12 The use of fluoride varnish for inhibiting caries in primary teeth has increased because of its attractive safety properties, as compared to gels and foams.13
In view of the high rate of dental caries in children in Taiwan, the government, in order to improve the oral status of preschool children, offers a free service twice a year for children under 5 years of age. The Preventive Dental Health Service for Children program handled by the Bureau of National Health Insurance (BNHI) in Taiwan, began in July 2004. The Preventive Dental Health Service for Children includes oral examinations, oral hygiene instruction and professional fluoride application. The purpose of this study was to examine the effect and trend of a professional fluoride application program on dental caries in children.
Materials and methods
Study design and population
This study was a secondary data analysis that adopted a sample of one million beneficiaries who were retrieved from Taiwan's National Health Insurance Research Database (NHIRD) in 2010. Taiwan launched a single-payer National Health Insurance program on March 1, 1995, and by 2014, 99.9% of Taiwan's population was enrolled. All contracted institutions must file claims according to standard formats, which are later transformed into the NHIRD. The Longitudinal Health Insurance Database (LHID) 2010 contains all the original claims data of 1,000,000 beneficiaries enrolled in the year 2010, who were randomly sampled from the year 2010 Registry for Beneficiaries of the NHIRD. There the registration data of everyone who was a beneficiary of the National Health Insurance program during the period of January 1, 2010 to December 31, 2010 was drawn for random sampling. There were approximately 27.38 million individuals in this registry at the time. All the registration and claims data of these million individuals collected by the National Health Insurance program constituted the LHID2010. There was no significant difference in the gender and age distribution between the patients in the LHID2010 and the original NHIRD. Therefore, using the LHID to analyze their medical records will be representative of the significance.
Because all personal information was de-identified in the database to protect privacy, no informed consent was required. We selected children who were between 1-to-5 years of age from 2000 to 2012. The exclusion criteria included children diagnosed with amelogenesis imperfecta or dentinogenesis imperfecta (Hereditary disturbances in tooth structure ICD-9-CM code, 520.5). The total population within the study will change based upon the number of people who meet the age range each year. With regards to the utilization of professional topical fluoride application, utilization of