Abstract
One-fifth of healthcare beneficiaries in developed nations get discharged from hospitals to physician supervised skilled nursing care facilities. In low-income and middle-income countries like India, postdischarge skilled nursing facilities are at a very nascent stage and largely underequipped in terms of infrastructure, skilled nursing and physician staff to manage complicated patients. Hence the responsibility of management of such patients lies largely with their families. We present a case where a 26-year-old man with Duchenne Muscular Dystrophy who became ventilator dependent following major surgeries was weaned off his ventilator and rehabilitated back to his prehospital state. This was done at his home with visiting nurses and rehabilitation services under telemedicine supervision by a critical care specialist. Use of telemedicine services could be a viable and cost-effective option to ensure adherence to evidence-based medicine and standardisation of care in resource limited countries such as India.
Keywords: rehabilitation medicine, intensive care, chronic disease / disability nursing, public health
Case presentation
A 26-year-old man who suffered from Duchenne muscular dystrophy (DMD) underwent surgical fixation of multiple fractures after he sustained a fall. The patient had osteopenia due to prolonged steroid use for his muscular dystrophy and 2 weeks prior to presentation, he sustained a fall resulting in multiple joint and rib fractures. An open surgical reduction and fixation of bilateral hip and right shoulder was performed. Postoperatively, the patient developed respiratory failure requiring mechanical ventilation and subsequently developed hospital acquired pneumonia and septic shock. While in the hospital, he was resuscitated with fluids, given appropriate antibiotic coverage and required vasopressor therapy. Subsequently his septic shock resolved, however he remained ventilator dependent due to critical illness polyneuromyopathy superimposed on his compromised respiratory reserve due to DMD. Over the next 2 weeks, he suffered several other complications including intensive care unit (ICU) delirium. After performing tracheostomy, the patient and family decided to provide home based long-term acute care/skilled nursing facility (LTAC/SNF) using telemedicine.
A team of teleintensivists that had significant experience providing tele-ICU services for a US-based health system were approached by the family. A careful analysis of available hardware and software was done to assemble the most cost-effective and reliable solution. This needed multiple reviews by the experienced team of local vendors and suppliers along with rapid testing of open source technologies following which computers and cameras were installed at the patient’s home for remote monitoring and teleconferencing in addition to standard patient monitoring equipment. The installed cameras had Pan-Tilt-Zoom functionality that was critical to a detailed review of the patient. The cameras could be remotely operated by the intensivists and could provide the intensivists with a detailed view of ventilator waveforms and breathing patterns of the patient. With these views and the assistance of the bedside nurse, the intensivists were able to change settings on the ventilator in real time while viewing the breathing patterns and ventilator waveforms. A reliable internet connection was chosen from the existing providers and a real-time video conferencing platform, freely available on the internet was used to communicate with the bedside team, family and the patient. Specially trained critical care nurses were arranged for daily visits in addition to a round the clock home health aide. Daily visits by a physical therapist was arranged for providing chest physiotherapy and limb exercises. Following his 2-week ICU stay, the patient was discharged from the hospital to his fully set up home LTAC facility in a severely debilitated condition requiring round the clock mandatory modes of mechanical ventilation to support his breathing.
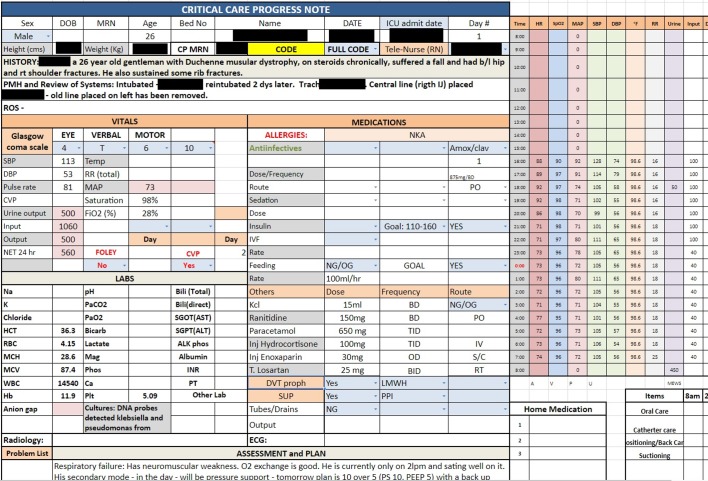
The initial days of this new set up were learning experience for the patient, family and the care team. The episodes of delirium from lack of sleep were particularly distressing for the family during this phase. The patient’s mother and sister were advised to be at his bedside and help reorient him during this period. In addition, sunlight exposure during the day and minimising interruption to his sleep at night in conjunction with minimal pharmacological interventions (melatonin) helped him tide over this predicament. Benzodiazepines were explicitly avoided. We were able to execute these measures effectively at a home setting as they were not limited by any visiting hour restrictions. The comfort of his parents’ company and their psychological support greatly helped in alleviating his mood and kept him motivated to continue his rehabilitation one day at a time. In view of his respiratory failure and his complex underlying neuromuscular disease, he was placed on a closely monitored protocol for ventilator weaning supervised by his team of teleintensivists who were also trained in pulmonology and had expertise in neuromuscular disease. Our protocol was similar to the one described by Bach et al.1 The patient was initially on volume control (VC) round the clock. Pressure support (PS) ventilation trials were done for a few hours every day and eventually he was on PS during the day and on VC at night. We began progressive reductions in the level PS once he was on PS for 24 hours. Subsequently, we transitioned to Continuous Positive Airway Pressure in the day and PS at night and eventually trach collar in the day and non-invasive ventilation (NIV) at night with a capped tracheostomy tube. Once we were satisfied with work of breathing and he met criteria with his peak cough flow assessment we decannulated him and transitioned him to nocturnal NIV via face mask. Daily telerounds were conducted with the bedside team, family and the patient to guide his therapy. Using a direct audiovisual interface, patient was assessed and inputs from the bedside caregivers were recorded on the electronic daily note (figure 1) along with the plan for the day. This was sent and printed out at the patient’s end for the use of bedside caregivers. In addition, a protocolised regimen of secretion clearance using a combination of hypertonic saline, bronchodilator nebulisations, cough assist device, vibrating vest and physical therapy was employed with great success.
Figure 1.
Snapshot of daily progress note used for the patient.
After 50 days, the patient was back to his usual routine of monthly outpatient visits to his doctor and weekly physical therapy sessions. At the end of 6 months, the patient was on a daily regimen of nocturnal NIV and was participating in regular social and professional activities including an overseas vacation with his family.
Global health problem list
Lack of LTAC and SNFs in India.
Shortage of intensivists in the country and the potential of telemedicine services to increase the outreach of their services and bridge the critical care service gap.
Disparities in the accessibility to post-ICU care and rehabilitation where home telemedicine may be a possible solution.
Lack of awareness about the potential of telemedicine among patients, doctors and healthcare decision-makers.
Global health problem analysis
Post-ICU rehabilitation is a multidisciplinary undertaking which is taxing both in terms of the healthcare resource utilisation and the effort from the patient’s family.2 A significant disparity has been shown to exist with the current approaches of post-ICU rehabilitation facilities even among developed countries.3 In countries such as USA, 20% of medicare beneficiaries admitted to hospitals get discharged to a short-term or long-term SNF.4 These facilities help reduce the hospital/ICU length of stay and thereby decongest acute care facilities and reduce family fatigue.
Such facilities for post-ICU rehabilitation are scant in number and are ill equipped to cater to the patients who require intensive rehabilitation in low-income and middle-income countries (LMIC) such as India. The burden of rehabilitation and nursing care at the time of recovery from a critical illness is either undertaken by the family or done partially in the hospital/intensive care wards, with the former being the rule and latter the exception. A shortage of doctors, nurses and paramedical personnel, poorly executed public health policies are few of the factors that led to this dire situation. The Indian government spending allocated to healthcare is 3.84% of GDP, which is lower than developed nations and even lower than several comparable LMIC.5 India currently has one doctor for every 1596 of its population which is below the WHO recommended ratio of one doctor for 1000 population.6 A shortage of trained intensive care specialists is even more alarming with the total number being about 3500 across the country.7 8 From our experience with the above presented case, the use of telemedicine in coordinating the delivery of home-based rehabilitation services seems promising in improving the overall efficiency of the system in LMIC such as India. Additionally, reduced family fatigue and increased satisfaction was reported from our patient’s family with this approach.
There are challenges involved in bringing about such a change to the current system. First, the inability to perform the conventional bedside face-to-face encounter with a thorough physical examination appears to be a barrier to many traditional practitioners. In our opinion, this is more due to a misunderstanding about the role of telemedicine and its benefits than an actual failure of the system. A lack of awareness of such options and their utility among the patients, healthcare management and policy-makers also lead to delays in adoption. In the USA, substantially more evidence exists regarding the cost efficacy and quality improvement that telemedicine brings to the health system.9 Tele-ICU networks are fairly prevalent in the USA and represent an active area of outcomes based research.10 11 Data on the benefits of telemedicine technology on the health system is currently lacking in the Indian setting and our hope is that our case report highlights the need for more studies in this area.