restorative treatment, and utilization of endodontic therapy, we gathered data on ambulatory care visits, medical orders, and registry of beneficiaries; included use of the health insurance declaration codes: IC81(Professional topical fluoride program), 89001C, 89002C, 89003C, 89004C, 89005C, 89012C, 89008C, 89009C, 89010C(Restoration treatment), 90005C, 90016C, 90018C (primary tooth endodontic therapy, included pulpotomy and pulpectomy).
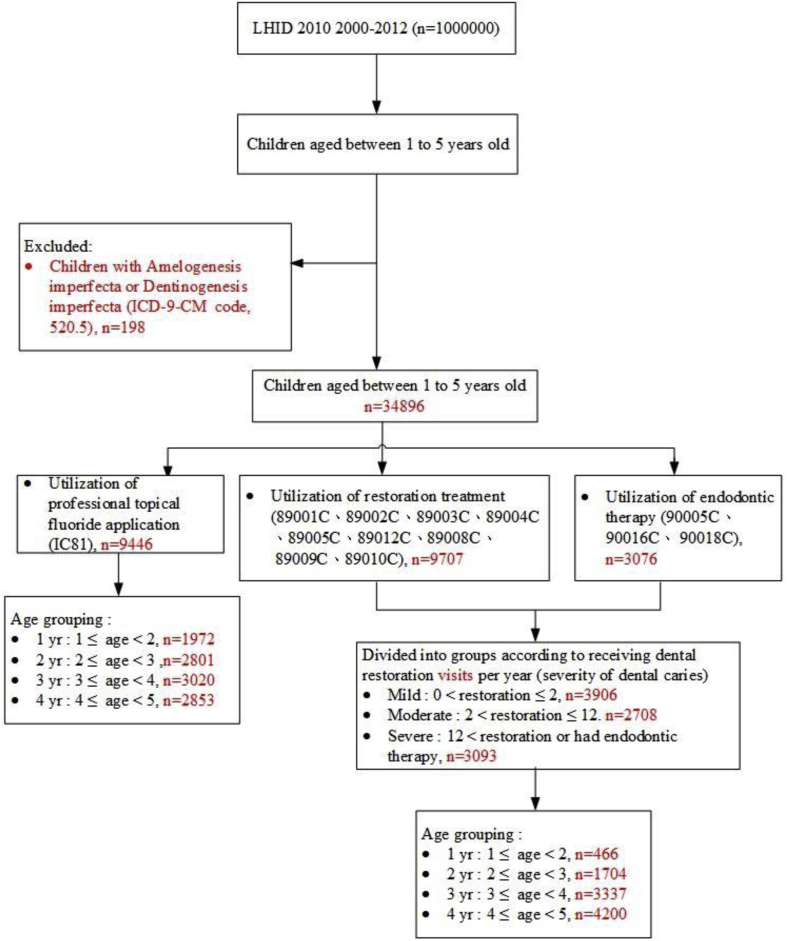
The utilization of professional topical fluoride and dental utilization were grouped according to age. Here, the group of 1 year olds indicates that the child's age is more than or equal to 1, but younger than 2. The remaining groups follow this suit. For the purpose of analysis, the children diagnosed with dental caries were divided into three groups according to the number of visits they had received dental restoration or endodontic therapy; mild, moderate, and severe. Mild level indicated that the number of restorative visits per year was 1 or 2. Moderate indicated that the number of restorative visits per year was between 3 and 12, while severe indicated that the number of restorative visits per year was more than 12, or the patient had undergone endodontic therapy (Fig. 1).
Figure 1.
Flow diagram of the process.
Statistical analysis
All data was managed and analyzed through the use of SAS software, version 9.4 (SAS Institute, Cary, NC, USA). A Cochran–Armitage trend test was used to understand any significant difference in annual utilization. A two-side P value < 0.05 was considered to represent a statistically significant difference.
Results
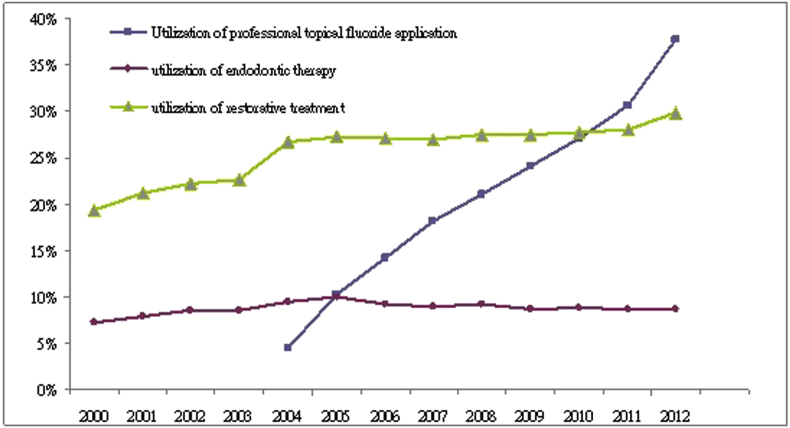
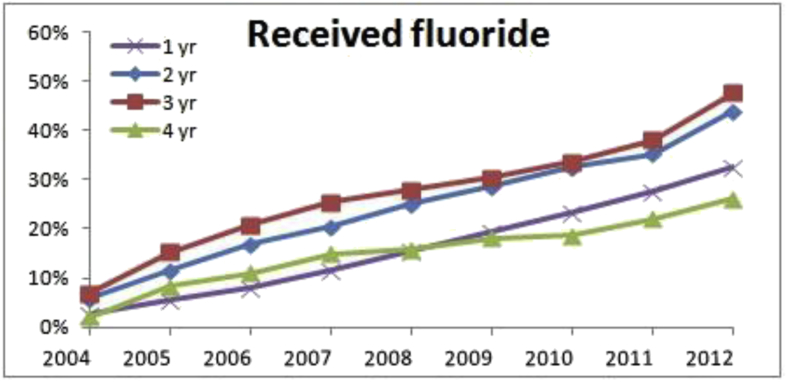
Due to LHID2010, there was no data on one-year old children in 2013, so we abandoned the data from the year 2013. Table 1 presented the utilization of preventive fluoride application and dental services. Overall, the total population who met the age parameters each year was declining. The utilization of professional topical fluoride application was significantly increasing year by year, but remained at no more than 50% (p < .001) (Fig. 2). The utilization of restoration treatment significantly increased from 2000 to 2005, though that trend tended to flatten out in later years (p < .001). The utilization of endodontic therapy initially increased at first, then significantly decreased after 2005 (p < .001). Fig. 3 showed professional topical fluoride utilization as grouped by age. The utilization of professional topical fluoride application throughout each age was significantly increasing (p < .001). Children aged between 2 and 4 years old were a major group receiving professional dental fluoride application (p < 0.001).
Table 1.
Utilization of preventive fluoride application and dental services in Taiwan, 2000–2012.
| year | Total population | Case size of received professional topical fluoride | Utilization of professional topical fluoride application | Case size of restoration treatment |
Utilization of restoration treatment | Case size of endodontic therapy | Utilization of endodontic therapy |
|---|---|---|---|---|---|---|---|
| 2000 | 52,348 | 10,091 | 19.28% | 3787 | 7.23% | ||
| 2001 | 50,583 | 10,706 | 21.17% | 3994 | 7.90% | ||
| 2002 | 49,713 | 11,085 | 22.30% | 4241 | 8.53% | ||
| 2003 | 47,229 | 10,706 | 22.67% | 4047 | 8.57% | ||
| 2004 | 46,131 | 2057 | 4.46% | 12,350 | 26.77% | 4398 | 9.53% |
| 2005 | 43,742 | 4460 | 10.20% | 11,940 | 27.30% | 4372 | 9.99% |
| 2006 | 40,373 | 5731 | 14.20% | 10,939 | 27.09% | 3729 | 9.24% |
| 2007 | 38,186 | 6926 | 18.14% | 10,321 | 27.03% | 3404 | 8.91% |
| 2008 | 36,934 | 7786 | 21.08% | 10,173 | 27.54% | 3416 | 9.25% |
| 2009 | 35,937 | 8673 | 24.13% | 9867 | 27.46% | 3146 | 8.75% |
| 2010 | 34,896 | 9446 | 27.07% | 9707 | 27.82% | 3076 | 8.81% |
| 2011 | 34,228 | 10,477 | 30.61% | 9593 | 28.03% | 2992 | 8.74% |
| 2012 | 31,633 | 11,947 | 37.77% | 9440 | 29.84% | 2743 | 8.67% |
| p-value | <0.001 | <0.001 | <0.001 |
p-value for trend test.
Figure 2.
Utilization of professional topical fluoride application and utilization of dental services in Taiwan, 2000–2012 (p-value for trend test, <0.001).
Figure 3.
Utilization of professional topical fluoride application by age grouping in Taiwan, 2004–2012 (p-value for trend test, <0.001 (all groups)). 1 yr: 1 ≤ age <2, 2 yr: 2 ≤ age <3, 3 yr: 3 ≤ age <4, 4 yr: 4 ≤ age <5.
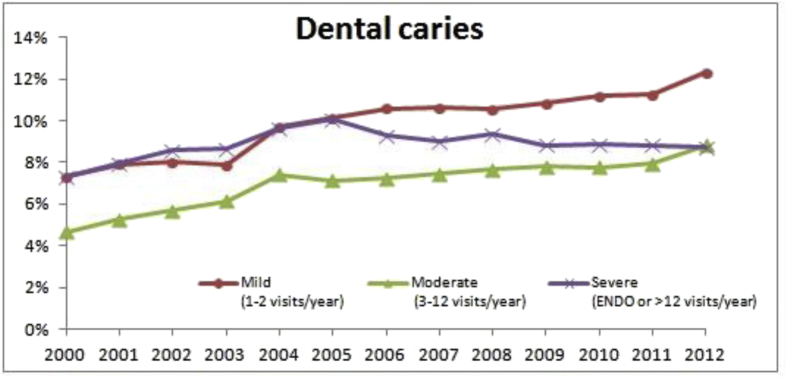
Children who received restoration once or twice per year were a major group in this study. The number within the mild group increased significantly, and this trend was also noted in the moderate group (p < .001) (Table 2). The trend within the severe group showed an increase from 2000 to 2005, but significantly decreased in later years (p < .001) (Fig. 4). Older children had more dental caries. Regardless of which group was studied, children younger than 3 years old whose dental utilization was less than 10%. In the group of 3–5 year olds, the mild caries group numbers increased, while the numbers for the severe caries group decreased, particularly after the year 2005 (p < .001).