Second, in our experience, telemedicine platforms and technology solutions developed in the West are far too expensive for the Indian setting. There is a perception among practitioners in rural India that such ‘expensive’ systems are not applicable to India. This is a significant barrier to adoption of telemedicine and in particular tele-ICU systems and can be solved if local talent and insight are utilised to develop pragmatic solutions.
Third, while internet bandwidth was not a concern in this case, internet penetration in various areas of India is suboptimal for high quality audio–video transmission. As the connectivity and communication infrastructure continues to improve we see this as a diminishing problem over time, at least as far as the Indian mainland is concerned.
Given the lack of LTACs/SNFs, if operations such as the one demonstrated in this case are rolled out in a structured fashion, telecentres which are staffed with experts in conjunction with trained bedside nurses and therapists could help take care of such patients in the home setting which may reduce overall systemic costs and potentially optimise resource utilisation without compromising patient safety.12 We face an acute shortage of intensivists and trained personnel in India and tools such as telemedicine may help us better ration these scarce resources.
Learning points.
There is a shortage of critical care specialists and a lack of long-term acute care or skilled nursing facilities (LTAC or SNFs) in India which leads to poor and inefficient delivery of rehabilitation services to patients to help them get back to their usual life post hospitalisation.
Provision of post intensive care unit discharge services at home by a bedside multidisciplinary team and the patient’s family, coordinated by a critical care specialist using telemedicine technology may pose a feasible and economic alternative to SNFs and LTACs in a resource-limited setting.
Cost-effective telemedicine technologies could be deployed in a resource-limited setting utilising homegrown/open source solutions. This requires analysis of available resources by a team with expertise in telemedicine and with a strong background in technology application and customisation.
Footnotes
Contributors: DU, DR, DJ and BSA have directly contributed to the manuscript preparation of the case report or care of the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Bach JR, Gonçalves MR, Hamdani I, Winck JC. Extubation of patients with neuromuscular weakness: a new management paradigm. Chest. 2010 May 1;137(5):1033-9. (cited 6 Dec 2018). [DOI] [PubMed]
- 2. Choi J, Tate JA, Hoffman LA, et al. . Fatigue in family caregivers of adult intensive care unit survivors. J Pain Symptom Manage 2014;48:353–63. 10.1016/j.jpainsymman.2013.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. SpringerLink. More than the tip of the iceberg: association between disabilities and inability to attend a clinic-based post-ICU follow-up and how it may impact on health inequalities. https://link.springer.com/article/10.1007%2Fs00134-018-5146-4 (cited 6 Dec 2018). [DOI] [PubMed]
- 4. march-2016-report-to-the-congress-medicare-payment-policy.pdf [Internet]. [ http://www.medpac.gov/docs/default-source/reports/march-2016-report-to-the-congress-medicare-payment-policy.pdf (cited 2018 Dec 6). [Google Scholar]
- 5. HFP-IND.pdf [Internet]. http://apps.who.int/iris/bitstream/handle/10665/259642/HFP-IND.pdf?sequence=1 (cited 6 Dec 2018).
- 6. WHO. Density of physicians (total number per 1000 population, latest available year) [Internet]. WHO. http://www.who.int/gho/health_workforce/physicians_density/en/ (cited 6 Dec 2018).
- 7. Courses [Internet]. https://isccm.org/courses.aspx (cited 6 Dec 2018).
- 8. Welcome To National Board Of Examination [Internet]. http://natboard.edu.in/fellowship.php (cited 6 Dec 2018).
- 9. de la Torre-Díez I, López-Coronado M, Vaca C, et al. . Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health 2015;21:81–5. 10.1089/tmj.2014.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lilly CM, Cody S, Zhao H, et al. . Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011;305:2175–83. 10.1001/jama.2011.697 [DOI] [PubMed] [Google Scholar]
- 11. Kohl BA, Fortino-Mullen M, Praestgaard A, et al. . The effect of ICU telemedicine on mortality and length of stay. J Telemed Telecare 2012;18:282–6. 10.1258/jtt.2012.120208 [DOI] [PubMed] [Google Scholar]
- 12. Udeh C, Udeh B, Rahman N, et al. . Telemedicine/Virtual ICU: Where Are We and Where Are We Going? Methodist Debakey Cardiovasc J 2018;14:126–33. 10.14797/mdcj-14-2-126 [DOI] [PMC free article] [PubMed] [Google Scholar]