Table 2.
Severity of dental caries in Taiwan, 2000–2012.
| Year | Total population | Severity of dental caries |
|||||
|---|---|---|---|---|---|---|---|
| Mild (1–2 visits/year) | Moderate (3–12 visits/year) | Severe (ENDO or >12 visits/year) | |||||
| 2000 | 52,348 | 3830 | 7.32% | 2447 | 4.67% | 3814 | 7.29% |
| 2001 | 50,583 | 4002 | 7.91% | 2675 | 5.29% | 4029 | 7.97% |
| 2002 | 49,713 | 3978 | 8.00% | 2833 | 5.70% | 4274 | 8.60% |
| 2003 | 47,229 | 3727 | 7.89% | 2901 | 6.14% | 4078 | 8.63% |
| 2004 | 46,131 | 4486 | 9.72% | 3423 | 7.42% | 4441 | 9.63% |
| 2005 | 43,742 | 4420 | 10.10% | 3120 | 7.13% | 4400 | 10.06% |
| 2006 | 40,373 | 4269 | 10.57% | 2916 | 7.22% | 3754 | 9.30% |
| 2007 | 38,186 | 4046 | 10.60% | 2841 | 7.44% | 3434 | 8.99% |
| 2008 | 36,934 | 3901 | 10.56% | 2827 | 7.65% | 3445 | 9.33% |
| 2009 | 35,937 | 3893 | 10.83% | 2803 | 7.80% | 3171 | 8.82% |
| 2010 | 34,896 | 3906 | 11.19% | 2708 | 7.76% | 3093 | 8.86% |
| 2011 | 34,228 | 3845 | 11.23% | 2726 | 7.96% | 3022 | 8.83% |
| 2012 | 31,633 | 3893 | 12.31% | 2791 | 8.82% | 2756 | 8.71% |
| p-value | <0.001 | <0.001 | <0.001 | ||||
p-value for trend test.
Figure 4.
Severity of dental caries in Taiwan, 2000–2012 (p-value for trend test, <0.001 (all groups)).
Discussion
The number of children who are younger than five years of age is declining year by year, most likely due to the impact of a low-birth rate. As can be seen from the results, the utilization of professional topical fluoride application was low, as less than 40% of children received professionally applied topical fluoride. A study reported by Kuo et al., in 1999 estimated that only 3% of subjects had ever received a professional topical fluoride application.14 This lower professional topical fluoride application rate was also noted in Liu et al. in a 2005 study (16.67%).15 The reasons for this we suspect could be its deliberate under-promotion by the government due to budget constraints, or patient's limited access to the service. The government later modified regulations, allowing dentists to go into kindergartens (“The children's dental fluoride community tour service program”), making the service more accessible to preschool children in November, 2012. We found an increased proportion of children receiving preventive dental fluoride after the year 2012. This shows the importance of this policy's promotion.
Both fluoridated community drinking water and fluoride toothpaste are the most common sources of fluoride in the United States, and are largely responsible for the low risk in dental caries for most individuals. The AAPD recommend using no more than a smear or rice-size amount of toothpaste in children less than three years of age and then a pea-size amount of fluoridated toothpaste is appropriate for children aged three to six.7 Fluoride toothpaste use in children younger than 6 years show that it is effective in reducing dental caries in primary dentition.16 But an important limitation is that the effectiveness of the toothpaste depends upon the behavior of the individual and the family in regularly using. Children at high risk for dental caries may require more frequent or more concentrated exposure to fluoride, and may well benefit from the use of other fluoride modalities (e.g. mouth rinse, dietary supplements, and topical gel, foam, or varnish). At present, most studies have found that the use of fluoride to prevent dental caries mainly form the local or post-eruptive effect, even if the use of systemic routes for fluoride, such as water fluoridation and fluoride tablets, the main prevention of dental caries effect, still from the local effect.17 Supervised regular use of fluoride mouth-rinse by children and adolescents is associated with a large reduction in caries increment in permanent teeth.18 In Taiwan, a national school-based fluoride mouth-rinse program has been conducted for ordinary children in elementary schools since 2000. The former results of a fluoride mouth-rinse program in Taiwan reported that 0.2% NaF fluoride mouth-rinse once a week is effective in reducing the incidence of new dental caries by 43.9% among ordinary children.19 But fluoride mouth-rinses is not recommended in children with younger age because their parents will be worried about poor skills with gargling or spitting out and swallowing. Fluoride tablets are considered as a safe and economical strategy in preventing and controlling dental caries.20,21 There are worth noting that may influence the efficacy of fluoride tablets involved high price and the compliance of parents or caregivers. In our study, the additional fluoride sources may affect the caries reduction. However, we do not know whether these people use other fluoride patterns (e.g. fluoridated mouth rinse, fluoridated toothpastes and fluoride tablets) from NHIRD.
Taiwan is a non-fluoridated country. One systemic fluoride program is being conducted since 2017, that is salt fluoridation. People can buy fluoridated salt in supermarkets. In Taiwan, the population-based strategies for caries prevention are professional topical fluoride application twice per year (for children less than six years old), school-based topical fluoride mouth rinse program and sealant application on permanent first molars. Fluoride had been shown to produce protection from dental caries on smooth surfaces. However, sealant showed protection on pitted and grooved occlusal surface. The high-risk based strategy for caries prevention is professional topical fluoride application four times per year for children with special conditions included disabled children, children whose families with low socioeconomic status, aboriginal children and children lived in remote areas. Fluoridated toothpaste is a simple, safe, noninvasive and relative inexpensive population intervention. The use of fluoridated toothpaste is recommended. Everyone should be encouraged to brush twice daily with a fluoridated toothpaste. In addition, where the incidence and prevalence of dental caries is moderate to high, or where there are firm indications that the incidence of caries is increasing, an additional source of fluoride should be considered. Three vehicles (water, salt, and milk) have been successfully used in community approaches for providing fluoride to people. If water fluoridation can't be used in Taiwan, salt or milk fluoridation may be the choice. It provides the benefits of fluoride without requiring the consumers to take particular responsibilities or change their behavior. It is important to start in early childhood to ensure an optimal effect on the primary teeth.22 According to AAPD guideline on caries risk assessment, children with high caries risk need professional topical fluoride application every three months.23 It is recommended that another topical fluoride application at their own expense between the two of the government launched topical fluoride applications.
The AAPD guidelines support a dental assessment before either a child's first birthday or first tooth eruption. Professional topical fluoride efficacy for these younger children provides an additional protective effect, particularly for those children in a caries high-risk group. Marinho and colleagues demonstrated a 37% reduction in decayed, missing, and filled tooth surfaces (dmfs) during primary dentition following regular fluoride varnish applications. This was independent of the patient's caries level and caries risk of the population, as well as exposure to other sources of fluoride.10 One randomized clinical trial found a statistically significant difference in caries incidence between children who received and those who did not receive fluoride varnish application twice a year, along with a dose–response effect regarding caries incidence Odds Ratios (OR).24 The odds of developing caries was higher for children who received only caregiver counseling, than it was for those who received fluoride varnish once per year (OR = 2.2) and twice per year (OR = 3.77). A study comparing the caries preventive effect of fluoride varnish application performed both two and four times a year during a 2-year clinical trial for children aged 9–13 years, found no difference in DMFS increments between the groups.25 The Taiwan government had launched a free professional fluoride application program every 180 days for children under 5 years of age (now for those under 6 years of age). The government may feel that there is a funding problem or actual clinical effect, but the program they have offered has been better than nothing.
The majority of children in Taiwan possess a high caries risk.26 The results of studies present the major group that received endodontic therapy to be 3-to-5 year old children. The utilization of dental restoration treatment was increased in this study because providing topical fluoride service increases the chances of additional visits and dental treatments. Decreased the severity of dental caries may be due to professional topical fluoride application. It may also due to professional topical fluoride application provide dentists the opportunity to diagnosis initial caries and then restore the cavity before it worsens further. This finding is very important to the clinician. We all know that prevention is better than treatment. When the complexity of the treatment is reduced, the number of times that children receive dental treatment will be reduced, and even the acceptance or cooperative attitude during dental treatment may be improved. As a result, fear of dentistry can be reduced. Peyon et al. examined the progression of proximal caries in the primary molars of preschool children over a 2-year period study. After 2 years, 66.7% of the caries lesions in the fluoride varnish group, and 91.2% in the control group showed progression using a radiographic scoring system (27% reduction).27 However, in three different 2-year long cluster-randomized controlled trials, they reported no statistically significant differences in caries incidence among test and control preschool childre.28, 29, 30 They explained that the negative results could be due to the habitual and established tooth brushing routines, along with other fluoride modalities.
It is well known that dental caries is a complex disease with a variety of risk factors. Concentrations of Mutans Streptococci (MS) bacteria, dietary factors and plaque levels have also been frequently associated with caries in young children. There were some limitations in this study. The NHIRD do not know the type of fluoride gel or varnish that dentists use, the children's oral hygiene conditions and whether there was use of any other fluoride modalities (e.g. fluoride toothpaste and fluoride tablets) in this study. This information will affect the results and increase the risk of bias. In addition, children with disabilities, children whose families with low socioeconomic status, aboriginal children and children lived in remote areas are included in this study. The government had launched a free topical fluoridation program every three months for these children.
We suggest that the government provide more available channels which will give its citizens better access to these publicly funded services. The government must also provide a professional topical fluoride program in conjunction with caregiver oral health education and health promotion programs targeting improvement in prenatal and young children's nutrition, in order to address the root causes of early childhood caries.
Although the dental caries rate for preschool children in Taiwan remains high, within the limitations of this field study it is beneficial to receive professional topical fluoride application for dental care, as it reduces the severity of dental caries and endodontic therapy needs.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
References
- 1.World Health Organization . 2003. The World Oral Health Report 2003. Geneva.http://www.who.int/oral_health/publications/world-oral-health-report-2003/en/ Available from: [Google Scholar]
- 2.Petersen P.E., Lennon M.A. Effective use of fluorides for the prevention of dental caries in the 21st century: the WHO approach. Community Dent Oral Epidemiol. 2004;32:319–321. doi: 10.1111/j.1600-0528.2004.00175.x. [DOI] [PubMed] [Google Scholar]
- 3.Tsai Y.L., Hsiang C.L., Lee L.A., Chi L. 1997. Oral Health Status Under 6 Years Old Children In Taiwan. Health Care Research Report Of Department Of Health, Executive Yuan; pp. 28–29. [Google Scholar]
- 4.Selwitz R.H., Ismail A.I., Pitts N.B. Dental caries. Lancet. 2007;369:51–59. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 5.Bratthall D., Hänsel Petersson G., Sundberg H. Reasons for the caries decline: what do the experts believe? Eur J Oral Sci. 1996;104:416–422. doi: 10.1111/j.1600-0722.1996.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 6.Iheozor-Ejiofor Z., Worthington H.V., Walsh T. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD010856.pub2. CD010856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Pediatric Dentistry Guideline on fluoride therapy. Pediatr Dent. 2016;38:181–184. [PubMed] [Google Scholar]
- 8.Helfenstein U., Steiner M. Fluoride varnishes (Durphat): a meta-analysis. Community Dent Oral Epidemiol. 1994;22:1–5. doi: 10.1111/j.1600-0528.1994.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 9.Strohmenger L., Brambilla E. The use of fluoride varnishes in the prevention of dental caries: a short review. Oral Dis. 2001;7:71–80. [PubMed] [Google Scholar]
- 10.Marinho V.C.C., Worthington H.V., Walsh T., Clarkson J.E. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD002279.pub2. CD002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NIH Diagnosis and management of dental caries throughout life. National institutes of health consensus development conference statement, March 26-28, 2001. J Dent Educ. 2001;65:1162–1168. [PubMed] [Google Scholar]
- 12.Marinho V.C., Higgins J.P., Logan S., Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2002;3 doi: 10.1002/14651858.CD002279. CD002279. [DOI] [PubMed] [Google Scholar]
- 13.Roberts J.F., Longhurst P. A clinical estimation of the fluoride used during application of a fluoride varnish. Br Dent J. 1987;162:463–466. doi: 10.1038/sj.bdj.4806168. [DOI] [PubMed] [Google Scholar]
- 14.Kuo H.W., Chen L.L., Huang H.Y., Wang R.Y., Lin H.C. Factors influencing knowledge of and attitude toward fluoride in Taiwan. Chin Dent J. 1999;18:9–18. [Google Scholar]
- 15.Liu Y.H., Lo C.H., Chen H.S. Utilization of topical fluoride gel in children: at the department of pediatric dentistry of a medical center in southern Taiwan. Taiwan J Pediatr Dent. 2005;5:152–156. [Google Scholar]
- 16.Wright J.T., Hanson N., Ristic H., Whall C.W., Estrich C.G., Zentz R.R. Fluoride toothpaste efficacy and safety in children younger than 6 years: a systematic review. J Am Dent Assoc. 2014;145:182–189. doi: 10.14219/jada.2013.37. [DOI] [PubMed] [Google Scholar]
- 17.Featherstone J.D. Prevention and reversal of dental caries: role of low level fluoride. Community Dent Oral Epidemiol. 1999;27:31–40. doi: 10.1111/j.1600-0528.1999.tb01989.x. [DOI] [PubMed] [Google Scholar]
- 18.Marinho V.C., Chong L.Y., Worthington H.V., Walsh T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2016;7 doi: 10.1002/14651858.CD002284.pub2. CD002284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuo M.K., Chia H.F., Wu Y.K., Chen C.S., Huang S.T. Department of Health, Executive Yuan; Taipei, Taiwan: 1997. Implementation Of School Fluoride Mouthrinsing Program And Its Effectiveness On Caries Prevention. (Report No. DOH86-HP004-3M02) [Google Scholar]
- 20.D'Hoore W., Van Nieuwenhuysen J.P. Benefits and risks of fluoride supplementation: caries prevention versus dental fluorosis. Eur J Pediatr. 1992;151:613–616. doi: 10.1007/BF01957733. [DOI] [PubMed] [Google Scholar]
- 21.O'Rourke C.A., Attrill M., Holloway P.J. Cost appraisal of a fluoride tablet programme to Manchester primary schoolchildren. Community Dent Oral Epidemiol. 1988;16:341–344. doi: 10.1111/j.1600-0528.1988.tb00578.x. [DOI] [PubMed] [Google Scholar]
- 22.Mariño R., Villa A., Guerrero S. A community trial of fluoridated powered milk in Chile. Community Dent Oral Epidemiol. 2001;29:435–442. doi: 10.1034/j.1600-0528.2001.290604.x. [DOI] [PubMed] [Google Scholar]
- 23.American Academy of Pediatric Dentistry Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent. 2016;38:142–149. [PubMed] [Google Scholar]
- 24.Weintraub J.A., Ramos-Gomez F., Jue B. Fluoride varnish efficacy in preventing early childhood caries. J Dent Res. 2006;85:172–176. doi: 10.1177/154405910608500211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seppä L., Tolonen T. Caries preventive effect of fluoride varnish applications performed two or four times a year. Scand J Dent Res. 1990;98:102–105. doi: 10.1111/j.1600-0722.1990.tb00947.x. [DOI] [PubMed] [Google Scholar]
- 26.Tsai A.I., Chen C.-Y., Li L.-A., Hsiang C.-L., Hsu K.-H. Risk indicators for early childhood caries in Taiwan. Community Dent Oral Epidemiol. 2006;34:437–445. doi: 10.1111/j.1600-0528.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- 27.Peyron M., Matsson L., Birkhed D. Progression of approximal caries in primary molars and the effect of Duraphat treatment. Scand J Dent Res. 1992;100:314–318. doi: 10.1111/j.1600-0722.1992.tb01078.x. [DOI] [PubMed] [Google Scholar]
- 28.Lawrence H.P., Binguis D., Douglas J. A 2-year community-randomized controlled trial of fluoride varnish to prevent early childhood caries in aboriginal children. Community Dent Oral Epidemiol. 2008;36:503–516. doi: 10.1111/j.1600-0528.2008.00427.x. [DOI] [PubMed] [Google Scholar]
- 29.Slade G.D., Bailie R.S., Roberts-Thomson K. Effect of health promotion and fluoride varnish on dental caries among Australian Aboriginal children: results from a community randomized controlled trial. Community Dent Oral Epidemiol. 2011;39:29–43. doi: 10.1111/j.1600-0528.2010.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson M., Dahllöf G., Twetman S., Jansson L., Bergenlid A.C., Grindefjord M. Effectiveness of early preventive intervention with semiannual fluoride varnish application in Toddlers living in high-risk areas: a stratified cluster-randomized controlled trial. Caries Res. 2016;50:17–23. doi: 10.1159/000442675. [DOI] [PubMed] [Google Scholar]